Abstract
Purpose
The systematic review aims to analyze and summarize the characteristics of living systematic review (LSR) for coronavirus disease 2019 (COVID-19).
Methods
Six databases including Medline, Excerpta Medica (Embase), Cochrane Library, China National Knowledge Infrastructure (CNKI), Wanfang Database and China Science, and Technology Journal Database (VIP), were searched as the source of basic information and methodology of LSR. Descriptive analytical methods were used to analyze the included COVID-19 LSRs, and the study characteristics of COVID-19 LSRs were further assessed.
Results
Sixty-four COVID-19 LSRs were included. Eighty-nine point one percent of LSRs were published on Science Citation Index (SCI) journals, and 64.1% publication with an impact factor (IF) >5 and 17.2% with an IF >15 among SCI journals. The first unit of the published LSRs for COVID-19 came from 19 countries, with the largest contribution from the UK (17.2%, 11/64). Forty point six percent of LSRs for COVID-19 were related to therapeutics topic which was considered the most concerned perspective for LSRs for COVID-19. Seventy-six point six percent of LSRs focused on the general population, with less attention to children, pregnant women and the elderly. However, the LSR for COVID-19 was reported incomplete on “living” process, including 40.6% of studies without search frequency, 79.7% of studies without screening frequency, 20.3% of studies without update frequency, and 65.6% of studies without the timing or criteria of transitioning LSR out of living mode.
Conclusion
Although researchers in many countries have applied LSRs to COVID-19, most of the LSRs for COVID-19 were incomplete in reporting on the “living” process and less focused on special populations. This could reduce the confidence of health-care providers and policy makers in the results of COVID-19 LSR, thereby hindering the translation of evidence on COVID-19 LSR into clinical practice. It was necessary to explicitly enact preferred reporting items for systematic reviews and meta-analyses (PRISMA) to improve the reporting quality of LSR and support ongoing efforts of therapeutics research for special patients with COVID-19.
Introduction
The outbreak of coronavirus disease 2019 (COVID-19) in December 2019, has rapidly spread to 220 countries and regions, leading to the global pandemicity.Citation1 According to the latest data from World Health Organization (WHO), over 562 million people have been diagnosed and over six million people have died from COVID-19 up tol July 22, 2022.Citation2 To cope with the epidemic and severity of COVID-19, many countries accelerated research of diagnosis, vaccination and therapeutics, which cause a surge in the number of clinical studies on COVID-19 in a short time.Citation3,Citation4 From January 1, 2020 to May 6, 2020, 1694 clinical trials related to COVID-19 were authorized and can be found in five international clinical trial registries.Citation5 However, a study from the British Medical Journal (BMJ) suggested that the large amount of studies on COVID-19 resulted in increased difficulty to respond quickly and effectively to devise an appropriate crisis response strategy to the novel coronavirus, which had also hugely impacted the mental health of health-care employees due to overload of work and exhaustion under the COVID-19 pandemic.Citation6
As high-level evidence in evidence-based medicine, a systematic review (SR) acts as a bridge to connect research outcomes and clinical practice, providing a reference for clinical practitioners to contribute quick and accurate decisions.Citation7–9 Although the methodology of SR is relatively mature, its updating mechanism for publication is immature.Citation10 Once literature been published, only a few SRs were updated within two years.Citation11 Most SRs failed to incorporate new evidence timely, resulting in their conclusions differing from the true effect of interventions.Citation10
To solve the delayed update of publication analyzed in SRs and accurately reflect the effect of interventions on COVID-19, Elliott et al proposed the concept of a living systematic review (LSR) in 2014, and defined it as a “systematic review which was continually updated, incorporating relevant new evidence as it becomes available”.Citation7,Citation12 Elliott et al suggested, an acceptable and appropriate LSR required to follow three criteria: (1) the review question is a particular challenge and its solution needs to be priorities to decision-making; (2) the existing evidence is insufficient and uncertain for questions to be solved; (3) the emerging evidence is likely to impact conclusions of the LSR.Citation7,Citation12 However, some studies showed that LSRs might face unexpected challenges and difficulties under the COVID-19 pandemic with a changeable epidemiological landscape and substantial clinical uncertainty.Citation13,Citation14
Therefore, this systematic review analyzes and summarizes the characteristics of LSRs for COVID-19, which aims to identify potential problems and provide references to further improve the quality of LSRs for COVID-19.
Methods
This study was a systematic review and conducted in accordance with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines.Citation15
Six databases were searched systematically, including Medline, Excerpta Medica (Embase), Cochrane Library, China National Knowledge Infrastructure (CNKI), Wanfang Database and China Science and Technology Journal Database (VIP), as of May 16, 2022. The search strategy was specific for each database and included a combination of the medical subject headings and free text terms for “living systematic review” or “living system review” or “living system evaluation” or “living systematic evaluation” or “living meta-analysis”.
This manuscript included all the living systematic reviews for COVID-19 and was not limited by language. Two researchers independently screened the studies. When two researchers had opposite opinions, disputes were decided by the third researcher. EndNote™ X8 software was used for deduplication and back-to-back screening by two researchers.
The information extraction table was designed in advance, and the pretest was conducted with 10% of the included LSR. Two researchers extracted the information of the included LSR back-to-back, and the extracted results were compared by the third researcher. The information extraction table included three parts: (1) general characteristics: title, author, published year, country, institution, name and impact factor of journal, topic, population, quality assessment tool, etc; (2) methodology of LSP: type of LSR, registration information, search methods, search frequency, data synthesis methods, updated frequency, etc; (3) transitioning LSR out of living mode: time or criteria for transitioning LSR out of living mode.
Searched records were managed by EndNote™ (V.X9, Clarivate, Philadelphia, Pennsylvania, USA). Statistical analysis was done by MS Excel 2019. Descriptive analysis and tables were used to present the results. Binary variables (such as first institution’s country, study topics and study population) were displayed in frequency and percentage. Continuous variables (such as impact factor, search frequency, screening frequency, update frequency) were displayed in mean, standard deviation and range. Due to the large heterogeneity of LSR included in this study, meta-analysis was not intended to be performed in this study.
Results
Study Selection
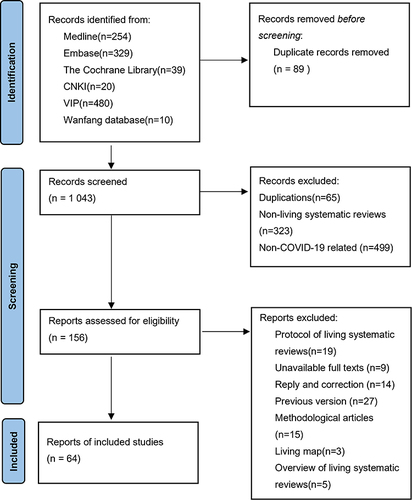
A total of 1132 studies were initially included. After excluding duplicate studies, 1043 studies remained. After reading the title, abstract and full text, 64Citation16–79 studies were included. A summary of the study selection process is reported in .
Basic Information of LSR for COVID-19
Most (89.1%) LSRs were published in SCI journal.Citation16–21,Citation23–44,Citation46–51,Citation53–57,Citation59–69,Citation73–79 The impact factor published in SCI journals ranged from 1.04 to 39.89, with an average of 11.72 and a standard deviation of 11.30. The impact factor of 64.1% studies was >5,Citation16–20,Citation23,Citation26,Citation27,Citation30,Citation32,Citation33,Citation36,Citation37,Citation39–44,Citation46,Citation47,Citation49–51,Citation54–57,Citation60–64,Citation67–69,Citation73–76,Citation79 the impact factor of 17.2% studies was >15.Citation16,Citation17,Citation23,Citation42,Citation43,Citation51,Citation62–64,Citation74,Citation76 LSRs were published in journals with high impact factor, which indicated COVID-19 related studies have attracted much attention from readers (). In addition, the included LSRs were distributed in 19 countries and regions around the world, covering high-income countries, upper-middle-income countries, low-middle-income countries and low-income countries.
Table 1 Basic Information of COVID-19 for LSR
The study topics covered all aspects of the health-care field, including prevalence, clinical manifestation, etiology, prevention, diagnosis, treatment, and prognosis. The topic most studied (40.6%) was the treatment of COVID-19.Citation20,Citation22,Citation25,Citation32,Citation37,Citation39,Citation43,Citation46,Citation47,Citation49,Citation51,Citation55,Citation56,Citation58,Citation62–64,Citation67–74,Citation79 The population most studied (76.6%) was general COVID-19 patients,Citation18–23,Citation26,Citation27,Citation29,Citation31–34,Citation36,Citation37,Citation39,Citation42–44,Citation46,Citation47,Citation49–65,Citation67–76,Citation79 but there were fewer (6.3%) studies concerning pregnant womenCitation16,Citation17,Citation30,Citation78 and childrenCitation28,Citation30,Citation77,Citation78 with COVID-19, even no study concerning the elderly with COVID-19. (, Supplementary Material Table 1)
Methodology of LSR for COVID-19
In the production phase of LSR, most of the LSRs registeredCitation16–22,Citation25,Citation26,Citation28–33,Citation35,Citation37,Citation39–42,Citation45–62,Citation65–67,Citation69–73,Citation76–79 (81.2%) and wrote the protocolCitation16–35,Citation37,Citation39–43,Citation45–67,Citation69–73,Citation76–79 (92.2%) before the study started. Less than one third of the LSRs searched the Chinese databaseCitation16–18,Citation23,Citation25,Citation34,Citation35,Citation43,Citation46,Citation48,Citation57,Citation62–64,Citation70,Citation79 (25%), and less than half of the LSRs searched the preprint databaseCitation16,Citation20,Citation21,Citation23–26,Citation28,Citation37,Citation39,Citation40,Citation43,Citation45,Citation46,Citation48,Citation51,Citation53,Citation57,Citation62–64,Citation67,Citation68,Citation73,Citation76,Citation77,Citation79 (42.2%), and two-thirds of the LSRs searched 12 COVID-19 databasesCitation16,Citation17,Citation20–23,Citation27,Citation30,Citation32,Citation33,Citation37–42,Citation44–46,Citation48,Citation49,Citation51,Citation54–56,Citation58–64,Citation67,Citation69–77,Citation79(67.2%)(Supplementary Material Table 2). More than half (51.6%) of LSRs used the same frequency to search different databases regularly,Citation16–18,Citation20,Citation24–26,Citation30,Citation32,Citation35–37,Citation39,Citation40,Citation43–46,Citation48,Citation49,Citation51,Citation52,Citation55,Citation59,Citation61,Citation62,Citation66–69,Citation73,Citation74,Citation79 and the frequency of searches ranged from once a day to once every six months, with an average of once every 28 days, with a standard deviation of 42.68 (Supplementary Material Table 3). Seventy-nine point seven percent of LSRs did not report screening frequency.Citation16–31,Citation33–36,Citation38,Citation39,Citation42–48,Citation50,Citation51,Citation53–55,Citation57–59,Citation61–64,Citation66,Citation69–72,Citation74–79 Less than one-third (19.5%) of LSRs took into account the possible false-positive probability of repeated meta-analyses.Citation23,Citation42,Citation46,Citation48,Citation56,Citation63,Citation64 Methods of data synthesis included traditional meta-analysis methods (80.5%) and nontraditional meta-analysis methods (19.5%), which respectively referred to “the statistical methods for meta-analysis in the Cochrane Guidelines for Systematic Reviews” and “use of meta-analytic methods to adjust for frequent updating, such as Bayesian, trial sequential analysis, sequential meta-analysis, the Shuster method, Law of the iterated logarithmCitation2–4”. Only 34.4% of LSRs reported time or criteria for transitioning LSR out of living modeCitation16,Citation17,Citation19,Citation21–24,Citation45,Citation52,Citation54–56,Citation58,Citation62–64,Citation66,Citation70–72,Citation76(Supplementary Material Table 4). Among them, the time to exit “living” mode is from one to two years, the average exit time is 1.78 years, and the standard deviation is 0.42. ()
Table 2 Methodology of LSR for COVID-19
In the review, publish and update phase of LSR, only a small number (7.8%) of LSRs had relatively stable peer reviewers.Citation23,Citation42,Citation43,Citation63,Citation64 All the LSRs presented the results to readers through journals. But there were still 23.4% of LSRs that showed the results through a more convenient and quick way (website or software).Citation23,Citation26,Citation32,Citation37,Citation38,Citation42,Citation46,Citation48,Citation50,Citation52,Citation54,Citation63,Citation64,Citation71,Citation72 Thirty-four point 4 percent of LSRs were updated regularly.Citation16,Citation18,Citation19,Citation21,Citation23,Citation26,Citation27,Citation31,Citation35,Citation37,Citation45,Citation50–52,Citation54,Citation56,Citation62,Citation64,Citation65,Citation74,Citation78 The update frequency of LSRs ranged from weekly to annually, with an average of every 95 days, with a standard deviation of 80.51. Seventy-six point six percent of LSRs were never updated (, Supplementary Material Tables 1 and 5).
In addition, less than one-fifth (18.8%) of LSRs used technology in the production process,Citation22,Citation23,Citation27,Citation37,Citation45,Citation56,Citation58,Citation64,Citation70–72,Citation76 and most of them (10.9%) were in the search process.Citation22,Citation37,Citation45,Citation58,Citation70–72 ()
Discussion
This study systematically reviewed 64 LSRs for COVID-19 and analyzed the characteristics of LSR for COVID-19. Meanwhile, we found unsolved challenges in LSRs by summarizing their basic information and methodology of LSRs. Consequently, we generated some suggestions to improve efficiency and quality of LSRs for COVID-19 with regard to these challenges.
It was noteworthy that 18.8% of LSRs for COVID-19 were not registered in advance, which might be the reason for the existence of partial LSRs for COVID-19 repeated in similar topics. For example, three similar LSRs in the clinical topic of remdesivir for COVID-19 were found.Citation20,Citation71,Citation74 In the meantime, three similar LSRs on the topic of cell therapy for COVID-19 also occurred.Citation47,Citation58,Citation63 Potential reasons for the replication might be that some authors considered publishing the study without registration could be quicker, especially under the requirement of numerous SRs applications for registration under the COVID-19 pandemic.Citation80 Although registration might delay publication of LSRs, to improve the quality of LSRs and reduce replicated publications, it was still recommended that LSRs should be registered prior to commencement.Citation81–83
Brierley et al found that nearly 37.5% of the COVID-19 studies were published in the preprint database,Citation84 but only 42.2% of LSRs for COVID-19 searched the preprint database. This might be due to concerns that preprints were not as reliable as peer-reviewed articles,Citation85 and relying on preprints to draw conclusions could cause unstable practical expressions in clinical practice. However, Brierley et al’s study demonstrated that there was no qualitative difference after tracking COVID-19 preprints and final published versions.Citation84 Therefore, considering the complicated and time-consuming progression of traditional peer review to be published and the urgency of COVID-19 pandemic, we suggested that LSRs for COVID-19 considered searching preprint databases, to open up the possibility of providing timely potential solutions for clinical challenges from COVID-19.
Among 38 LSRs for COVID-19, the average search frequency was 28 days, similar to the monthly search frequency suggested by Cochrane Guidance and Lansky.Citation12,Citation86 However, searching monthly was still difficult to persist in most studies. In studies by Cochrane GuidanceCitation12 and Millard,Citation8 hours of monthly search could be as high as 32 hours, along with the aggravated workload. Regarding to the elevated time consumption for research of COVID-19, the establishment of COVID-19 Comprehensive Database became increasingly important in the development of LSRs.Citation7,Citation12,Citation87–89 The L·OVE COVID-19 platform, which obtained information from the Epistemonikos database and used artificial intelligence and expert opinions, integrates the information and releases the heavy workload on data search and organization for the researcher.Citation14,Citation90 The L·OVE COVID-19 platform was characterized with real-time updating of COVID-19 studies, Pierre et al and Butcher et al demonstrated that the L·OVE COVID-19 platform had a very good sensitivity for identifying studies evaluating interventions for COVID-19.Citation89,Citation91 To improve work efficiency, LSR for COVID-19 should search a comprehensive database of COVID-19.
Among 20 LSRs for COVID-19, the average search frequency was 95 days, much higher than the yearly update suggested by Créquit et al,Citation92 indicating that research evidence was produced rapidly under the COVID-19 pandemic. However, frequent updates which is premature could drain the research team’s resources and ultimately lead to the disruption of the LSR, which is a problem that would be magnified especially during the COVID-19 pandemic.Citation14 Therefore, LSRs should have an appropriate update frequency in combination with comprehensive research focusing on this newly emerged evidence.
Subsequently, we found that only about one-third of COVID-19 LSRs reported a time or criterion for exiting living mode, and the remaining COVID-19 LSRs did not report or even consider this matter. It was impossible to stay in living mode in terms of time or funding. Therefore, clear time or criterion for exiting living mode is as important as deciding to start living mode in an LSR, especially under the COVID-19 pandemic when it was hard to predict when new evidence would emerge. Taken together, authors of the LSR should periodically review the clinical topics of interest, the speed and amount of new evidence produced, and its own resources, and then combine the above points to decide whether to transition LSR out of living mode.
Meanwhile, we found only 18.8% of LSRs for COVID-19 used machine automation to increase productivity. Thomas et al believed that human resources were scarce resources in LSR, so use of machine automation could improve the feasibility and sustainability of LSR. Automation could assist with some LSR tasks, including searching, eligibility assessment, data extraction or collection, quality evaluation, and synthesis. However, Thomas et al and Tercero-Hidalgo et al also recognized that the existing automation technology was only suitable for the early stages of the LSR production process (ie searching, eligibility assessment, etc), and the automation technology in the later stages of the LSR production process still required further research and development.Citation87,Citation93 Therefore, we propose LSR should be developed with automated techniques.
In addition, the poor reporting quality of the 64 LSRs for COVID-19, especially the part of the methodology of LSR, were observed. Iannizzi et al suggested that transparent and traceable reporting of changes in LSR methods became challenging under the COVID-19 pandemic.Citation14 One of the reasons for this challenge might be currently no reporting guideline for LSRs. Although the PRISMA statement was updated in 2020, it emphasized that when used for LSRs, some additional obstacles need to be addressed.Citation94 Four key modules assessed in traditional SRs (publication format, work processes, author team management, and statistical methods),Citation7 could not be evaluated in PRISMA 2020 statement for LSRs. Therefore, the evaluation process following PRISMA 2020 statement only promises the reporting quality of LSR as a traditional SR, but not the reporting quality of a “living” SR. Fortunately, the deficiency of PRISMA 2020 statement was noticed by the PRISMA team. The specific protocol of PRISMA for LSR had been published, and it is claimed that PRISMA for LSR would be part of the PRISMA extension.Citation9
In contrast, there are still several limitations in this study. First, the methodological quality and reporting quality of LSR has not been considered in this study. Although the recently updated PRISMA 2020Citation94 statement claimed that it could be used for LSR, there were still some additional problems. Moreover, the commonly used methodological quality assessment tools AMSTAR 2 and ROBIS were not suitable for LSR.Citation95,Citation96 Second, this study did not identify the optimal search frequency, update frequency, and appropriate technological enablers. In the future, we could focus on developing appropriate PRISMA for LSR and exploring suitable search frequency, update frequency, and more available technological enablers, which may improve the quality of LSR.
Conclusion
LSRs are high-quality, up-to-date online summaries of health research, updated as new research becomes available,Citation7 and enabled by improved production efficiency. Transparent reporting of changes in methodology between review updates is essential. And transparent reporting is needed to avoid biases in the review process. But most of the LSRs for COVID-19 were incomplete in reporting on the “living” process. This could reduce the confidence of health-care providers and policy makers in the results of COVID-19 LSRs, thereby hindering the translation of evidence on COVID-19 LSR into clinical practice. The results of this work not only provide an evidential foundation for PRISMA for the LSR development team, but also make recommendations for further applications of LSR under COVID-19.
Disclosure
Zhe Chen and Jiefeng Luo should be considered as co-first authors. The authors report no conflicts of interest in this work.
References
- CNN health. Tracking Covid-19ʹs global spread; 2022. Available from: https://edition.cnn.com/interactive/2020/health/coronavirus-maps-and-cases/. Accessed May 16, 2022.
- World Health Organization. WHO coronavirus disease (COVID-19) dashboard; 2022. Available from: https://covid19.who.int/. Accessed August 1, 2022.
- Cai X, Fry CV, Wagner CS. International collaboration during the COVID-19 crisis: autumn 2020 developments. Scientometrics. 2021;126(4):3683–3692. doi:10.1007/s11192-021-03873-7
- Else H. How a torrent of COVID science changed research publishing — in seven charts. Nature. 2020;588(7839):553. doi:10.1038/d41586-020-03564-y
- Ramanan M, Stolz A, Rooplalsingh R, et al. An evaluation of the quality and impact of the global research response to the COVID-19 pandemic. Med J Aust. 2020;213(8):380–80.e1. doi:10.5694/mja2.50790
- Casigliani V, De Nard F, De Vita E, et al. Too much information, too little evidence: is waste in research fuelling the covid-19 infodemic? BMJ. 2020;370:m2672. doi:10.1136/bmj.m2672
- Elliott JH, Turner T, Clavisi O, et al. Living systematic reviews: an emerging opportunity to narrow the evidence-practice gap. PLoS Med. 2014;11(2):e1001603. doi:10.1371/journal.pmed.1001603
- Millard T, Synnot A, Elliott J, et al. Feasibility and acceptability of living systematic reviews: results from a mixed-methods evaluation. Syst Rev. 2019;8(1):325–425. doi:10.1186/s13643-019-1248-5
- Iannizzi C, Akl EA, Kahale LA, et al. Methods and guidance on conducting, reporting, publishing and appraising living systematic reviews: a scoping review protocol. F1000Res. 2021;10:802–902. doi:10.12688/f1000research.55108.1
- Ji DH XU. A brief introduction of living systematic review. Chin J Evid Based Med. 2020;20(2):244–248.
- Jadad AR, Cook DJ, Jones A, et al. Methodology and reports of systematic reviews and meta-analyses: a comparison of Cochrane reviews with articles published in paper-based journals. JAMA. 1998;280(3):278–280. doi:10.1001/jama.280.3.278
- Brooker J, Synnot A, McDonald S,et al. Guidance for the production and publication of Cochrane living systematic reviews: Cochrane Reviews in living mode; 2019. Available from: https://community.cochrane.org/sites/default/files/uploads/inline-files/Transform/201912_LSR_Revised_Guidance.pdf. Accessed March 9, 2022.
- Negrini S, Ceravolo MG, Côté P, et al. A systematic review that is ``rapid’’ and ``living’’: a specific answer to the COVID-19 pandemic. J Clin Epidemiol. 2021;138:194–198. doi:10.1016/j.jclinepi.2021.05.025
- Iannizzi C, Dorando E, Burns J, et al. Methodological challenges for living systematic reviews conducted during the COVID-19 pandemic: a concept paper. J Clin Epidemiol. 2022;141:82–89. doi:10.1016/j.jclinepi.2021.09.013
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339(jul21 1):b2535. doi:10.1136/bmj.b2535
- Allotey J, Chatterjee S, Kew T, et al. SARS-CoV-2 positivity in offspring and timing of mother-to-child transmission: living systematic review and meta-analysis. BMJ. 2022;376:e067696. doi:10.1136/bmj-2021-067696
- Allotey J, Fernandez S, Bonet M, et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020;370:m3320. doi:10.1136/bmj.m3320
- Amer YS, Titi MA, Godah MW, et al. International alliance and AGREE-ment of 71 clinical practice guidelines on the management of critical care patients with COVID-19: a living systematic review. J Clin Epidemiol. 2022;142:333–370. doi:10.1016/j.jclinepi.2021.11.010
- Amorim Dos Santos J, Normando AGC, Carvalho da Silva RL, et al. Oral manifestations in patients with COVID-19: a 6-month update. J Dent Res. 2021;100(12):1321–1329. doi:10.1177/00220345211029637
- Ansems K, Grundeis F, Dahms K, et al. Remdesivir for the treatment of COVID-19. Cochrane Database Syst Rev. 2021;8(8):Cd014962. doi:10.1002/14651858.Cd014962
- Asiimwe IG, Pushpakom S, Turner RM, et al. Cardiovascular drugs and COVID-19 clinical outcomes: a living systematic review and meta-analysis. Br J Clin Pharmacol. 2021;87(12):4534–4545. doi:10.1111/bcp.14927
- Baladia E, Pizarro AB, Ortiz-Muñoz L, et al. Vitamin C for COVID-19: a living systematic review. Medwave. 2020;20(6):e7978. doi:10.5867/medwave.2020.06.7978
- Bartoszko JJ, Siemieniuk RAC, Kum E, et al. Prophylaxis against covid-19: living systematic review and network meta-analysis. BMJ. 2021;373(949). doi:10.1136/bmj.n949
- Bell V, Wade D. Mental health of clinical staff working in high-risk epidemic and pandemic health emergencies a rapid review of the evidence and living meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2021;56(1):1–11. doi:10.1007/s00127-020-01990-x
- Bonardi O, Wang Y, Li K, et al. Effects of COVID-19 mental health interventions among children, adolescents, and adults not quarantined or undergoing treatment due to COVID-19 infection: a systematic review of randomised controlled trials. The Canadian Journal of Psychiatry. 2022;67(5):336–350. doi:10.1177/07067437211070648
- Brümmer LE, Katzenschlager S, Gaeddert M, et al. Accuracy of novel antigen rapid diagnostics for SARS-CoV-2: a living systematic review and meta-analysis. PLoS Med. 2021;18(8):e1003735. doi:10.1371/journal.pmed.1003735
- Buitrago-Garcia D, Egli-Gany D, Counotte MJ, et al. Occurrence and transmission potential of asymptomatic and presymptomatic SARS-CoV-2 infections: a living systematic review and meta-analysis. PLoS Med. 2020;17(9):e1003346. doi:10.1371/journal.pmed.1003346
- Bwire GM, Njiro BJ, Mwakawanga DL, et al. Possible vertical transmission and antibodies against SARS-CoV-2 among infants born to mothers with COVID-19: a living systematic review. J Med Virol. 2021;93(3):1361–1369. doi:10.1002/jmv.26622
- Cares-Marambio K, Montenegro-Jiménez Y, Torres-Castro R, et al. Prevalence of potential respiratory symptoms in survivors of hospital admission after coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis. Chron Respir Dis. 2021;18:14799731211002240. doi:10.1177/14799731211002240
- Centeno‐Tablante E, Medina‐Rivera M, Finkelstein JL, et al. Transmission of SARS-CoV-2 through breast milk and breastfeeding: a living systematic review. Ann N Y Acad Sci. 2021;1484(1):32–54. doi:10.1111/nyas.14477
- Ceravolo MG, Andrenelli E, Arienti C, et al. Rehabilitation and COVID-19: rapid living systematic review by cochrane rehabilitation field - third edition. Eur J Phys Rehabil Med. 2021;57(5):850–857. doi:10.23736/s1973-9087.21.07301-9
- Davidson M, Menon S, Chaimani A, et al. Interleukin-1 blocking agents for treating COVID-19. Cochrane Database Syst Rev. 2022;1(1):Cd015308. doi:10.1002/14651858.Cd015308
- Deeks JJ, Dinnes J, Takwoingi Y, et al. Antibody tests for identification of current and past infection with SARS-CoV-2. Cochrane Database Syst Rev. 2020;6(6):Cd013652. doi:10.1002/14651858.Cd013652
- Dong F, Liu H-L, Dai N, et al. A living systematic review of the psychological problems in people suffering from COVID-19. J Affect Disord. 2021;292:172–188. doi:10.1016/j.jad.2021.05.060
- Dzinamarira T, Nkambule SJ, Hlongwa M, et al. Risk factors for COVID-19 infection among healthcare workers. A first report from a living systematic review and meta-analysis. Saf Health Work. 2022. doi:10.1016/j.shaw.2022.04.001
- Elvidge J, Summerfield A, Nicholls D, et al. Diagnostics and treatments of COVID-19: a living systematic review of economic evaluations. Value Health. 2022;25(5):773–784. doi:10.1016/j.jval.2022.01.001
- Ghosn L, Chaimani A, Evrenoglou T, et al. Interleukin-6 blocking agents for treating COVID-19: a living systematic review. Cochrane Database Syst Rev. 2021;3(3):Cd013881. doi:10.1002/14651858.Cd013881
- Gómez-Ochoa SA, Franco OH, Rojas LZ, et al. COVID-19 in health-care workers: a living systematic review and meta-analysis of prevalence, risk factors, clinical characteristics, and outcomes. Am J Epidemiol. 2021;190(1):161–175. doi:10.1093/aje/kwaa191
- Griesel M, Wagner C, Mikolajewska A, et al. Inhaled corticosteroids for the treatment of COVID-19. Cochrane Database Syst Rev. 2022;3(3):Cd015125. doi:10.1002/14651858.Cd015125
- Harder T, Koch J, Vygen-Bonnet S, et al. Efficacy and effectiveness of COVID-19 vaccines against SARS-CoV-2 infection: interim results of a living systematic review, 1 January to 14 May 2021. Euro Surv. 2021;26(28). doi:10.2807/1560-7917.Es.2021.26.28.2100563
- Harder T, Külper-Schiek W, Reda S, et al. Effectiveness of COVID-19 vaccines against SARS-CoV-2 infection with the Delta (B.1.617.2) variant: second interim results of a living systematic review and meta-analysis. Euro Surv. 2021;26(41). doi:10.2807/1560-7917.Es.2021.26.41.2100920
- Helfand M, Fiordalisi C, Wiedrick J, et al. Risk for reinfection after SARS-CoV-2: a living, rapid review for American College of physicians practice points on the role of the antibody response in conferring immunity following SARS-CoV-2 infection. Ann Intern Med. 2022. doi:10.7326/m21-4245
- Hernandez AV, Roman YM, Pasupuleti V, et al. Hydroxychloroquine or chloroquine for treatment or prophylaxis of COVID-19: a living systematic review. Ann Intern Med. 2020;173(4):287–296. doi:10.7326/m20-2496
- Hussain S, Riad A, Singh A, et al. Global prevalence of COVID-19-associated mucormycosis (CAM): living systematic review and meta-analysis. J Fungi. 2021;7(11). doi:10.3390/jof7110985
- John A, Eyles E, Webb RT, et al. The impact of the COVID-19 pandemic on self-harm and suicidal behaviour: update of living systematic review. F1000Res. 2020;9:1097. doi:10.12688/f1000research.25522.2
- Juul S, Nielsen EE, Feinberg J, et al. Interventions for treatment of COVID-19: a living systematic review with meta-analyses and trial sequential analyses (The LIVING Project). PLoS Med. 2020;17(9):e1003293. doi:10.1371/journal.pmed.1003293
- Kirkham AM, Monaghan M, Bailey AJM, et al. Mesenchymal stem/stromal cell-based therapies for COVID-19: first iteration of a living systematic review and meta-analysis: mSCs and COVID-19. Cytotherapy. 2022. doi:10.1016/j.jcyt.2021.12.001
- Korang SK, von Rohden E, Veroniki AA, et al. Vaccines to prevent COVID-19: a living systematic review with Trial Sequential Analysis and network meta-analysis of randomized clinical trials. PLoS One. 2022;17(1):e0260733. doi:10.1371/journal.pone.0260733
- Kreuzberger N, Hirsch C, Chai KL, et al. SARS-CoV-2-neutralising monoclonal antibodies for treatment of COVID-19. Cochrane Database Syst Rev. 2021;9(9):Cd013825. doi:10.1002/14651858.CD013825
- Langford BJ, So M, Raybardhan S, et al. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect. 2020;26(12):1622–1629. doi:10.1016/j.cmi.2020.07.016
- Mackey K, King VJ, Gurley S, et al. Risks and impact of angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers on SARS-CoV-2 infection in adults: a living systematic review. Ann Intern Med. 2020;173(3):195–203. doi:10.7326/m20-1515
- Maguire BJ, McLean ARD, Rashan S, et al. Baseline results of a living systematic review for COVID-19 clinical trial registrations. Wellcome Open Res. 2020;5:116. doi:10.12688/wellcomeopenres.15933.1
- Melo AKG, Milby KM, Caparroz A, et al. Biomarkers of cytokine storm as red flags for severe and fatal COVID-19 cases: a living systematic review and meta-analysis. PLoS One. 2021;16(6):e0253894. doi:10.1371/journal.pone.0253894
- Michelen M, Manoharan L, Elkheir N, et al. Characterising long COVID: a living systematic review. BMJ Global Health. 2021;6(9). doi:10.1136/bmjgh-2021-005427
- Mikolajewska A, Fischer AL, Piechotta V, et al. Colchicine for the treatment of COVID-19. Cochrane Database Syst Rev. 2021;10(10):Cd015045. doi:10.1002/14651858.Cd015045
- O’Byrne L, Webster KE, MacKeith S, et al. Interventions for the treatment of persistent post-COVID-19 olfactory dysfunction. Cochrane Database Syst Rev. 2021;7(7):Cd013876. doi:10.1002/14651858.CD013876
- Qiu X, Nergiz AI, Maraolo AE, et al. The role of asymptomatic and pre-symptomatic infection in SARS-CoV-2 transmission-a living systematic review. Clin Microbiol Infect. 2021;27(4):511–519. doi:10.1016/j.cmi.2021.01.011
- Rada G, Corbalán J, Rojas P. Cell-based therapies for COVID-19: a living, systematic review. Medwave. 2020;20(11):e8079. doi:10.5867/medwave.2020.11.8078
- Rocha APD, Atallah ÁN, Pinto A, et al. COVID-19 and patients with immune-mediated inflammatory diseases undergoing pharmacological treatments: a rapid living systematic review. Sao Paulo Med J. 2020;138(6):515–520. doi:10.1590/1516-3180.2020.0421.R2.10092020
- Salameh JP, Leeflang MM, Hooft L, et al. Thoracic imaging tests for the diagnosis of COVID-19. Cochrane Database Syst Rev. 2020;9:Cd013639. doi:10.1002/14651858.CD013639
- Schlesinger S, Neuenschwander M, Lang A, et al. Risk phenotypes of diabetes and association with COVID-19 severity and death: a living systematic review and meta-analysis. Diabetologia. 2021;64(7):1480–1491. doi:10.1007/s00125-021-05458-8
- Schünemann HJ, Khabsa J, Solo K, et al. Ventilation techniques and risk for transmission of coronavirus disease, including COVID-19: a living systematic review of multiple streams of evidence. Ann Intern Med. 2020;173(3):204–216. doi:10.7326/m20-2306
- Siemieniuk RA, Bartoszko JJ, Díaz Martinez JP, et al. Antibody and cellular therapies for treatment of covid-19: a living systematic review and network meta-analysis. BMJ. 2021;374:n2231. doi:10.1136/bmj.n2231
- Siemieniuk RA, Bartoszko JJ, Ge L, et al. Drug treatments for covid-19: living systematic review and network meta-analysis. BMJ. 2020;370:m2980.
- Silveira FM, Mello ALR, da Silva Fonseca L, et al. Morphological and tissue-based molecular characterization of oral lesions in patients with COVID-19: a living systematic review. Arch Oral Biol. 2022;136:105374. doi:10.1016/j.archoralbio.2022.105374
- Soto-Cámara R, García-Santa-Basilia N, Onrubia-Baticón H, et al. Psychological Impact of the COVID-19 pandemic on out-of-hospital health professionals: a living systematic review. J Clin Med. 2021;10(23). doi:10.3390/jcm10235578
- Stroehlein JK, Wallqvist J, Iannizzi C, et al. Vitamin D supplementation for the treatment of COVID-19: a living systematic review. Cochrane Database Syst Rev. 2021;5(5):Cd015043. doi:10.1002/14651858.Cd015043
- Tleyjeh IM, Kashour Z, Riaz M, et al. Efficacy and safety of tocilizumab in COVID-19 patients: a living systematic review and meta-analysis, first update. Clin Microbiol Infect. 2021;27(8):1076–1082. doi:10.1016/j.cmi.2021.04.019
- Valk SJ, Piechotta V, Chai KL, et al. Convalescent plasma or hyperimmune immunoglobulin for people with COVID-19: a rapid review. Cochrane Database Syst Rev. 2020;5(5):Cd013600. doi:10.1002/14651858.Cd013600
- Verdejo C, Vergara-Merino L, Meza N, et al. Macrolides for the treatment of COVID-19: a living, systematic review. Medwave. 2020;20(11):e8074. doi:10.5867/medwave.2020.11.8073
- Verdugo-Paiva F, Acuña MP, Solá I, et al. Remdesivir for the treatment of COVID-19: a living systematic review. Medwave. 2020;20(11):e8080. doi:10.5867/medwave.2020.11.8080
- Verdugo-Paiva F, Izcovich A, Ragusa M, et al. Lopinavir-ritonavir for COVID-19: a living systematic review. Medwave. 2020;20(6):e7967. doi:10.5867/medwave.2020.06.7966
- Wagner C, Griesel M, Mikolajewska A, et al. Systemic corticosteroids for the treatment of COVID-19. Cochrane Database Syst Rev. 2021;8(8):Cd014963. doi:10.1002/14651858.Cd014963
- Wilt TJ, Kaka AS, MacDonald R, et al. Remdesivir for adults with COVID-19: a living systematic review for American College of physicians practice points. Ann Intern Med. 2021;174(2):209–220. doi:10.7326/m20-5752
- Webster KE, O'Byrne L, MacKeith S, et al. Interventions for the prevention of persistent post-COVID-19 olfactory dysfunction.Interventions for the prevention of persistent post-COVID-19 olfactory dysfunction. Cochrane Database Syst Rev. 2021;7(7):Cd013877. doi:10.1002/14651858.CD013877.pub2
- Wynants L, Van Calster B, Collins GS, et al. Prediction models for diagnosis and prognosis of covid-19: systematic review and critical appraisal. BMJ. 2020;369:m1328. doi:10.1136/bmj.m1328
- Xu W, Li X, Dong Y, et al. SARS-CoV-2 transmission in schools: an updated living systematic review. J Glob Health. 2021;11:10004. doi:10.7189/jogh.11.10004
- Yang J, D’Souza R, Kharrat A, et al. Coronavirus disease 2019 pandemic and pregnancy and neonatal outcomes in general population: a living systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2022;101(1):7–24. doi:10.1111/aogs.14277
- Zhang X, Shang L, Fan G, et al. The efficacy and safety of janus kinase inhibitors for patients with COVID-19: a living systematic review and meta-analysis. Front Med. 2021;8:800492. doi:10.3389/fmed.2021.800492
- Dotto L, Kinalski MA, Machado PS, et al. The mass production of systematic reviews about COVID-19: an analysis of PROSPERO records. J Evid Based Med. 2021;14(1):56–64. doi:10.1111/jebm.12426
- Sideri S, Papageorgiou SN, Eliades T. Registration in the international prospective register of systematic reviews (PROSPERO) of systematic review protocols was associated with increased review quality. J Clin Epidemiol. 2018;100:103–110. doi:10.1016/j.jclinepi.2018.01.003
- Chien PF, Khan KS, Siassakos D. Registration of systematic reviews: PROSPERO. BJOG. 2012;119(8):903–905. doi:10.1111/j.1471-0528.2011.03242.x
- Ge L, Tian JH, Li YN, et al. Association between prospective registration and overall reporting and methodological quality of systematic reviews: a meta-epidemiological study. J Clin Epidemiol. 2018;93:45–55. doi:10.1016/j.jclinepi.2017.10.012
- Brierley L, Nanni F, Polka JK, et al. Tracking changes between preprint posting and journal publication during a pandemic. PLoS Biol. 2022;20(2):e3001285. doi:10.1371/journal.pbio.3001285
- Rawlinson C, Bloom T. New preprint server for medical research. BMJ. 2019;365:l2301. doi:10.1136/bmj.l2301
- Lansky A, Wethington HR. Living systematic reviews and other approaches for updating evidence. Am J Public Health. 2020;110(11):1687–1688. doi:10.2105/ajph.2020.305920
- Thomas J, Noel-Storr A, Marshall I, et al. Living systematic reviews: 2. Combining human and machine effort. J Clin Epidemiol. 2017;91:31–37. doi:10.1016/j.jclinepi.2017.08.011
- Chou R, Dana T, Shetty KD. Testing a machine learning tool for facilitating living systematic reviews of chronic pain treatments. In: AHRQ Methods for Effective Health Care. Rockville (MD): Agency for Healthcare Research and Quality (US); 2020.
- Butcher R, Sampson M, Couban RJ, et al. The currency and completeness of specialized databases of COVID-19 publications. J Clin Epidemiol. 2022;147:52–59. doi:10.1016/j.jclinepi.2022.03.006
- Rada G, Pérez D, Araya-Quintanilla F, et al. Epistemonikos: a comprehensive database of systematic reviews for health decision-making. BMC Med Res Methodol. 2020;20(1):286. doi:10.1186/s12874-020-01157-x
- Pierre O, Riveros C, Charpy S, et al. Secondary electronic sources demonstrated very good sensitivity for identifying studies evaluating interventions for COVID-19. J Clin Epidemiol. 2021;141:46–53. doi:10.1016/j.jclinepi.2021.09.022
- Créquit P, Martin-Montoya T, Attiche N, et al. Living network meta-analysis was feasible when considering the pace of evidence generation. J Clin Epidemiol. 2019;108:10–16. doi:10.1016/j.jclinepi.2018.12.008
- Tercero-Hidalgo JR, Khan KS, Bueno-Cavanillas A, et al. Artificial intelligence in COVID-19 evidence syntheses was underutilized, but impactful: a methodological study. J Clin Epidemiol. 2022;148:124–134. doi:10.1016/j.jclinepi.2022.04.027
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71–n71. doi:10.1136/bmj.n71
- Whiting P, Savović J, Higgins JP, et al. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225–234. doi:10.1016/j.jclinepi.2015.06.005
- Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi:10.1136/bmj.j4008