Abstract
Aim of the Database
The aim of the Danish Cardiac Arrest Registry is to monitor the quality of prehospital cardiac arrest treatment, evaluate initiatives regarding prehospital treatment of cardiac arrest, and facilitate research.
Study Population
All patients with prehospital cardiac arrest in Denmark treated by the emergency medical services in whom resuscitation or defibrillation has been attempted.
Main Variables
The Danish Cardiac Arrest Register records descriptive and qualitative variables as outlined in the “Utstein” template for reporting out-of-hospital-cardiac arrest. Main variables include whether the case was witnessed, whether the cardiac arrest was electrocardiographically monitored, the timing of cardiopulmonary resuscitation, and the timing of the first analysis of the cardiac rhythm. The outcome measures are the status of the patient at handover to the hospital, return of spontaneous circulation, and 30-day survival after event.
Database Status
The Danish Cardiac Arrest Registry was established in June 2001, and all Danish emergency medical services are reporting to the database.
Conclusion
The Danish Cardiac Arrest Registry is among the oldest Danish national clinical registries, with a high quality of clinical data and coverage. This registry provides the prerequisite for all research on out-of-hospital cardiac arrest research in Denmark and is essential for monitoring and improving the quality of care for patients suffering from out-of-hospital cardiac arrest.
Introduction
The Danish Cardiac Arrest Registry (DCAR) for Out-of-Hospital Cardiac Arrest (OHCA) collects data on prehospital treatment and post-event outcomes for patients with OHCA in Denmark since 2001. The registry was implemented to provide a tool for benchmarking the initiatives in the treatment of prehospital cardiac arrest. The objective of this paper is to describe the register, the results from the register and the quality indicators associated to the registry. The results obtained from the registry have supported some central initiatives to increase survival in the treatment of Danish OHCA.
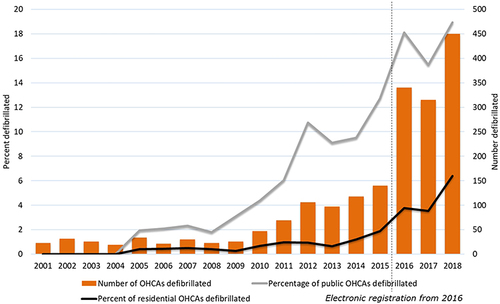
Among the examples is the continuous monitoring of bystander-assisted cardiopulmonary resuscitation (CPR) rate, which serves as a vital indicator for large-scale national programs to increase survival.Citation1,Citation2 Furthermore, specific indicators related to the treatment of patients with OHCA have been developed. Therefore, to describe the use of automatic external defibrillators (AED) by bystanders or citizen responders, the registry has implemented an indicator on the use of AED before the arrival of the Emergency Medical Services (EMS) personnel. Indicators such as this have enabled the national steering committee of the registry to support campaigns nudging the society to increase the public willingness to intervene in cases of OHCA by providing numbers and figures on the activity of citizen responders activity. This, undoubtedly, has led to an increase in the survival of patients suffering from OHCA.Citation1 See .
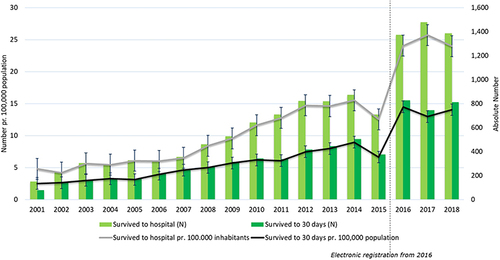
Figure 1 Number of survivors of cardiac arrest outside hospital per 100,000 inhabitants and in absolute numbers 2001–2018.
The data available from the registry also enabled reports documenting an improved overall survival of all patients with OHCA significantly, and in particular of patients in public spaces with easy access to AEDs.Citation1 See .
The registry has further spurred different projects in Denmark: A National AED register providing an overview of all publicly available AEDs has been implemented.Citation3 This registry has been made available to all emergency medical dispatch centers (EMDC). Thus, in cases of OHCA, the dispatcher can guide bystanders and citizen responders over the phone to access the nearest AED and bring it to the scene of the cardiac arrest.Citation4 This effort further led to a different project where the individual EMDC could activate citizen responders to go to the scene of the cardiac arrest or to pick up an AED on their way to the scene of the OHCA. If a citizen responder arrived at the scene before the ambulance, the citizen responder could thus contribute to the treatment of the patient by defibrillating patients with shockable rhythm and perform CPR. This project, the national Heart Runner Project, is presently awaiting evaluation that will be based on data from the DCAR. Yet another project inspired by the results from the registry was a study on improving recognition of OHCA by medical dispatchers over the phone.Citation5 The use of artificial intelligence (AI) on the actual conversations to 1-1-2 emergency helpline has proven so good in recognising over 85% of all OHCA that it has been decided to implement this AI model in all EMSs in Denmark to assist the medical dispatchers in their work.Citation2,Citation6 Furthermore, the registry has been used in formal quality assurance projects.Citation7
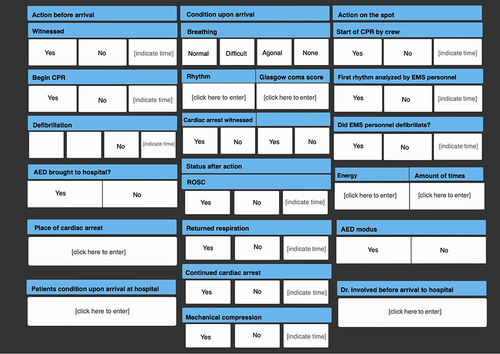
All Danish emergency medical services are reporting to the registry using a standardized electronic reporting system based via a tablet for data entry at the scene of the cardiac arrest (see ). During the last 20 years, the register has undergone a transition from manual data collection (2001–2015) to the use of digital, online data registering (from 2016). The registry has been accepted as a National Clinical Registry in the program of the National Clinical Registries under the Danish Health Law. Moreover, the results of the quality measured on bystander CPR, use of a public AED and the treatment given by the EMS personnel have improved a lot over the years.Citation1 Delivery of data to the registry has been changed from paper-based forms that were electronically entered into the database. These data are now automatically extracted from prehospital medical records allowing daily delivery of reliable data back to each regional EMS organization and is in scope for the register to work upon as a part of the National Clinical Registries.Citation8 Immediate detection of particular trends in the treatment of OHCA has been made possible. In collaboration with a wide range of bodies, the national steering committee of the DCAR together with the Danish National Clinical Registries has attempted to make the DCAR more resilient and more comparable to other national registers in Europe and the world. In 2019, a study from the International Liaison Committee on Resuscitation (ILCOR) showed that in comparison with other national registries on OHCA, the DCAR does not quite live up to the Utstein Guidelines for registration of OHCACitation9 and the international development in the treatment of OHCA. In the paper, ILCOR pointed out that especially the treatment as well as the rehabilitation in the hospitals was needed as a part of the registry. Also, variables on AEDs and registering the specifics of the resuscitative effort need to be improved.
Figure 3 The section of the tablet used in the ambulances for entering data to the Danish Cardiac Arrest Registry in 2020.
The Danish Cardiac Arrest Register records a set of descriptive and quality of care variables according to international standards. This is a description of these variables and the indicators as they are at the time of writing as well as the intentions from the steering committee of the register to increase the quality on the hospital treatment of the patients.
Method Section
Setting
Denmark has a population of 5.8 million inhabitants (Statistics Denmark, Q4 – 2018). The geographical area of Denmark is 42.933 square kilometers. Healthcare is provided by The Danish National Health Service as a tax-supported public service. Redistributionist taxation finances approx. 85% of overall health care costs, including access to general practitioners (GPs), EMS, hospitals, outpatient specialty clinics, and partial reimbursement of prescribed medications. Acute disease and emergencies are also covered by the National Health Services. Therefore, EMS, as well as hospitalization, is without immediate cost for the person involved.Citation10
In Denmark, every resident is assigned a personal identification number in The Danish Civil Registration System.Citation11 This nationwide registry of administrative information was established on April 2, 1968. It assigns a unique ten-digit Civil Personal Register Number (CPR-number) to all persons residing in Denmark.Citation11 This number is used for identification and registration in public and private services. Having this system allows for exact individual-level record linkage of all Danish registries facilitating research.Citation12 For patients without Danish citizenship, a temporary CPR-number will be assigned upon contact with the public health care system.
Data Collection
Inclusion in the DCAR takes place if a patient for a cardiac arrest outside of the hospitals receives CPR or is defibrillated by bystander or EMS personnel.Citation9,Citation13 Data is collected from the section on the electronic tablet used by EMS personnel to collect daily medical records in their everyday work. See .
The inclusion and coverage of cardiac arrest cases are regarded as high because the EMS system is activated for all emergencies concerning cardiac arrest. Exclusion criteria are cases with late signs of death (decomposition, rigor mortis or livor mortis) or lesions incompatible with sustained life or if the patients did not have a cardiac arrest but had another reason to be unconscious such as suffering from a drug overdose, a stroke, or where resuscitative efforts are obviously futile from the onset. Since the implementation of the Cardiac Arrest Registry in 2001, EMS personnel have been required to complete a short case report paper form for the Danish Cardiac Arrest Register in every out-of-hospital cardiac. The paper registrations were collected and manually entered the registry. In 2015, an electronic medical record was introduced nationally in all ambulances and medical critical care units.Citation10 Data were to be registered on an electronic tablet with internet connection, whenever an OHCA was treated by EMS personnel. Through the year 2016, the short paper-based form was gradually abandoned. Data is now recorded in immediate connection to the OHCA and acts as a documentation of the treatment and outcome. Data on long-term survival (30-days) is collected from the Civil Personal Register and linked to the DCAR via the CPR-number.Citation11
Ethics Statement
Retrospective registry research does not require ethical approval by Danish law. The Danish Cardiac Arrest Registry is a part of the National Registries (with health records) collected and administered under the legislation of the Danish Health law. In this, the legislation sanctions the collection of health data on every person, who has been treated with the diseases described, without obtaining informed consent (85 different areas of disease are currently described). These data must be used for the development of quality indicators formed in a national consensus format and exposed to every professional who has reported patients to the register.
Variables
The variables included in the register have been adjusted in accordance with other registries such as UtsteinCitation14 and Cardiac Arrest Registry to Enhance SurvivalCitation15(CARES). The variables are further defined in alignment with the Utstein criteria on OHCA and have been continuously modified accordingly to the Utstein criteria over the years. See for the present variables.
Table 1 Variables in the Danish Cardiac Arrest Registry
The tabulation in the electronic medical record used from 2015 and onwards contains the same variables in the same order to accommodate recognition and ease when filling it in. Variables contain information on the identification number of the prehospital response unit (ambulance, Mobile Critical Care Unit, physician-manned Helicopter), CPR-number, the hospital to which the patient is subsequently referred, the location of the incident, time, whether the arrest was witnessed by laymen or EMS, any treatment given before the arrival of EMS personnel, involvement of a physician in prehospital treatment, the observations made by and treatment given by the EMS staff, and finally, the condition of the patient upon arrival to the hospital (see for more detailed information). All fields are required to be filled in with the option “No” if the question asked is irrelevant to the patient’s treatment.
Indicators
In , the indicators presently describing and measuring the entire process of events in the treatment of an OHCA are shown. There are indicators to measure the survival of patients to the hospital and 30-days survival in certain categories. Moreover, there is also an indicator for ambulance time to arrive at the scene (median time). Documentation of variables and indicators in the register can be found at https://www.rkkp-dokumentation.dk/ where new and old versions of the register are held.
Table 2 The Indicators in the Danish Cardiac Arrest Registry
In the future, the steering committee of the registry intends to increase the number of variables in several areas. The suggested new indicators are shown in .
Table 3 New Indicators and Variables Suggested for the Danish Cardiac Arrest Registry
At present, the data for the DCAR is supplied for central analysis once every year where a yearly report is made to illustrate the treatment and outcomes of the past year (WWW.OHCA.DK). The goal of the national steering committee is to have data available every month for quality assessment and outcome measures.
Discussion
In 2001–2020 a total of 57,000 patients with OHCA have been included in the register. These data have proven to be useful not only in benchmarking daily activity but also when evaluating the outcome of local or national projects in OHCA treatment. The register steering committee aims to implement further indicators on the treatment and thereby the outcome of OHCA by increasing the number of indicators in the next coming years.
Other registries have undergone the development from paper to electronic records similar to the DCAR has with the same successCitation16,Citation17 In 2016 the validation of data became more substantial and additional variables were added. Survival after 30 days has increased throughout the years along with the rising incidence of OHCA, and in 2018, the 30-day survival following OHCA was 16%. The core findings of the register in 2018 are a substantial yearly increase in bystander CPR to 77%, an increase in the use of AED before ambulance arrival to 9.3%, and an increase in survival (ROSC on arrival to hospital) to 24%. In the selected group of patients, the Utstein population, patients with witnessed cardiac arrest with a shockable rhythm, survival increased from 12.5% in 2001 to 62% in 2018. In the early years of the registry, the average age of the patients was 69 years but as the inclusion of cases rose, the age has stabilized at 72 years.Citation1,Citation8,Citation18 During the years 2001–2018, the 30-day survival has increased (). However, there is a non-significant decrease in both 30-day survival and immediate survival in the years 2017 and 2018, probably reflecting a change in registration practice following the transition to an electronic medical record.Citation1
The completeness of the register is high, as the incidence of OHCA was 93 per 100,000 inhabitants in 2018. A comparison was made in a European collaboration, the EURECA study, where the Danish incidences were among the highest.Citation19 The registry has been used in numerous publications and are highly active (see Appendix 1 Publications made with data from the DCAR in 2021).
Strengths and Limitations
A key strength of the registry is the complete national coverage of all people treated for OHCA in Denmark. This allows for calculations representative of national epidemiological measures and benchmarks. Another strength is the Danish Civil Personal Registration System, where all citizens are identified. Thus, it is possible to have an almost complete follow-up. The latest data from the DCAR comprise the years 2001 through 2018, covering a period when the registration has been transferred from paper-based case record forms to electronic registration. The centralized education of the validators, the possibility to draw data out of the entire medical record uniformly and the use of electronic medical records enables an even more thorough validation of data than the paper form did. Thus, data from 2016 and forward are therefore not necessarily immediately comparable to the previous years. In the new electronic medical records, several new variables can be used to widen the perspective of the registry. Among these new variables are medication administered, time spent at the scene, or the number of shocks delivered during resuscitation.
A limitation to the registry is the measurement of data completeness. There are many public registries but none of these describe the area of EMS or OHCA. Over the years, we have experienced an increase in the number of reported OHCAs without a markedly effect on the indicators. This could indicate underreporting in the initial years. The inclusion criteria for registering an OHCA in the DCAR, namely OHCA with either non-professional or professional resuscitation attempts, may further influence the number of registered OHCAs in Denmark. The increased willingness from the general population to initiate CPR on any person who falls unconscious onto the ground has probably changed the number of patients included in the registry.
A Registry Steering Committee is assigned to the registry by the five regional EMS’, the national scientific societies, and other stakeholders. The major role of the committee is to assure national consensus on the quality measures for the treatment and outcome of OHCA, to assure a proper framework for the register, to oversee the process of data collection, to develop the means of quality improvement, and to approve research projects that require the use of data from the registry.
Data from the DCAR are available upon reasonable request. More can be learned by entering this website: WWW.OHCA.DK. Here, all the links to the steering committee to request the relevant data can be found. To ascertain data from the registry, a detailed protocol for the proposed study and supplemental information about the funding and the scientific resources available to conduct the study should be forwarded.
Most of the external funding required for the DCAR has been provided by The TrygFoundation. Grants are provided to maintain, develop and report national data, to support data processing, as well as to financing associated Ph.D. students. In addition, the TrygFoundation supports the dissemination of the annual report and its results in connection to the publication. The TrygFoundation is a Danish non-profit private foundation with core areas that include safety, health, and well-being.
Conclusion
The Danish cardiac arrest registry has been used to work with the quality of the resuscitative effort performed prehospitally, or outside of the hospitals, for 20 years. Between 2001 and 2021, the number of bystanders who have performed CPR in OHCA before the arrival of the ambulance has tripled. Coincidentally, the overall survival has tripled. The registry has recently been accepted as a national clinical registry within the National Clinical Registries, and through this collaboration, further improvements will be sought by the national steering committee in the coming years.
Disclosure
Professor Christian Torp-Pedersen reports grants from Bayer, grants from Novo Nordisk, outside the submitted work.
The Copenhagen Emergency Medical Services have received unrestricted grants from the Laerdal Foundation. The TrygFoundation has supported a large number of projects, where several of the authors have participated. None of these occurrences has influenced data collection, data processing, analysis, or interpretation of data.
The authors report no other conflicts of interest in this work.
Acknowledgments
A very special thanks to the Danish Cardiac Arrest Registry Group: Members of the collaborative group, Danish Cardiac Arrest Registry Group, are Gunhild Kjærgaard-Andersen, Louise Milling, René Arne Bergmann, Heinrich Dedenroth Larsen, Lars Borup, Theo Walther Jensen, Mathias Geldermann Holgersen, Stig Nikolaj Fasmer Blomberg, Julie Linding Bogh Kjerulff, Kristian Bundgaard Ringgren and Kenneth Lübcke. All members of the Danish Cardiac Arrest Registry validation group are affiliated to The Danish Clinical Quality Program, National Clinical Registries, Copenhagen, Denmark.
Special thanks to the ambulance staff and physicians in the emergency medical services in Denmark that have collected data for the Danish Cardiac Arrest Registry. The documentation is important and without it, the recorded monitoring of real improvements would not have been possible.
This work is supported by the TrygFoundation (TrygFonden), who has supported the Danish Cardiac Arrest Registry in the collection and analysis of 18 years of data.
References
- Ringreen KC, Schoenau L, Lipper F, et al. Yearly report for the Danish Cardiac Arrest Registry 2016–2018 [Årsrapport for Dansk Hjertestop Register 2016–2018]; August 16, 2018. Available from: https://hjertestopregister.dk/wp-content/uploads/2019/11/Dansk-Hjertestopregister-2018-2.pdf. Accessed March 9, 2022.
- Blomberg SN, Christensen HC, Lippert F, et al. Effect of machine learning on dispatcher recognition of out-of-hospital cardiac arrest during calls to emergency medical services: a randomized clinical trial. JAMA Netw Open. 2021;4(1):e2032320–e2032320. doi:10.1001/jamanetworkopen.2020.32320
- Karlsson L, Hansen CM, Wissenberg M, et al. Automated external defibrillator accessibility is crucial for bystander defibrillation and survival: a registry-based study. Resuscitation. 2019;136:30–37. doi:10.1016/j.resuscitation.2019.01.014
- Andelius L, Malta Hansen C, Lippert FK, et al. Smartphone activation of citizen responders to facilitate defibrillation in out-of-hospital cardiac arrest. J Am Coll Cardiol. 2020;76(1):43–53. doi:10.1016/j.jacc.2020.04.073
- Viereck S, Møller TP, Ersbøll AK, et al. Recognising out-of-hospital cardiac arrest during emergency calls increases bystander cardiopulmonary resuscitation and survival. Resuscitation. 2017;115:141–147. doi:10.1016/j.resuscitation.2017.04.006
- Blomberg SN, Folke F, Ersbøll AK, et al. Machine learning as a supportive tool to recognize cardiac arrest in emergency calls. Resuscitation. 2019;138:322–329. doi:10.1016/j.resuscitation.2019.01.015
- Gram KH, Præst M, Laulund O, Mikkelsen S. Assessment of a quality improvement programme to improve telephone dispatchers’ accuracy in identifying out-of-hospital cardiac arrest. Resuscitation Plus. 2021;6:100096. doi:10.1016/j.resplu.2021.100096
- Ringreen KC, Schoenau L, Lippert F, et al. Yearly report on the Danish Cardiac Arrest Registry [årsrapport for Dansk Hjertestop Register] (2020); October 16, 2021. Available from: https://hjertestopregister.dk/wp-content/uploads/2022/01/Dansk-Hjertestopregister-aarsrapport-2020_opdateret-jan21.pdf. Accessed March 11, 2022.
- Kiguchi T, Okubo M, Nishiyama C, et al. Out-of-hospital cardiac arrest across the World: first report from the International Liaison Committee on Resuscitation (ILCOR). Resuscitation. 2020;152:39–49. doi:10.1016/j.resuscitation.2020.02.044
- Lindskou TA, Mikkelsen S, Christensen EF, et al. The Danish prehospital emergency healthcare system and research possibilities. Scand J Trauma Resusc Emerg Med. 2019;27(1):100. doi:10.1186/s13049-019-0676-5
- Schmidt M, Pedersen L, Sørensen HT. The Danish civil registration system as a tool in epidemiology. Eur J Epidemiol. 2014;29(8):541–549. doi:10.1007/s10654-014-9930-3
- Frank L. When an entire country is a cohort. Science. 2000;287(5462):2398–2399. doi:10.1126/science.287.5462.2398
- Akahane M, Tanabe S, Ogawa T, et al. Characteristics and outcomes of pediatric out-of-hospital cardiac arrest by scholastic age category. Pediatr Crit Care Med. 2013;14(2):130–136. doi:10.1097/PCC.0b013e31827129b3
- Eisenberg MSL, Castren M, Moor F, et al. Acting on the Call. 2018 update from the global resuscitation alliance – report; April, 2018. Available from: https://www.globalresuscitationalliance.org/wp-content/pdf/acting_on_the_call.pdf. Accessed June, 2020.
- McNally B, Robb R, Mehta M, et al. Out-of-hospital cardiac arrest surveillance—cardiac arrest registry to enhance survival (CARES), United States, October 1, 2005–December 31, 2010. MMWR Morb Mortal Wkly Rep. 2011;60(8):1–19.
- Odone A, Buttigieg S, Ricciardi W, Azzopardi-Muscat N, Staines A. Public health digitalization in Europe: EUPHA vision, action and role in digital public health. Eur J Public Health. 2019;29(Supplement_3):28–35. doi:10.1093/eurpub/ckz161
- Taber N, Mehmood A, Vedagiri P, Gupta S, Pinto R, Bachani AM. Paper versus digital data collection methods for road safety observations: comparative efficiency analysis of cost, timeliness, reliability, and results. J Med Internet Res. 2020;22(5):e17129. doi:10.2196/17129
- Ringreen KC, Schoenau L, Lippert F, et al. Yearly report for the Danish Cardiac Arrest Registry [Årsrapport for Dansk Hjertestop Register] (2019); October 16, 2020. Available from: https://hjertestopregister.dk/wp-content/uploads/2020/12/%C3%85rsrapport_Dansk_Hjertestopregister_2019.pdf. Accessed March 11, 2022.
- Gräsner J-T, Lefering R, Koster RW, et al. EuReCa ONE–27 Nations, ONE Europe, ONE Registry: a prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation. 2016;105:188–195. doi:10.1016/j.resuscitation.2016.06.004