Abstract
Aim
The study aimed to analyze the associations between estimated pulse wave velocity (ePWV) and 5-year mortality in atherosclerotic cardiovascular disease (ASCVD) patients with and without standard modifiable risk factors (SMuRFs), which included smoking status, hypertension, diabetes, and hypercholesterolemia.
Methods
The present retrospective cohort study utilized data from the National Health and Nutrition Examination Survey (NHANES) between 1999 and 2016. Patients with ASCVD who completed both the questionnaire survey and serum testing were included. Patients were categorized into the ≥1 SMuRF group if they had at least one SMuRF, while those without any SMuRFs were classified into the SMuRF-less group. The ePWV, which was calculated using the age and mean blood pressure, was evenly divided into three categories: low (Q1), medium (Q2), and high (Q3). Multivariable weighted Cox proportional-hazard regression analyses were utilized to explore the risk factors associated with 5-year mortality in patients with and without SMuRFs. And restricted cubic spline curve (RCS) was used to assess their nonlinear correlation.
Results
A total of 1901 patients with ASCVD were included in the study. For the patients in ≥1 SMuRF group, the Q3 group included patients who were older, with a higher proportion of males, more comorbidities, and a lower body mass index than the Q1 group (P<0.05). The Cox proportional-hazard regression model results revealed, the Q3 group had a higher risk of 5-year mortality than the Q1 group [hazard ratio (HR) 4.30, 95% confidence interval (CI) (2.66, 6.95), P<0.001]. RCS demonstrated a linear trend between high level of ePWV and decreased risks of mortality. Similar results were observed in the SMuRF-less group [HR 10.62, 95% CI (1.22, 92.06), P=0.032].
Conclusion
A high level of ePWV signified a higher risk of 5-year mortality in ASCVD patients with and without SMuRFs.
Introduction
Atherosclerotic cardiovascular disease (ASCVD) is caused by plaque buildup in arterial walls and refers to conditions that include coronary artery disease (CAD) and stroke, and it remains a leading cause of the global burden of morbidity and mortality.Citation1–3 The prevention and treatment of cardiovascular disease has always been in the spotlight. The Framingham Heart Study (FHS) first described four standard modifiable risk factors (SMuRFs), including smoking status, hypertension, diabetes, and hypercholesterolemia.Citation4 This milestone research has enhanced primary healthcare for patients with ASCVD, emphasizing the identification and management of SMuRFs as effective measures for improving prognosis.Citation5 In 2021, modifiable risk factors recommended by the European Society of Cardiology (ESC) in patients with ASCVD were defined as high nonHDL-cholesterol, high blood pressure, cigarette smoking, and diabetes. The systematic coronary risk estimation 2 (SCORE 2) and SCORE 2-older persons risk charts have been designed to assess the risk of fatal and non-fatal (myocardial infarction, stroke) cardiovascular disease, based on age, sex, nonHDL-cholesterol, blood pressure and smoking status.Citation6 Most cardiovascular disease cases and mortality can be attributable to these common SMuRFs globally.Citation7 However, even with stringent control of these factors, cardiovascular disease remains a leading cause of mortality worldwide.Citation8 This suggests that there may be potential risk factors that are currently unknown affecting the prognosis of cardiovascular diseases.
Recent studies have revealed a significant proportion of patients without any SMuRFs (SMuRF-less) in clinical practice.Citation9 The ASCVD patients with SMuRF-less have similar risk of future adverse cardiovascular events and mortality with those with ≥1 SMuRF.Citation10,Citation11 And many of them are not aware that their underlying coronary atherosclerosis had occurred until a heart attack occurs.Citation12 Although these patients are traditionally perceived as low-risk groups, face a worse prognosis with a higher mortality rate compared to those with at least one SMuRF (≥1 SMuRF), particularly in patients with CAD.Citation13 The increase in the number of ASCVD patients with SMuRFs-less and their high mortality may be attributed to the currently unidentified risk factors. It is urgent to find a new biomarker to effectively identify the prognosis of patients at high risk, providing an evidence-based foundation for subsequent treatment and prevention strategies.
Arteriosclerosis plays a crucial role in the occurrence and progression of ASCVD.Citation14 Early vascular aging is considered a significant contributor to arteriosclerosis and an independent predictor of future cardiovascular events in patients with ASCVD.Citation15,Citation16 Carotid-femoral pulse wave velocity (cfPWV), which is measured using specialized equipment, is the gold standard for assessing vascular stiffness and aging.Citation17 However, due to equipment and location limitations, estimated pulse wave velocity (ePWV) has emerged as a more cost-effective and readily available alternative for measuring vascular aging using age and mean arterial blood pressure (MAP) equations. The ePWV has been shown to have similar predictive value for arterial stiffness with that of cfPWV, making it a reasonable substitute.Citation18,Citation19 Previous studies have demonstrated that ePWV independently predicted cardiovascular events and all-cause mortality in individuals beyond the Framingham Risk Score.Citation20 Nevertheless, the associations between ePWV and mortality in ASCVD patients with and without SMuRF remains unclear, particularly in terms of the potential clinical predictive value in the relatively low-risk patients with ASCVD in SMuRFs-less.
Therefore, the present study aimed to investigate the relationship between ePWV and 5-year mortality in patients with ASCVD with or without SMuRFs using nationally representative data provided by the National Health and Nutrition Examination Survey (NHANES).
Methods
Data Source and Study Population
NHANES database is a population-based cross-sectional survey program carried out by the Centers for Disease Control and Prevention (CDC) and the National Center for Health Statistics (NCHS). Initiated in 1999 and conducted every 2 years, the program aims to assess the health and nutritional status of both adults and children in the United States. Through interview surveys, physical examinations, and laboratory tests, this study collects detailed demographic information and conducts long-term follow-ups. On the NHANES homepage, all the data were freely available and with unrestricted re-use permitted via an open license (http://www.cdc.gov/nchs/nhanes.htm). All NHANES protocols have received approval from the NCHS Ethics Committee (National Center for Health Statistics, 2012) and written informed consent has been obtained from all participants. This study was exempted from approval by the Institutional Review Board of 920th Hospital of Joint Logistics Support Force, PLA, as the use of deidentified and open access data does not constitute human subject research.
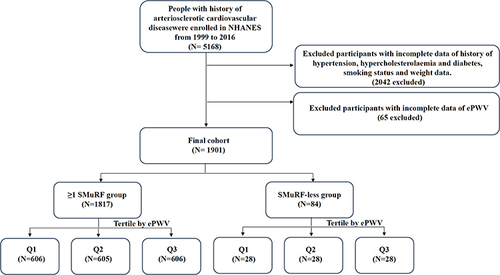
The present study collected population data between 1999 and 2016 from the NHANES. Patients with ASCVD were defined as individuals whose responses in the NHANES questionnaire indicated a “yes” to either of the following questions: “Has a doctor or other health professional ever told you that you had stroke?”, “Has a doctor or other health professional ever told you that you had a heart attack also called myocardial infarction?”, “Has a doctor or other health professional ever told you that you had coronary heart disease?” and “Has a doctor or other health professional ever told you that you had angina also called angina pectoris?”. This method of identifying patients with ASCVD has been adopted in previous studies.Citation21–24 The data for 5168 patients with ASCVD were analyzed in NHANES (). The analysis excluded 2042 patients with incomplete medical histories and 65 patients lacking ePWV records, ultimately including 1901 patients with ASCVD with complete data.
Definition of ≥1 SMuRF and SMuRF-Less
SMuRF refers to the presence of at least one of the following conditions: current smoking status (whose responses in the NHANES questionnaire indicated a “Every day”or ‘Some days’ to the questions: Do you now smoke cigarettes?), hypertension (having a previous diagnosis of hypertension, previous or ongoing antihypertensive pharmacotherapy?), diabetes (has a doctor or other health professional ever told you that you had diabetes?), and hypercholesterolemia (previous or ongoing oral low-density lipoprotein cholesterol (LDL-C)-lowering treatment, LDL-C concentration of ≥3.5 mmol/L, or total cholesterol concentration of ≥5.5 mmol/L).Citation13 SMuRF-less was defined as the absence of any of these SMuRFs.
Calculation of ePWV
The ePWV was calculated based on the patient’s age and mean blood pressure (MBP) using the following equation:Citation18
In the NHANES, each participant’s systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured three times, and the mean of these three measurements was used to calculate the final SBP and DBP values. MBP was then calculated as DBP+0.4 (SBP-DBP).Citation25 The collected ePWV values were divided into three equal categories and categorized as low (Q1), medium (Q2), and high (Q3).
The Collection of Survival Data
The NCHS has linked data collected from several NCHS population surveys with death certificate records from the National Death Index (NDI). We used the International Classification of Diseases 10th Revision to determine the all causes mortality (010).Citation26 The definition of all-cause mortality included all kinds of deaths which derived from NDI data (coding by International Classification of Diseases). Our study’s primary endpoint was 5-year all-cause mortality. The 5-year mortality information from the NHANES updated until 2021. Thus, patients with ASCVD enrolled after 2016 were excluded due to lack of 5-year mortality information.
Assessment of Covariates
In the population data obtained from NHANES between 1999 and 2016, baseline information collected from family interviews and physical examinations included age, sex (male/female), race (non-hispanic white/other), smoking status (no, former, current), body mass index (BMI; calculated as weight divided by height), and blood pressure. Medical history data obtained from questionnaire surveys included status information for hypertension (yes or no), diabetes mellitus (yes or no), hypercholesterolemia (yes or no), congestive heart failure (yes or no), stroke (yes or no), cancer (yes or no), and chronic obstructive pulmonary disease (COPD) (yes or no). Please refer to the NHANES Laboratory Testing Manual (http://www.cdc.gov/nchs/nhanes.htm) for detailed guidelines and methods related to the applicable laboratory data. The collected laboratory examination data included levels of total cholesterol (TC), LDL-C, high-density lipoprotein-cholesterol (HDL-C), white blood cells (WBCs), and C-reactive protein (CRP). These covariates were selected because they were considered clinically relevant as confounders in the association between cardiovascular and metabolic outcomes.
Statistical Analysis
Statistical analyses in the present study were performed using IBM SPSS Statistics (v26.0; IBM, Armonk, NY) and R (Version 4.3.0) software packages. All statistical procedures were conducted following the guidelines outlined by the CDC. Due to the complex, stratified, multi-stage sampling design of NHANES, appropriate sample weights were applied based on the NCHS analysis guidelines. This ensured that the samples was nationally representative. Weighted samples reflected the characteristics of the US population, while unweighted samples showed the characteristics of the registered population. Continuous variables with a normal distribution were presented as the mean [standard deviation (SD)], while those without a normal distribution were described as the median [interquartile range (IQR)]. Weighted Student’s t-test, weighted Wilcoxon rank sum test, and weighted chi-square test were used to evaluate baseline and ePWV characteristics at different levels. Univariable and multivariable weighted Cox proportional-hazard regression analyses were utilized to explore the associations between ePWV and five-year mortality in patients with ASCVD in the ≥1 SMuRF and SMuRF-less groups. Weighted Kaplan-Meier analysis was used to examine the difference in 5-year mortality among patients in the ≥1 SMuRF and SMuRF-less groups across various levels of ePWV. Weighted Cox proportional hazards regression models with restricted cubic splines and smooth curve fitting (penalized spline method) were conducted to explore association between ePWV and all-cause mortality in patients in the ≥1 SMuRF and SMuRF-less groups. If the relationship was nonlinear, we estimate the threshold value by trying all possible values and choosing the threshold point with the highest likelihood. All tests were two-tailed, and P < 0.05 was considered statistically significant.
Results
Baseline Characteristics
The flow chart for inclusion and exclusion criteria was shown in . A total of 1901 patients with ASCVD with complete data from NHANES were analyzed in the present study, including 1817 patients with ≥1 SMuRF and 84 patients with SMuRF-less. showed the characteristics of the total ASCVD population included in the study. The mean age of these patients was 66.75±12.61 years, and most of them were male (58.1%) and non-hispanic white (58.3%). The mean value of BMI was 29.76±6.64kg/m2, and the mean value of ePWV was 10.55±2.19. After assigning statistical weights, the total number of patients with ASCVD in the US was 16,583,797, including 15,811,897 patients with ≥1 SMuRF and 771,900 patients with SMuRF-less (Supplementary Table 1).
Table 1 Characteristics of the Study Patients
Clinical Characteristics of Patients with ASCVD in ≥1 SMuRF and SMuRF-Less Groups at Different ePWV Levels
showed the clinical characteristics of patients with ASCVD who were divided into three equal groups based on their ePWV levels in the ≥1 SMuRF and SMuRF-less groups. Our results showed that in the ≥1 SMuRF group, compared with the low ePWV (Q1) group, the high ePWV (Q3) group were older (78.11±4.92 vs 54.57±9.88, P<0.001) and had a higher proportion of male (58.3% vs 52.8%, P=0.001), higher percentage of non-Hispanic white individuals (70.1% vs 49.5%, P<0.01), lower BMI values (27.94±5.21 vs 31.18±7.58, P<0.01), higher HDL-C levels (1.36±0.43 vs 1.25±0.40, P<0.01), and higher percentage of those with cancer history (29.5% vs 12.1%, P<0.001). In addition, in the SMuRF-less group, the Q3 group was older (80.25±4.42 vs 38.36±10.38, P<0.001) and had a higher proportion of male (78.6% vs 28.6%, P<0.001), higher percentage of non-Hispanic white individuals (82.1% vs 50%, P=0.025), lower BMI values (24.58±4.59 vs 27.55±4.90, P=0.003), and higher percentage of those with COPD history (17.9% vs 0%, P=0.023) than the Q1 group. There was no statistically significant difference in other parameters across these groups (P>0.05). Similar results were still observed in the weighted data analysis (Supplementary Table 2).
Table 2 The Associations Between ePWV and Characteristics of the Study Patients in the ≥1 SMuRF and SMuRF-Less Cohort
The Associations Between ePWV and 5-Year Mortality in Patients with ASCVD in ≥1 SMuRF and SMuRF-Less Groups
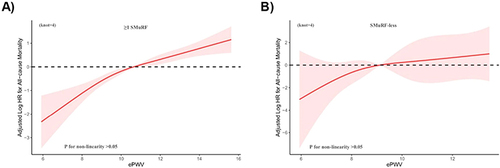
In the restricted cubic spline model, a linear trend was observed between higher ePWV and increased risks of all-cause mortality among patients with ASCVD in ≥1 SMuRF () and SMuRF-less groups (). It revealed that higher levels of ePWV was associated with an increased risk of 5-year mortality among patients with ASCVD both in ≥1 SMuRF and SMuRF-less groups.
Figure 2 Association between ePWV and 5-year all-cause mortality in ASCVD patients with ≥1 SMuRF (A) and SMuRF-less (B). The solid line and red area represent the estimated values and their corresponding 95% CIs, respectively. (ePWV, estimated Pulse Wave Velocity; SMuRFs, Standard modifiable risk factors).
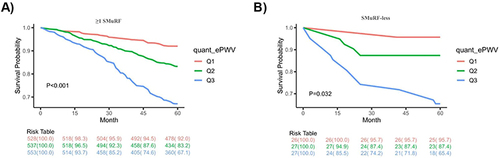
Kaplan-Meier analysis revealed significant differences in the 5-year mortality between the Q3 and Q1 group among patients with ASCVD in the ≥1 SMuRF group (P<0.001; ). It revealed a decreasing trend in 5-year all-cause mortality among patients with ASCVD with an increase in ePWV. Similar results were observed in patients with ASCVD in the SMuRF-Less group (P=0.032; ).
Figure 3 In the ≥1 SMuRF (A) and SMuRF-less groups (B), the 5-year all-cause mortality for different groups based on the level of ePWV. (ePWV, estimated Pulse Wave Velocity; SMuRFs, Standard modifiable risk factors).
In ASCVD patients with ≥1 SMuRF, univariable Cox proportional-hazard regression analysis (Crude model) revealed that higher level of ePWV (hazard ratio (HR) 1.38, 95% confidence interval (CI) 1.29–1.47, P<0.001) were associated with the 5-year mortality. The Q3 group exhibited a significantly higher five-year mortality risk than the Q1 group (P<0.001). After adjusting for race and BMI (Model 1), the Q3 group had a higher five-year all-cause mortality risk than the Q1 group (P<0.001). After adjusting for race, BMI, congestive heart failure, stroke and cancer (Model 2), the Q3 group still showed a significantly higher five-year mortality risk than the Q1 group (P<0.001) ().
Table 3 Unadjusted and Adjusted Cox Proportional Regression Model of ePWV with 5-Year Mortality in the Patients with ≥1 SMuRF and SMuRF-Less
In ASCVD patients with SMuRF-less, univariable Cox proportional-hazard regression analysis (Crude model) indicated that higher level of ePWV (HR 1.44, 95% CI 1.16–1.80, P=0.001) were associated with the five-year mortality. The Q3 group had a significantly higher five-year mortality risk than the Q1 group (P=0.028). After adjusting for race and BMI (Model 1), the Q3 group had a higher five-year all-cause mortality risk than the Q1 group (P=0.032). Even after adjusting for race, BMI, congestive heart failure, stroke and cancer (Model 2), the Q3 group continued to exhibit a higher 5-year mortality risk than the Q1 group (P=0.032) ().
Discussion
In the present study, ePWV was independently associated with 5-year all-cause mortality in patients with ASCVD regardless of the presence of SMuRFs. Moreover, the 5-year all-cause mortality increased as the ePWV level increased. Our findings had important clinical significance because they described a convenient, practical, and superior index for assessing arterial stiffness. The higher ePWV level still signified a poorer 5-year all-cause mortality, particularly for patients with ASCVD in the SMuRF-less group who were traditionally considered to be at low risk. Such patients required a similar level of attention in clinical practice in order take the necessary secondary prevention measures.
With the advancements in modern medical technology, a considerable number of patients with early-stage ASCVD have been detected. Based on the modifiable risk factors of ASCVD (smoking status, hypertension, diabetes, and hypercholesterolemia), the risk charts have been developed for the early prevention and future risk assessment of ASCVD, including the Framingham General Cardiovascular Risk Score (FGCRS) in the United States, the SCORE 2 in Europe and China’s Prediction for ASCVD Risk model (China-PAR), etc.Citation27 They all indicated that the presence of more SMuRFs in patients with ASCVD indicated a higher health risk in the future. However, there was a lack of effective methods for predicting future cardiovascular risk in individuals without SMuRF. A study based on 14 international randomized clinical trials of coronary heart disease (CHD) revealed that around 90% of patients with CHD had at least one SMuRF,Citation5 which was broadly consistent with the present research findings (95.6%). However, recent research has identified an increasing trend in the proportion of SMuRF-less patients with CAD in recent years, which can possibly be attributed to the advancements in medical care and heightened public health awareness.Citation9 Our results showed that older male were more likely to have a high level of ePWV, particularly among those with SMuRF-less. It indicated that older male may have a higher cardiovascular risk in future even without any traditional risk factors. This was consistent with the results of a community survey in China.Citation28
Arteriosclerosis causes irreversible cardiovascular damage over time and has risk factors similar to ASCVD.Citation29 Increased arterial stiffness has been shown to predict future cardiovascular events and improve cardiovascular risk stratification.Citation30 Previous studies have found that SMuRF-less patients with CAD had a similar progression of coronary artery calcification and a higher incidence of major adverse cardiovascular events (MACEs) and mortality than those with ≥1 SMuRF.Citation31,Citation32 Therefore, the traditional risk assessment methods for ASCVD may miss the diagnosis of high risk patients. Several previous studies recommend incorporating ePWV as a noninvasive biomarker to assess atherosclerosis into existing cardiovascular risk prediction models in order to enhance their accuracy.Citation18,Citation33,Citation34 The present study found that ePWV was an independent predictor of all-cause mortality over the course of 5 years in ASCVD patients with ≥1 SMuRF and SMuRF-less. These findings were consistent with those described in the study by Chen et al, which included patients with CAD.Citation35 The present study was also in line with the findings described in the study by Laugesen et al, which analyzed patients with stable angina undergoing elective coronary angiography.Citation36 These researches suggested that high levels of ePWV were associated with a poorer prognosis. Our study further confirmed the importance of ePWV in detecting prognosis of cardiovascular disease. However, our study focused more on patients with SMuRF-less at a relatively lower-risk, and aimed to identify potential indicators beyond SMuRFs used to predict mortality of patients with SMuRF-less. Measure should be taken towards identifying individuals at increased cardiovascular risk in the asymptomatic subclinical stages to prevent the progression of disease.Citation37 The present study revealed that an elevated level of ePWV had higher risk of the 5-year all-cause mortality in ASCVD patients with SMuRFs-less, similar results were observed in ASCVD patients with ≥1 SMuRF. Therefore, even in the absence of traditional risk factors, ePWV can be used to assess risk stratification in ASCVD patients in clinical practice. This provides an efficient and convenient means of risk assessment for individual patients, clinicians, healthcare policy makers, and society to reduce the future burden of cardiovascular disease.
Despite its significant findings, there were still some limitations in the present study. First, the analysis results only suggested an association between ePWV and the overall mortality rate in patients with ASCVD with or without SMuRFs. Further prospective data are needed to validate this causal relationship. Second, the present study was designed to assess fatal events. Therefore, the effect of ePWV on non-fatal MACEs and other prognostic events was not examined. Third, Atherosclerosis was an inflammatory disease of blood vessels, and although our study compared the difference of CRP at different ePWV levels, the high sensitivity CRP seems to be a more effective predictor of pathological PWV values.Citation38 Fourth, the present study data were derived from the NHANES database of American adults. Whether the study results are applicable to other populations with different economic and geographic characteristics requires further research to evaluate. Finally, despite the adjustment for relevant confounding factors, the possibility of unadjusted potential confounders that might be correlated remains. For example, lifestyle (sedentary lifestyle, physical activity, diet, pressure), social background, family history, noise pollution and chronic kidney disease have all been reported to be associated with the development of atherosclerosis.Citation39,Citation40 Therefore, studies with larger sample sizes and more variables are necessary for further research to establish the relationship between ePWV and all-cause mortality in patients with ASCVD with or without SMuRFs.
Conclusion
In conclusion, elevated level of ePWV predicted a higher 5-year all-cause mortality in patients with ASCVD regardless of the presence of SMuRFs. Patients with SMuRF-less, who were at a relatively low risk in the current prognostic risk stratification of ASCVD, should be carefully monitored for their ePWV levels. It can identify the population at high risk early and utilize necessary treatment strategies to improve their prognosis.
Abbreviations
ePWV, estimated Pulse Wave Velocity; ASCVD, Atherosclerotic cardiovascular disease; SMuRFs, Standard modifiable risk factors; MBP, Mean blood pressure; HR, Hazard ratio; CI, Confidence interval; RCS, restricted cubic spline curve.
Ethics Approval and Consent to Participate
All NHANES protocols have received approval from the NCHS Ethics Committee (National Center for Health Statistics, 2012) and written informed consent has been obtained from all participants. This study was exempted from approval by the Institutional Review Board of 920th Hospital of Joint Logistics Support Force, PLA, as the use of deidentified and open access data does not constitute human subjects research.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
Data Sharing Statement
The datasets used and analyzed in the current study are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Aboyans V; Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2015;385(9963):117–171. doi:10.1016/s0140-6736(14)61682-2
- Kim AS, Johnston SC. Global variation in the relative burden of stroke and ischemic heart disease. Circulation. 2011;124(3):314–323. doi:10.1161/circulationaha.111.018820
- Barquera S, Pedroza-Tobías A, Medina C, et al. Global overview of the epidemiology of atherosclerotic cardiovascular disease. Arch Med Res. 2015;46(5):328–338. doi:10.1016/j.arcmed.2015.06.006
- Wilson PW, Rb D, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837–1847. doi:10.1161/01.cir.97.18.1837
- Khot UN, Khot MB, Bajzer CT, et al. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA. 2003;290(7):898–904. doi:10.1001/jama.290.7.898
- Visseren FLJ, Mach F, Smulders YM, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42(34):3227–3337. doi:10.1093/eurheartj/ehab484
- Yusuf S, Joseph P, Rangarajan S, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. 2020;395(10226):795–808. doi:10.1016/s0140-6736(19)32008-2
- Roth GA, Mensah GA, Johnson CO, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76(25):2982–3021. doi:10.1016/j.jacc.2020.11.010
- Figtree GA, Vernon ST. Coronary artery disease patients without standard modifiable risk factors (SMuRFs)- a forgotten group calling out for new discoveries. Cardiovasc Res. 2021;117(6):e76–e78. doi:10.1093/cvr/cvab145
- Escudero-Sánchez G, Rico-Martín S, Sánchez-Bacaicoa C, et al. Optimal control of all modifiable vascular risk factors among patients with atherosclerotic disease. A real-life study. Curr Probl Cardiol. 2023;48(3):101530. doi:10.1016/j.cpcardiol.2022.101530
- Mahtta D, Khalid U, Misra A, Samad Z, Nasir K, Virani SS. Premature atherosclerotic cardiovascular disease: what have we learned recently? Curr Atheroscler Rep. 2020;22(9):44. doi:10.1007/s11883-020-00862-8
- Vikulova DN, Grubisic M, Zhao Y, et al. Premature atherosclerotic cardiovascular disease: trends in incidence, risk factors, and sex-related differences, 2000 to 2016. J Am Heart Assoc. 2019;8(14):e012178. doi:10.1161/jaha.119.012178
- Figtree GA, Vernon ST, Hadziosmanovic N, et al. Mortality in STEMI patients without standard modifiable risk factors: a sex-disaggregated analysis of SWEDEHEART registry data. Lancet. 2021;397(10279):1085–1094. doi:10.1016/s0140-6736(21)00272-5
- Park SM, Seo HS, Lim HE, et al. Assessment of arterial stiffness index as a clinical parameter for atherosclerotic coronary artery disease. Circ J. 2005;69(10):1218–1222. doi:10.1253/circj.69.1218
- Boutouyrie P, Bruno RM. The clinical significance and application of vascular stiffness measurements. Am J Hypertens. 2019;32(1):4–11. doi:10.1093/ajh/hpy145
- Lacolley P, Regnault V, Segers P, Laurent S. Vascular smooth muscle cells and arterial stiffening: relevance in development, aging, and disease. Physiol Rev. 2017;97(4):1555–1617. doi:10.1152/physrev.00003.2017
- Townsend RR, Wilkinson IB, Schiffrin EL, et al. Recommendations for improving and standardizing vascular research on arterial stiffness: a scientific statement from the American heart association. Hypertension. 2015;66(3):698–722. doi:10.1161/hyp.0000000000000033
- Greve SV, Blicher MK, Kruger R, et al. Estimated carotid-femoral pulse wave velocity has similar predictive value as measured carotid-femoral pulse wave velocity. J Hypertens. 2016;34(7):1279–1289. doi:10.1097/hjh.0000000000000935
- Hametner B, Wassertheurer S, Mayer CC, Danninger K, Binder RK, Weber T. Aortic pulse wave velocity predicts cardiovascular events and mortality in patients undergoing coronary angiography: a comparison of invasive measurements and noninvasive estimates. Hypertension. 2021;77(2):571–581. doi:10.1161/hypertensionaha.120.15336
- Vlachopoulos C, Terentes-Printzios D, Laurent S, et al. Association of estimated pulse wave velocity with survival: a secondary analysis of SPRINT. JAMA Network Open. 2019;2(10):e1912831. doi:10.1001/jamanetworkopen.2019.12831
- Skipina TM, Patel N, Upadhya B, Soliman EZ. Cannabis use is associated with prevalent coronary artery disease. Am J Med Sci. 2022;364(3):304–308. doi:10.1016/j.amjms.2022.04.005
- Sule S, Fontaine K. Coronary artery disease in adults with a history of juvenile arthritis. Arthritis Care Res. 2020;72(12):1790–1793. doi:10.1002/acr.24087
- Ding X, Wang X, Wu J, Zhang M, Cui M. Triglyceride-glucose index and the incidence of atherosclerotic cardiovascular diseases: a meta-analysis of cohort studies. Cardiovasc Diabetol. 2021;20(1):76. doi:10.1186/s12933-021-01268-9
- Liu C, Lai W, Zhao M, Zhang Y, Hu Y. Association between the composite dietary antioxidant index and atherosclerotic cardiovascular disease in postmenopausal women: a cross-sectional study of NHANES data, 2013–2018. Antioxidants. 2023;12(9):1740. doi:10.3390/antiox12091740
- Reference Values for Arterial Stiffness’ Collaboration. Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: ‘establishing normal and reference values’. Eur Heart J. 2010;31(19):2338–2350. doi:10.1093/eurheartj/ehq165
- Harris ST, Zeng X, Ford L. International classification of diseases, 10th Revision: it’s coming, ready or not. Health Care Manag. 2011;30(3):227–235. doi:10.1097/HCM.0b013e318225e0a2
- Yang X, Li J, Hu D, et al. Predicting the 10-year risks of atherosclerotic cardiovascular disease in Chinese Population: the China-PAR Project (Prediction for ASCVD Risk in China). Circulation. 2016;134(19):1430–1440. doi:10.1161/circulationaha.116.022367
- Yi T, Gao L, Fan F, et al. Association between pulse wave velocity and the 10-year risk of atherosclerotic cardiovascular disease in the Chinese population: a community-based study. J Clin Hypertens. 2023;25(3):278–285. doi:10.1111/jch.14642
- He XW, Park J, Huang WS, et al. Usefulness of estimated pulse wave velocity for identifying prevalent coronary heart disease: findings from a general Chinese population. BMC Cardiovasc Disord. 2022;22(1):9. doi:10.1186/s12872-022-02456-5
- Vlachopoulos C, Aznaouridis K, Mf O, Safar ME, Baou K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J. 2010;31(15):1865–1871. doi:10.1093/eurheartj/ehq024
- Mazhar J, Figtree G, Vernon ST, et al. Progression of coronary atherosclerosis in patients without standard modifiable risk factors. Am J Prev Cardiol. 2020;4:100116. doi:10.1016/j.ajpc.2020.100116
- Leipsic J, Taylor CM, Grunau G, et al. Cardiovascular risk among stable individuals suspected of having coronary artery disease with no modifiable risk factors: results from an international multicenter study of 5262 patients. Radiology. 2013;267(3):718–726. doi:10.1148/radiol.13121669
- Ben-Shlomo Y, Spears M, Boustred C, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol. 2014;63(7):636–646. doi:10.1016/j.jacc.2013.09.063
- Greve SV, Blicher MK, Kruger R, et al. Elevated estimated arterial age is associated with metabolic syndrome and low-grade inflammation. J Hypertens. 2016;34(12):2410–2417. doi:10.1097/hjh.0000000000001083
- Chen C, Bao W, Chen C, Chen L, Wang L, Gong H. Association between estimated pulse wave velocity and all-cause mortality in patients with coronary artery disease: a cohort study from NHANES 2005–2008. BMC Cardiovasc Disord. 2023;23(1):412. doi:10.1186/s12872-023-03435-0
- Laugesen E, Olesen KKW, Peters CD, et al. Estimated pulse wave velocity is associated with all-cause mortality during 8.5 years follow-up in patients undergoing elective coronary angiography. J Am Heart Assoc. 2022;11(10):e025173. doi:10.1161/jaha.121.025173
- Olsen MH, Angell SY, Asma S, et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on hypertension. Lancet. 2016;388(10060):2665–2712. doi:10.1016/s0140-6736(16)31134-5
- Mozos I, Jianu D, Gug C, Stoian D. Links between high-sensitivity c-reactive protein and pulse wave analysis in middle-aged patients with hypertension and high normal blood pressure. Dis Markers. 2019;2019:2568069. doi:10.1155/2019/2568069
- Climie RE, Alastruey J, Mayer CC, et al. Vascular ageing: moving from bench towards bedside. Eur J Prev Cardiol. 2023;30(11):1101–1117. doi:10.1093/eurjpc/zwad028
- Seeland U, Nemcsik J, Lønnebakken MT, et al. Sex and gender aspects in vascular ageing - focus on epidemiology, pathophysiology, and outcomes. Heart Lung Circ. 2021;30(11):1637–1646. doi:10.1016/j.hlc.2021.07.006