Abstract
Introduction
Ambulance requests by general practitioners for primary care patients (GP-requested) are often omitted in studies on increased demand within emergency care but may comprise a substantial patient group. We aimed to assess acute severity, intensive care unit (ICU) admission, and diagnostic pattern, including comorbidity, and mortality among GP-requested ambulance patients, compared to emergency call ambulance patients. Our hypothesis was that emergency call patients had more severe health issues than GP-requested ambulance patients.
Methods
Historic population-based cohort study of ambulance patients in the North Denmark Region, 2016–2020. Hospital contact data including diagnoses, ambulance data, vital signs and vital status was linked using each patient’s unique identification number. Primary outcome measure was mortality within 1, 7, and 30 days. Secondary outcomes were disease severity expressed as modified National Early Warning Score (NEWS2), and ICU admission. Admission status and hospital diagnostic pattern, including comorbidity were described and compared.
Results
We included 255,487 patients. GP-requested patients (N = 119,361, 46.7%) were older (median years [IQR] 73 [58–83] versus 61 [37–76]) and more had moderate/severe comorbidity (11.9%, N = 13,806 versus 4.9%, N = 6145) than the emergency call patients. Prehospital mNEWS2 median scores were lower for GP-requested patients. For both groups, mNEWS2 was highest among patients aged 66+. GP-requested patients had higher 30-day mortality (9.0% (95% CI: 8.8–9.2), N = 8996) than emergency call patients (5.2% (95% CI: 5.1–5.4), N = 6727). Circulatory (12.0%, 11,695/97,112) and respiratory diseases (11.6%, 11,219/97,112) were more frequent among GP-requested patients than emergency call patients ((10.7%, 12,640/118,102) and (5.8%, 6858/118,102)). The highest number of deaths was found for health issues ‘circulatory diseases’ in the emergency call group and ‘other factors’ followed by “respiratory diseases” in the GP-requested group.
Conclusion
GP-requested patients constituted nearly half of the EMS volume, they were older, with more comorbidity, had serious conditions with substantial acute severity, and a higher 30-day mortality than emergency call patients.
Introduction
The entire emergency medical care chain, both the prehospital emergency services (EMS) and the hospitals’ emergency departments (ED) face increasing numbers of patients. One of the main reasons are the changes in demography with more elderly and more living with chronic diseases and multimorbidity.Citation1–4
As a result, alternative solutions for optimizing the use of ambulances and reducing the number of hospitalized patients are explored. These include campaigns for when to call for an ambulance, non-conveyance of patients, community paramedics, subacute ambulatory/outpatient care etc.Citation5–9 The initiatives, often local and concerning a subset of patients, miss the larger picture of the effect on the entire acute EMS population.
In Europe and globally, access to an ED differs from direct access (Sweden), recommended contacting a general practitioner (GP) or out-of-hours GP prior (Netherlands), or requiring referral (Norway). For Denmark, access to hospital care is only possible through referral by either a GP, out-of-hours GP or the national emergency number 112 as triage prior to hospital attendance is mandatory. GPs take care of the less urgent situations during office hours, and out-of-hours GPs are intended for less urgent health problems that cannot wait until the patient’s own GP is available in normal office hours. The national emergency number is for potential life or limb threatening and other emergencies where urgent assistance is required.Citation10 If deemed necessary, ambulances are dispatched following a call to 112, but GPs may also request an ambulance at all hours. When referring to an increasing demand and number of emergency ambulances, ambulances requested by primary care (ie, GPs) are often left out. In countries with established primary care sectors such requests may contribute substantially to the number of ambulances needed.Citation10 In Denmark, patients do not always contact the emergency number for serious conditions but call the GP and the emergency number is contacted for non-urgent conditions as well.Citation11
The demand for and use of ambulances changes over time according to changes in demography and the disease pattern in the patient population. To give a complete picture, we must cover the entire patient population in the ambulances, including ambulances requested both from 112-calls, GPs, and others. The numerous patient registries in Denmark, as well as other Scandinavian countries, enable such studies.Citation12 To facilitate stable solutions, studies on a population-based level, elucidating the disease pattern of the entire group of ambulance patients, are needed.
We aimed to assess acute severity, ICU admission, and diagnostic pattern, among GP-requested ambulance patients, and mortality compared to emergency call ambulance patients.
Our hypothesis was that the emergency call patients have more severe health issues compared to the GP-requested patients.
Materials and Methods
Design
Historic population-based cohort study. Reporting was done following STROBE guidelines.Citation13
Setting
In Denmark, healthcare is tax-financed and thereby free of charge for all inhabitants. The country is divided into five regions, each responsible for the healthcare services within the region. The North Denmark region is a mixed rural-urban region with a population of 590,000 inhabitants, corresponding to 10% of the Danish population.Citation14 In the region, GPs (during office hours), out-of-hours GPs, and EMS (around the clock) are available for acute disease or injury. Access to hospital care is only possible through one of the three services as triage prior hospital attendance is mandatory. All patients with a hospital contact receive a diagnosis according to the International Classification of Diseases 10th Edition (ICD-10) and may receive multiple diagnoses during hospitalization.Citation15
Participants
Patients transported to a hospital by an ambulance following either a call to the national emergency number 112, emergency call patients, or a request from a GP (in and out-of-hours), GP-requested patients, during July 1st 2016 to December 31st 2020 in the North Denmark Region, were included.
We excluded patients with no valid Civil Registration Number (number not obtained due to acute situation, unconscious or dead patient, tourist, etc. or invalid format entered), patients with time of death before time of medical record creation or missing vital status, and those who were registered as dead upon hospital arrival: “R092 respiratory arrest”, “R96 sudden death”, “R98 unattended death”, and “R99 certain circumstances regarding death”.
Variables and Data Sources
Data concerning sex, age and date of death were retrieved from the Danish Civil Registration System.
Prehospital vital signs were retrieved from the prehospital electronic medical record.Citation10,Citation16 The patients’ first measured vital signs (heart rate, systolic blood pressure, SpO2, Glasgow coma scale and respiratory rate) were used to calculate the modified NEWS2 (mNEWS2) score (temperature excluded as this is rarely measured in the ambulances).Citation16 mNEWS2 was only calculated for patients older than 16 years.
Logistic data concerning dispatched ambulances were retrieved from the logistic system (LogisCAD).
Administrative information on hospital visits (admission, discharge dates, department and ICU admission) and in-hospital diagnoses according to the ICD-10 were retrieved from the regional patient administrative system.Citation15 The ICD-10 main chapters comprise cause-specific diagnoses that are organ- or pathology specific (such as Infections, Respiratory diseases, Injuries etc).Citation15 The patients’ initial primary diagnosis was reported. If a patient was registered as having received a non-specific diagnosis (ICD-10 main chapter 18 “symptoms and signs” or chapter 21 “other factors”), we investigated all diagnoses given during hospitalization. If the patient at any point received an organ- or pathology-specific diagnosis during their hospitalization, the later specific diagnosis was used instead of the initial non-specific diagnosis”.
Admissions to individual wards were linked into care episodes where there were less than 24 hours since last admission, provided another emergency episode did not take place between admissions.
Hospital contacts were determined to be associated with an emergency episode if the contact time was within six hours of the emergency dispatch.
Comorbidity was evaluated according to the Charlson Comorbidity Index score (CCI) for patients above 16 years and based on the past five years of hospital diagnoses only.Citation17 Comorbidity is categorized as none/missing if no diagnoses were found, mild if CCI score was 1–2, and moderate/severe if the score was 3 or more. All data sources were linked using the patients’ unique civil registration numbers.
Outcomes
Our primary outcome measure was mortality within 1, 7, and 30 days.
Secondary outcomes were disease severity expressed as modified National Early Warning Score (NEWS2), and ICU admission.Citation18 Furthermore, admission status and diagnoses given, including comorbidity, were described and compared.
Statistical Analysis
Data was pseudonymized prior to analysis.
Outcome rates were stratified by emergency call patients and GP-requested patients and calculated for subgroups.
Mortality within 1-, 7- and 30 days was estimated via Kaplan–Meier survival analysis. To address the possibility of a patient being registered as dead more than once, due to multiple contacts, patients were omitted from the mortality analysis, if they had a subsequent episode within the follow-up period. Mortality estimates are reported with 95% confidence intervals. Differences in survival functions were assessed using a Peto-weighted Log rank test. Differences in point estimates of survival were assessed using log-log transformed survival functions. Adjusted survival was estimated using a Cox Proportional Hazards model with age, sex, mNEWS2, CCI and 112-call status as covariates. Survival analysis was performed using the “lifelines” package.
The mortality analysis was further stratified by initial primary diagnosis and by age groups.
The mNEWS2 was calculated using the first measured vital signs in each patient’s prehospital medical record. If one or more vital signs were missing, mNEWS2 was calculated based on the vital signs available with the assumption that the missing data were normal, ie, not adding further to the calculated mNEWS2 score. eFigure 1 shows the proportion of missing values in relation to the mNEWS2 scores. This approach to missing values was used in previously published work.Citation19
Categorical data were described as n (%), and continuous data described as median [IQR]. Differences between categorical data were assessed using the chi-squared test. Differences between continuous data were assessed using the non-parametric Mann–Whitney U-test.
All analysis was done in Python version 3.10. Survival analysis used the lifelines package (version 0.27.8). Hypothesis tests used the implementations in the SciPy package (version 1.11.3).Citation20
Results
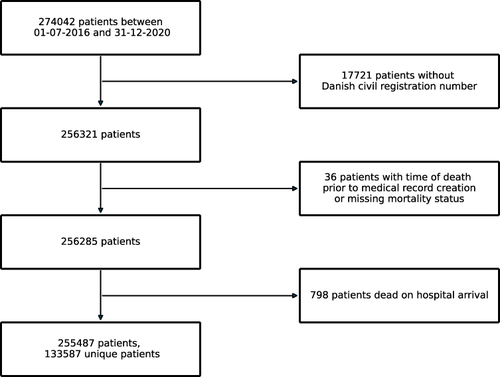
A total of 274,042 patients requested an ambulance in the study period. The exclusion criteria resulted in 255,487 included patients, consisting of 113,587 unique patients (). Of the 255,487 included patients, 136,126 (53.3%) were emergency call patients, and 119,361 (46.7%) were GP-requested patients. The total number of prehospital medical records created for each unique patient over the study period can be seen in eTable 1. Most patients received an ambulance after either calling 112 or the GP, and 24.9% of the population (33,237/133,587) received an ambulance calling both 112 and the GP (eTable 1). Most of the ambulance patients were brought to the hospital (84.2%, (215,214/255,487)) and thus had a diagnosis assigned.
Figure 1 Study inclusion flowchart of all ambulance patients between July 1st 2016 to December 31st 2020 in the North Denmark Region (N = 255487).
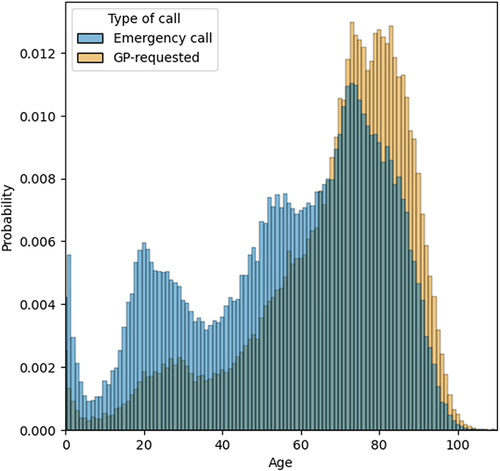
There were three age peaks at infant age, early twenties, and older age (). The GP-requested patients were older (median 73 years IQR [58–83]) than the emergency call patients (median 61 years IQR [37–76]) ().
Table 1 Demographics, Characteristics, and Outcome Rates for All Ambulance Patients (N = 255487)
Figure 2 Age distribution of all ambulance patients stratified by emergency call status (N = 255,487).
Overall, comorbidity was more prevalent among GP-requested patients compared to emergency call patients, as was moderate/severe comorbidity ().
Most patients 82.4% (N = 215,214/255,487) were brought to the emergency department as the first department, but less frequent for the GP-requested patients (72.4% (70,296/97,112) than for the emergency call patients (90.7% (107,118/118,102).
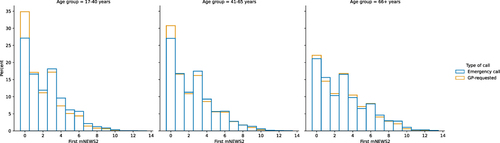
Disease severity based on the mNEWS2 score differed across age groups and by emergency call status. GP-requested patients had lower median mNEWS2 scores in all age groups compared to emergency call patients, with low scores most frequent among the younger patients. However, in patients aged 66 years and above, score distribution was more similar, the median score was higher and acute disease severity increased with age for both GP-requested and emergency call patients (eTable 2 and ). In less than 10% of the population, no vital signs were measured and a mNEWS2 score could not be calculated. Most patients had three or more vital signs measured (eFigure 1).
Figure 3 Distribution of mNEWS2 scores for all ambulance patients aged >16 years stratified by emergency call status (N = 220344).
For GP-requested patients, hospital length of stay was longer, with a median 2.2 days compared to 0.5 days for emergency call patients, whereas ICU admissions were more frequent among emergency call patients (). The distribution of first primary diagnoses at ICD-10-chapter level stratified by age and call-status is illustrated in eFigure 2 and eTable 3. The most frequent diagnoses assigned were within the two non-specific diagnostic chapters, “symptoms and signs”, “other factors”, and the chapter “injuries and poisoning”. Injuries were more frequent among the younger part of the population, and especially for the emergency call patients. The proportion of patients diagnosed within the ICD-10 main chapter “circulatory diseases”, generally increased with age in both groups. Patients diagnosed within chapter 10 “respiratory diseases”, were most prominent among the youngest and oldest, for both the GP-requested and emergency call patients. Overall, the proportions of non-causal diagnoses were higher among the emergency call patients, 44.8% (52,941/118,102), versus 35.8% (34,805/97,112) among GP-requested patients (eTable 3).
Mortality
The 30-day mortality among GP-requested patients was higher, when compared to emergency call patients, with 8996 (9.0%) and 6727 (5.2%) deaths, respectively (). Probability of survival was lower for GP-requested patients especially in the interval 7–30 days following the ambulance run. Mortality closer to the ambulance run (days 1–6) was higher for emergency call patients, especially 1-day mortality.
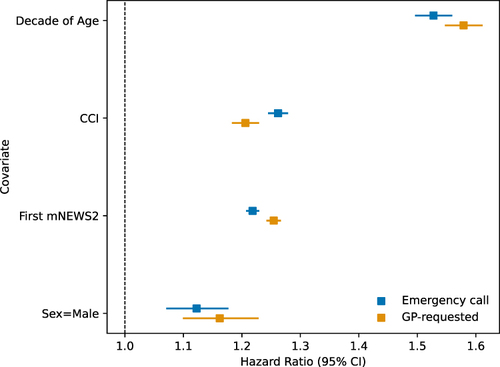
In the Cox proportional hazards model, the hazard ratios for age were 1.58 (1.55–1.61) for GP-requested and 1.53 (1.50–1.56) for emergency call patients. For comorbidity, it was 1.21 (1.18–1.23) and 1.26 (1.25–1.28), respectively, mNEWS2 score 1.25 (1.24–1.27) and 1.22 (1.21–1.23), and for male sex 1.16 (1.10–1.23) and 1.12 (1.07–1.18) ().
Figure 4 Plot of co-variate hazard ratios for the Cox Proportional Hazard model of mortality (N = 220,344).
For GP-requested patients, the two non-specific diagnosis chapters, “symptoms and signs” and “other factors”, as well as “diseases of the respiratory system” were associated with the highest number of deaths. Compared to emergency call patients, the number of deaths within these main diagnostic chapters was twice as high ().
Figure 5 Number of diagnoses, mortality and number of deaths stratified by emergency call status and first primary diagnosis, according to the International Classification of Diseases 10th Edition (ICD-10) for ambulance patients brought to hospital (N = 215214).
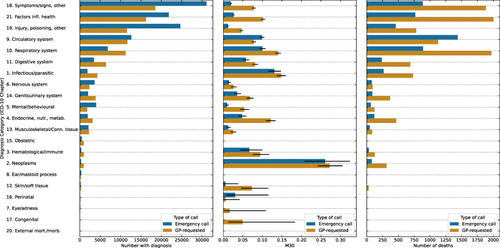
Deaths among patients diagnosed with “diseases of the circulatory system” were the most frequent group among the emergency call patients and more frequent than among GP-requested patients ().
Discussion
Key Results
Mortality was significantly higher for GP-requested patients by 7 to 30 days following the ambulance run, yet mortality closer to the ambulance run (days 1–6) was higher for emergency call patients. GP-requested patients had significantly lower mNEWS2 scores in all age groups. In patients aged 66 years and above, median scores for both GP-requested and emergency call patients were similar and higher. GP-requested patients were older, with a higher degree of comorbidity and significantly longer hospital stays, whereas emergency call patients were more often admitted to the ICU. Age, comorbidity, mNEWS2 score and male sex were associated with increased risk of mortality for both groups. Non-specific diagnoses were frequently assigned in both groups, though most prevalent for emergency call patients. For GP-requested patients, the highest number of deaths were among the non-specific diagnoses and respiratory diseases, whereas most deaths were found among patients with circulatory diseases in the emergency call group.
In a Danish population of adult emergency department patients, Bech et al found that abnormal vital sign values and urgency level were associated with immediate mortality (within 4 hours of ED arrival), whereas age, male sex, and comorbidity were all increasingly associated with 30-day mortality.Citation21 Immediate mortality was also associated with circulatory diseases. In the present study, abnormal vital signs (high mNEWS2 score) and ICU admission were more frequent among emergency call patients, as were deaths among patients with circulatory diseases, partially explaining the higher immediate mortality in this group. At 7 days, the difference in mortality between the two groups diminished and beyond one week mortality was more frequent in the group of GP-requested patients, who were older and with more comorbidity. During our study period, 25% of the patients had runs with both emergency calls and GP-requested ambulances, which could suggest overlap in patient groups or independent disease episodes of different character. Patients often experience difficulty in navigating acute healthcare services, which may result in both more calls to primary care rather than 112, even for time-critical diseases, and more calls to 112 among patients not in need of urgent healthcare.Citation22,Citation23
In the UK, a new medical hotline number for non-emergency health problems was introduced in 2013. The expectation was that this would reduce calls to emergency medical services, yet following the introduction there was an increase in ambulance dispatches.Citation24,Citation25 Similarly, in 2014 a medical hotline number staffed primarily by nurses was introduced in the Capital Region of Denmark, replacing the out-of-hours GP service. The number was for non-life- or limb-threatening acute disease or injury that could not wait until GP office hours. After implementation, an increase in acute hospital contacts was reported.Citation25
Patient diagnoses were dominated by injuries, non-specific diagnoses, circulatory- and respiratory diseases in the present study. This is in accordance with earlier findings in other Danish regions and other countries.Citation26–30 The proportion of non-specific diagnoses was lower among the GP-requested patients. In Denmark, patients are often seen and examined physically by a GP before ambulance request and conveyance to hospital, improving triage ability. As opposed to a physical examination, telephone triage is limited by lack of visual clues and vital signs.Citation31
Non-specific diagnoses comprised the largest groups of assigned diagnoses in both groups, and especially in the GP-requested patients, there were many deaths within these diagnoses. The oldest ambulance patients in the current study exhibited a high degree of acute disease severity, putting them at a higher risk of dying within a short-time frame.
Study Limitations
Medical records without a registered Danish civil registration number were excluded from the study (N = 17,721), corresponding to 6.5% of the initial data set. This could introduce a possibility of bias as these patients may have unknown common characteristics that would be missing from the included data set. Since GPs know the identity of the majority of their patients, most patients with missing registration number are found in the emergency call group. Here, more than twice as many registration numbers are missing, which is a limitation in the comparison of the two groups as missingness could be associated with both high or low disease severity.
Danish registries are among the best in the world, strengthening the follow-up and information on preexisting conditions.Citation12,Citation32 In the present study, comorbidity was based on patients with hospital contacts within the last five years only, while comorbidities managed by their GP only were not included. This will most likely mean that patients with the most serious comorbidities are included (since they will more often require hospital contacts in outpatient clinics and similar setups).
The exclusion of patients with certain diagnoses who died upon hospital arrival is a limitation as they represent seriously ill patients. However, since the use of these diagnoses is inconsistent, this presents a poor basis for comparison, which was the reason for exclusion.
Another limitation is the possible overlap between the GP-requested and emergency call groups. One fourth of the patients had ambulance runs both after emergency calls and requested by a GP during the entire study period. Since patients could potentially be part of both groups, this might lead to an underestimating of the differences between the two groups, especially regarding inherent patient characteristics such as age, sex, and comorbidity, less so disease severity in each independent disease episode.
The missing measurements of vital signs is a limitation. In our calculation of the mNEWS2 score, we chose to consider missing vital signs as normal – ie, not changing the score calculation based on the vital signs available. Missing vital signs may be associated with both severe and mild disease. In a previous study by our group using the same method and a similar cohort, high degree of missing vital signs was associated with higher mortality.Citation19 In our study, less than 10% had no vital signs measured and a mNEWS2 score could therefore not be calculated. However, most patients had more than three vital signs measured and especially for high mNEWS2 scores there were only few missing values (eFigure 1). Despite this, in the comparison of disease severity, our approach may have led to an underestimation – both in the GP-requested and emergency call group.
The study period included the covid-19 pandemic period, although this only accounts for a minor portion of the study period. A previous Danish study found a marked reduction in unplanned hospital attendances during the pandemic, which should be taken into consideration when interpreting the results of the current study.
Conclusion
GP-requested ambulance patients constituted close to half of all emergency ambulance runs and mortality surpassed that of the emergency call ambulance patients a week after the ambulance run. GP-requested patients were older and with more comorbidity, but also with substantial acute disease severity, longer hospital stays and serious conditions, especially among the oldest patients.
As the proportion of older people increases in most western countries, it is expected that ambulance requests will also increase. This study showed that especially older patients were conveyed by ambulance after primary care contacts. Thus, it is not unlikely that primary care ambulance requests may rise substantially in the coming years in countries with similar healthcare setups (eg, Norway, the Netherlands, UK). Alongside the increasing focus by ambulance services on non-conveyance of emergency call patients, perhaps it is time to revisit collaboration between primary care and ambulance services to ensure the best possible planning of patient courses and resource utilization. Especially, as reducing or altering access to one type of emergency care, will most likely lead to increased flow to another access point. This has been seen in both the UK and Denmark. It is important to investigate how these reductions or alterations may affect the entire acute patient population and the entire healthcare system and which solutions are possible going forward.
Ethics
As per Danish legislation, registry-based studies do not need approval by an Ethical Committee. Handover of medical records without informed patient consent was approved by the Danish Patient Safety Authority (2021-012621).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
LMW and MLM are minor shareholders in Treat Systems ApS. The authors report no other conflicts of interest in this work.
Data Sharing Statement
Data cannot be shared publicly as it contains sensitive patient information and restrictions apply. However, for researchers who have obtained approval for the handover of medical records (https://rn.dk/da/Til-fagfolk/Sundhed/Forskning/Videregivelse-af-patientjournaloplysninger), the dataset can be constructed by requesting data from the North Denmark EMS, and the Danish health data Authority at https://sundhedsdatastyrelsen.dk/da/english/health_data_and_registers/research_services/before_applying.
Additional information
Funding
References
- Lowthian JA, Jolley DJ, Curtis AJ, et al. The challenges of population ageing: accelerating demand for emergency ambulance services by older patients, 1995–2015. Med j Aust. 2011;194(11):574–578. doi:10.5694/j.1326-5377.2011.tb03107.x
- Dinh MM, Muecke S, Berendsen Russell S, et al. Demand for emergency services trends in new south wales years 2010–2014 (DESTINY): age and clinical factors associated with ambulance transportation to emergency departments. Prehosp Emerg Care. 2016;20(6):776–782. doi:10.1080/10903127.2016.1182603
- Evans CS, Platts-Mills TF, Fernandez AR, et al. Repeated emergency medical services use by older adults: analysis of a comprehensive statewide database. Ann Emergency Med. 2017;70(4):506–515.e3. doi:10.1016/j.annemergmed.2017.03.058
- World Health Organization. Ageing and health. www.who.int. Available from: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health. Accessed May 12, 2023.
- Torjesen I. Almost 1.5m emergency hospital admissions could have been avoided last year. BMJ. 2018;k2542. doi:10.1136/bmj.k2542
- Limb M. Ambulances should treat more and transport fewer patients, NHS Improvement says. BMJ. 2018;k4106. doi:10.1136/bmj.k4106
- Blodgett JM, Robertson DJ, Pennington E, Ratcliffe D, Rockwood K. Alternatives to direct emergency department conveyance of ambulance patients: a scoping review of the evidence. Scand J Trauma Resusc Emerg Med. 2021;29(1):4. doi:10.1186/s13049-020-00821-x
- Oosterwold J, Sagel D, Berben S, Roodbol P, Broekhuis M. Factors influencing the decision to convey or not to convey elderly people to the emergency department after emergency ambulance attendance: a systematic mixed studies review. BMJ Open. 2018;8(8):e021732. doi:10.1136/bmjopen-2018-021732
- Shepperd S, Cradduck-Bamford A, Butler C, et al. Hospital at Home admission avoidance with comprehensive geriatric assessment to maintain living at home for people aged 65 years and over: a RCT. Health Soc Care Deliv Res. 2022;10(2):1–124. doi:10.3310/HTAF1569
- Lindskou TA, Mikkelsen S, Christensen EF, et al. The Danish prehospital emergency healthcare system and research possibilities. Scand J Trauma Resusc Emerg Med. 2019;27(1):100. doi:10.1186/s13049-019-0676-5
- Søvsø MB, Huibers L, Bech BH, Christensen HC, Christensen MB, Christensen EF. Acute care pathways for patients calling the out-of-hours services. BMC Health Serv Res. 2020;20(1):146. doi:10.1186/s12913-020-4994-0
- Laugesen K, Ludvigsson JF, Schmidt M, et al. Nordic health registry-based research: a review of health care systems and key registries. CLEP. 2021;13:533–554. doi:10.2147/CLEP.S314959
- von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. doi:10.1016/j.jclinepi.2007.11.008
- Statistics Denmark. FOLK1A: population on the 1st day of the quarter, by area, sex, age and marital status. Available from: https://www.statistikbanken.dk/FOLK1A. Accessed July 23, 2024.
- World Health Organization. international classification of diseases (ICD). international statistical classification of diseases and related health problems (ICD). Available from: https://www.who.int/standards/classifications/classification-of-diseases. Accessed May 12, 2023.
- Poulsen NR, Kløjgård TA, Lübcke K, Lindskou TA, Søvsø MB, Christensen EF. Completeness in the recording of vital signs in ambulances increases over time. Dan Med J. 2020;67(2):A07190421.
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8
- Royal College of Physicians. National Early Warning Score (NEWS): Standardising the Assessment of Acute-Illness Severity in the NHS. Royal College of Physicians; 2012.
- Lindskou TA, Ward LM, Søvsø MB, Mogensen ML, Christensen EF. Prehospital early warning scores to predict mortality in patients using ambulances. JAMA Network Open. 2023;6(8):e2328128. doi:10.1001/jamanetworkopen.2023.28128
- Davidson-Pilon C. lifelines: survival analysis in Python. JOSS. 2019;4(40):1317. doi:10.21105/joss.01317
- Bech CN, Brabrand M, Mikkelsen S, Lassen A. Risk factors associated with short term mortality changes over time, after arrival to the emergency department. Scand J Trauma Resusc Emerg Med. 2018;26(1):29. doi:10.1186/s13049-018-0493-2
- Lehm KK, Andersen MS, Riddervold IS. Non-urgent emergency callers: characteristics and prognosis. Prehosp Emerg Care. 2017;21(2):166–173. doi:10.1080/10903127.2016.1218981
- Doggen CJM, Zwerink M, Droste HM, et al. Prehospital paths and hospital arrival time of patients with acute coronary syndrome or stroke, a prospective observational study. BMC Emerg Med. 2016;16(1):3. doi:10.1186/s12873-015-0065-y
- Turner J, O’Cathain A, Knowles E, Nicholl J. Impact of the urgent care telephone service NHS 111 pilot sites: a controlled before and after study. BMJ Open. 2013;3(11):e003451. doi:10.1136/bmjopen-2013-003451
- Fløjstrup M, Bogh SB, Henriksen DP, Bech M, Johnsen SP, Brabrand M. Increasing emergency hospital activity in Denmark, 2005–2016: a nationwide descriptive study. BMJ Open. 2020;10(2):e031409. doi:10.1136/bmjopen-2019-031409
- Christensen EF, Larsen TM, Jensen FB, et al. Diagnosis and mortality in prehospital emergency patients transported to hospital: a population-based and registry-based cohort study. BMJ Open. 2016;6(7):e011558. doi:10.1136/bmjopen-2016-011558
- Arvig M, Mogensen C, Skjøt-Arkil H, Johansen I, Rosenvinge F, Lassen A. Chief complaints, underlying diagnoses, and mortality in adult, non-trauma emergency department visits: a population-based, multicenter cohort study. WestJEM. 2022;23(6). doi:10.5811/westjem.2022.9.56332
- Blinkenberg J, Pahlavanyali S, Hetlevik Ø, Sandvik H, Hunskaar S. General practitioners’ and out-of-hours doctors’ role as gatekeeper in emergency admissions to somatic hospitals in Norway: registry-based observational study. BMC Health Serv Res. 2019;19(1):568. doi:10.1186/s12913-019-4419-0
- Okamoto J, Katayama Y, Kitamura T, et al. Profile of the ORION (Osaka emergency information Research Intelligent Operation Network system) between 2015 and 2016 in Osaka, Japan: a population-based registry of emergency patients with both ambulance and in-hospital records. Acute Med Surg. 2019;6(1):12–24. doi:10.1002/ams2.371
- Vloet LCM, De Kreek A, Van Der Linden EMC, et al. A retrospective comparison between non-conveyed and conveyed patients in ambulance care. Scand J Trauma Resusc Emerg Med. 2018;26(1):91. doi:10.1186/s13049-018-0557-3
- Salk ED, Schriger DL, Hubbell KA, Schwartz BL. Effect of visual cues, vital signs, and protocols on triage: a prospective randomized crossover trial. Ann Emergency Med. 1998;32(6):655–664. doi:10.1016/S0196-0644(98)70063-0
- Frank L. The Epidemiologist’s Dream: Denmark. Science. 2003;301(5630):163. doi:10.1126/science.301.5630.163
