Abstract
Objective
To examine the prevalence of comorbidity among patients diagnosed with epithelial ovarian cancer in the Central Denmark Region and to study the impact of comorbidity on cancer survival over time.
Methods
We included women recorded with a first-time diagnosis of epithelial ovarian cancer in the Danish National Registry of Patients in the Central Denmark region between 2000 and 2011. We followed their survival through the Danish Civil Registration System. We estimated 1- and 5-year survival overall and stratified by Charlson Comorbidity Index score. We used Cox proportional hazard regression analyses to compute adjusted mortality rate ratios (MRRs) within different calendar time periods overall and by comorbidity level.
Results
We identified 1,540 patients. In 2000–2002, 25% of the newly diagnosed ovarian cancer patients had a comorbidity diagnosis compared with 35% in 2009–2011. Median age increased from 61 to 66 years. One-year overall survival changed from 73% (95% confidence interval [CI]: 69–78) in 2000–2002 to 69% (95% CI: 63–73) in 2009–2011, corresponding to an age- and comorbidity-adjusted MRR of 1.03 (95% CI: 0.79–1.36). Five-year survival changed only slightly during the study period, from 37% (95% CI: 32–42) in 2000–2002 to 39% (95% CI: 34–44) in 2009–2011. In patients with Charlson score ≥3, 1-year survival changed from 63% (95% CI: 35–81) in 2000–2002 to 41% (95% CI: 24–57) in 2003–2005 and thereafter stabilized. One-year survival changed from 56% (95% CI: 44–66) to 64% (95% CI: 53–74) in patients with Charlson score 1–2. Compared with Charlson score 0, adjusted 1-year MRRs for Charlson score ≥3 were 1.44 (95% CI: 0.62–3.36) in 2000–2002 and 2.11 (95% CI: 1.27–3.51) in 2009–2011, whereas adjusted 1-year MRRs for Charlson score 1–2 changed from 2.04 (95% CI: 1.33–3.14) in 2000–2002 to 1.09 (95% CI: 0.69–1.71) in 2009–2011.
Conclusion
Comorbidity increased among ovarian cancer patients over time and was associated with poor survival. One- and 5-year overall survivals changed only little and an expected decrease in survival, following increased prevalence of comorbidity and increasing age of patients, may have been counteracted by more aggressive surgery.
Introduction
Epithelial ovarian cancer is the leading cause of death among women diagnosed with gynecological cancer in Western countriesCitation1,Citation2 with a 5-year survival of 40% or less.Citation3,Citation4 Because of its intra-abdominal location, diagnosis of ovarian cancer is difficult. Lack of clearly defined symptoms often makes ovarian cancer undetected until an advanced stage with poor prognosis.Citation5
Average age in women at cancer diagnosis is 63 years,Citation6 and comorbidity is therefore frequent.Citation7,Citation8 The often unspecific symptoms of ovarian cancer may be disguised by symptoms of prevalent comorbid diseases or their treatment, and thereby delay cancer diagnosis. The main treatments for ovarian cancer are radically intended surgery and postoperative chemotherapy.Citation9,Citation10 However, in order to undergo surgery or receive chemotherapy, the patient has to meet the criteria required for treatment regarding functional status and comorbidities. Patients with reduced functional status or severe comorbidity may tolerate anticancer treatment less well than patients without comorbidity and may therefore be excluded from anticancer treatment or receive the treatment in a reduced form.Citation11 Previous studies have shown that presence of comorbidity is associated with poorer prognosis of ovarian cancer.Citation5,Citation11,Citation12 Comorbid diseases may increase the risk of complications resulting in lowering of functional status.
This study extends a previous study from Denmark during 1995–2005,Citation12 which showed that 5% of ovarian cancer had severe comorbidity at diagnosis and that comorbidity was associated with reduced survival of ovarian cancer patients. Our aims were to examine the prevalence of comorbidity in patients diagnosed with epithelial ovarian cancer in the Central Denmark Region from 2000 through 2011 and to examine recent temporal changes in survival and mortality according to level of comorbidity.
Materials and methods
Study population
We conducted this population-based cohort study in the Central Denmark region, which has approximately 1.2 million inhabitants. The Danish National Health Service provides universal, tax-supported health care, guaranteeing unfettered access to general practitioners and hospitals and partial reimbursement for prescribed drugs. Virtually no ovarian cancer patients were treated in private hospitals during the study period. Accurate and unambiguous linkage of all registries at the individual level is possible in Denmark by means of the unique civil personal registry number (CPR-number) assigned to each Danish citizen at birth or immigration.
Identification of patients with ovarian cancer
The Danish National Registry of Patients (DNRP) contains information on all discharges from nonpsychiatric hospitals in Denmark since 1977 and from emergency room and outpatient visits at hospitals since 1995.Citation13 Each hospital discharge or outpatient visit is recorded in the registry with one primary diagnosis and one or more secondary diagnoses classified according to the International Classification of Diseases, 8th edition (ICD-8) until the end of 1993, and ICD-10 thereafter. Using the DNRP, we identified all patients with a diagnosis of ovarian cancer (ICD-8 code 183.00–183.09 and ICD-10 code C56.x) from January 1, 2000 to December 31, 2011.
Comorbidity at diagnosis
To assess patient comorbidity, we computed Charlson Comorbidity Index (CCI) scores for each patient based on DNRP hospitalization records within 10 years preceding the date of cancer diagnosis. The CCI has been adapted and validated for use with hospital discharge data for the prediction of short- and long-term mortality.Citation14 A recent study found the positive predictive value of the Charlson comorbidities in the DNPR to be consistently high.Citation15 The following disease categories are included: liver diseases; myocardial infarction; congestive heart failure; peripheral vascular disease; chronic pulmonary disease; cerebrovascular disease; hemiplegia; dementia; connective tissue disease; ulcer disease; diabetes; renal disease; solid and hematological cancer; and HIV/AIDS. For this study, ovarian cancer was excluded from the solid cancer category when we computed the CCI. Cancer diagnoses within 60 days before the ovarian cancer diagnosis were excluded from the calculations in order to eliminate possible nonspecific cancer diagnoses registered during the diagnostic process of the ovarian cancer. We categorized comorbidities as hospital-registered comorbidity (Charlson score 0), moderate (Charlson score 1–2), or severe (Charlson score ≥3).
Vital status
We linked members of the study cohort via their CPR-number to the Danish Civil Registration System to obtain vital status. This registry has recorded all changes in vital status and migration for the entire Danish population since 1968, with daily electronic updates. Follow-up was through date of death or December 31, 2011, whichever occurred first.
Statistical analysis
We computed the prevalence of comorbidity in study patients during four 3-year study periods (2000–2002, 2003–2005, 2006–2008, 2009–2011). For each comorbidity category, we constructed Kaplan–Meier survival curves for the different study periods. Next, we used Cox proportional hazards regression to compute 1- and 5-year crude and age-adjusted hazard ratios as a measure of relative mortality to assess the association of comorbidity with mortality using the Charlson score of 0 as the reference category in each time period. In the latter periods, we estimated 1- and 5-year survival using a hybrid analysis in which survival was estimated using the survival experience of patients in the previous periods.Citation16 The proportional hazards assumption was assessed graphically and found to be appropriate. All analyses were performed using SAS software (v 9.2; SAS Institute Inc, Cary, NC, USA). The Danish Data Protection Agency approved the study (record number 2009-41-3866).
Results
Descriptive characteristics of the ovarian cancer cohort
A total of 1,540 women were diagnosed with epithelial ovarian cancer from 2000 through 2011 (). Among these women, 1,054 (68%) had Charlson score 0, 357 (23%) had Charlson score 1–2, and 129 (8%) had Charlson score ≥3. During the study period, the proportion of patients with registered comorbidity increased steadily from 25% in 2000–2002 to 35% in 2009–2011. The proportion of patients with Charlson score ≥3 increased from 4% in 2000–2002 to 11% in 2009–2011. Median age increased from 61 to 66 years in the same period. Any cancer was the most prevalent comorbidity, registered in 7.9% (121) of the ovarian cancer patients, followed by cerebrovascular disease in 5.8% (89), chronic obstructive pulmonary disease COPD) in 5.3% (81), and previous metastatic cancer in 3.9% (60). The increasing prevalence of comorbidity over time was evenly distributed among the most frequent comorbidities. Metastatic cancer had the largest increase in prevalence from a low of 0.8% in 2000–2002 (probably due to chance) to 4.3% in 2003–2005, thereafter remaining at the same level.
Table 1 Characteristics of women diagnosed with epithelial ovarian cancer from 2000 through 2011
Survival and mortality by level of comorbidity
One-year overall survival changed from 73% in 2000–2002 to 69% in 2009–2011, corresponding to an age- and comorbidity-adjusted mortality rate ratio (MRR) of 1.03 (95% confidence interval [CI]: 0.79–1.36) (). Five-year survival changed only slightly from 37% in 2000–2002 to a predicted survival of 39% in 2009–2011, and the corresponding adjusted MRR was 0.86 (95% CI: 0.72–1.03) in 2009–2011 compared with patients diagnosed in 2000–2002.
Table 2 Overall survival and adjusted mortality rate ratios for epithelial ovarian cancer patients diagnosed from 2000 through 2011
When stratifying on comorbidity level, both 1-year and 5-year survival was clearly lowest in those with high comorbidity scores ().
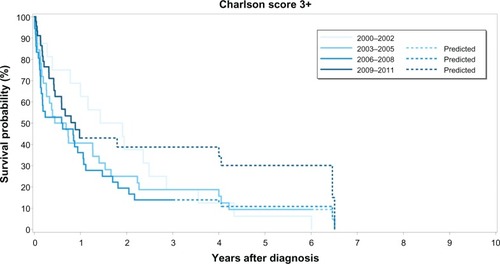
shows survival curves by year of diagnosis for women with Charlson score 0. One-year survival was 79% (95% CI: 74%–83%) in 2000–2002 and 74% (95% CI: 68%–80%) in 2009–2011 () whereas, 5-year survival seemed to rise slightly from 42% (95% CI: 37%–48%) in 2000–2002 to predicted 47% (95% CI: 41%–53%) in 2009–2011. For women with Charlson score 1–2, 1-year-survival increased from 56% (95% CI: 44%–66%) in 2000–2002 to 64% (95% CI: 53%–74%) for those diagnosed in 2009–2011 (). Five-year survival remained stable around 26% (). Women with Charlson score ≥3 () had a 1-year survival of 63% (95% CI: 35%–81%) in 2000–2002, which decreased to 41% (95% CI: 24%–57%) in the following period, 2003–2005, and was 43% (95% CI: 26%–59%) in 2009–2011. Five-year survival for women with Charlson score ≥3 was generally low, but appeared to increase from 6% (95% CI: 0%–25%) in 2000–2002 to predicted 21% (95% CI: 9%–37%) in 2009–2011. Compared with women with Charlson score 0, the age-adjusted 1-year MRR was increased in patients with Charlson score 1–2 in 2000–2002 (MRR 2.04, 95% CI: 1.33–3.14). In 2009–2011, the difference had decreased to MRR 1.09 (95% CI: 0.69–1.71). One-year MRR for women with Charlson score ≥3 was 1.44 (95% CI: 0.62–3.36) in 2000–2002 and 2.11 (95% CI: 1.27–3.51) in 2009–2011 compared with women with Charlson score 0. Five-year MRR for women with Charlson score 1–2 was 1.73 (95% CI: 1.28–3.24) in 2000–2002 and 1.39 (95% CI: 1.04–1.86) in 2009–2011. For women with Charlson score ≥3, the 5-year MRR was 2.23 (95% CI: 1.31–3.80) in 2000–2002 and 2.06 (95% CI: 1.36–3.10) in 2009–2011.
Figure 1 Kaplan–Meier survival curves for epithelial ovarian cancer patients diagnosed without Charlson Comorbidity IndexCitation14 score 0, according to four time periods of epithelial ovarian cancer diagnosis.
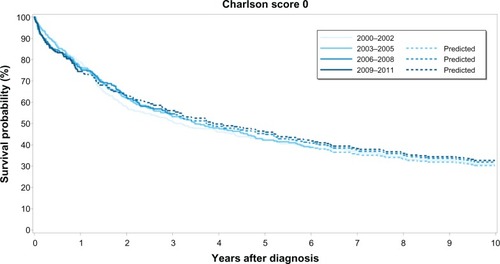
Figure 2 Kaplan–Meier survival curves for epithelial ovarian cancer patients diagnosed with Charlson Comorbidity IndexCitation14 score 1–2, according to four time periods of epithelial ovarian cancer diagnosis.
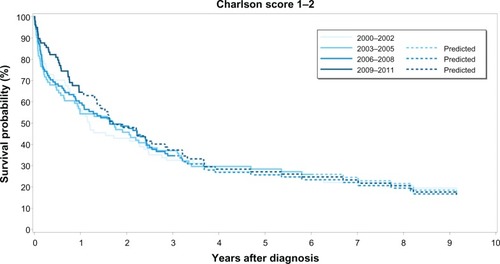
Figure 3 Kaplan–Meier survival curves for epithelial ovarian cancer patients diagnosed with Charlson Comorbidity IndexCitation14 score ≥3, according to four time periods of ovarian cancer diagnosis.
Discussion
In this population-based cohort study including 1,540 women with ovarian cancer, the overall 1- and 5-year survivals remained largely unchanged. The proportion of patients registered with any comorbidity increased steadily during the study period. When stratifying by comorbidity level, we found that survival consistently decreased with increasing comorbidity.
This study provides up-to-date information about the prevalence of comorbidity in women with ovarian cancer and how comorbidity influences the prognosis. Our study corroborates and extends prior Danish studies which have documented an association between comorbidity and ovarian cancer prognosis based on data from the Danish Cancer Registry (DCR).Citation5,Citation11 In accordance with Tetsche et al, who found a 6% increase in the prevalence of comorbidity from 19% among those diagnosed in 1995–1997 to 25% among those diagnosed in 2001–2004,Citation12 we observed a 10% increase in the prevalence of comorbidity. A Danish study, based on hospital discharge registries, similarly found that Charlson score ≥3 was a predictor of poorer survival.Citation12 Jørgensen et al found that elderly (≥70 years) ovarian cancer patients had higher comorbidity and a higher prevalence of advanced disease stage, and that severe comorbidity was a poor prognostic factor.Citation11 During our study, the median patient age increased by 5 years, which, to some extent, explains the increasing prevalence of comorbidity over time. However, the completeness of registration of medical diseases in the DNRP may also have increased over time. The relationship between stage of ovarian cancer and comorbidity has been investigated in a Danish study.Citation5 The authors found that presence of severe comorbidity was associated with advanced cancer stage and possibly related to delay in cancer diagnosis, maybe because ovarian cancer symptoms were ascribed to the comorbidities.Citation5 We did not have information on cancer stage, which is a limitation of our study. It is possible that severe comorbidity, also in our study, was related to advanced cancer stage at diagnosis. Neither did we have information on cancer treatment and it is possible that increased attention to the comorbidity and its manifestations may have led to suboptimal anticancer (surgical and medical) treatment.Citation11 It is also possible that the decrease in 1-year survival for women with Charlson score ≥3 could be due to an increase in the number and complexity of the comorbid diseases within this category.
Surgical treatment of ovarian cancer in Denmark has been centralized.Citation17 Centralization and more extensive surgery have been implemented in recent years. Despite an increasing median age of the patients and increased prevalence of comorbidity, overall 1- and 5-year survivals changed only little during the study time. More aggressive surgery may have counteracted an expected decrease in survival.
The main strengths of our study are the population-based approach, minimizing the risk of systematic errors, and virtually complete follow-up for mortality through the Civil Registry System. Prior cancer studies have often used data from the DCR because of its high completeness and accuracy.Citation18,Citation19 Because we aimed to provide up-to-date information on ovarian cancer prognosis, we used the DNRP to identify patients with ovarian cancer since incidence data for the most recent period is not available in the DCR: the DCR is updated until December 31, 2010. However, ovarian cancer diagnoses in the DNRP may be affected by some degree of misclassification.Citation20 By comparing data from the hospital registry with the DCR, a previous Danish study found that borderline tumors comprised 18% of ovarian cancers diagnosed between 1994 and 2003.Citation20 Patients with borderline tumors have a 5-year survival of 86%,Citation21 which is higher than for patients with invasive ovarian cancer. Before 2001, there was no specific code for borderline tumors in the DNRP and these were coded as ovarian tumors. Thus, when interpreting our results from before 2001, and until the new code was properly implemented, it is important to bear in mind that the survival estimates may differ from results based purely on invasive cancers because our first study period, 2000–2002, is likely to contain some degree of misclassified borderline tumors. Therefore, the better 1-year survival of patients diagnosed in 2000–2002 may have been caused by a higher proportion of patients registered with less aggressive borderline tumors.
Accuracy of coding of the Charlson comorbidities in the DNRP is reported to be very high.Citation15 Still, ovarian cancer may be difficult to diagnose and the patient may have unspecific symptoms for some time preceding the ovarian cancer diagnosis. Such paraneoplastic phenomena may have been misdiagnosed as comorbidities included in the CCI and may have inflated the prevalence of comorbidity. The study was conducted using discharge diagnose from the DNRP to obtain information on comorbidities, thereby avoiding recall bias. However, only severe cases of chronic diseases have been treated in hospital and thereby registered in the DNRP. Mild or moderate cases of diseases (eg, COPD, diabetes) may only have received treatment in general practice and are not included in this study.
In this population-based study of ovarian cancer patients, we found an increasing prevalence of comorbid diseases during the study period and an elevated mortality in those with high comorbidity level. Overall 1- and 5-year survival in ovarian cancer patients changed only slightly over the last decade, from 73% to 69% and from 37% to 39%, respectively.
Despite increased prevalence of comorbidity and increasing age, survival changed only little. Centralization and more aggressive surgery may have counteracted an expected decrease in survival.
Acknowledgments
Cancer analyses in the Central Denmark Region were conducted as part of the Aarhus University Disease Epidemiology and Outcomes (AUDEO) Project at the Department of Clinical Epidemiology, Aarhus University Hospital.
Disclosure
The authors report no conflicts of interest in this work.
References
- JemalABrayFCenterMMFerlayJWardEFormanDGlobal cancer statisticsCA Cancer J Clin2011612699021296855
- SuZGraybillWSZhuYDetection and monitoring of ovarian cancerClin Chim Acta201341534134523165217
- GrannAFNørgaardMBlaakærJSøgaard-AndersenEJacobsenJBSurvival of patients with ovarian cancer in central and northern Denmark, 1998–2009Clin Epidemiol20113Suppl 1596421814472
- TetscheMSNørgaardMJacobsenJImproved survival of patients with ovarian cancer in Northern Denmark, 1985–2004Eur J Gynaecol Oncol200627211912216620051
- TetscheMSDethlefsenCPedersenLSorensenHTNorgaardMThe impact of comorbidity and stage on ovarian cancer mortality: a nationwide Danish cohort studyBMC Cancer200883118230177
- Cancer Facts and Figures 2012Atlanta, GAAmerican Cancer Society2012 Available from: http://www.cancer.org/acs/groups/content/@epide-miologysurveilance/documents/document/acspc-031941.pdfAccessed December 15th, 2012
- JørgensenTLHallasJFriisSHerrstedtJComorbidity in elderly cancer patients in relation to overall and cancer-specific mortalityBr J Cancer201210671353136022353805
- WeddingURoehrigBKlippsteinAComorbidity in patients with cancer: prevalence and severity measured by cumulative illness rating scaleCrit Rev Oncol Hematol200761326927617207632
- BrunJLFeylerACheneGSaurelJBrunGHockeCLong-term results and prognostic factors in patients with epithelial ovarian cancerGynecol Oncol2000781212710873404
- FujiwaraKSakuragiNSuzukiSFirst-line intraperitoneal carboplatin-based chemotherapy for 165 patients with epithelial ovarian carcinoma: results of long-term follow-upGynecol Oncol200390363764313678738
- JørgensenTLTeiblumSPaludanMSignificance of age and comorbidity on treatment modality, treatment adherence, and prognosis in elderly ovarian cancer patientsGynecol Oncol2012127236737422800653
- TetscheMSNørgaardMJacobsenJWogeliusPSørensenHTComorbidity and ovarian cancer survival in Denmark, 1995–2005: a population-based cohort studyInt J Gynecol Cancer200818342142717692093
- LyngeESandegaardJLReboljMThe Danish National Patient RegisterScand J Public Health201139Suppl 7303321775347
- CharlsonMEPompeiPAlesKLMacKenzieCRA new method of classifying prognostic comorbidity in longitudinal studies: development and validationJ Chronic Dis19874053733833558716
- ThygesenSKChristiansenCFChristensenSLashTLSørensenHTThe predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of PatientsBMC Med Res Methodol2011118321619668
- BrennerHRachetBHybrid analysis for up-to-date long-term survival rates in cancer registries with delayed recording of incident casesEur J Cancer200440162494250115519525
- OttesenBIversenMGKehletHSurgical treatment for ovarian cancer in Denmark 2004–2007Ugeskr Laeger20091714217220 Danish19174035
- StormHHCompleteness of cancer registration in Denmark 1943–1966 and efficacy of record linkage proceduresInt J Epidemiol198817144493384548
- StormHHMichelsenEVClemmensenIHPihlJThe Danish Cancer Registry – history, content, quality and useDan Med Bull19974455355399408738
- TetscheMSNørgaardMSkriverMVAndersenESLashTLSørensenHTAccuracy of ovarian cancer ICD-10 diagnosis in a Danish population-based hospital discharge registryEur J Gynaecol Oncol200526326627015991523
- MenzinAWGalDLovecchioJLContemporary surgical management of borderline ovarian tumors: a survey of the Society of Gynecologic OncologistsGynecol Oncol20007817910873401