Abstract
Objective
Current data on hospitalization and prognosis of acute asthma and status asthmaticus are inconclusive. We aim to analyze the rate of first-time hospitalizations for status asthmaticus among patients of all ages, the proportion admitted to intensive care units (ICU), and the 30-day mortality over a 16-year period.
Methods
In this population-based cohort study, we used medical registries to identify all first-time status asthmaticus hospitalizations in Denmark from 1996 through 2011. Data on comorbidities were also obtained. We computed yearly hospitalization rates overall and by gender and age groups, and estimated the proportion requiring ICU admission. We estimated 30-day age- and gender-standardized mortality. We examined potential misclassification from acute exacerbation of chronic obstructive pulmonary disease (COPD) by excluding patients with preexisting or concurrent COPD.
Results
Of the 5,001 patients identified with a first-time status asthmaticus hospitalization, 50.5% were male, 40.3% were <15 years old, and 12.4% had comorbidity. The hospitalization rate increased from 48.0 per 1,000,000 person-years (PY) (95% confidence interval [CI]: 45.1–51.1 PY) during 1996–1999 to 70.1 per 1,000,000 PY (95% CI: 66.7–73.7 PY) during 2008–2011. This may be explained by an increased hospitalization rate of children. The standardized 30-day mortality risk declined from 3.3% (95% CI: 2.5%–4.1%) in 1996–1999 to 1.5% (95% CI: 0.9%–2.1%) in 2008–2011. During 2005–2011, 10.1% of status asthmaticus patients were admitted to the ICU. Hospitalization rates and mortality risk decreased by excluding 939 patients also registered with COPD, but overall temporal changes did not change.
Conclusion
From 1996 to 2011, status asthmaticus hospitalization rate increased but remained below 100 hospitalizations per 1,000,000 PY. Thirty-day mortality risk was halved to less than 2%.
Introduction
Status asthmaticus is a life-threatening medical emergency, defined as an acute exacerbation of asthma that is refractory to initial standard treatment.Citation1–Citation4 Status asthmaticus involves a risk of respiratory failure, and intensive care may be needed.Citation5 The prevalence of asthma has increased for decades, although some data now indicate a stable prevalence within the last decade.Citation6–Citation11 The World Health Organization reported in 2007 that 300 million people worldwide had asthma, and reported asthma as the most common chronic disease among children.Citation12,Citation13
Appendix 4 First-time hospitalization rates of patients with status asthmaticus, Denmark, 1996–2011, stratified by gender. Patients with a registry diagnosis of chronic obstructive pulmonary disease excluded.
Current data about hospitalization rates and prognosis of acute asthma and status asthmaticus are inconclusive.Citation1,Citation3,Citation5,Citation7–Citation9,Citation14–Citation26 We identified 19 studies on status asthmaticus hospitalizations and prognosis using the definition of status asthmaticus provided above.Citation1,Citation3,Citation5,Citation7–Citation9,Citation14–Citation26 These studies were restricted to either adult or pediatric study populationsCitation1,Citation7–Citation9,Citation14–Citation20,Citation22–Citation26 or were limited to a few hospitals or intensive care units (ICUs),Citation7,Citation8,Citation14,Citation15,Citation18,Citation21,Citation23,Citation25,Citation26 reducing generalizability. Furthermore, 14 studies included readmissions,Citation1,Citation7,Citation8,Citation14–Citation16,Citation18–Citation21,Citation23–Citation26 which may affect estimates of hospitalization rates and prognosis due to the increased risk of further admissions and worsened prognosis.Citation7 A large population-based longitudinal study of patients of all ages is needed to provide more accurate estimates of hospitalization rate and prognosis of first-time status asthmaticus episodes.
We conducted a registry-based longitudinal cohort study, encompassing all first-time pediatric and adult hospitalizations for status asthmaticus registered in Denmark during the past 16 years, to analyze changes in hospitalization rates and 30-day mortality, and to assess the proportion of status asthmaticus patients admitted to an ICU.
Methods and materials
Study design and setting
We conducted this cohort study using population-based medical registries in Denmark.
The Danish population (approximately 5.5 million personsCitation27) has unfettered access to outpatient and inpatient medical care through the tax-funded national health care system. We linked population databases at the individual level using the unique Danish 10-digit identification number (CPR) assigned to all Danish residents by the Danish Civil Registration System since January 1, 1968.Citation28
Patients with status asthmaticus
We identified all Danish residents hospitalized with a first-time primary or secondary diagnosis of status asthmaticus from January 1, 1996 to December 31, 2011, by searching the Danish National Patient Registry (NPR).Citation29 The study period was based on the availability of relevant registries and allows an implementation period of the International Classification of Diseases, 10th revision (ICD-10) introduced in Denmark in 1994. We eliminated recurrent status asthmaticus by omitting subjects with a diagnosis of status asthmaticus from 1980 through 1995.
The NPR, established in 1977, contains virtually complete information on patient contacts with Danish nonpsychiatric hospitals. Since 1995, the NPR also has included data on outpatient clinic and emergency department visits.Citation29,Citation30 Data on ICU admissions have been routinely recorded since 2005,Citation31 enabling us to assess the proportion of patients admitted to an ICU during the last 7 years of the study period.
Records in the NPR contain hospital and department codes, admission and discharge dates, diagnoses (one primary diagnosis and up to 19 secondary diagnoses) assigned by the discharging physicians, major medical treatments, and surgical procedures. Diagnoses have been coded according to the Danish version of the International Classification of Diseases, 8th revision (ICD-8) from 1977 to 1993 and according to the ICD-10 since 1994. The International Classification of Diseases, 9th revision (ICD-9) has never been used in Denmark. We used the ICD-8 code and the ICD-10 code for status asthmaticus () to identify all patients with a primary or secondary inpatient diagnosis of status asthmaticus.
Appendix 1 Diagnostic codes in the International Classification of Diseases
Demographics and mortality
We obtained data from the Danish Civil Registration System on gender, age, and date of death in deceased patients. The Civil Registration System is electronically updated daily and contains complete information for all Danish residents on gender, residence, vital status, and dates of birth, death, and emigration.
Comorbidity
We obtained information from the NPR on diagnoses of comorbid conditions included in the Charlson Comorbidity Index (CCI).Citation32 We included all inpatient and outpatient clinic diagnoses recorded within 5 years before the current status asthmaticus hospitalization. The CCI, a widely used comorbidity scoring system adapted for hospital discharge data, includes 19 conditions ().Citation33 Each condition is assigned a weight between one and six, reflecting prognostic impact, and the CCI score is computed as the sum of the weights. We defined three levels of comorbidity severity based on the CCI scores: 0 (low comorbidity level), 1–2 (medium comorbidity level), and ≥3 (high comorbidity level). We excluded chronic pulmonary diseases from the CCI, but included chronic obstructive pulmonary disease (COPD) () as a separate comorbidity, because an acute exacerbation of COPD can be clinically difficult to distinguish from status asthmaticus and can therefore cause possible misclassification.Citation34
Validation of the status asthmaticus diagnosis in the NPR
To validate the diagnosis of status asthmaticus in the NPR, we randomly selected three patients per calendar year, from January 1, 1994 to December 31, 2009, from a subset of our North Jutland cohort and retrieved their hospital discharge summaries. Based on the current definition of status asthmaticusCitation1–Citation4 and the level of details available in the discharge summaries, the diagnosis was confirmed when ≥2 of the following criteria were fulfilled: (1) presence of asthma symptoms (ie, dyspnea, wheezing, cough, chest tightness, and/or decreased peak flow); (2) the condition was refractory to standard initial treatment (inhalation of bronchodilators and/or steroids) and hospitalization was required; and (3) the condition was a medical emergency. A researcher with a Bachelor of Medical Science degree (JMCS) reviewed all the discharge records, and a physician (HG) re-reviewed the discharge records in cases of uncertainty. If disagreement occurred, a second physician (CFC) assessed the discharge record in question, and the majority determined the outcome. We calculated the positive predictive value of the NPR status asthmaticus diagnosis as the percentage of our random sample with an NPR status asthmaticus diagnosis that was confirmed by review of the discharge record,Citation35 according to the algorithm presented above. The exact 95% confidence interval (CI) for the positive predictive value was computed.
Statistical analysis
We computed frequencies of first-time status asthmaticus hospitalizations, overall and within categories of gender, age group, and comorbidity level. We divided status asthmaticus patients into five age groups: 0–1 years, 2–14 years, 15–39 years, 40–59 years, and ≥60 years. We analyzed data for children aged 0–1 year separately because of the uncertainty of diagnosing respiratory conditions in young children.Citation36 We also reported interquartile range (IQR) and median age. We presented results both for the study period as a whole and for four-year calendar periods (1996–1999, 2000–2003, 2004–2007, and 2008–2011). We chose four-year intervals to allow sufficient statistical precision, while keeping enough intervals to allow comparison over time during the 16-year study period. For the period January 1, 2005 to December 31, 2011, we also examined the proportion of first-time status asthmaticus patients who were admitted to an ICU.
We estimated annual rates of first-time status asthmaticus hospitalizations with 95% CIs for all patients and by gender and age group, and illustrated annual hospitalization rates. The rates were calculated by dividing the number of first-time status asthmaticus hospitalizations by total time at risk of disease among all Danish residents, assuming that each person alive on January 1 of the year of interest contributed one person-year (PY; the denominator).Citation27 For gender and age groups, we used the corresponding subgroup of the population as the denominator. The resulting hospitalization rates are reported per 1,000,000 PY for all years together and for four-year calendar periods during the study period, respectively.
Patients were followed from admission until death, emigration, or for up to 30 days, whichever came first. We computed 30-day mortality overall and for each four-year calendar period. We used direct standardization to compute 30-day mortality risk,Citation37 including 95% CIs, standardized to the gender and age group distribution in the study population of the 2008–2011 period.
We conducted two sensitivity analyses. First, to assess potential misclassification of an acute exacerbation of COPD as status asthmaticus, we identified and excluded all status asthmaticus patients with a previous or concurrent COPD diagnosis recorded in the NPR, repeated all analyses, and assessed potential changes in the results. Second, to improve the specificity of the status asthmaticus diagnosis, we examined the number of hospitalizations among patients with status asthmaticus as their primary diagnosis, excluding patients with status asthmaticus only as their secondary diagnosis.
All statistical analyses were performed using Stata Release 11 (StataCorp, LP, College Station, TX, USA).
Results
Characteristics of study subjects
We identified 5,001 patients hospitalized with a first-time status asthmaticus diagnosis in Denmark from 1996 through 2011 (). Of these, 50.5% were male, 40.3% were younger than 15 years, and 87.6%, 10.1%, and 2.3% had a low, medium, and high comorbidity level, respectively ().
Table 1 Characteristics of patients with a first-time status asthmaticus hospitalization, Denmark, 1996–2011
Hospitalizations
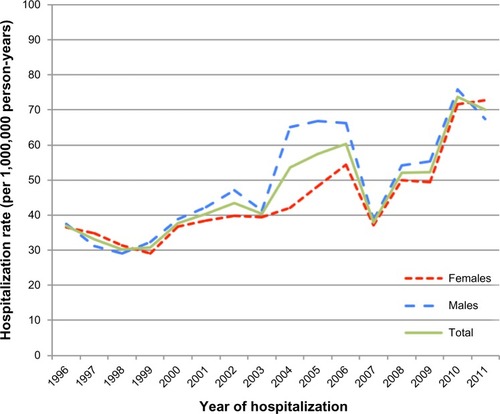
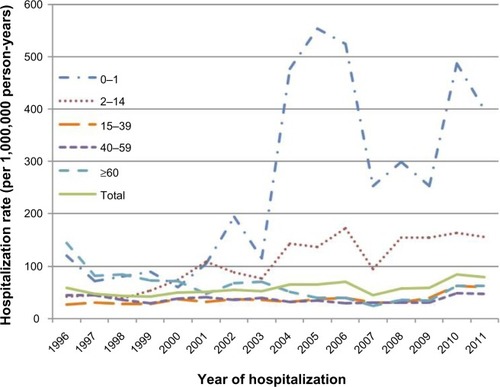
The annual hospitalization rates for all patients are illustrated in and . The hospitalization rate of all status asthmaticus patients increased during the study period: the hospitalization rate was 48.0 per 1,000,000 PY (95% CI: 45.1–51.1 per 1,000,000 PY) in 1996–1999, 52.0 per 1,000,000 PY (95% CI: 49.0–55.1 per 1,000,000 PY) in 2000–2003, 67.1 per 1,000,000 PY (95% CI: 57.8–64.4 per 1,000,000 PY) in 2004–2007, and 70.1 per 1,000,000 PY (95% CI: 66.7–73.7 per 1,000,000 PY) in 2008–2011.
Figure 1 First-time hospitalization rates of patients with status asthmaticus, Denmark, 1996–2011, stratified by gender.
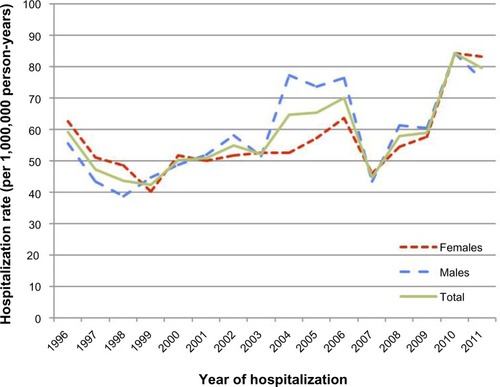
Figure 2 First-time hospitalization rates of patients with status asthmaticus, Denmark, 1996–2011, stratified by age group (years).
The gender distribution of patients with first-time status asthmaticus was similar throughout the study period, except for a higher hospitalization rate in 2004–2007 for males (67.6 per 1,000,000 PY [95% CI: 62.7–72.7 per 1,000,000 PY]) than for females (54.7 per 1,000,000 PY [95% CI: 50.4–59.2 per 1,000,000 PY]) ( and ).
The median age of the cohort declined during the study period, from 51.4 years (IQR: 23.1–68.7 years) in 1996–1999 to 17.2 years (IQR: 5.6–48.0 years) in 2008–2011 (). Hospitalization rates by age group are illustrated in . A steady increase in the hospitalization rate of 2–14 year olds was observed: from 44.9 per 1,000,000 PY (95% CI: 37.9–52.9 per 1,000,000 PY) in 1996–1999 to 157.3 per 1,000,000 PY (95% CI: 144.4–171.0 per 1,000,000 PY) in 2008–2011. A conspicuous peak among children under age 2 was seen in 2004–2007 (452.8 per 1,000,000 PY [95% CI: 396.8–514.6 per 1,000,000 PY]), compared with 1996–1999 (91.1 per 1,000,000 PY [95% CI: 67.6–120.1 per 1,000,000 PY]). The majority (68.5%) of this subgroup was between 1 and 2 years old. The hospitalization rate for patients aged ≥60 years decreased from 96.0 per 1,000,000 PY (95% CI: 86.8–105.9 per 1,000,000 PY) in 1996–1999 to 38.7 per 1,000,000 PY (95% CI: 33.2–44.9 per 1,000,000 PY) in 2004–2007. The hospitalization rate was even lower for patients aged 15–59 years ().
In all four-year calendar periods, the majority of status asthmaticus patients had no comorbid conditions according to CCI (). The proportion of patients with comorbidity (score ≥1) declined during the study period from 18.2% in 1996–1999 to 10.7% in 2008–2011.
During 2005–2011, 256 status asthmaticus patients were admitted to an ICU, corresponding to 10.1% of all 2,524 first-time status asthmaticus hospitalizations during the 2005–2011 period.
Mortality
In total, 162 (3.2%) of the 5,001 patients died within 30 days after their first-time hospitalization for status asthmaticus (). The standardized 30-day mortality risk declined during the 16-year period from 3.3% (95% CI: 2.5%–4.1%) in 1996–1999 to 1.5% (95% CI: 0.9%–2.1%) in 2008–2011.
Table 2 Thirty-day mortality of patients with a first-time status asthmaticus hospitalization, Denmark, 1996–2011
Sensitivity analyses
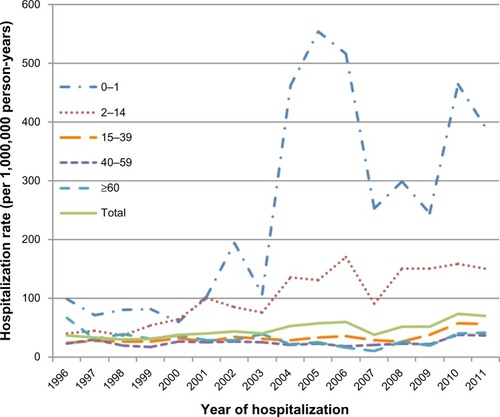
After excluding 939 (18.8%) COPD patients, we observed a lower rate of first-time status asthmaticus hospitalizations and a lower 30-day mortality, but similar temporal trends (–).
Appendix 5 First-time hospitalization rates of patients with status asthmaticus, Denmark, 1996–2011, stratified by age group (years). Patients with a registry diagnosis of chronic obstructive pulmonary disease excluded.
Appendix 2 Characteristics of patients with a first-time status asthmaticus hospitalization, Denmark, 1996–2011. Patients with a registry diagnosis of chronic obstructive pulmonary disease excluded
The second sensitivity analysis, excluding 860 (17.1%) patients registered with a secondary diagnosis of status asthmaticus only, showed virtually no changes in hospitalization trends or age distribution ().
Appendix 6 Characteristics of patients with a first-time status asthmaticus hospitalization, Denmark, 1996–2011. Patients registered with status asthmaticus as a “secondary” diagnosis excluded
Validation of the status asthmaticus registry diagnosis
The status asthmaticus diagnosis was confirmed in 42 out of a sample of 48 hospitalizations with a diagnosis of status asthmaticus, corresponding to a positive predictive value of 87.5% (95% CI: 74.7%–95.3%). A second reviewer reviewed 20 discharge summaries; of these, twelve were re-reviewed by a third reviewer because of disagreement between the first two reviewers.
Discussion
To the best of our knowledge, this is the first population-based study of first-time hospitalization for status asthmaticus among patients of all ages. We found that the status asthmaticus hospitalization rate increased over a 16-year period, which may be explained by the increase in hospitalization rates among children. During the same period, the associated 30-day mortality decreased. Ten percent of hospitalized status asthmaticus patients were admitted to an ICU.
Limitations and strengths
Our study relies on the quality of status asthmaticus diagnoses registered in the NPR. Although the NPR includes data on 99.4% of hospitalizations,Citation30 incomplete registrations of status asthmaticus in this registry would have led to underestimation of the hospitalization rates. Follow-up for death was virtually complete.
Changes in registration practices may have influenced our findings. However, this was minimized through use of the same ICD revision for diagnostic coding throughout the study period.
The process of clinical diagnosis of acute exacerbations in asthma can be difficult and can result in misclassification. Although a definition of status asthmaticus is available,Citation1–Citation4 there are several different terms, including acute asthma, severe asthma, and hospital admission due to asthma.Citation2,Citation5,Citation17,Citation19–Citation22,Citation24,Citation25,Citation38 Furthermore, status asthmaticus is the only sub-code among the asthma diagnoses in the ICD-10 that denotes an acute asthmatic condition. Clinicians could therefore be prone to diagnose and report less serious asthmatic attacks as status asthmaticus. However, we found a reasonable high positive predictive value for the status asthmaticus diagnosis in the NPR, and observed no major changes in our results when we excluded patients recorded as having COPD or had received status asthmaticus as a secondary diagnosis.
Comparison with other studies
In contrast to our findings, Hartman et al observed a halving in the rate of hospital admissions for status asthmaticus from 1.98 per 1,000 children in 1992 to 0.93 per 1,000 children in 2006 in their study of 28,309 hospitalized children in the US state of New Jersey.Citation16 The higher estimates compared with our findings may be explained by their inclusion of readmissions.Citation16
Rodrigo et al included 3,038 patients hospitalized for acute severe asthma at 19 tertiary-care hospitals in Spain and Latin America in 1994, 1999, and 2004, and found that 6.8% were admitted to an ICU.Citation17 The smaller proportion of patients admitted to the ICU compared with our findings may be explained by their restriction to patients aged 15–69 years.Citation17
The 30-day mortality observed in the present study was in the lower range compared with other studies showing status asthmaticus mortality ranging from 0.4% to 12% (and even higher among patients receiving mechanical ventilation).Citation1,Citation5,Citation7,Citation14,Citation15,Citation18–Citation20,Citation22,Citation23,Citation25 However, comparisons among studies are complicated by the restriction to ICU patients or different age groups in some studies.Citation7,Citation8,Citation14,Citation15,Citation18–Citation23,Citation25,Citation26
Our observation of decreased 30-day mortality over time is consistent with several studies finding a decreasing mortality due to asthma during the past decades.Citation1,Citation5,Citation6,Citation19,Citation21,Citation22 Stow et alCitation19 reported a significant decline in mortality risk from acute severe asthma among ICU patients between 1997 (4.7%) and 2003 (1.1%) in Australia, Gershon et alCitation6 reported a decrease in all-cause mortality in individuals with asthma between 1996 and 2005 in the state of Ontario, and Roberts et alCitation1 reported a 30-day case-fatality following asthma or status asthmaticus admission (0.9%) in Scotland, which has been decreasing since the mid-1990s.
Our 30-day mortality finding could possibly be explained by the restriction to first-time status asthmaticus hospitalizations, since the risk of further admissions and poor prognosis is increased by readmission,Citation7 and by the encompassing of all patients hospitalized with status asthmaticus, and not only patients admitted to an ICU or both patients hospitalized with asthma and status asthmaticus.Citation1,Citation7,Citation8,Citation14,Citation15,Citation18,Citation19,Citation21,Citation23,Citation26
Potential mechanisms
Several mechanisms may explain our findings. The increased hospitalization rate of status asthmaticus may be due to the increased prevalence of asthma during recent decades in line with international reports.Citation6,Citation7,Citation10,Citation12,Citation13 In addition, fuctuations in hospitalization rates for status asthmaticus could be related to fuctuations in other airway diseases, eg, asthmatic bronchitis, pneumonia, pseudo croup, and viral infections, provoking respiratory symptoms resembling asthma or exacerbation of asthma.Citation39 This applies especially to children and challenges the following control of asthma to avoid readmission and the risk of worsened prognosis.Citation7
The increased hospitalization rate of younger patients could explain the decreasing mortality over time, because younger patients have fewer comorbid conditions and in general a greater chance of surviving an emergency than older patients. The centralization of pediatric ICUs in Denmark and improved disease management, guidelines, and medical protocols during recent years could also explain the decreasing mortality over time,Citation40 because increased expertise and judicious judgments are advantageous when treating serious conditions as status asthmaticus.Citation38,Citation39,Citation41
Finally, changes in registration practices, over time, geographically, and/or related to pediatric/adult units that we are unaware of could have played a role. Our study was conducted in Denmark, a Western country with a tax-funded health care system, and our observations may be generalizable to other populations with similar demographics and health care systems. Future research needs to further examine possible underlying mechanisms and trends in disease severity.
Conclusion
We found that the first-time hospitalization rate for status asthmaticus in Denmark increased during the recent 16 years, but remained below 100 hospitalizations per 1,000,000 PY. This increase may be explained by increased hospitalization rates of children. Simultaneously, 30-day mortality halved to below 2%.
Acknowledgments
We are thankful to Elisabeth Kristoffersen at the Department of Clinical Epidemiology, who retrieved the medical discharge records used in the validation study of the status asthmaticus diagnosis in the NPR. The Department of Clinical Epidemiology, Aarhus University Hospital, and Aarhus University financially supported this research.
Disclosure
The authors report no conflicts of interest in this work.
References
- RobertsNJLewseyJDGilliesMTime trends in 30 day case-fatality following hospitalisation for asthma in adults in Scotland: a retrospective cohort study from 1981 to 2009Respir Med201310781172117723643488
- ShahRSaltounCAChapter 14: acute severe asthma (status asthmaticus)Allergy Asthma Proc201233Suppl 1S47S5022794687
- JagodaAShepherdSMSpevitzAJosephMMRefractory asthma, part 1: epidemiology, pathophysiology, pharmacologic interventionsAnn Emerg Med19972922622749018193
- CohenNHEigenHShaughnessyTEStatus asthmaticusCrit Care Clin19971334594769246526
- PapirisSKotanidouAMalagariKRoussosCClinical review: severe asthmaCrit Care200261304411940264
- GershonASGuanJWangCToTTrends in asthma prevalence and incidence in Ontario, Canada, 1996–2005: a population studyAm J Epidemiol2010172672873620716702
- TriasihRDukeTRobertsonCFOutcomes following admission to intensive care for asthmaArch Dis Child201196872973421540482
- ElsayeghDSaitoSEdenEShapiroJIncreasing severity of status asthmaticus in an urban medical intensive care unitJ Hosp Med20083320621118571779
- MannixRBachurRStatus asthmaticus in childrenCurr Opin Pediatr200719328128717505187
- PearceNAit-KhaledNBeasleyRWorldwide trends in the prevalence of asthma symptoms: phase III of the international study of asthma and allergies in childhood (ISAAC)Thorax200762975876617504817
- RobertsonCFRobertsMFKappersJHAsthma prevalence in Melbourne schoolchildren: have we reached the peak?Med J Aust2004180627327615012564
- World Health OrganizationAsthma Available from: http://www.who.int/respiratory/asthma/enAccessed June 25, 2013
- Global Alliance against Chronic Respiratory Disease (GARD)Global surveillance, prevention and control of chronic respiratory diseases: a comprehensive approachGenevaGARD2007
- SheikhSKhanNRyan-WengerNMcCoyKSDemographics, clinical course, and outcomes of children with status asthmaticus treated in a pediatric intensive care unit: 8-year reviewJ Asthma201350436436923379585
- PetersJIStupkaJESinghHStatus asthmaticus in the medical intensive care unit: a 30-year experienceRespir Med2012106334434822188845
- HartmanMELinde-ZwirbleWTAngusDCWatsonRSTrends in admissions for pediatric status asthmaticus in New Jersey over a 15-year periodPediatrics20101264e904e91120876177
- RodrigoGJPlazaVBellido-CasadoJThe study of severe asthma in Latin America and Spain (1994–2004): characteristics of patients hospitalized with acute severe asthmaJ Bras Pneumol2009357635644 Portuguese19669001
- ChiangBLHsiehCTWangLCClinical course and outcome of children with status asthmaticus treated in a pediatric intensive care unit: a 15-year reviewJ Microbiol Immunol Infect200942648849320422133
- StowPJPilcherDWilsonJImproved outcomes from acute severe asthma in Australian intensive care units (1996 2003)Thorax2007621084284717389751
- GuptaDKeoghBChungKFCharacteristics and outcome for admissions to adult, general critical care units with acute severe asthma: a secondary analysis of the ICNARC case mix programme databaseCrit Care200482R112R12115025785
- HanPColeRPEvolving differences in the presentation of severe asthma requiring intensive care unit admissionRespiration200471545846215467322
- RodrigoGJRodrigoCHallJBAcute asthma in adults: a reviewChest200412531081110215006973
- AfessaBMoralesICuryJDClinical course and outcome of patients admitted to an ICU for status asthmaticusChest200112051616162111713143
- MalmströmKKorhonenKKailaMAcute childhood asthma in Finland: a retrospective review of hospital admissions from 1976 to 1995Pediatr Allergy Immunol200011423624011110578
- LeeKHTanWCLimTKSevere asthmaSingapore Med J19973862382409294335
- BramanSSKaemmerlenJTIntensive care of status asthmaticus. A 10-year experienceJAMA199026433663682362333
- Statistics DenmarkStatbank Denmark Available from: http://statbank.dk/statbank5a/default.asp?w=1843Accessed June 25, 2013
- PedersenCBThe Danish Civil Registration SystemScand J Public Health201139Suppl 7222521775345
- LyngeESandegaardJLReboljMThe Danish National Patient RegisterScand J Public Health201139Suppl 7303321775347
- NickelsenTNData validity and coverage in the Danish National Health Registry. A literature reviewUgeskr Laeger200116413337 Danish11810794
- ChristiansenCFChristensenSJohansenMBLarsenKMTønnesenESørensenHTThe impact of pre-admission morbidity level on 3-year mortality after intensive care: a Danish cohort studyActa Anaesthesiol Scand201155896297021770901
- CharlsonMEPompeiPAlesKLMacKenzieCRA new method of classifying prognostic comorbidity in longitudinal studies: development and validationJ Chronic Dis1987403733833558716
- ThygesenSKChristiansenCFChristensenSLashTLSorensenHTThe predictive value of ICD-10 diagnostic coding used to assess Charlson Comorbidity Index conditions in the population-based Danish National Registry of PatientsBMC Med Res Methodol2011118321619668
- GibsonPGMcDonaldVMMarksGBAsthma in older adultsLancet2010376974380381320816547
- FletcherRHFletcherSWDiagnosisFletcherRHFletcherSWClinical Epidemiology: The Essentials4th edPhiladelphiaLippincott Williams and Wilkins20053538
- Wever-HessJKouwenbergJDuivermanEHermansJWeverAPrognostic characteristics of asthma diagnosis in early childhood in clinical practiceActa Paediatr199988882783410503680
- RothmanKJGreenlandSIntroduction to stratified analysisRothmanKJGreenlandSLashTLModern Epidemiology3rd edPhiladelphia, PALippincott Williams and Wilkins2008258282
- PapirisSAManaliEDKolilekasLTriantafillidouCTsangarisIAcute severe asthma: new approaches to assessment and treatmentDrugs200969172363239119911854
- HansenLGAsthma treatment in children: by general practioners and on hospitalsLaegemagasinet20102453338 Danish
- HansenTGJepsenSBPaediatric intensive care in DenmarkUgeskr Laeger20071698687689 Danish17313915
- HigashiAZhuSStaffordRSAlexanderGCNational trends in ambulatory asthma treatment, 1997–2009J Gen Intern Med201126121465147021769507
Appendix materials
Appendix 3 Thirty-day mortality of patients with a first-time status asthmaticus hospitalization, Denmark, 1996–2011. Patients with a registry diagnosis of chronic obstructive pulmonary disease excluded