Abstract
Objectives
We describe several methodological issues that were addressed in conducting a Danish population-based matched cohort study comparing rates of new primary cancers (NPCs) in men with and without prostate cancer (PC).
Methods
We matched 30,220 men with PC to 151,100 men without PC (comparators) on age (±2 years) and PC diagnosis/index date. We focused on several methodological issues: 1) to address survival differences between the cohorts we compared rates with and without censoring comparators on the date their matched PC patient died or was censored; 2) to address diagnostic bias, we excluded men with a history of cancer from the comparator cohort; 3) to address prostate cancer immunity, we graphed the hazard of NPC in both cohorts, with and without prostate cancer as an outcome; 4) we used empirical Bayes methods to explore the effect of adjusting for multiple comparisons.
Results
After 18 months of follow-up, cumulative person-time was lower in the PC than comparator cohort due to higher mortality among PC patients. Terminating person-time in comparators at the matched PC patient’s death or loss to follow-up resulted in comparable person-time up to 30 months of follow-up and lower person-time among comparators thereafter. The hazard of NPC was lower among men with PC than comparators throughout follow-up. There was little difference in rates beyond the first four years of follow-up after removing PC as an outcome. Empirical Bayes adjustment for multiple comparisons had little effect on the estimates.
Conclusion
Addressing the issues of competing risks, treatment interference or diagnostic bias, prostate cancer immunity due to radical prostatectomy, and multiple comparisons lowered the deficit rate of NPCs among men with a history of PC compared with those without PC. However, the differing rates of NPCs may also be due to risk factor differences between the cohorts.
Introduction
There are an estimated 2 million prostate cancer survivors in the US alone.Citation1 This prevalent survivor pool highlights the need for a better understanding of the long-term health of men with prostate cancer, including their risk of new primary cancers. We therefore conducted a Danish population-based cohort study to examine the risk of new primary cancers in men with prostate cancer compared with that in a matched cohort of men with no history of prostate cancer.Citation2 We had to resolve several methodological issues to appropriately compare the rates of new primary cancers in men with and without prostate cancer, and this paper focuses on these issues.
First, competing mortality risks can shorten follow-up time faster and more frequently among prostate cancer survivors than in a comparison cohort free of the disease. The clinical course of prostate cancer and survival vary substantially by stage at diagnosis and geographic region. Prostate cancer is frequently diagnosed at an early stage with a favorable prognosis in countries with population-based prostate specific antigen (PSA) screening, such as the US. Accordingly, many men with prostate cancer in the US die with, rather than from, their prostate cancer.Citation3–Citation6 In contrast, in countries without PSA screening, men are diagnosed more often with clinically relevant prostate cancer at a more advanced stage, and a higher proportion die of the disease.Citation7,Citation8 Therefore differential competing mortality risks should be addressed when comparing new primary cancer rates in prostate cancer survivors with rates in men without this disease, especially in a country such as Denmark, where the prevalence of PSA screening is low.
Second, men with a history of cancer may have a different diagnostic work-up and treatment regimen compared with men without any previous cancer. Therefore, when studying the rate of new primary cancers in men with and without prostate cancer, steps should be taken to minimize the effects of any potential treatment interference or diagnostic bias.
Third, some men diagnosed with prostate cancer receive a radical prostatectomy (complete removal of the prostate) during the course of their primary treatment and so are no longer at risk for a new primary prostate cancer. In addition, almost 90% of prostate cancers are multi-focal at diagnosis.Citation9 Therefore, the recognition and coding of a completely separate second primary cancer within the prostate of a man with a history of prostate cancer is unlikely. As prostate cancer accounts for about 14% of all cancers in men globally,Citation10 men with a history of prostate cancer may appear to have lower rates of any new primary cancer than the background population because they are no longer at risk for prostate cancer itself.
Fourth, multiple comparisons of cancer-specific rates, often within strata of age or clinical variables, can yield false-positive associations.Citation11 Therefore, analytic methods should be implemented to reduce the potential for spurious, but statistically significant, results.
Finally, an imbalance in risk factors, such as smoking, between cohorts may contribute to differences in rates of new primary cancers between cohorts. However, controlling for these risk factors, particularly when relying on registries as a data source, can be beyond the scope of most studies.
This paper focuses on the methods and rationale used to address some of these issues in our comparison of rates of new primary cancers in a matched cohort study of Danish men with and without prostate cancer.
Methods
Study population
We conducted this cohort study among men aged ≥15 years old in Denmark. All health-related services in Denmark are recorded for individual patients using their civil personal registration (CPR) number – a unique identifier encoding sex and date of birth assigned to all Danish residents since 1968. We used the CPR number to link data on an individual level from the Danish Cancer Registry (DCR), Danish National Registry of Patients (DNRP) (covering all Danish hospitals), and the Danish Civil Registration System (CRS).Citation12–Citation14
Prostate cancer cohort
The DCRCitation15 allowed us to identify all men diagnosed with incident prostate cancer (ICD-10 code C61) between January 1, 1978 and December 31, 2003. We excluded men with a history of cancer before their prostate cancer diagnosis (n=3,983). We also excluded men diagnosed with any new primary cancer in the first 4 months after diagnosis (n=600).
Matched comparison cohort
We used the CRS to assemble a matched comparison cohort.Citation12 For each prostate cancer patient, we selected a pool of men from the general population who had similar age (matched ±2 years), county of residence, and no history of any cancer on the index date (date of diagnosis for the corresponding prostate cancer patient). We randomly selected five men per prostate cancer patient from this pool of matched men. We terminated follow-up of members of the comparison cohort when they were diagnosed with prostate cancer (n=699); at which point they joined the prostate cancer cohort. As for the prostate cancer cohort, we excluded any men diagnosed with cancer in the first 4 months after the index date. We also terminated follow-up of members of the comparison cohort upon the death or censorship of their matched prostate cancer patient.
Other study variables
We obtained information on any potentially confounding comorbid diseases from the DNRP (since 1977). These included alcoholism, diabetes, chronic obstructive pulmonary disease (COPD), cardiovascular disease, and obesity. We also computed the Charlson comorbidity score on the prostate cancer diagnosis date for prostate cancer patients and on the index date for the comparison cohort members.Citation16 Cancer was completely removed from the Charlson comorbidity index (including prostate cancer for the prostate cancer cohort).
The DCR and CRS provided information on patient demographics. We also used the DCR to retrieve information on disease characteristics for the members of the prostate cancer cohort (cancer stage and initial treatment of prostate cancer). We stratified patients based on the following calendar periods: 1978–1984; 1985–1996; and 1997–2006. These time periods were selected based on important changes that occurred in prostate cancer treatment in Denmark over time.Citation7,Citation17
Study outcomes
Men were followed from 4 months after their prostate cancer diagnosis/index date until the date of diagnosis of a subsequent cancer and follow-up continued until the date of death, emigration, or 31 December 2006, whichever occurred first, or, for members of the comparison cohort, until censoring or prostate cancer diagnosis. We chose this 4 month cut-off point as the DCR only records cancer-directed treatment up to 4 months after cancer diagnosis date. Ideally we would have started follow-up on the date of completion of prostate cancer treatment.
Statistical analyses
Competing mortality risks and person-time
To examine the impact of the higher death rate in the prostate cancer cohort and the consequently older average age and greater person-time of men in the comparison cohort, we graphed cumulative person-years in both cohorts (dividing by 5 to account for the 5:1 matching of the comparison cohort). We plotted these curves with and without terminating or censoring follow-up of persons in the comparison cohort on the date that their matched prostate cancer patient died or was censored, respectively. Based on these analyses, we chose to terminate members of the comparison cohort from all further analysis when their matched prostate cancer patient died or censor their follow-up on the date their matched prostate cancer patient was censored.
Diagnostic bias
To remove any potential effect of treatment interference or diagnostic bias, we excluded men with a history of cancer from both cohorts.
Immunity from prostate cancer
We graphed the rate of all cancers, calculated in overlapping 4 month windows of follow-up, to examine changes in the approximate cancer hazard in both cohorts over time. We graphed this rate with and without counting cases of prostate cancer in the comparison cohort, to assess whether the difference in rates of new primary cancer was attributable to the impact of “immunity” from incident prostate cancer in the prostate cancer cohort.
Multiple comparisons
We used Cox proportional hazards regression to estimate hazard ratios (HRs) as a measure of the relative risk (RR) of new primary cancers among prostate cancer patients and among men in the comparison cohort, adjusting for comorbidity. We used empirical Bayes methods to adjust for multiple comparisons in the analyses. Empirical Bayes adjustment shrinks individual associations toward the mean of a larger population of associations, in proportion to the ratios of individual variances to the population variance, thereby bringing values with relatively higher variances more toward the central tendency.Citation18 We report comparisons with and without empirical Bayes shrinkage. All statistical analyses were carried out using SAS 9.13 (SAS Institute Inc., Cary, NC, USA).
Results
shows descriptive characteristics of the study population, including patient-, clinical-, and treatment-related factors.
Table 1 Descriptive characteristics of the prostate cancer cohort (n=30,220) and comparison cohort (n=151,100) – excluding men with a history of cancer from both cohorts
Competing mortality risk: person-time in the prostate cancer cohort and comparison cohort
illustrates the cumulative person-time in the prostate cancer and comparison cohorts without terminating or censoring follow-up of men in the comparison cohort at the time of the matched prostate cancer member’s death or loss to follow-up, respectively. Cumulative person-time was similar in both cohorts for the first 18 months of follow-up. Subsequently, cumulative person-time was much lower in the prostate cancer cohort, leveling off within approximately 10 years. In contrast, person-time in the comparison cohort continued to increase up to approximately 15 years after the index date before plateauing.
Figure 1 (A) Cumulative person-time (per 10,000 years) in the prostate cancer cohort and the comparison cohort (adjusted for 5:1 matching). (B) Cumulative person-time (per 10,000 years) in the prostate cancer cohort and the comparison cohort, with censoring of matched persons in the comparison cohort at the time of the prostate cancer patient’s death.
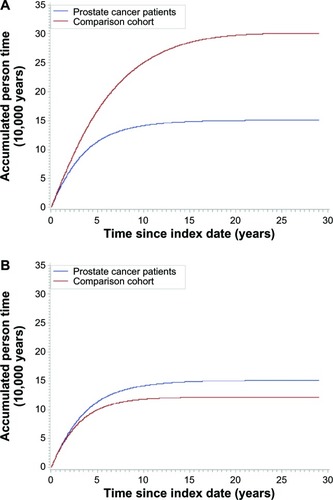
shows person-time in both cohorts with terminating or censoring follow-up of comparison cohort members at the time of the matched prostate cancer member’s death or loss to follow-up, respectively. Person-time was similar for both cohorts during the first 30 months of follow-up. Subsequently, person-time in the comparison cohort was somewhat lower than person-time in the prostate cancer cohort because of terminating or censoring follow-up of the matched persons in the comparison cohort when a man with prostate cancer died or was lost to follow-up. We did not censor follow-up of members of the prostate cancer cohort when a matched person in the comparison cohort died, which explains the small difference in cumulative person-time.
Diagnostic bias
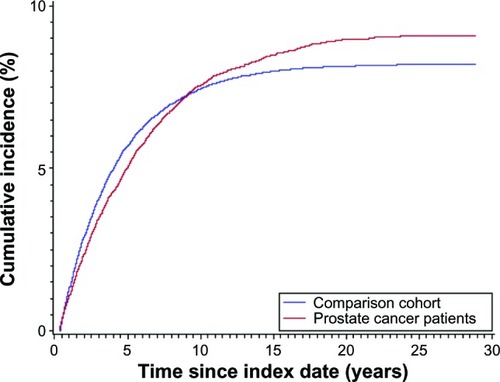
shows the cumulative incidence of new primary cancers in both cohorts excluding men with a history of other cancers. We note that the decreased incidence of new primary cancers in the prostate cancer cohort only persisted for the first 8 to 10 years of follow-up, at which point incidence became higher in the comparison cohort.
Figure 2 Cumulative incidence of new primary cancers in the prostate cancer cohort (n=30,220) and the comparison cohort (n=151,100) (excluding men with a history of other cancers) with terminating or censoring follow-up of the comparison cohort at the death or loss to follow-up of their index man with prostate cancer.
“Immunity” from prostate cancer: hazard of new primary cancer in the prostate cancer and comparison cohorts
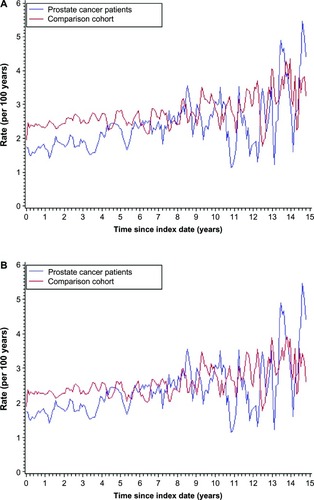
shows the approximate hazard of any new primary cancer, including prostate cancer, in the prostate cancer and comparison cohorts, calculated in sliding and overlapping 4 month windows. shows the rate of new primary cancers in both cohorts excluding prostate cancer as an outcome. For the first four years of follow-up, the rate of new primary cancer was lower in the prostate cancer cohort than in the comparison cohort. Subsequently, there was little difference in the rates of new primaries between the two cohorts.
Figure 3 (A) Rate of new primary cancers in the prostate cancer cohort and comparison cohort, calculated within sliding and overlapping 4 month windows, excluding men with a history of cancer, and including prostate cancer as an outcome. (B) Rate of new primary cancers in the prostate cancer cohort and comparison cohort, calculated within sliding and overlapping 4 month windows, excluding men with a history of cancer, and excluding prostate cancer as an outcome.
Multiple comparisons: empirical Bayes shrinkage methods
and show the HR for new primary cancer in the prostate cancer and comparison cohorts by cancer site, with and without empirical Bayes shrinkage. Shrinkage resulted in a change in the rank order of one cancer site (brain cancer, for which the HR changed from 0.47 to 0.72). As indicated in , there was otherwise little change in the HR estimates between using each of the methods.
Figure 4 Hazard ratios of new primary malignancies in the prostate cancer cohort vs the comparison cohort with and without empirical Bayes shrinkage.
Abbreviation: CI, confidence interval.
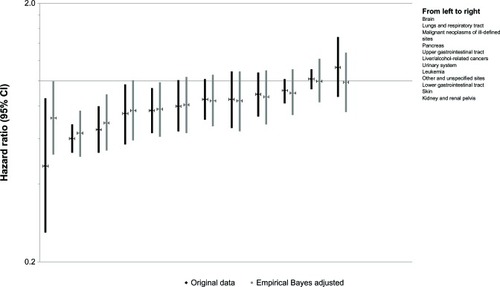
Table 2 Hazard ratio (HR) of a new primary cancer in the prostate cancer cohort vs the comparison cohort, by cancer site. HR with and without empirical Bayes (EB) adjustments for 27 cancer sites, with lower and upper confidence limits (CL)
Discussion
Overall, our analyses found a lower rate of new primary cancers in a cohort of men with prostate cancer compared with a matched cohort of men without prostate cancer. These findings are consistent with a monograph from the US National Cancer Institute, which used Surveillance Epidemiology and End Results (SEER) cancer registry data to describe and quantify the risk of new malignancies among approximately 300,000 prostate cancer survivors in the US.Citation19 However in the current manuscript, we extend this previous research by focusing on epidemiological methods we used to overcome the non-equivalent person-time in the two cohorts, treatment interference/diagnostic bias, prostate cancer “immunity” among men with prostate cancer, and potential multiple comparisons.
The SEER study reported a standardized incidence rate (SIR) of any new primary cancer including and excluding prostate cancer as an outcome (SIR =0.60, and SIR =0.90, respectively). Accordingly, we graphed the approximate hazard with and without prostate cancer as an outcome. Excluding prostate cancer as an outcome reduced the difference in the rate of new primary cancers in the two cohorts, and the lower rate in the prostate cancer cohort persisted only during the first 5 years after prostate cancer diagnosis/index date. These graphs agree with the SEER study findings and suggest that new primary prostate cancers in the comparison cohort may have contributed to the overall deficit of new primary cancers among men with prostate cancer. This deficit is expected, as some men with prostate cancer are treated with radical prostatectomy and therefore are no longer at risk of the disease. In addition, due to the multifocal nature of prostate cancer, a new primary cancer in the prostate may be unlikely to be regarded as a separate cancer to the original prostate cancer.
As the cancer hazard increases with age, the lower rate of new primary cancers among men with prostate cancer may be attributable to less person-time at risk than men without the disease. Evidence of the tendency toward such noncomparability as follow-up time increases comes from our initial analyses (without censoring of the comparison cohort at the time of the matched prostate cancer patient’s death or loss to follow-up), which demonstrated that the initial 5:1 ratio of men matched to prostate cancer patients yielded a 10:1 ratio in person-years by the end of follow-up (data not presented), despite baseline matching on age. This difference resulted from a much higher death rate in the prostate cancer cohort and a progressively older age distribution among men in the comparison cohort. We illustrated this imbalance in person-time between the two cohorts by graphing the cumulative person-time with and without terminating or censoring follow-up of members of the comparison cohort when the corresponding prostate cancer patient died or was lost to follow-up. Based on these graphs, in all subsequent analyses we terminated or censored follow-up of men in the comparison cohort upon the death or loss to follow-up of the corresponding prostate cancer patient. This method allowed us to preserve the age matching and substantially reduced any residual confounding due to age.
The difference in the rate of new primary cancers among men with and without prostate cancer reported in the SEER study lies closer to the null than the difference we observed in this Danish population (0.90, 95% CI =0.89, 0.91 in the SEER study vs 0.84, 95% CI =0.80, 0.88 in our study). There are some plausible reasons for this. First, in our study, terminating or censoring the person-time of the comparison cohort is equivalent to calculating a SIR, as used by SEER.Citation19 A prototypical SIR uses the person-time of the exposed cohort (prostate cancer cohort) and the outcome rates of the unexposed cohort (comparison cohort).Citation20 In many SIR calculations, including that in the SEER study,Citation19 these comparative rates are obtained as age-, sex-, and calendar-specific rates. However, these comparative rates are often based on the whole population, which includes prostate cancer survivors. Since prostate cancer survivors are not rare, the comparison is between a part and the whole, rather than a comparison of two distinct parts (prostate cancer survivors compared with men without a history of prostate cancer). Our design retained the person-time comparability of the SIR method, with the advantage of calculating rates for two non-overlapping populations. Second, although PSA screening has increased on an opportunistic basis in Denmark over the past decade,Citation21 more prevalent PSA screening in the US is likely to contribute to longer average prostate cancer survival in the US compared with Denmark.Citation22 In the US, prostate cancer is somewhat over-diagnosed (PSA screening can uncover clinically irrelevant tumors or benign abnormalities) and represents a mix of aggressive disease with poor survival and relatively latent disease with long survival and a low potential for metastasis.Citation23 If only more aggressive prostate cancer diagnoses are markers of reduced risk for subsequent cancers, then the difference between rates of new primary cancer in prostate cancer patients and men free of this disease in the US population would be diluted given the case mix. This mixing would bias the SEER result towards the null compared with the result in our largely unscreened Danish population.
Removal of prostate cancer as an outcome in both cohorts had a slight effect on the hazard rate of new primary cancers in the two cohorts. This suggests that prostate cancer immunity contributed slightly to the deficit rate of new primary cancers in the prostate cancer cohort.
In studies such as ours, with multiple cancer outcomes, it is important to consider the issue of multiple comparisons, which can lead to undue attention to spurious associations. Consistent with Greenland’s guidelines, we used empirical Bayes shrinkage methods to address the problem.Citation18 The empirical Bayes method reduces the potential for false positive results due to multiple comparisons. With the exception of one cancer site (brain), our findings show similar associations and rankings with and without empirical Bayes adjustment. This insensitivity to adjustment probably stems from large numbers of nearly all cancers in both the prostate cancer cohort and the matched comparison cohort.
Despite our best efforts to address the issues of competing mortality risks, diagnostic bias, prostate cancer immunity, and multiple comparisons, our study showed a substantial difference in the rates of new primary cancer in a cohort of men with and without prostate cancer. This may be a real effect or may be reflective of factors beyond our methodological control. We were unable to assess the influence of cancer-related risk factors, which may have been imbalanced between the two cohorts. For example, men with prostate cancer who smoke are said to have a worse prognosis than non-smokers. We did note a higher rate of chronic obstructive pulmonary disease in the prostate cancer cohort, and accordingly, a higher rate of smoking-related cancers in the comparison cohort.Citation2 This suggests that the true difference in the rate of new primary cancers between the two cohorts is likely to be even smaller than what resulted from our methodological approaches.
Acknowledgments
The study received financial support from Amgen Incorporated, CA, USA and the Department of Clinical Epidemiology Research Fund, Aarhus University Hospital, Denmark.
Disclosure
The authors report no conflicts of interest in this work. Authors K Cetin, A Daniels and J Acquavella are employed by Amgen Incorporated. The Department of Clinical Epidemiology is involved in studies with research grant funding from various other companies that are administered by Aarhus University Hospital. None of these other studies have any relation to the present study.
References
- HornerMRiesLAGKrapchoMSEER Cancer Statistics Review, 1975–2006Bethesda, MD, USA2009 Available from: http://seer.cancer.gov/scr/1975_2006/Accessed January 1, 2013
- Cronin-FentonDPAntonsenSCetinKMortality and incidence of new primary cancers following prostate cancer: A Danish population-based cohort studyCancer Epidemiology201337556256823830884
- FeuerEJMerrillRMHankeyBFCancer surveillance series: interpreting trends in prostate cancer – part II: Cause of death misclassification and the recent rise and fall in prostate cancer mortalityJ Natl Cancer Inst199991121025103210379965
- HankeyBFFeuerEJCleggLXCancer surveillance series: interpreting trends in prostate cancer – part I: Evidence of the effects of screening in recent prostate cancer incidence, mortality, and survival ratesJ Natl Cancer Inst199991121017102410379964
- EtzioniRLeglerJMFeuerEJMerrillRMCroninKAHankeyBFCancer surveillance series: interpreting trends in prostate cancer – part III: Quantifying the link between population prostate-specific antigen testing and recent declines in prostate cancer mortalityJ Natl Cancer Inst199991121033103910379966
- OberaignerWHorningerWKlockerHSchonitzerDStuhlingerWBartschGReduction of prostate cancer mortality in Tyrol, Austria, after introduction of prostate-specific antigen testingAm J Epidemiol2006164437638416829552
- KvaleRAuvinenAAdamiHOInterpreting trends in prostate cancer incidence and mortality in the five Nordic countriesJ Natl Cancer Inst200799241881188718073376
- CarsinAEDrummondFJBlackAImpact of PSA testing and prostatic biopsy on cancer incidence and mortality: comparative study between the Republic of Ireland and Northern IrelandCancer Causes Control20102191523153120514514
- KaravitakisMAhmedHUAbelPDHazellSWinklerMHTumor focality in prostate cancer: implications for focal therapyNat Rev Clin Oncol201181485521116296
- ParkinDMBrayFFerlayJPisaniPGlobal cancer statistics, 2002CA Cancer J Clin20055527410815761078
- RothmanKJNo adjustments are needed for multiple comparisonsEpidemiology19901143462081237
- FrankLEpidemiology. When an entire country is a cohortScience200028754622398239910766613
- AndersenTFMadsenMJorgensenJMellemkjoerLOlsenJHThe Danish National Hospital Register. A valuable source of data for modern health sciencesDan Med Bull199946326326810421985
- PedersenCBGotzscheHMollerJOMortensenPBThe Danish Civil Registration System. A cohort of eight million personsDan Med Bull200653444144917150149
- StormHHMichelsenEVClemmensenIHPihlJThe Danish Cancer Registry-history, content, quality and useDan Med Bull19974455355399408738
- CharlsonMEPompeiPAlesKLMacKenzieCRA new method of classifying prognostic comorbidity in longitudinal studies: development and validationJ Chronic Dis19874053733833558716
- BorreMErichsenRLundLLarsenEHNorgaardMJacobsenJBSurvival of prostate cancer patients in central and northern Denmark, 1998–2009Clin Epidemiol20113Suppl 1414621814469
- GreenlandSRobinsJMEmpirical-Bayes adjustments for multiple comparisons are sometimes usefulEpidemiology1991242442511912039
- McMasterMFeuerEJTuckerMANew Malignancies Following Cancer of the Male Genital TractBethesda, MD, USANational Cancer Institute, NIH2006 NIH Publ No 05–5402
- RothmanKGreenlandSLashTLModern Epidemiology, Third Edition3rd editionPA, USALippincott Williams and Wilkins2008
- BrassoKIngimarsdottirIJThomassenLFriisSIversenP[Prostate cancer in Denmark 1943–2002.] Prostatacancer i Danmark 1943–2002Ugeskr Laeger2007169212913217227660
- HsingAWTsaoLDevesaSSInternational trends and patterns of prostate cancer incidence and mortalityInt J Cancer2000851606710585584
- WelchHGAlbertsenPCProstate cancer diagnosis and treatment after the introduction of prostate-specific antigen screening: 1986–2005J Natl Cancer Inst2009101191325132919720969