Abstract
Objective
Skeletal-related events (SREs) among patients with bone metastases from lung cancer may be associated with considerable use of health care resources. We analyzed in- and outpatient hospital contacts in relation to SREs among all Danish lung cancer patients with bone metastases.
Methods
For this cohort study, we used the Danish Cancer Registry and the Danish National Registry of Patients to identify all persons diagnosed with first-time lung cancer and bone metastases from 2003 through 2009 in Denmark. We followed these patients until December 31, 2010, for the development of SREs (spinal cord compression; pathological or osteoporotic fracture, surgery to bone; or conventional external radiation therapy). We examined the number of inpatient hospitalizations, inpatient bed-days, hospital outpatient clinic visits, and emergency room visits within three time periods: a pre-SRE period (90-day period prior to the diagnostic period), a SRE diagnostic period (14-day period prior to the SRE), and a post-SRE period (90-day period after the SRE).
Results
We identified 1,146 patients with lung cancer, bone metastases, and ≥1 subsequent SRE among 28,443 patients with incident lung cancer. Over 75% of patients with SREs (n=852) had more than one SRE. The number of hospital bed-days was high in the post-SRE period compared to the pre-SRE period, as illustrated by patients with multiple SREs who had 10.7 (95% confidence interval, 10.4–10.9) hospital bed-days per 100 person-days in the pre-SRE period and 28.2 (95% confidence interval, 27.8–28.6) bed-days per 100 person-days in the post-SRE period.
Conclusion
SREs secondary to bone metastases in lung cancer patients are associated with a substantial number of hospital contacts and hospital bed-days.
Introduction
Lung cancer is one of the most common cancers worldwide, accounting for nearly 13% of all incident cancers in 2008.Citation1 It is the leading cause of cancer-related deaths in males and the second leading cause of cancer-related deaths among females. Each year, an estimated 1.6 million patients are diagnosed with lung cancer, and 1.4 million die from this disease.Citation1
Lung cancer in early stages is often asymptomatic, which is why the disease is commonly advanced at the time of diagnosis.Citation2 It has a special propensity to metastasize to bone; bone metastases occur in 30%–40% of patients with lung cancer at some point in the course of their disease.Citation3 For these patients, the risk of subsequent skeletal-related events (SREs) – including severe bone pain requiring radiation therapy; pathological or osteoporotic fractures; spinal cord compression; or bone instability requiring orthopedic surgery – is high.Citation4,Citation5 Approximately half of all lung cancer patients with bone metastases will experience one of these events.Citation5,Citation6 SREs are potentially debilitating complications that negatively affect quality of life and increase morbidity and the need for supportive care in lung cancer patients.Citation7,Citation8 Alongside being a severe physiological and psychological burden to the patients, the economic consequences of SREs secondary to bone metastatic lung cancer are substantial.Citation9
As the treatment landscape for advanced lung cancer continues to evolve, life expectancy for patients with lung cancer will likely increase, and therefore bone metastasis and treatment of SREs may play an even greater role in the future management of these patients.Citation4 To date, few studies have examined the use of hospital resources in lung cancer patients with bone metastasis and SREs,Citation8–Citation10 and we are unaware of any that have investigated and compared the use of hospital resources in adjacent time periods before and after the first SRE in these patients. Such information could provide important information for health care planning. Therefore, we examined the frequency and density of hospital contacts before, during, and after SREs in a cohort of Danish patients with SREs secondary to bone metastases from lung cancer.
Methods
Study design and setting
We conducted this nationwide population-based cohort study in Denmark (population 5.6 million) using prospectively collected data from Danish medical and administrative registries. The Danish health care system provides tax-supported health care to all residents with universal and free access to general practitioners and public hospitals.Citation11 All Danish residents are assigned a unique ten-digit civil registration number at birth or immigration, permitting accurate linkage between all medical and administrative databases.Citation12
Study population
First, we identified incident lung cancer patients registered in the Danish Cancer Registry (DCR) from January 1, 2003 to December 31, 2009. We then restricted the cohort to those who had a diagnosis of bone metastasis registered in the Danish National Registry of Patients (DNRP) in the same time period and who subsequently experienced a SRE before December 31, 2010. The DCR includes data on incident cancers in Denmark since 1943, with mandatory registration since 1987. It records data on patient demographics; tumor site and morphology; and the extent of tumor spread at the time of diagnosis.Citation13 Until 2004, DCR recorded tumor stage as local, regional, or distant (summary staging), and thereafter according to the tumor, nodes, metastasis (TNM) classification. Conversion of TNM classification system to summary staging is presented in Table S1.Citation14 The DNRP includes mandatorily reported data from all hospitals in Denmark, including information on all outpatient and inpatient hospital contacts.Citation15 The DNRP contains data on all non-psychiatric hospital admissions since 1977, and on emergency rooms and outpatient clinic visits since 1995. The registry serves as a basis for reimbursement in the Danish health care system and includes information on patients’ civil registration numbers; dates of admission and discharge; planned versus acute admissions; and hospital and department identification codes. The DNRP also holds clinical information on surgical procedures, major treatments, primary discharge diagnosis (main reason for hospitalization), and up to 19 secondary discharge diagnoses coded by physicians according to the International Classification of Diseases, Eighth Revision from 1977 to 1993, and tenth revision thereafter.Citation15
The Danish Civil Registration System includes data on date of birth, sex, address, changes in vital status, and migration for the entire Danish population since 1968.Citation12
Skeletal-related events
SREs were defined as first date of spinal cord compression; pathological or osteoporotic fracture; surgery to bone; or conventional external radiation therapy.Citation4 We used the DNRP to obtain data on SREs as previously described.Citation16 Relevant codes are presented in Table S2.
Hospital contacts
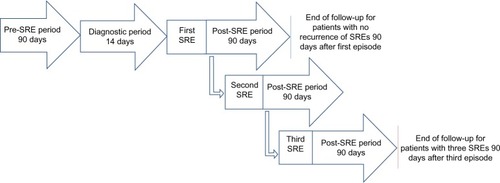
We assessed the number of inpatient hospital admissions, inpatient bed-days, hospital outpatient clinic visits, and emergency room visits using the DNRP. Hospital use was assessed for three observation periods: a pre-SRE period (90 days prior to the diagnostic period), a SRE diagnostic period (14 days prior to the SRE until the diagnosis of first SRE), and a post-SRE period (from the SRE until 90 days after). We defined patients who experienced more than one SRE during the post-SRE period as having multiple SREs and followed them until 90 days after the last SRE ().
Statistical analysis
We described the number of inpatient hospital admissions, inpatient bed-days, hospital outpatient clinic visits, and emergency room visits by frequency, median, and interquartile range (IQR). Each lung cancer patient was followed for development of SREs from date of bone metastasis until December 31, 2010, or death; whichever came first. Furthermore, we computed intensity as the number of hospital contacts per 100 person-days of follow-up according to the number of SREs (1 SRE, >1 SREs) within the three observation periods, and computed corresponding rate ratios comparing the SRE diagnostic period and post-SRE period with the pre-SRE period. The study was approved by the Danish Data Protection Agency.
Results
Among 28,443 patients with lung cancer, we identified 1,668 patients with bone metastasis, of which 1,146 patients had at least one subsequent SRE.
The median age at lung cancer diagnosis was 65.0 years (IQR 58.5–72.4) in patients with bone metastases and SREs, and 57.7% were male (). Most SRE patients (81.2%) had metastatic illness at the time of cancer diagnosis (). Conventional external radiation therapy accounted for the majority of SREs, both in the group of patients having a single SRE and in the group having multiple SREs. Only 24.5% of patients had a single SRE. The median length from first SRE to end of follow-up was 2.3 months (IQR 0.9–3.1) (). A total of 66.3% and 64.6% of patients with single and multiple SREs died in the post-SRE period, respectively. Metastatic illness at other sites was common among lung cancer patients with bone metastasis and at least one SRE. The most common sites for distant metastases were brain (17.1%) and liver (16.1%) ().
Table 1 Descriptive characteristics of 1,147 lung cancer patients with bone metastases and at least one subsequent SRE
The occurrence of an SRE was associated with a high number of hospital contacts. Taking the shorter time window (14 days) into account, there was up to 2.5-times (95% confidence interval [CI], 2.3–2.6) higher intensity of hospital bed-days in the SRE diagnostic period compared with the pre-SRE period, irrespective of the number of SREs (). Similarly, we found 1.8- (95% CI, 1.7–1.9) and 2.6-times (95% CI, 2.6–2.7) higher intensity of hospital bed-days when comparing the post-SRE period with the pre-SRE period for patients with one SRE and patients with multiple SREs, respectively (). The rate of outpatient clinic visits were 1.3- (95% CI, 1.2–1.4) and 2.2-fold (95% CI, 2.1–2.3) higher in the post-SRE period compared to the pre-SRE period for patients with one and multiple SREs, respectively.
Table 2 Hospital use and follow-up time
Patients with multiple SREs generally had a higher number of hospital bed-days compared to those with a single SRE, particularly in the post-SRE period (). For example, the number of inpatient bed-days per 100 person-days was 24.8 (95% CI, 24.0–25.7) days among patients with a single SRE and 28.2 (95% CI, 27.8–28.6) days among patients with multiple SREs.
Discussion
Key findings
In this nationwide cohort study of 1,146 patients with lung cancer, bone metastases, and subsequent SREs, we observed substantial hospital use in relation to SREs. SREs were associated with an increased frequency of hospital contacts and a greater number of hospital days in the SRE diagnostic period and post-SRE period compared to the pre-SRE period, irrespective of the number of SREs during the post-SRE period.
Strengths and limitations
The main strengths of our study include its large size, complete follow-up, high-quality medical databases, and the nationwide population-based design in a country with a uniform tax-supported health care system. Together, this reduced the potential information bias. Still, some limitations should be considered when interpreting our results. First, our findings are limited by the study’s reliance on diagnosis codes in the DNRP to identify bone metastases and SREs. Although the coding of bone metastases and SREs secondary to lung cancer has not yet been validated, a Danish study validating codes of bone metastases or SREs in relation to breast and prostate cancer showed that these conditions are under-recorded in the DNRP.Citation17 For example, for prostate cancer, the sensitivity of bone metastases and/or SRE coding was 54% (95% CI, 39–69) and the specificity was 96% (95% CI, 87–100).Citation17 Therefore, underreporting of bone metastases and/or SREs might have caused some selection bias if hospital contacts differed among patients registered and those not registered. Second, we were not able to distinguish between hospital contacts for SRE and non-SRE reasons, and so the utilization we report here may not exclusively reflect SRE-mediated hospital contacts. Other factors such as tumor stage at diagnosis, other metastatic sites, age, civil status, and general health status may influence the use of hospital bed-days. As our aim was to describe hospital use, we did not take into account patient differences and consequently cannot draw any conclusions regarding causality. However, the comparison of hospital use in adjacent time periods before and after the SRE minimizes this problem. Third, we did not include comprehensive data on health resource utilization, and there may be considerable costs associated with hospital medication use and procedures not included. Furthermore, we did not analyze hospital use by type of SRE. Consequently, we may not have fully elucidated the total use of hospital resources in our study population. Fourth, our results may not be directly applicable to other and more heterogeneous health care systems.
Other studies
To our knowledge, no other studies have investigated and compared the use of hospital resources in adjacent time periods before and after the first SRE in patients with bone metastasizing lung cancer. Our results are in concordance with other studies examining the hospital burden and costs of SREs in relation to bone metastases from lung cancer.Citation8–Citation10 However, SREs as a composite endpoint may be underestimated compared to other studiesCitation9,Citation10 because hypercalcemia of malignancy was not included in our definition of SRE. In a Spanish cohort study, Pockett et al investigated the hospital burden of disease associated with bone metastases and SREs following breast, lung, and prostate cancer during 2003. They found that lung cancer patients with bone metastases and subsequent SREs had markedly longer inpatient lengths of stay (32 days) compared to patients with lung cancer only (15 days) or lung cancer with bone metastases only (22 days).Citation8 In a propensity-score matched cohort study, Delea et al estimated the impact of SREs on total medical costs for patients with bone metastases from lung cancer by investigating a US health insurance claims database in the period from 1994 to 2002. They found that the difference in total costs were $27,982 (95% CI, 15,921–40,625) in patients with at least one SRE compared with matched patients without an SRE.Citation9 In a French multicenter cohort study from May 2006 to May 2007, Decroisette et al investigated the consumption of health care resources (eg, cost of hospitalization and medication) among patients with bone metastases from lung cancer. They found that the mean monthly costs of metastatic bone disease were €190, €374, and €4,672 for asymptomatic patients, symptomatic patients, and patients with an SRE, respectively.Citation10
Conclusion
SREs in lung cancer patients with bone metastases are associated with substantial hospital resource use. These data may prove useful to health care planning as therapies for advanced lung cancer improve and more lung cancer patients are living with bone metastases and SREs.
Acknowledgments
Funding was provided by a research grant to Aarhus University from Amgen Inc.
Disclosure
KC is an employee of Amgen Inc. None of the other authors report receiving fees, honoraria, grants or consultancies from Amgen, but are former (KSD, CS) and current (HG, CFC) employees at the Department of Clinical Epidemiology, Aarhus University Hospital, Aarhus, Denmark. The department receives funding from various companies (including Amgen Inc.) as research grants to and administered by Aarhus University. The authors report no other conflicts of interest in this work.
References
- JemalABrayFCenterMMFerlayJWardEFormanDGlobal cancer statisticsCA Cancer J Clin2011612699021296855
- HirshVSkeletal disease contributes substantially to morbidity and mortality in patients with lung cancerClin Lung Cancer200910422322919632938
- Al HusainiHWheatley-PricePClemonsMShepherdFAPrevention and management of bone metastases in lung cancer: a reviewJ Thorac Oncol20094225125919179905
- BrodowiczTO’ByrneKManegoldCBone matters in lung cancerAnn Oncol20122392215222222357445
- OsterGLameratoLGlassAGNatural history of skeletal-related events in patients with breast, lung, or prostate cancer and metastases to bone: a 15-year study in two large US health systemsSupport Care Cancer201321123279328623884473
- SathiakumarNDelzellEMorriseyMAMortality following bone metastasis and skeletal-related events among patients 65 years and above with lung cancer: A population-based analysis of US Medicare beneficiaries, 1999–2006Lung India2013301202623661912
- CostaLBadiaXChowELiptonAWardleyAImpact of skeletal complications on patients’ quality of life, mobility, and functional independenceSupport Care Cancer200816887988918392862
- PockettRDCastellanoDMcEwanPOglesbyABarberBLChungKThe hospital burden of disease associated with bone metastases and skeletal-related events in patients with breast cancer, lung cancer, or prostate cancer in SpainEur J Cancer Care (Engl)201019675576019708928
- DeleaTEMcKiernanJBrandmanJImpact of skeletal complications on total medical care costs among patients with bone metastases of lung cancerJ Thorac Oncol20061657157617409919
- DecroisetteCMonnetIBerardHEpidemiology and treatment costs of bone metastases from lung cancer: a French prospective, observational, multicenter study (GFPC 0601)J Thorac Oncol20116357658221270669
- Ministry of Health and PreventionHealth Care in DenmarkCopenhagen: Ministry of Health and Prevention2008 Available from: http://www.sum.dk/Aktuelt/Publikationer/~/media/Filer%20-%20Publikationer_i_pdf/2008/UK_Healthcare_in_dk/pdf.ashxAccessed June 15, 2015
- PedersenCBThe Danish Civil Registration SystemScand J Public Health2011397 Suppl222521775345
- GjerstorffMLThe Danish Cancer RegistryScand J Public Health2011397 Suppl424521775350
- OrdingAGNielssonMSFrøslevTFriisSGarneJPSøgaardMCompleteness of breast cancer staging in the Danish Cancer Registry, 2004–2009Clin Epidemiol20124Suppl 2111622936852
- LyngeESandegaardJLReboljMThe Danish National Patient RegisterScand J Public Health2011397 Suppl303321775347
- SvendsenMLGammelagerHSværkeCHospital visits among women with skeletal-related events secondary to breast cancer and bone metastases: a nationwide population-based cohort study in DenmarkClin Epidemiol201359710323576882
- JensenAØNørgaardMYongMFryzekJPSørensenHTValidity of the recorded International Classification of Diseases, 10th edition diagnoses codes of bone metastases and skeletal-related events in breast and prostate cancer patients in the Danish National Registry of PatientsClin Epidemiol2009110110820865091