Abstract
Objective
We aimed to summarize the pooled frequency of mediastinitis following open-heart surgery caused by Gram-positive bacteria, including methicillin-resistant Staphylococcus aureus (MRSA), and Gram-negative bacteria.
Design
This study was a systematic review and a meta-analysis of prospective and retrospective cohort studies.
Materials and methods
We searched the literature, and a total of 97 cohort studies were identified. Random-effect model was used to synthesize the results. Heterogeneity between studies was examined by subgroup and meta-regression analyses, considering study and patient-level variables. Small-study effect was evaluated.
Results
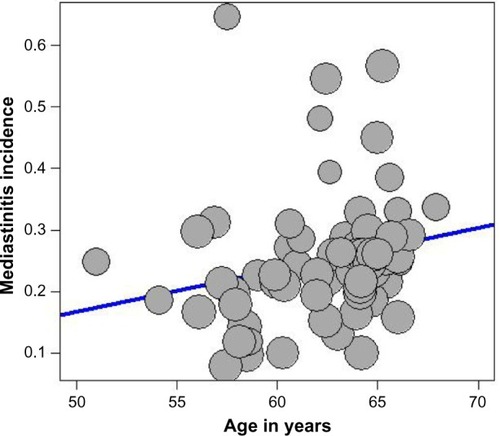
Substantial heterogeneity was present. The estimated incidence of mediastinitis evaluated from 97 studies was 1.58% (95% confidence intervals [CI] 1.42, 1.75) and that of Gram-positive bacteria, Gram-negative bacteria, and MRSA bacteria evaluated from 63 studies was 0.90% (95% CI 0.81, 1.21), 0.24% (95% CI 0.18, 0.32), and 0.08% (95% CI 0.05, 0.12), respectively. A meta-regression pinpointed negative association between the frequency of mediastinitis and latitude of study place and positive association between the frequency of mediastinitis and the age of the patient at operation. Multivariate meta-regression showed that prospective cohort design and age of the patients and latitude of study place together or in combination accounted for 17% of heterogeneity for end point frequency of mediastinitis, 16.3% for Gram-positive bacteria, 14.7% for Gram-negative bacteria, and 23.3% for MRSA bacteria.
Conclusion
Evidence from this study suggests the importance of latitude of study place and advanced age as risk factors of mediastinitis. Latitude is a marker of thermally regulated bacterial virulence and other local surgical practice. There is concern of increasing risk of mediastinitis and of MRSA in elderly patients undergoing sternotomy.
Keywords:
Introduction
The reported incidence of mediastinitis after coronary artery bypass grafting (CABG) is 0.4%–4%.Citation1 Mediastinitis is associated with increased morbidity, mortality, and cost.
The etiology and pathophysiology of mediastinitis are complex and multifactorial. Also, mediastinitis carries an excess of long-term risk of mortality over 10 years of follow-up.Citation1,Citation2
The variability of incidence of mediastinitis in the literature is due to different study designs, population of patients, surgical cardiac procedures, and geographical area of the world with climate and latitude differences. We know that the latitude where the study took place is an important marker for variation in rainfall, humidity, temperature, and environmental mycobacteria that may alter the natural immunity and other factors. Latitude is associated with intensity and duration of sun exposure. Also, ambient temperature and latitude are strongly correlated.Citation3 Previous studies have used latitude of study site as proxy for ambient temperature and environmental mycobacteria.Citation4,Citation5 We used the same method to assess the etiological role of ambient temperature and mycobacteria on the incidence and microbiology of Helicobacter pylori in a systematic review combined with meta-analysis of the literature.Citation6 This systematic review considered worldwide studies of incidence and microbiology of mediastinitis after open-heart surgery.
Materials and methods
Literature search
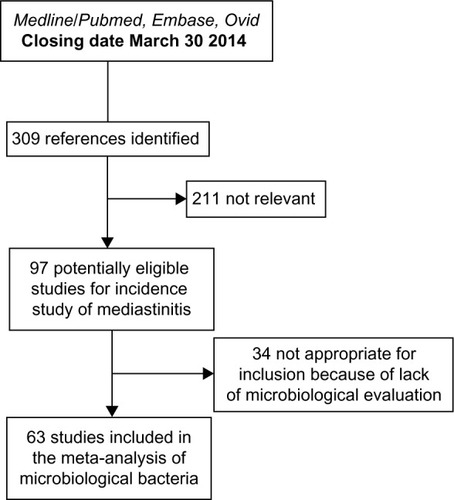
A qualified medical librarian of Medical Library, Oslo University Hospital, was consulted. We searched the Cochrane Central Register of Controlled Trials (1970–2014), Medline/PubMed (1966–2014), and Embase (1980–2014) databases. We used a combination of keywords and details of the search procedure as shown in the Supplementary materials. We used similar strategies to identify previously published meta-analyses and reviews. In addition, we manually searched conference proceedings and textbooks, screened reference lists of all papers, and contacted investigators, experts, and translators. The last update for research was done on August 8, 2014. No limitation on language was considered ().
Study selection
We included prospective and retrospective studies on patients with open-heart surgery coronary artery bypass graft (CABG and valve replacement). Two reviewers independently evaluated reports for eligibility criteria defined as cohort of open-heart surgery patients operated in different centers of the world. Finally, 97 cohorts were considered eligible for the incidence studyCitation1,Citation7–Citation102 and 63 of them were considered for microbiological incidence of Gram-positive cocci and Gram-negative bacilli and fungi.
Quality assessment of the cohort studies: the component approach
Unfortunately, there is no agreed “gold standard” appraisal tool for evaluating quality in observational epidemiologic studies, and there are many tools from which to choose. For the purpose of critically appraising cohort studies, we used a checklist based on recommendations by Elwood,Citation103 including: a) methods for selecting study participant; b) directionality of the cohort, prospective versus retrospective; and c) enough power to catch the true incidence. The poor reporting on important methodological details may be due to the fact that most papers were published before the STROBE statements.Citation104 Sanderson et alCitation105 evaluated a large number of tools for assessing quality of observational epidemiological studies, recommending a simple checklist, including a small number of key domains being specific to the study design under consideration rather than a scale. Scales resulting in numerical summary of quality scores might look simple to use, but such an approach can introduce a bias when assessing study quality.Citation106
Data abstraction
Data regarding publication status, study design, patient-related characteristics, outcome methods, and results and funding were extracted in duplicate on a standardized form according to an a priori protocol. Authors were contacted for additional data and corrections. Disagreements were resolved by discussion with a third reviewer and subsequent consensus. Patient-related variables were considered in the protocol and included mean age of the cohort, frequency of female sex, and frequency of CABG surgery. The study-level variables included the nature of the cohort, prospective versus retrospective; latitude and longitude of the place of the study, year of publication, and the presence of adequate power. The adequate power was based on the total incidence of deep sternal wound infection (DSWI).
Of the 97 studies, the observed median incidence was 1.5% and the lower and higher quartile were 0.70% and 2.3%, respectively. Considering the median of 1.5% and accepting a precision of 0.8% (half the interquartile range), we will need a cohort of at least 887 patients to have a 95% probability to catch this incidence.
End points considered
The primary end point was the incidence of mediastinitis infection. The diagnosis of post sternotomy mediastinitis was based on the criteria established by the Centres for Disease Control and Prevention. We know that according to Centres for Disease Control and Prevention, surgical site infections can be classified into three categories: superficial incisional sternum superficial infections (SSIs; involving only skin and subcutaneous tissues), deep incisional SSIs (involving deep soft tissue), and organ/space SSIs (involving any part of the body other than the incision itself), which is opened or manipulated during the operative procedure. The definition of mediastinitis must meet at least one of the following criteria: 1) positive bacterial culture from the mediastinal space; 2) evidence of mediastinitis during surgery or histology; or 3) one of the following: fever (>38°C), chest pain, sternal instability, purulent discharge from the mediastinal area, organisms cultured from blood or from discharge of the mediastinal area, or mediastinal widening in radiology.
Unfortunately, in the literature, various terms for chest SSIs have been used, including sternal infection, deep sternal infection, and major infection. The inconsistent definitions could create misclassification of mediastinitis.
Secondary end points were the incidence of different microorganisms recovered in mediastinitis secondary to cardiovascular surgery. They included: 1) Gram-positive cocci (Staphylococcus aureus including methicillin- resistant S. aureus [MRSA], Staphylococcus epidermis, and Enterococcus spp); 2) Gram-negative bacilli (Esherichia coli, Enterobacter spp., Klebsiella spp., Proteus spp., and other Enterobacteri-aceae and Pseudomonas spp.); 3) fungi (Candida albicans and others); and 4) polymicrobial mediastinitis (mixed Gram-positive and Gram-negative organisms account for >10%). Other microorganisms were occasionally reported.
Quantitative data synthesis
Statistical pooling
Random-effects meta-analysis of single proportions was considered to estimate a cumulative incidence. The DerSimonian–Laird estimateCitation107 is used in the random-effects model. To obtain summary measures, we used random-effects model due to the large heterogeneity of the results. To pool the incidence measures, logit transformation and sometimes logarithm transformation were initially performed to handle the distribution asymmetry. Sometimes, we considered the Freeman-Tukey double arcsine transformation of the proportions to calculate an overall pooled proportion and to stabilize the variance.Citation108 These incidences were weighted by the inverse variance. When using the logit transformation, a continuity correction was applied if any studies had a zero cell count. By default, 0.5 is added to all cell frequencies of studies with a zero cell count. For individual studies, the Clopper-Pearson confidence interval was estimated.Citation109
Sources of heterogeneity, evaluation, and quantification
Statistical heterogeneity among studies was assessed with Cochran’s Q test. The magnitude of heterogeneity was evaluated by the I2 statistics, which describes the proportion of total variation due to heterogeneity rather than chance.Citation110 In order to investigate possible sources of heterogeneity, two different methods were used: subgroup analyses and meta-regression. We stratified our data according to the following study characteristics: nature of the cohort, prospective versus retrospective, and presence of a priori power estimation for the study.
A random-effects model was used to combine subgroups with separate estimate of τ2.Citation110 After doing the subgroup analyses, we ran a random-effect meta-regression analysis, where the outcome variable was the transformated observed incidence from every study, indicating effect and study-level and patient-level characteristics (covariates). This random-effect regression model was done to enable exploration of the source of heterogeneity in the association between incidence of DWSI and covariates. The mixed model is an extension of the random-effect model. In this model, some heterogeneity is explained by moderators (covariates) and the rest by the random-effect term.
Publication bias or small-study effect
In order to assess potential publication bias or small-study effect, we used the funnel plot, which is a good visual evaluation of sampling bias or small-study effect.
Begg and Mazumdar rank correlation test
Begg and MazumdarCitation111 suggested a test statistics based on rank correlation between standardized outcome estimates and variance estimates of estimated outcome effect. Kendall’s tau is used as a correlation measure. The test statistics follows a standard normal distribution.
Egger’s test of asymmetry
Another test of asymmetry (Egger’s test)Citation112 applied on the funnel plot was performed. The test statistics is based on a weighted linear regression of the treatment effect on its standard error. The test statistics follows a normal distribution with number of studies −2 as degrees of freedom. Nowadays, Egger’s test is mostly seen as a test of small-study effects.
Detection and correction for publication bias/small-study effect using the trim and fill method
Publication bias is a serious issue, as it may lead to biased estimates, which appears to be precise. A popular method for detecting and adjusting bias is the trim and fill method.Citation113 When there is substantial heterogeneity, the trim and fill method is inappropriate to control for publication bias.Citation114
Power considerations in meta-analysis and meta-regression
The test of funnel plot asymmetry and meta-regression analysis can be used only when at least ten studies are included in the meta-analysis because of power limitations. As underlined by Borenstein et alCitation110 under the fixed model, the number of subjects in the studies and the effect size we need to pinpoint determine the power of the meta-analysis. Under the random-effect model, power is a function of not only the total number of subjects but also the number of studies, the effect size, and the variance between studies (heterogeneity).
For power consideration, we used a minimum of ten studies per covariate in a multivariate model of meta-regression. On the other hand, it is well known that aggregate variables (patient-related variables) are subject to ecological fallacy and must be considered only as hypothesis generating.
All statistical analyses were performed using the R package metaCitation115 and Stata 13.0.Citation116 We have followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines for meta-analyses and systematic reviews of observational studies in the present report.Citation117
Results
Trial flow
After identifying 309 references, 211 were excluded due to irrelevant content and duplicate publications, leaving 97 potentially eligible studies for incidence of mediastinitis. From these 97 eligible studies, 63 studies had microbiological evaluation. Finally, 97 studies were included in our systematic review of incidence and 63 for microbiological specific bacteria ().
Study characteristics
The study characteristics considered were the place and latitude of the study, the year of publication, the mean age of the study population, frequency of female patients, frequency of isolated CABG, the prospective or retrospective nature of the cohort design, and the adequacy of power of the study.
End point total incidence of DSWI or mediastinitis
A total of 1,420,845 patients were included in the 97 studies, and the number of patients with DSWI or mediastinitis was 13,662. The mean age was 62.24 years (n=61 studies) with a range from 51 years to 67.9 years. The frequency of female patients was 28.2% with a range from 1% to 75% (n=68 studies). Mean frequency of CABG was 81.1% (n=61 studies) with a range from 36.6% to 100%. For the study-level characteristics, all the studies had a cohort design with 59 prospective and 48 retrospective. Of the total 97 (85.7%) studies, 84 were adequately powered.
End point bacteriology (incidence of microorganisms)
Only 63 of 97 studies have performed microbiological analysis and reported their results. Considering these studies, the number of patients included was 306,440 and the number of microorganisms (bacteria and fungi) was 3,724. The total number of Gram-positive cocci was n=2,958 (77.3%), including 343 MRSA microorganisms. Gram-negative bacilli represented 733 microorganisms, and the number of fungi infections was 33 ().
Table 1 Incidence of microorganisms recovered in mediastinitis secondary to cardiothoracic surgery with frequency in 63 cohort studies
Quantitative data synthesis
End point incidence of DSWI (mediastinitis) in 97 studies worldwide
The summarized pooled estimate incidence of DSWI in the 97 studies using the random-effect model was 0.0158 (95% CI 0.0142–0.0175) with a substantial heterogeneity ( and ).
Table 2 Estimate of incidence of mediastinitis with stratification on prospective nature and power of the cohort and on latitude of the study place using the random-effect model
Table 3 Meta-regression between incidence of mediastinitis and the different study-level and patient-level variables in a univariate analysis
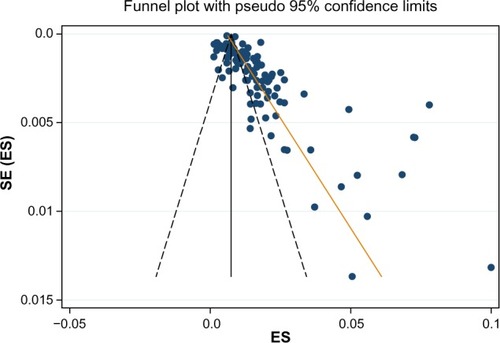
The funnel plot in visually showed evidence of bias and small-study effect. This was verified using Begg and Mazumdar rank correlation test and confirmed by the Egger’s test, which had a P-value of 0.001 accepting the null hypothesis of small-study effect. Because of substantial heterogeneity, we did not correct for selection bias considering the trim and fill simulation method.
Figure 2 A funnel plot for the incidence of mediastinitis in 97 studies with Egger line.
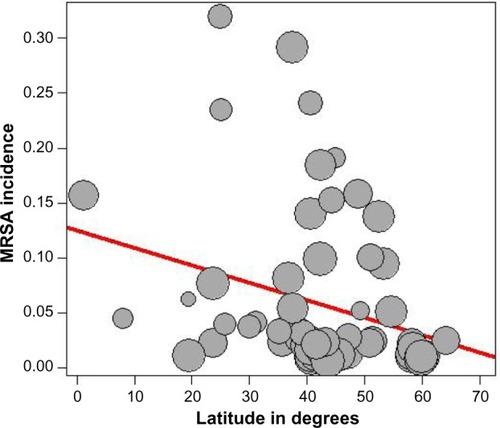
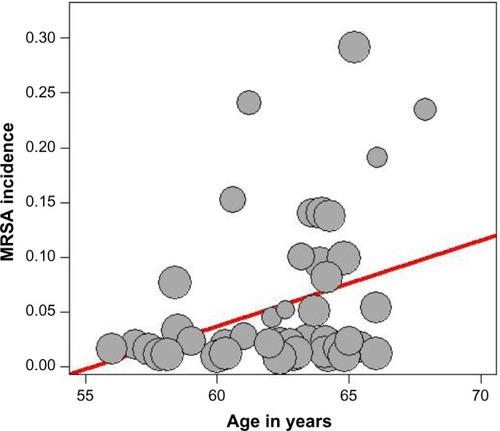
The presence of heterogeneity led us to an investigation of its origin. A stratification analysis on the prospective versus retrospective nature of the cohorts, the adequacy of powered studies versus power-deficient studies, and the median latitude of the place of the studies showed a significant difference between subgroups. We extended the analyses with a meta-regression model taking into account moderator variables such as mean age, frequency of CABG in the total open-heart surgery, frequency of female patients, and latitude. One important study-level variable identified was latitude () with decreasing incidence of mediastinitis with increasing latitude. There was an increasing incidence of DSWI with the increasing age of patient at sternotomy ().
Figure 3 Meta-regression of incidence of mediastinitis and latitude of study place.
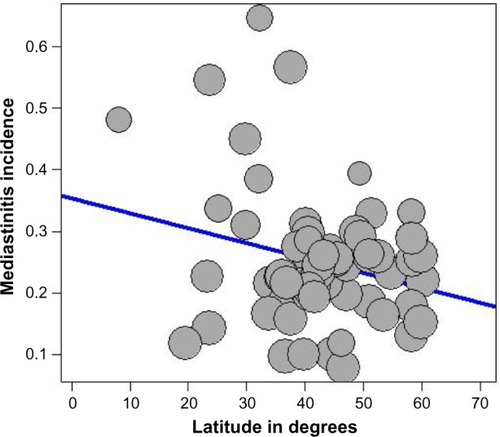
Figure 4 Meta-regression of incidence of mediastinitis and mean age of the patient.
A multivariate meta-regression was performed, which considered study-level and patient-level variables together. This, using random- and mixed-effect models, identified the presence of prospective design, age of the patient, and the latitude of the study as risk factors of DSWI, with 17% of heterogeneity accounted for by these three variables together.
End points incidence of microorganisms recovered in mediastinitis
Gram-positive cocci
and summarize the pooled estimate incidence of Gram-positive cocci in 63 studies using the random-effect model. The incidence was 0.009, 95% CI (0.0081–0.0121), with a substantial heterogeneity. The funnel plot visually showed evidence of bias and small-study effect. This was confirmed by the Begg and Mazumdar rank correlation test (P=0.018) and by the Egger’s test, which had a P-value of 0.006 accepting the null hypothesis of small-study effect or selection bias. Because of substantial heterogeneity, we did not correct for selection bias considering the trim and fill simulation method.
Table 4 Estimate of incidence of Gram-positive cocci with stratification on prospective nature of the cohort and latitude of the study place using the random-effect model
Table 5 Meta-regression model between incidence of Gram-positive cocci and the different study-level and patient-level variables in a univariate analysis using the 63 cohorts
The presence of heterogeneity led us to an investigation of its origin. A stratification analysis on the prospective versus retrospective nature of the cohort and the median latitude of the place of the study showed a significant difference between subgroups. When we extended the analyses with a mixed-effect meta-regression model, one important patient-related variable was identified: age of the patient at sternotomy, with increasing incidence of Gram-positive cocci with increasing age. A multivariate meta-regression was performed, which considered study-level and patient-level variables together. The multivariate mixed-effect model identified age and the prospective nature of the cohort as risk factors of Gram-positive cocci with 16.3% of heterogeneity accounted for by these two variables together.
Methicillin-resistant S. aureus
and summarize the pooled estimate incidence of MRSA in 63 studies using the random-effect model. The incidence was 0.0008, 95% CI (0.0005–0.0012), with a substantial heterogeneity. The funnel plot visually showed evidence of bias and small-study effect. This was confirmed by the Begg and Mazumdar rank correlation test with continuity correction (P=0.0007) and by the Egger’s test, which had a P-value of 0.0128 accepting the null hypothesis of small-study effect or selection bias. Because of substantial heterogeneity, we did not correct for selection bias considering the trim and fill simulation method.
Table 6 Estimate of total incidence of MRSA with stratification on prospective nature of cohort and latitude of the study place using the random-effect model
Table 7 Meta-regression model between incidence of MRSA and the different study-level and patient-level variables in a univariate analysis using the 63 cohorts
The presence of heterogeneity led us to an investigation of its origin. A stratification analysis on the prospective versus retrospective nature of the cohort and the median latitude of the place of the study showed a significant difference between subgroups. When we extended the analyses with a mixed-effect meta-regression model, one important study-level variable was identified: the latitude of the place of the study, with decreasing incidence of MRSA with increasing latitude (). Also, we identified increasing incidence of MRSA with increasing age of the patients (). A multivariate meta-regression was performed, which considered study-level and patient-level variables. The multivariate using mixed-effect meta regression model identified latitude and age of the patient as independent risk factors of MRSA with 23.13% of heterogeneity accounted for by these two variables together.
Gram-negative bacilli
and summarize the pooled estimate incidence of Gram-negative bacilli in 63 studies using the random-effect model. The incidence was 0.0024, 95% CI (0.0018–0.032), with a substantial heterogeneity. The funnel plot visually showed evidence of bias and small-study effect. The Begg and Mazumdar rank correlation test confirmed this with continuity correction (P=0.037) and by the Egger’s test, which had a P-value of 0.00061 accepting the null hypothesis of small-study effect or selection bias. Because of substantial heterogeneity, we did not correct for selection bias considering the trim and fill simulation method.
Table 8 Estimate of total incidence of Gram-negative bacilli with stratification on prospective nature of cohort and latitude of the study place using the random-effect model
Table 9 Meta regression model between incidence of Gram-negative bacilli and the different study-level and patient-level variables in a univariate analysis using the 63 cohorts
The presence of heterogeneity led us to an investigation of its origin. A stratification analysis on the prospective versus retrospective nature of the cohort and the median latitude of the place of the study showed a significant difference between subgroups. When we extended the analyses with a mixed-effect meta-regression model, one important study-level related variable was identified: the latitude of the place of the study, with decreasing incidence of Gram-negative bacilli with increasing latitude. A multivariate meta-regression was performed, which considered study-level variables also. The multivariate mixed-effect regression model identified latitude and the prospective nature of the cohort as risk factors of Gram-negative bacilli with 14.7% of heterogeneity accounted for by these two variables together.
Discussion
Our systematic review and meta-analysis of cohorts estimating incidence of DSWI and incidence of different microorganisms after sternotomy showed a high degree of heterogeneity among cohorts for all the outcomes. Also, publication bias or small-size effect was found to influence the outcomes. Meta-regression analyses indicated that heterogeneity could be explained by patient-related variables and study-level characteristics. For studies reporting on DSWI, the latitude of the study place and age of the patients were important determinants of incidence of this complication. Our results do not support the importance of CABG compared with valve replacement or sex of the patients as associated with incidence of DSWI. Determinants of Gram-positive cocci, including MRSA and Gram-negative bacilli microorganisms, are different. Also, latitude of the study place and age of the patients were determinants for the incidence of MRSA.
Strengths and limitations
Our review is based on a broad literature search, and it seems unlikely that we have missed relevant studies. Study selection and data extraction, including data assessment, were done by two authors to minimize bias and transcription errors.Citation118 The major limitation of our study is the quality of cohort studies; it is clear that there is bias introduced by retrospective cohort design. The prospective cohorts showed higher incidence of mediastinitis and specific microorganisms. In the retrospective cohort studies, the accuracy of the parameters recorded and the quality of wound surveillance are therefore variable. The second problem is a misclassification of the end points DSWI, with some studies pooling DSWIs with infections at other sites, superficial sternal wound infections, or sternal and mechanical complications. Most importantly, all these studies are from different centers. It is likely that selection of patients, choice of procedures, and management of the perioperative period vary greatly among cardiac surgical units. These parameters, although difficult to record, may be important determinants of DSWI. Prospective multicentre studies would ascertain DSWI and identify high-risk patients and procedures and protect cohorts against attrition bias (dropout and loss to follow-up). Another limitation was the impossibility to control the small-study effect due to substantial heterogeneity. Finally, underpowered designed cohorts represented another limitation of our study.
Problem of heterogeneity due to patient-level and study-level variables on the incidence of mediastinitis and specific microorganisms
Latitude of the place of the study and temperature-regulated bacterial virulence
Latitude of the study site is a proxy and marker of rainfall, humidity, and environmental mycobacteria that may alter the natural immunity. Latitude and temperature are correlated.Citation4
As it was underlined by Shapiro and CowenCitation119 for diverse microbial species including viruses, bacteria and fungi temperatures represent a critical environmental factor that is well established. It has been known for some time that temperature is a critical environmental trigger for many bacterial species.Citation119
Also, temperature influences developmental transitions in the human fungal pathogen C. Albicans’s morphogenetic transition between yeast and filamentous growth and resistance to antifungal drugs.
Eber et al,Citation120 with data from 132 US hospitals in the period 1999–2006, found that summer season and higher mean monthly outdoor temperature were associated with substantial increases of bloodstream infection. There were increases in monthly count of S. aureus including MRSA and other Gram-negative bacteria such as E. coli and Acinetobacter. This study focused on blood culture to ensure that blood culture reflects infection and not merely colonizing organisms and that the association is with monthly bacterial count and monthly mean temperature, total precipitation, and mean relative humidity. There are several potential explanations of frequency of bacterial bloodstream infections compared with outdoor temperature levels. First, relatively higher temperatures not >37°C may facilitate increased growth of bacteria in the environment, which may, in turn, increase colonization of humans.
Mechanisms of bacterial growth and optimal growth temperature vary by organism, which may explain the observed difference in association with outdoor temperature between organisms.
Investigators Mermel et alCitation121 have observed peaks of community-associated MRSA during summer and autumn and its association with seasonal skin infections. It is well known that each infection agent has an optimal temperature for growth; most grow best at temperature close to 37°C, and too low or too high temperature will not promote growth. Sahoo et alCitation122 in a time series analysis showed that a combination of weekly average maximum temperature above 33°C coinciding with weekly average relative humidity ranging between 55% and 78% is most favorable for occurrence of skin and soft tissue infections due to S. aureus and MRSA, and within these parameters, each unit increase in occurrence of MRSA was associated with increase in weekly average temperature of 1.7°C and weekly average relative humidity of 10%.
Another experimental work done by Madiraju et alCitation123 challenging MRSA strains in exponential phase cultures by methicillin observed that growth and peptidoglycan synthesis were much more resistant at 30°C than 40°C.
Latitude of the study place as a marker of surgical and other local practices
The latitude of the place of the study is a marker of operating room practices in open-heart surgery. Surgical procedures as risk factors of mediastinitis were investigated extensively by Eklund et al.Citation27 The risk of infection in the operating theater is dependent on a lot of factors. One of them the beneficial effect of a preoperative antiseptic shower for reducing the microbial colony count on the patient’s skin is still controversial on lowering the infection rate.Citation124 Shaving the hair from the incision site, especially the night before surgery, is still controversial.Citation72,Citation125 A Cochrane collaboration review in 2011Citation126 concluded that when it is necessary to remove hair, the existence evidence suggests that clippers are associated with fewer surgical site infections than razors.
In diabetic patients, during cardiopulmonary bypass, a peak core body temperature >37.9 C could increase the risk of mediastinitis postoperatively as underlined by Groom et al.Citation127
The air contamination control in the operating roomCitation128 is important as contamination of the sternal wound was reduced by 46%, pinpointed by Verkkala et al.Citation128
High incidence of glove perforation rates (26%–40%) was found after sternotomy.Citation129,Citation130
Also, an incidence of 36% of surgeons’ fingertips was contaminated by Gram-positive bacteria.Citation131 High prevalence of skin recolonization at the end of surgery was highlighted.Citation129
There is variability in regimens of antimicrobial prophylaxis throughout the world. Nowadays, the effectiveness of these regimens in reducing SSI is falling short of standard,Citation132,Citation133 and there is increasing incidence of multiresistant bacteria worldwide.
Elderly patient and increasing risk of mediastinitis and MRSA
Age of the patients was associated with increasing incidence of total mediastinitis and incidence of specifically Gram-positive bacteria, including MRSA. The elderly patients are a population of people who have a long history of using antibiotics in previous time and have acquired some resistance to these drugs. Suffering from a weakened immune system, the elderly patients are particularly susceptible to all infections, especially MRSA.
In a population study in overall Sweden,Citation134 the incidence of MRSA per 100,000 inhabitants during the period of 2000–2003 was constant with ~5 cases/100,000 inhabitants of 1–59 years and suddenly increased to 10 cases/100,000 inhabitants between 60 and 79 years and to 20 cases/100,000 inhabitants >80 years. This study showed the same trend of increasing incidence by age as in our study on a population of open-heart operated patients.
Elderly patients have high frequency of infectious diseases such as influenza, pneumonia, and urinary tract infection with difficulties in performing early diagnosis because the usual symptoms such as fever and leukocytosis are missing and they are on a high risk of mortality. Little effectiveness of antibiotic treatment in the elderly patients has been shown. On the other hand, there is an alarming upsurge nowadays of antibiotic-resistant bacteria such as MRSA in the community and hospitals and old-people’s home institutions.
This strong association between MRSA and mortality among elderly patients is making preventive actions and politics mandatory and of paramount importance. Nowadays, MRSA is a serious threat to public health throughout the world and to the early and long-term outcome of open-heart surgery.
Conclusion
Evidence from this study suggests the importance of latitude of study place and advanced age as risk factors of mediastinitis. Latitude is a marker of thermally regulated bacterial virulence and variability of surgical and local practices in open-heart surgery in different places of the world. There is deep concern for the high incidence of mediastinitis and MRSA in the elderly patients undergoing sternotomy, and there is urgent need of preventive action.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
We would like to thank our Medical Librarian, Marie Isachsen, for assisting in the literature search.
Disclosure
The authors report no conflicts of interest in this work.
References
- RisnesIAbdelnoorMAlmdahlSMSvennevigJLMediastinitis after coronary artery bypass grafting risk factors and long-term survivalAnn Thorac Surg20108951502150920417768
- RisnesIAbdelnoorMVeelTSvennevigJLLundbladRRynningSEMediastinitis after coronary artery bypass grafting: the effect of vacuum-assisted closure versus traditional closed drainage on survival and re-infection rateInt Wound J201411217718222925188
- StrahlerAHStrahlerANPhysical Geography: Science and Systems of the Human EnvironmentNew YorkThird Wiley2005256282
- ColditzGABrewerTFBerkeyCSEfficacy of BCG vaccine in the prevention of tuberculosis. Meta-analysis of the published literatureJAMA199427196987028309034
- ChengJYKoJSChenRYNgEMMeta-regression analysis using latitude as moderator of paternal age related schizophrenia risk: high ambient temperature induced de novo mutations or is it related to the cold?Schizophr Res2008991–3717618042349
- SandvenIAbdelnoorMNesheimBIMelbyKKHelicobacter pylori infection and hyperemesis gravidarum: a systematic review and meta-analysis of case control studiesActa Obstet Gynecol Scand2009881190120019900137
- AbboudCSWeySBBaltarVTRisk factors for mediastinitis after cardiac surgeryAnn Thorac Surg200477267668314759458
- AhmedDCheemaFHAhmedYIIncidence and predictors of infection in patients undergoing primary isolated coronary artery bypass grafting: a report from a tertiary care hospital in a developing countryJ Cardiovasc Surg (Torino)201152199104
- AlseriusTAndersonREHammarNNordqvistTIvertTElevated glycosylated haemoglobin (HbA1c) is a risk marker in coronary artery bypass surgeryScand Cardiovasc J200842639239818609043
- AntunesPEBernardoJEEugénioLde OliveiraJFAntunesMJMediastinitis after aorto-coronary bypass surgeryEur J Cardiothorac Surg19971234434499332924
- AriyaratnamPBlandMLoubaniMRisk factors and mortality associated with deep sternal wound infections following coronary bypass surgery with or without concomitant procedures in a UK population: a basis for a new risk model?Interact Cardiovasc Thorac Surg201011554354620739410
- SáMPFigueiraESSantosCAValidation of MagedanzSCORE as a predictor of mediastinitis after coronary artery bypass graft surgeryRev Bras Cir Cardiovasc201126338639222086575
- BaskettRJMacDougallCERossDBIs mediastinitis a preventable complication? A 10-year reviewAnn Thorac Surg199967246246510197671
- BitkoverCYGårdlundBMediastinitis after cardiovascular operations: a case-control study of risk factorsAnn Thorac Surg199865136409456092
- BlanchardAHurniMRuchatPStumpeFFischerASadeghiHIncidence of deep and superficial sternal infection after open heart surgery. A ten years retrospective study from 1981 to 1991Eur J Cardiothorac Surg1995931531577786533
- BorgerMARaoVWeiselRDDeep sternal wound infection: risk factors and outcomesAnn Thorac Surg1998654105010569564926
- BraxtonJHMarrinCAMcGrathPD10-year follow-up of patients with and without mediastinitisSemin Thorac Cardiovasc Surg2004161707615366690
- BreyerRHMillsSAHudspethASJohnstonFRCordellARA prospective study of sternal wound complicationsAnn Thorac Surg19843754124166370159
- CayciCRussoMCheemaFHRisk analysis of deep sternal wound infections and their impact on long-term survival: a propensity analysisAnn Plast Surg200861329430118724131
- CentofantiPSaviaFLa TorreMA prospective study of prevalence of 60-days postoperative wound infections after cardiac surgery. An updated risk factor analysisJ Cardiovasc Surg (Torino)2007485641646
- CullifordATCunninghamJNJrZeffRHIsomOWTeikoPSpencerFCSternal and costochondral infections following open-heart surgery. A review of 2,594 casesJ Thorac Cardiovasc Surg19767257147261086408
- DanzerDChristensonJTKalangosAKhatchatourianGBednarkiewiczMFaiduttiBImpact of double internal thoracic artery grafts on long-term outcomes in coronary artery bypass graftingTex Heart Inst J2001282899511453138
- De FeoMRenzulliAIsmenoGVariables predicting adverse outcome in patients with deep sternal wound infectionAnn Thorac Surg200171132433111216770
- De MoraesAAAbboudCSChammasAZLong term mortality of deep sternal wound infection after coronary artery bypass surgeryRev Bras Cir Cardiovasc201227337738223288178
- DemmyTLParkSBLieblerGARecent experience with major sternal wound complicationsAnn Thorac Surg19904934584622310254
- DiezCKochDKussOSilberREFriedrichIBoergermannJRisk factors for mediastinitis after cardiac surgery – a retrospective analysis of 1700 patientsJ Cardiothorac Surg200722317511885
- EklundAMLyytikäinenOKlemetsPMediastinitis after more than 10,000 cardiac surgical proceduresAnn Thorac Surg20068251784178917062248
- ElenbaasTWSoliman HamadMASchönbergerJPMartensEJvan ZundertAAvan StratenAHPreoperative atrial fibrillation and elevated C-reactive protein levels as predictors of mediastinitis after coronary artery bypass graftingAnn Thorac Surg201089370470920172114
- EngelmanRMWilliamsCDGougeTHMediastinitis following open-heart surgery. Review of two years’ experienceArch Surg197310757727784582921
- FakihMGSharmaMKhatibRIncrease in the rate of sternal surgical site infection after coronary artery bypass graft: a marker of higher severity of illnessInfect Control Hosp Epidemiol200728665566017520536
- FarskyPSGranerHDucciniPRisk factors for sternal wound infections and application of the STS score in coronary artery bypass graft surgeryRev Bras Cir Cardiovasc201126462462922358279
- FilsoufiFRahmanianPBCastilloJGMechanickJISharmaSKAdamsDHDiabetes is not a risk factor for hospital mortality following contemporary coronary artery bypass graftingInteract Cardiovasc Thorac Surg20076675375817901106
- FowlerVGJrO’BrienSMMuhlbaierLHCoreyGRFergusonTBPetersonEDClinical predictors of major infections after cardiac surgeryCirculation20051129 SupplI358I36516159846
- GareyKWKumarNDaoTTamVHGentryLORisk factors for postoperative chest wound infections due to gram-negative bacteria in cardiac surgery patientsJ Chemother200618440240817024796
- GaynesRMarosokRMowry-HanleyJMediastinitis following coronary artery bypass surgery: a 3-year reviewJ Infect Dis199116311171211984458
- GhotaslouRYagoubiARKhaliliAAMahmodianRMediastinitis after cardiac surgery in Madani Heart Center, Tabriz, IranJpn J Infect Dis200861431832018653980
- GrmoljezPFBarnerHHWillmanVLKaiserGCMajor complications of median sternotomyAm J Surg197513066796811200281
- GrossiEACullifordATKriegerKHA survey of 77 major infectious complications of median sternotomy: a review of 7,949 consecutive operative proceduresAnn Thorac Surg19854032142234037913
- GrossiEAEspositoRHarrisLJSternal wound infections and use of internal mammary artery graftsJ Thorac Cardiovasc Surg19911023342346 discussion 346–3471881174
- GwelyNDNKhalafSAAbol MaatyRADeep median sternotomy wound infection after open heart surgeryEgypt J Surg2001204742748
- GårdlundBBitkoverCYVaageJPostoperative mediastinitis in cardiac surgery – microbiology and pathogenesisEur J Cardiothorac Surg200221582583012062270
- HarringtonGRussoPSpelmanDSurgical-site infection rates and risk factor analysis in coronary artery bypass graft surgeryInfect Control Hosp Epidemiol200425647247615242194
- HassanMSmithJMEngelAMPredictors and outcomes of sternal wound complications in patients after coronary artery bypass graft surgeryAm Surg200672651552016808205
- HazelriggSRWellonsHAJrSchneiderJAKolmPWound complications after median sternotomy. Relationship to internal mammary graftingJ Thorac Cardiovasc Surg1989986109610992586126
- HosseinrezaeiHRafieiHAmiriMIncidence and risk factors of sternal wound infection at site of incision after open-heart surgeryJ Wound Care201221840841122885314
- ImmerFFDurrerMMühlemannKSErniDGahlBCarrelTPDeep sternal wound infection after cardiac surgery: modality of treatment and outcomeAnn Thorac Surg200580395796116122463
- IvertTLindblomDSahniJEldhJManagement of deep sternal wound infection after cardiac surgery–Hanuman syndromeScand J Thorac Cardiovasc Surg19912521111171947904
- JakobHGBorneff-LippMBachAThe endogenous pathway is a major route for deep sternal wound infectionEur J Cardiothorac Surg200017215416010731651
- Jiménez-MartínezMArgüero-SánchezRPérez-AlvarezJJMina-CastañedaPAnterior mediastinitis as a complication of median sternotomy incisions: diagnostic and surgical considerationsSurgery19706769299344914018
- JonkersDElenbaasTTerportenPNiemanFStobberinghEPrevalence of 90-days postoperative wound infections after cardiac surgeryEur J Cardiothorac Surg20032319710212493512
- JurkiewiczMJBostwickJ3rdHesterTRBishopJBCraverJInfected median sternotomy wound. Successful treatment by muscle flapsAnn Surg198019167387447387236
- KhooAKTanKCOngKKDeep-seated infective mediastinitis in post-coronary artery bypass grafting patientsAnn Acad Med Singapore19942368328377741494
- KimJHammarNJakobssonKLuepkerRVMcGovernPGIvertTObesity and the risk of early and late mortality after coronary artery bypass graft surgeryAm Heart J2003146355556012947378
- KohliMYuanLEscobarMA risk index for sternal surgical wound infection after cardiovascular surgeryInfect Control Hosp Epidemiol2003241172512558231
- KubotaHMiyataHMotomuraNDeep sternal wound infection after cardiac surgeryJ Cardiothorac Surg2013813223688324
- LepelletierDPerronSBizouarnPSurgical-site infection after cardiac surgery: incidence, microbiology, and risk factorsInfect Control Hosp Epidemiol200526546647215954485
- LoopFDLytleBWCosgroveDMMaxwell Chamberlain memorial paper. Sternal wound complications after isolated coronary artery bypass grafting: early and late mortality, morbidity, and cost of careAnn Thorac Surg1990492179186 discussion 186–1872306138
- LuJCGraysonADJhaPSrinivasanAKFabriBMRisk factors for sternal wound infection and mid-term survival following coronary artery bypass surgeryEur J Cardiothorac Surg200323694394912829070
- MacmanusQOkiesJEMediastinal wound infection and aortocoronary graft patencyAm J Surg197613255585611086601
- MagedanzEHBodaneseLCGuaragnaJCRisk score elaboration for mediastinitis after coronary artery bypass graftingRev Bras Cir Cardiovasc201025215415920802905
- MatrosEArankiSFBayerLRMcGurkSNeuwalderJOrgillDPReduction in incidence of deep sternal wound infections: random or real?J Thorac Cardiovasc Surg2010139368068520018307
- OritaHShimanukiTFukasawaMA clinical study of postoperative infections following open-heart surgery: occurrence and microbiological findings in 782 casesSurg Today19922232072121392323
- PaulMRazALeiboviciLMadarHHolingerRRubinovitchBSternal wound infection after coronary artery bypass graft surgery: validation of existing risk scoresJ Thorac Cardiovasc Surg2007133239740317258572
- MilanoCAKeslerKArchibaldNSextonDJJonesRHMediastinitis after coronary artery bypass graft surgery. Risk factors and long-term survivalCirculation1995928224522517554208
- MuñozPMenasalvasABernaldo de QuirósJCDescoMVallejoJLBouzaEPostsurgical mediastinitis: a case-control studyClin Infect Dis1997255106010649402357
- NagachintaTStephensMReitzBPolkBFRisk factors for surgical-wound infection following cardiac surgeryJ Infect Dis198715669679733680996
- NewmanLSSzczukowskiLCBainRPPerlinoCASuppurative mediastinitis after open heart surgery. A case control study of risk factorsChest19889435465533409734
- NoyezLvan DrutenJAMulderJSchroënAMSkotnickiSHBrouwerRMSternal wound complications after primary isolated myocardial revascularization: the importance of the post-operative variablesEur J Cardiothorac Surg200119447147611306315
- OchsnerJLMillsNLWoolvertonWCDisruption and infection of the median sternotomy incisionJ Cardiovasc Surg (Torino)1972135394399
- OlsenMALock-BuckleyPHopkinsDPolishLBSundtTMFraserVJThe risk factors for deep and superficial chest surgical-site infections after coronary artery bypass graft surgery are differentJ Thorac Cardiovasc Surg2002124113614512091819
- OttinoGDe PaulisRPansiniSMajor sternal wound infection after open-heart surgery: a multivariate analysis of risk factors in 2,579 consecutive operative proceduresAnn Thorac Surg19874421731793619541
- Parisian Mediastinitis Study GroupRisk factors for deep sternal wound infection after sternotomy: a prospective, multicenter studyJ Thorac Cardiovasc Surg19961116120012078642821
- ParissisHAl-AlaoBSooAOrrDYoungVRisk analysis and outcome of mediastinal wound and deep mediastinal wound infections with specific emphasis to omental transpositionJ Cardiothorac Surg2011611121923951
- PopovicBVoillotDMaureiraPBilateral internal mammary artery bypass grafting: long-term clinical benefits in a series of 1000 patientsHeart2013991285485923514978
- PrabhakarGHaanCKPetersonEDCoombsLPCruzzavalaJLMurrayGFThe risks of moderate and extreme obesity for coronary artery bypass grafting outcomes: a study from the Society of Thoracic Surgeons’ databaseAnn Thorac Surg200274411251130 discussion 1130–112400756
- RahmanianPBAdamsDHCastilloJGCarpentierAFilsoufiFPredicting hospital mortality and analysis of long-term survival after major noncardiac complications in cardiac surgery patientsAnn Thorac Surg20109041221122920868817
- Careaga ReynaGAguirre BacaGGMedina ConcebidaLEBorrayo SánchezGPrado VillegasGArgüero SánchezRRisk factors for mediastinitis and sternal dehiscence after cardiac surgeryRev Esp Cardiol200659213013516540034
- RidderstolpeLGillHGranfeldtHAhlfeldtHRutbergHSuperficial and deep sternal wound complications: incidence, risk factors and mortalityEur J Cardiothorac Surg20012061168117511717023
- RussoPLBullABennettNInfections after coronary artery bypass graft surgery in Victorian hospitals--VICNISS Hospital Acquired Infection SurveillanceAust N Z J Public Health200529324424815991772
- SachithanandanANanjaiahPNightingalePDeep sternal wound infection requiring revision surgery: impact on mid-term survival following cardiac surgeryEur J Cardiothorac Surg200833467367818243720
- SakamotoHFukudaIOosakaMNakataHRisk factors and treatment of deep sternal wound infection after cardiac operationAnn Thorac Cardiovasc Surg20039422623213129420
- Salehi OmranAKarimiAAhmadiSHSuperficial and deep sternal wound infection after more than 9000 coronary artery bypass graft (CABG): incidence, risk factors and mortalityBMC Infect Dis2007711217888179
- Leung Wai SangSChaturvediRAlamASamoukovicGde VarennesBLachapelleKPreoperative hospital length of stay as a modifiable risk factor for mediastinitis after cardiac surgeryJ Cardio-thorac Surg2013845
- SerryCBleckPCJavidHSternal wound complications. Management and resultsJ Thorac Cardiovasc Surg19808068618677431985
- SharmaMBerriel-CassDBaranJJrSternal surgical-site infection following coronary artery bypass graft: prevalence, microbiology, and complications during a 42-month periodInfect Control Hosp Epidemiol200425646847115242193
- SteingrimssonSGottfredssonMKristinssonKGGudbjartssonTDeep sternal wound infections following open heart surgery in Iceland: a population-based studyScand Cardiovasc J200842320821318569953
- StreckerTRöschJHorchREWeyandMKneserUSternal wound infections following cardiac surgery: risk factor analysis and interdisciplinary treatmentHeart Surg Forum2007105E366E37117855200
- StåhleETammelinABergströmRHambreusANyströmSOHanssonHESternal wound complications--incidence, microbiology and risk factorsEur J Cardiothorac Surg1997116114611539237601
- SutherlandRDMartinezHEGuynesWAMillerLPostoperative chest wound infections in patients requiring coronary bypass. A controlled study evaluating prophylactic antibioticsJ Thorac Cardiovasc Surg1977736944947300825
- SzabóZHåkansonESvedjeholmREarly postoperative outcome and medium-term survival in 540 diabetic and 2239 nondiabetic patients undergoing coronary artery bypass graftingAnn Thorac Surg200274371271912238829
- ToumpoulisIKAnagnostopoulosCEToumpoulisSKDe RoseJJJrSwistelDGRisk factors for sepsis and endocarditis and long-term survival following coronary artery bypass graftingWorld J Surg2005295621627 discussion 627–62815827847
- TangGHMagantiMWeiselRDBorgerMAPrevention and management of deep sternal wound infectionSemin Thorac Cardiovasc Surg2004161626915366689
- ThurerRJBognoloDVargasAIschJHKaiserGAThe management of mediastinal infection following cardiac surgery. An experience utilizing continuous irrigation with povidone-iodineJ Thorac Cardiovasc Surg1974686962968 No abstract available4608531
- TiveronMGFiorelliAIMotaEMPreoperative risk factors for mediastinitis after cardiac surgery: analysis of 2768 patientsRev Bras Cir Cardiovasc2012272203210 English, Portuguese22996970
- ToumpoulisIKAnagnostopoulosCEDeroseJJJrSwistelDGThe impact of deep sternal wound infection on long-term survival after coronary artery bypass graftingChest2005127246447115705983
- TrickWESchecklerWETokarsJIModifiable risk factors associated with deep sternal site infection after coronary artery bypass graftingJ Thorac Cardiovasc Surg2000119110811410612768
- UptonARobertsSAMilsomPMorrisAJStaphylococcal post-sternotomy mediastinitis: five year auditANZ J Surg200575419820315839964
- WalkesJCEarleNReardonMJOutcomes in single versus bilateral internal thoracic artery grafting in coronary artery bypass surgeryCurr Opin Cardiol200217659860112466700
- WangFDChangCHRisk factors of deep sternal wound infections in coronary artery bypass graft surgeryJ Cardiovasc Surg (Torino)2000415709713
- WilsonSJSextonDJElevated preoperative fasting serum glucose levels increase the risk of postoperative mediastinitis in patients undergoing open heart surgeryInfect Control Hosp Epidemiol2003241077677814587944
- WoutersRWellensFVanermenHDe GeestRDegrieckIDe MeerleerFSternitis and mediastinitis after coronary artery bypass grafting. Analysis of risk factorsTex Heart Inst J19942131831888000263
- ZachariasAHabibRHFactors predisposing to median sternotomy complications. Deep vs superficial infectionChest19961105117311788915216
- ElwoodMCritical Appraisal of Epidemiological Studies and Clinical TrialsOxfordOxford University Press2007
- Von ElmEAltmanDGEggerMPocockSJGøtzschePCVandenbrouckeJPThe strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studiesLancet20073701453145718064739
- SandersonSTattIDHigginsJPTTools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliographyInt J Epidemiol20073666667617470488
- GreenlandSO’RourkeKOn the bias produced by quality scores in meta-analysis, and a hierarchical view of proposed solutionsBiostatistics2001246347112933636
- DerSimonianRLairdNMeta-analysis in clinical trialsControl Clin Trials198671771883802833
- FreemanMFTukeyJWTransformations related to the angular and the square rootAnn Math Stat195021607611
- NewcombeRGTwo-sided confidence intervals for the single proportion: comparison of seven methodsStat Med1998178578729595616
- BorensteinMHeggesLVHigginsJPTRothsteinHIntroduction to Meta-AnalysisThird edWiltshire, UKJohn Wiley & Sons2011
- BeggCBMazumdarMOperating characteristics of a rank correlation test for publication biasBiometrics199450108811017786990
- EggerMSmithGDSchneiderMMinderCBias in meta-analysis detected by a simple, graphical testBr Med J19973156296349310563
- DuvalSTweedieRTrim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysisBiometrics200056245546310877304
- TerrinNSchmidtCLauJOlkinIAdjusting publication bias in the presence of heterogeneityStat Med2003222113212612820277
- SchwarzerGmeta: an R package for meta-analysisR News2007734045
- StataCorp LP [homepage on the Internet]STATA Data Analysis and Statistical SoftwareCollege Station, TXStataCorp LP Available from: www.stata.comAccessed March 12, 2016
- MoherDLiberatiATetzlaffJAltmanDGPRISMA GroupPreferred reporting items for systematic reviews and meta-analyses: the PRISMA StatementAnn Intern Med200915126426919622511
- EggerMSmithGDAltmanDGSystematic Reviews in Health Care: Meta-Analysis in ContextSecond edLondonBMJ Publishing Group1995
- ShapiroRSCowenLEThermal control of microbial development and virulence: molecular mechanisms of microbial temperature sensingMBio20122;35e002381210.1128/mBio.00238-12 Print 2012
- EberMRShardellMSchweizerMLLaxminarayanRPerencevichENSeasonal and temperature-associated increases in gram-negative bacterial bloodstream infections among hospitalized patientsPLoS One201169e2529821966489
- MermelLAMachanJTParenteauSSeasonality of MRSA infectionsPLoS One201163e1792521468350
- SahooKCSahooSMarroneGPathakALundborgCSTamhankarAJClimatic factors and community-associated methicillin-resistant Staphylococcus aureus skin and soft-tissue infections – a time-series analysis studyInt J Environ Res Public Health20141198996900725177823
- MadirajuMVBrunnerDPWilkinsonBJEffects of temperature, NaCl, and methicillin on penicillin-binding proteins, growth, peptidoglycan synthesis, and autolysis in methicillin-resistant Staphylococcus aureusAntimicrob Agents Chemother19873111172717333435121
- AyliffeGANoyMFBabbJRDaviesJGJacksonJA comparison of pre-operative bathing with chlorhexidine-detergent and non-medicated soap in the prevention of wound infectionJ Hosp Infect198342372446195236
- WoodheadKTaylorEWBannisterGChesworthTHoffmanPHumphreysHBehaviours and rituals in the operating theatre. A report from the Hospital Infection Society Working Party on Infection Control in Operating TheatresJ Hosp Infect20025124125512183138
- TannerJNorriePMelenKPreoperative hair removal to reduce surgical site infection (review)Cochrane Database Syst Rev201111CD00412222071812
- GroomRCRassiasAJCormackJENorthern New England Cardiovascular Disease Study Group. Highest core temperature during cardiopulmonary bypass and rate of mediastinitisPerfusion20041911912515162927
- VerkkalaKMakelaPOjajarviJTiittanenLHobornJAir contamination in open heart surgery with disposable coveralls, gowns and drapesAnn Thorac Surg1990507577602241338
- BergGAKirkAJBainWHPunctured surgical gloves and bacterial re-colonisation of hands during open heart surgery: implications for prosthetic valve replacementBr J Clin Pract1987419039063451773
- DrieverRBeieMSchmitzESurgical glove perforation in cardiac sugeryThorac Cardiovasc Surg20014932833011745053
- ChristensenJBAndersenBMThomassenSMJohansenOLieMThe effects of ‘in-use’ surgical handwashing on the pre- and postoperative fingertip flora during cardiothoracic and orthopaedic surgeryJ Hosp Infect199595325335
- BratzlerDWHouckPMRichardsCUse of antimicrobial prophylaxis for major surgery:baseline results from the National Surgical Infection Prevention ProjectArch Surg20053817061715
- BratzlerDWHouckPMThe Surgical Infection Prevention Guidelines Writers WorkgroupAntimicrobial prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention ProjectClin Infect Dis2004381706171515227616
- StenhemMOrtqvistARingbergHEpidemiology of methicillin-resistant Staphylococcus aureus (MRSA) in Sweden 2000–2003, increasing incidence and regional differencesBMC Infect Dis200663016504036