Abstract
Background
Given the increasing incidence in cutaneous malignant melanoma (CMM) and the recent changes in the treatment landscape, it is important to understand stage-specific overall and recurrence-free survival patterns in Europe. Despite publications such as EUROCARE-5, there is limited information on stage-specific survival for CMM in Europe.
Method
We carried out a systematic literature review to provide an up-to-date summary of stage-specific survival and recurrence-free survival patterns in patients with CMM in Europe. Studies were included if they were published in Medline during the past 12 years and included information on stage-specific survival and/or recurrence in CMM.
Results
Of the 8,749 studies identified, 26 studies were included, representing nine countries. Collectively, the studies covered a population of 152,422 patients and included data from 1978 to 2011. Randomized clinical trials and single-center observational studies comprised the most common study designs, including five large registry-based studies. Stage-specific information for survival and recurrence varied: 5-year overall survival: 95%–100% (stage I), 65%–92.8% (stage II), 41%–71% (stage III), and 9%–28% (stage IV); 5-year relapse-free survival was reported less frequently: 56% (stage II), and 28%–44% (stage III). Studies reporting survival by sentinel node (SN) status reported 5-year overall survival as 80%–95% for negative SN (stage I/II) and 35%–75% for positive SN (stage III) status; recurrence-free survival at 5 years: 76%–90% for negative and 35%–58% for positive SN status. Some studies included comparisons of survival by key patient sociodemographic characteristics, suggesting that these have a substantial influence on survival and recurrence estimates.
Conclusion
The studies identified in this review show large variations in stage-specific overall and recurrence-free survival by study type and by country. Owing to differing study designs and populations, it is difficult to make detailed comparisons. Large population-based studies that include stage-specific survival and recurrence in Europe are therefore important.
Introduction
Cutaneous malignant melanoma (CMM) is the ninth most common cancer in Europe, with an annual incidence of 13.5 new cases per 100,000 population and over 100,000 new cases diagnosed in 2012 (3% of total cancers).Citation1
With a steady increasing trend in annual incidence rates,Citation2 the incidence of CMM is increasing more rapidly than that of any other cancer in Europe – apart from lung cancer in women.Citation3 Large differences in CMM incidence and mortality exist between European countries, with the highest estimated age-standardized incidence of CMM reported in Switzerland for men and in Denmark for women. Central and Eastern European countries have the lowest reported incidence rates in Europe. A total of 22,211 deaths due to CMM were estimated in Europe in 2012, with annual CMM mortality rates per 100,000 population ranging between 0.5 (Albania) and 3.6 (Norway).Citation1 It has been suggested that some of the differences in CMM incidence and mortality may be due to missed opportunities for early diagnosis and incomplete reporting of CMM.Citation4
In cancer, early detection alone may not necessarily lead to good survival rates; however, CMM is an example in which early detection is associated with higher cure rates.Citation5 There is known variation in reported 5-year survival by country and region in Europe. EUROCARE-5Citation6 analyzed data from more than 10 million patients with cancer diagnosed up to 2007 with follow-up until 2008. Five-year relative survival for CMM was 83.2%, which has not improved since EUROCARE-4.Citation7,Citation8 EUROCARE-5 reports variation in 5-year relative survival by region, with best survival rates in northern and central Europe (87.7% and 87.6%, respectively) compared to 82.6% in southern Europe and 74.3% in Eastern Europe. This variation may be due to later stage at diagnosis and differences in treatment regimes.Citation6,Citation9
Despite attempts to collect and consolidate information in various databases, there are limited published data on stage-specific survival in Europe. Although surgery remains the definitive treatment for patients with earlier-stage CMM (stage I–III), there has been an increase in the use of newly approved drugs for systemic treatment of patients with unresectable and stage IV disease. However, since these novel therapies were introduced relatively recently, it is unlikely that they have influenced survival rates presented in this study. Until recently, interferon 2α remained the only approved systemic adjuvant therapy for patients with stage IIB–III CMM and has minimal effect on patient overall survival (OS). Ipilimumab as adjuvant therapy has now been shown to improve progression-free survival (PFS) in patients with radically resected stage III CMM and is approved in the USA for this indication.Citation10 Ipilimumab is a monoclonal antibody approved for first- and second-line treatment of advanced CMM since 2011; it typically achieves response rates of 5%–15% in patients with regional and distant metastasesCitation11 and is associated with long-term survival in approximately 20% of patients.Citation12 In patients with BRAF V600E (or the rarer V600K) mutated stage IV CMM, the BRAF inhibitors vemurafenib and dabrafenib have demonstrated response rates of approximately 50%.Citation13 Encouragingly, treatment of advanced CMM continues to evolve, with new agents now targeting the programmed death ligand–receptor interaction, such as the anti-PD1 antibodies pembrolizumab and nivolumab, and also targeted drugs that can be used in combination with BRAF inhibitors to inhibit the MAP-kinase pathway, such as the MEK inhibitors trametinib and cobimetinib.Citation14,Citation15
Given the increasing incidence of all-stages CMM and changes in the treatment landscape, it is important to understand the stage-specific survival and recurrence-free survival patterns in Europe from contemporary data and review the reported variation. Reporting stage-specific survival is of importance as the overall CMM survival data may be confounded by an increase over time in proportions of patients diagnosed with early-stage disease (stage I) and a change in staging because of implementation of sentinel node (SN) procedure.Citation16
We carried out a systematic review with the objective to evaluate published robust data on stage-specific survival as well as recurrence-free survival by stage in patients with CMM in Europe.
Materials and methods
Search strategy and study inclusion criteria
We developed and followed a standard protocol for this review according to the PRISMA guidelines for systematic reviews, which define a rigorous process of study identification, screening, eligibility, and inclusion ().Citation17 Studies were considered eligible for inclusion in this review if they were published during the past 12 years (period of publication from January 1, 2004 to December 31, 2015). All included studies were published in English. To ensure study quality, only those published in national or international peer-reviewed journals were considered. Studies were considered for inclusion only if they reported stage-specific rates of survival and/or recurrence in adult (≥18 years of age) patients with CMM. In order to include only studies with more robust outcome data with stage-specific information, studies with fewer than 400 patients were excluded. The cutoff of 400 patients per study was reached after initial review of studies, which showed that the quality of smaller studies was poorer and included mainly single-institution retrospective studies. With only a small proportion of patients in the advanced and metastatic setting in these publications, the accuracy of survival reported and follow-up time recorded in smaller studies was seen to be of poor quality and not relevant to this review paper. Also excluded were reviews, meta-analyses, and case reports.
Study identification and data extraction were performed by searching the Medline scientific literature database using the following search terms: “melanoma”, “skin cancer”, “ survival”, “mortality”, “recurrence”, “metastatic”, “ metastases” (full search terms provided in ). In addition, relevant references and bibliographies were manually searched by trained researchers for additional studies. An initial review of titles and abstracts, and subsequently, a full review of all remaining search results were carried out independently by two reviewers to determine whether they met the criteria for inclusion in this review (). All disagreements were resolved via review by a third reviewer.
Data extraction and synthesis
From each of the identified studies, the following information was extracted: author name(s), date of publication, date/period of coverage of study, study country/countries, description of study population, demographic information, follow-up duration, overall and stage-specific survival, and overall and stage-specific recurrence-free survival rate. Additional information of interest for the particular study was also noted, including potential sources of confounding and whether any sensitivity analyses were performed. In studies where rates were provided for various years, only the most recent estimates were included.
All extracted information was synthesized with the overall interpretation of the findings, taking into account potential sources of study heterogeneity, demographic background of CMM patients, follow-up duration, and potential sources of confounding.
Results
A total of 8,749 studies were identified from the Medline database search, of which 26 studies were included. The studies included populations from nine countries (Denmark, Finland, France, Germany, Italy, the Netherlands, Poland, Sweden, and the United Kingdom), with the majority of studies being from northern Europe ().Citation18–Citation43 Collectively, the identified studies covered a population of 152,422 European patients. We included 5 large population-based registry studiesCitation18–Citation20,Citation42,Citation43 (), 7 randomized clinical trials (RCTs)Citation21–Citation27 (), and 14 observational studiesCitation28–Citation41 (). The 26 identified studies collectively included data on CMM patients from 1978 to 2011. Overall, across countries and by study type, stage-specific information for survival and recurrence varied: 5-year OS: 95%–100% (stage I), 65%–92.8% (stage II), 41%–71% (stage III), and 9%–28% (stage IV); 5-year relapse-free survival (RFS) was reported less frequently: 56% (stage II) and 28%–44% (stage III). Studies reporting survival by SN status reported 5-year OS as 80%–95% for negative SN (stage I/II) and 35%–75% for positive SN (stage III) status; recurrence-free survival at 5 years was 76%–90% for negative and 35%–58% for positive SN status.
Table 1 Number of included studies by country and key study characteristics
Table 2 Five-year stage-specific survival from five large population-based registry studies (Denmark, Germany, Sweden, and the Netherlands)
Table 3 Stage-specific survival rate and recurrence-free survival rate in CMM patients from seven randomized controlled trials (at 5 years unless reported otherwise)
Table 4 Five-year stage-specific survival and recurrence-free survival rate reported in 14 observational studies
Pooling the survival data from population registry studies, RCTs, and observational studies provides a wide variation in the survival and recurrence data. We have presented these data by study type in –.
Although the staging system used by studies included in this review was not always clearly stated, most studies used the staging system of the American Joint Committee on Cancer (AJCC) or the corresponding Union for International Cancer Control (UICC) staging system.
Five population registries with large patient cohorts were identified from Denmark,Citation43 Germany,Citation18 Sweden,Citation19,Citation42 and the Netherlands.Citation20 The Danish study included 27,010 patients; the German study, 37,155 patients; the two Swedish studies, 5,915 and 27,235 patients; and the Dutch registry, 33,181 patients (). Although the primary purpose of the Dutch publication was to study outcomes from CMM of unknown primary origin, only 2.6% of patients (n=857) fell into this category. No significant difference existed between the two groups of patients (CMM of known primary and unknown primary) reporting a 5-year survival of 55% for stage III and 9% for stage IV.Citation20 The first Swedish study is a comprehensive nationwide study of the survival pattern of CMM. The primary purpose of this study was to report the association of level of education with stage at diagnosis and survival in CMM, and this study reported poorer survival in those with lower level of education.Citation19 For this review, we obtained results from study authors (J Lyth, Regional Cancer Center, Linköping, Sweden, personal communication, March, 2015), with 5-year survival reported as 41.3% (95% confidence interval 37.0%–45.5%) for stage III disease and 17.8% (12.3%–24.1%) for stage IV disease. The second Swedish study extracts information from an extensive population-based register covering a population of 2 million people. The main objective of this study was to compare the epidemiological data, management, and outcome of CMM between the younger and the older patient population. Results presented show a significant difference between these two groups of patients regarding all the aspects mentioned earlier, with younger patients having better survival rates.Citation42 The German registry study of CMM covers 40% of the total German population. Results are reported as age-adjusted relative survival by TNM classification, and we estimated the stage IV age-adjusted relative survival to be 18%–28% at 5 years.Citation18 Finally, the Danish population-based register study included 27,010 CMM patients diagnosed between 1989 and 2011 with the aim to investigate the trends in incidence and in survival of CMM in Denmark. The study found that the incidence of CMM in Denmark had more than doubled over the 23-year study period, with the increase seen mainly in lower stage groups and superficial spreading CMM. Age-standardized relative OS had increased in recent years for both men and women.Citation43
We included seven RCTs () that reported survival using Kaplan–Meier methodology and recurrence rates from 4 to 8 years. Six RCTs compared outcomes in patients with CMM with stage IIB–III or stage III disease using interferon alfa 2a or 2b as the investigational treatment arm. The number of patients included ranged from 444Citation24 to 1,388 patients.Citation23 The results show some differences in long-term OS and some improvement in RFS in patients treated with interferon.Citation23,Citation24,Citation26 Survival varied from approximately 35%–50%Citation21,Citation23–Citation26 in control groups to approximately 50%–60% for those treated with interferon for stage IIB/III patients.Citation23–Citation26 The recurrence-/RFS rate in stage IIB/III patients reported at 5 years was approximately 30%Citation21,Citation22 overall; in stage III patients, the rate was approximately 30%–35% for those patients not treated with interferon, and was 40%–45% for those treated with interferon.Citation24,Citation25 As these studies report recurrence-free survival rates in different groups, further comparisons are difficult to make. Gillgren et alCitation27 presented results comparing 2 versus 4 cm excision margins on survival for 936 patients with stage II CMM and reported OS to be 65% at 5 years, and stage-specific rate of recurrence to be 56%.
provides a summary of 14 observational studies: four retrospective and 10 prospective studies, including one from a CMM university registryCitation31 that reported 13 years of follow-up. The range of median follow-up in the prospective studies was from 3 yearsCitation38 to more than 18 yearsCitation36. Ten studies were designed to study outcomes after SN biopsy in early-stage CMM, with follow-up to more advanced disease.Citation28–Citation30,Citation32–Citation35,Citation38,Citation40,Citation41 These studies do not report stage, rather they report the outcome of SN biopsy (negative or positive). It is possible to assume that a patient with a negative SN biopsy is stage I or II, while those with a positive SN are stage III (or possibly stage IV) CMM. Survival in SN-negative patients is consistently higher than that for SN-positive patients: range 80%–95% at 5 years compared to 35%–75%, respectively. Recurrence-free survival rate at 5 years ranges from 76% to 90% in SN-negative patients and from 35% to 58% in SN-positive patients. Of the remaining four observational studies listed in , one study was designed to look at recurrence and survival in a large registry study,Citation31 one studied CMM associated vitiligo,Citation36 one studied the effect of socioeconomic status (SES) on survival,Citation37 and the final studyCitation39 reported the outcomes in patients with unknown primary disease compared to those with known primary disease.
Discussion
To our knowledge, this is the first systematic review of stage-specific survival and recurrence of CMM patients in Europe. Our review identified a relatively small number of published studies (n=26) with over 400 patients and stage-specific outcome data. These were predominantly based in Northern Europe, where considerably higher CMM incidence rates are reported,Citation44 compared with southern Europe, and survival is known to be better.Citation6 Apart from the differences in the incidence and survival between countries, there are also differences in screening, early detection, treatment, and follow-up. Straightforward between-country comparisons are complicated by the large differences observed in study design and patient inclusion criteria, treatments, patient numbers, measurements reported for survival and recurrence, and duration of follow-up. The data provided by the identified studies, when taken collectively, provide an informative general overview of the range and variability of CMM stage-specific treatment outcomes in Europe, as well as of the research gaps, which are evident in this area. Patients included in these studies were diagnosed between 1978 and 2011. The SN biopsy procedure, introduced in the 1990s, has likely led to stage migration in all European countries where it has been implemented. This may mean that some patients previously classified as stage I and II are now being categorized as stage III. This may have led to a perceived improvement in survival for stages I and II, because patients with microscopically positive lymph nodes and poorer prognosis are now correctly being classified as stage III. At the same time, the stage III group may now include patients with a relatively better prognosis (with microscopically positive lymph nodes), which may have led to an overall improved prognosis in stage III CMM (so-called Will Rogers phenomenon).Citation16
Currently, 5-year relative survival after CMM in Europe is, overall, 83%, with variation by country and region.Citation6,Citation9 Survival after a diagnosis of CMM varies widely by stage, and, in this review, we confirmed a large variability in survival. We included five large population-based registry studies from Denmark, Germany, Sweden, and the Netherlands: survival reported varied by study.Citation18–Citation20,Citation42,Citation43 The German,Citation18 the Danish,Citation43 and one of the Swedish studiesCitation42 reported relative survival; the Dutch studyCitation20 reported the crude all-cause survival; and the other Swedish studyCitation19 reported the crude disease-specific survival (DSS). Five-year survival in stage IV disease was the lowest in the Dutch study and was better in the Swedish (18%) and German studies (18%–28%). The completeness of stage at primary diagnosis and mortality data in all five registries is thought to be comprehensive; however, it is not known how accurately recurrence is reported. The Swedish studyCitation19 linked several population-based nationwide registers and censuses, including the Swedish Melanoma Register and the Swedish Cancer Registry, for which completeness of information at diagnosis is known to be very high. In the Dutch national cancer registry, all newly diagnosed malignancies are recorded, and it has nationwide coverage since 1989, whereas the Danish cancer registry began systematic data collection in 1943, and registration has been mandated by administrative order since 1987.Citation45
The reported stage-specific information, for both survival and recurrence, varies widely in the other non-population-based studies included in our review (both RCTs and observational studies). Specific studies, which reported survival and recurrence by different sociodemographic, biological, and clinical patient backgrounds identified that survival rates may be substantially affected by these factors. For example, substantial differences in survival are reported by SES. Stage I/II OS ranged from 91.6% for low SES patients to 97.3%–98.3% for middle/high SES patients.Citation37 This is mostly likely due to differences in early detection, as well as treatment patterns and follow-up.Citation19 Three studies included OS and DSS estimates according to number of lymph nodes involved in CMM patients, with all studies reporting substantial differences.Citation20,Citation32,Citation33 For example, the Dutch registry study and an Italian retrospective study reported approximately half the 5-year OS rate when two or more lymph nodes were involved compared to only one lymph node involved (27.1% versus 50.1% for the Dutch study; 39.6% versus 81.4% for the Italian study).Citation20,Citation33 This further supports the importance of adequate substaging of stage III CMM patients according to number of involved lymph nodes. Differences were also observed for RFS, for example, by SES (from 81.7% for low SES patients to 91.8% for high SES patients).Citation37
Stage-specific recurrence-free survival rates were not reported from any of the large registry studies, probably due to a lack of structured follow-up reporting in these settings; consequently, the best sources for the assessment of recurrence risk by stage were RCTs (), while nine observational studies also reported recurrence-free survival rates (). As was the case with the reported stage-specific survival data, most of the studies reporting recurrence outcomes had defined inclusion criteria in terms of the CMM stage their patient population sample comprised.
Limitations
Although the five registry studiesCitation18–Citation20,Citation42,Citation43 included are assumed to be of higher quality than the small-sized single-center studies, in practice, most registries may suffer from various degrees of underreporting. While the Swedish, the Danish, and the Dutch registry studies are nationwide population studies with high coverage of the national population, the German study covered only a section, 40%, of the population. This could mean that regional differences in CMM prevalence and quality of diagnosis and treatment options can influence stage at diagnosis and related survival. Also, the lack of completeness in stage-specific information at recurrence in the registry studies as well as incomplete information on histopathological prognostic factors may influence the reported results. For example, more than 5,000 patients in the Swedish study had unknown stage of disease at diagnosis.
Furthermore, registry studies may not capture follow-up data as accurately as prospective cohort studies or RCTs. Missing information on death, owing to incompleteness of follow-up, may have a disproportionate effect on survival estimates, although linking of registries to national cause of death registries limits this bias.Citation19,Citation20 In addition, changes in treatment strategies like sentinel lymph node biopsy and staging classification provides further challenges for the interpretation of the overall data.
The data generated from seven RCTs included in our study may not be representative of survival patterns in the general patient population, because the trial populations are typically highly selective due to strict inclusion and exclusion criteria; however, they also provide data with high quality since the follow-up may have been more stringent. Indeed, it may be valuable for potential authors interested in performing a trial with similar inclusion criteria to have the available data from these RCTs listed in our review.
Most of the identified studies had defined inclusion criteria in terms of CMM stage and treatments under review. In effect, this limited the reporting of stage-specific data to subsets of patients for each study. However, when taken together, the studies cover all CMM stages and, hence, provide an overview of the general landscape in Europe in terms of stage-specific survival.
It should also be emphasized that it is challenging to compare data from different timeframes owing to the change in behavior (sun exposure) and awareness over time. Interventions such as SN procedures have also resulted in a change in staging, with more accurate staging in recent years.
Conclusion
The studies identified in this review highlight large variations in stage-specific survival and rates of recurrence between European countries. From the 26 included studies, which represented nine countries, stage-specific information for survival and recurrence varied: 5-year OS rates were 95%–101% (stage I), 65%–92.8% (stage II), 41%–71% (stage III), and 9%–28% (stage IV); 5-year RFS was reported less frequently: 56% (stage II) and 28%–44% (stage III).
Owing to differing study designs and populations, it is difficult to make detailed comparisons between studies. It is likely that differences in country guidelines and success in early diagnosis of CMM, as well as approaches to treatment contribute to differences in reported outcomes. However, a number of studies included evaluations enabling comparisons in OS and recurrence-free survival estimates by key patient sociodemographic characteristics, which suggest that differences in these factors can result in substantial attenuation or reduction of the survival estimates for separate patient groups. Further large-sample population-based studies are needed to provide a more comprehensive overview of patterns of CMM stage-specific survival within European populations.
Changes in epidemiology may be of relevance for planned future studies in CMM, with new agents likely to enter the adjuvant setting. Recently in Europe, stage migration toward less-advanced CMM at diagnosis and a shift in distribution toward higher proportion of patients with better prognosis have been seen. This can lead to underestimation of required sample size and a delay until clinical trials report outcome. In addition, the degree of heterogeneity in treatment of early-stage CMM in different parts of Europe and its impact on clinical outcome is not well characterized. A characterization of stage-specific risk of recurrence and survival in more modern cohorts is thus relevant from a clinical and patient perspective and might also be helpful in the design of clinical trials.
Acknowledgments
Scientific consultancy on the study was provided by IMS Health, Sweden. This study was funded by Amgen Limited.
Supplementary materials
Figure S1 Search flow diagram (according to the PRISMA statement).
Abbreviation: PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
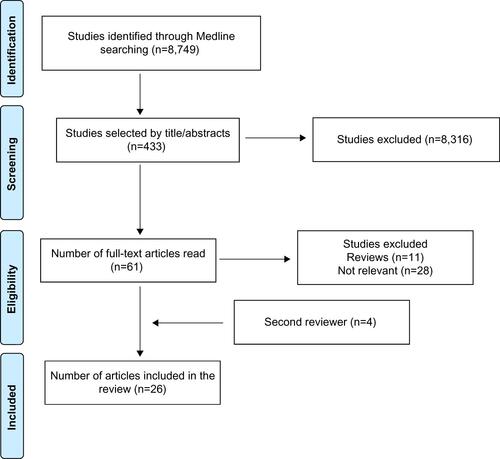
Table S1 PRISMA systematic review reporting checklist
Table S2 Medline search command
Disclosure
This study was supported by Amgen Limited. Johan Hansson was funded by The Swedish Cancer Society, The Radiumhemmet Research Funds, The Swedish Research Council, and The Stockholm County Council. At the time of writing, Demetris Pillas, Aliki Taylor, and Moninder Kaur were employed by Amgen Limited, and Aliki Taylor owned Amgen stock. Fernanda Costa Svedman has no conflicts of interest. Johan Hansson was acting as a consultant for IMS Health (formerly Pygargus) during the conduct of the study. Johan Hansson has received personal fees from Roche, Bristol-Myers Squibb, Novartis, and Merck, outside the submitted work. Ragnar Linder received a grant from Amgen Ltd to carry out the study to develop a report on survival after CMM in Europe. No grant was given for the manuscript development. Amgen and other pharmaceutical companies are regular clients to Pygargus/IMS Health, outside the submitted work. The authors report no other conflicts of interest in this work.
References
- International Agency for Research on CancerGLOBOCAN 2012: Estimated Cancer Incidence, Mortality, and Prevalence Worldwide in 2012Lyon, FranceInternational Agency for Research on Cancer2012 Available from: http://globocan.iarc.frAccessed November 10, 2014
- ErdmannFLortet-TieulentJSchüzJInternational trends in the incidence of malignant melanoma 1953–2008 – are recent generations at higher or lower risk?Int J Cancer2013132238540022532371
- JemalASiegelRWardECancer statistics, 2006CA Cancer J Clin200656210613016514137
- ForseaAMDel MarmolVde VriesEBaileyEEGellerACMelanoma incidence and mortality in Europe: new estimates, persistent disparitiesBr J Dermatol201216751124113022759278
- HowladerNNooneAMKrapchoMSEER Cancer Statistics Review, 1975–2008Bethesda, MDNational Cancer Institute2011
- De AngelisRSantMColemanMPEUROCARE-5 Working GroupCancer survival in Europe 1999–2007 by country and age: results of EUROCARE-5 – a population-based studyLancet Oncol201415233424314615
- BerrinoFDe AngelisRSantMSurvival for eight major cancers and all cancers combined for European adults diagnosed in 1995–1999: results of the EUROCARE-4 studyLancet Oncol20078977378317714991
- SantMAllemaniCSantaquilaniMEUROCARE-4. Survival of cancer patients diagnosed in 1995–1999. Results and commentaryEur J Cancer200945693199119171476
- CrocettiEMalloneSRobsahmTESurvival of patients with skin melanoma in Europe increases further: results of the EUROCARE-5 studyEur J Cancer Epub952015
- EggermontAMChiarion-SileniVGrobJJAdjuvant ipilimumab versus placebo after complete resection of high-risk stage III melanoma (EORTC 18071): a randomised, double-blind, phase 3 trialLancet Oncol201516552253025840693
- GuidaMPiscontiSColucciGMetastatic melanoma: the new era of targeted therapyExpert Opin Ther Targets201216Suppl 2S61S7022443134
- SchadendorfDHodiFSRobertCPooled analysis of long-term survival data from phase II and phase III trials of ipilimumab in unresectable or metastatic melanomaJ Clin Oncol201533171889189425667295
- ChapmanPBHauschildARobertCImproved survival with vemurafenib in melanoma with BRAF V600E mutationN Engl J Med2011364262507251621639808
- FDA Approves Second PD-1 InhibitorNivolumab, for MelanomaDepartment of Health and Human Services. FDA U.S. Food and Drug Administration Available from: http://www.cancernetwork.com/melanoma/fda-approves-second-pd-1-inhibitor-nivolumab-melanomaAccessed March 16, 2016
- Trametinib and DabrafenibDepartment of Health and Human Services. FDA U.S. Food and Drug Administration Available from: http://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm381451.htmAccessed March 16, 2016
- FeinsteinARSosinDMWellsCKThe Will Rogers phenomenon. Stage migration and new diagnostic techniques as a source of misleading statistics for survival in cancerN Engl J Med198531225160416084000199
- MoherDLiberatiATezlaffJAltman DG; PRISMA GroupPreferred reporting items for systematic reviews and meta-analyses: the PRISMA statementPLoS Med20096e10000097
- EisemannNJansenLHolleczekBUp-to-date results on survival of patients with melanoma in GermanyBr J Dermatol2012167360661222564081
- ErikssonHLythJMansson-BrahmeELow level of education is associated with later stage at diagnosis and reduced survival in cutaneous malignant melanoma: a nationwide population-based study in SwedenEur J Cancer201349122705271623583439
- de WaalACAbenKKvan RossumMMKiemeneyLAMelanoma of unknown primary origin: a population-based study in the NetherlandsEur J Cancer201349367668323031553
- HancockBWWheatleyKHarrisSAdjuvant interferon in high-risk melanoma: the AIM HIGH Study – United Kingdom Coordinating Committee on Cancer Research randomized study of adjuvant low-dose extended-duration interferon Alfa-2a in high-risk resected malignant melanomaJ Clin Oncol2004221536114665609
- KleebergURSuciuSBrockerEBFinal results of the EORTC 18871/DKG 80-1 randomised phase III trial. rIFN-α2b versus rIFN-γ versus ISCADOR M versus observation after surgery in melanoma patients with either high-risk primary (thickness >3 mm) or regional lymph node metastasisEur J Cancer200440339040214746858
- EggermontAMSuciuSMacKieRPost-surgery adjuvant therapy with intermediate doses of interferon alfa 2b versus observation in patients with stage IIb/III melanoma (EORTC 18952): randomised controlled trialLancet200536694921189119616198768
- GarbeCRadnyPLinseRAdjuvant low-dose interferon {α}2a with or without dacarbazine compared with surgery alone: a prospective-randomized phase III DeCOG trial in melanoma patients with regional lymph node metastasisAnn Oncol20081961195120118281266
- EggermontAMSuciuSTestoriALong-term results of the randomized phase III trial EORTC 18991 of adjuvant therapy with pegylated interferon alfa-2b versus observation in resected stage III melanomaJ Clin Oncol201230313810381823008300
- HanssonJAamdalSBastholtLTwo different durations of adjuvant therapy with intermediate-dose interferon alfa-2b in patients with high-risk melanoma (Nordic IFN trial): a randomised phase 3 trialLancet Oncol201112214415221256809
- GillgrenPDrzewieckiKTNiinM2 cm versus 4 cm surgical excision margins for primary cutaneous melanoma thicker than 2 mm: a randomised, multicentre trialLancet201137898031635164222027547
- KoskivuoIHernbergMVihinenPSentinel lymph node biopsy and survival in elderly patients with cutaneous melanomaBr J Surg201198101400140721638276
- DebarbieuxSDuruGDalleSBeatrixOBalmeBThomasLSentinel lymph node biopsy in melanoma: a micromorphometric study relating to prognosis and completion lymph node dissectionBr J Dermatol20071571586717501957
- KunteCGeimerTBaumertJPrognostic factors associated with sentinel lymph node positivity and effect of sentinel status on survival: an analysis of 1,049 patients with cutaneous melanomaMelanoma Res201020433033720526218
- HohnheiserAMGefellerOGohlJSchulerGHohenbergerWMerkelSMalignant melanoma of the skin: long-term follow-up and time to first recurrenceWorld J Surg201135358058921125274
- MeierASatzgerIVolkerBKappAGutzmerRComparison of classification systems in melanoma sentinel lymph nodes – an analysis of 697 patients from a single centerCancer2010116133178318820564647
- CascinelliNBombardieriEBufalinoRSentinel and non-sentinel node status in stage IB and II melanoma patients: two-step prognostic indicators of survivalJ Clin Oncol200624274464447116983115
- MandalaMImbertiGLPiazzalungaDClinical and histopathological risk factors to predict sentinel lymph node positivity, disease-free and overall survival in clinical stages I–II AJCC skin melanoma: outcome analysis from a single-institution prospectively collected databaseEur J Cancer200945142537234519553103
- TestoriADe SalvoGLMontescoMCClinical considerations on sentinel node biopsy in melanoma from an Italian multi-centric study on 1,313 patients (SOLISM-IMI)Ann Surg Oncol20091672018202719132446
- QuaglinoPMarencoFOsella-AbateSVitiligo is an independent favourable prognostic factor in stage III and IV metastatic melanoma patients: results from a single-institution hospital-based observational cohort studyAnn Oncol201021240941419622589
- MandalàMImbertiGLPiazzalungaDAssociation of socioeconomic status with Breslow thickness and disease-free and overall survival in stage I-II primary cutaneous melanomaMayo Clin Proc201186211311921282485
- NoweckiZIRutkowskiPNasierowska-GuttmejerARukaWSurvival analysis and clinicopathological factors associated with false-negative sentinel lymph node biopsy findings in patients with cutaneous melanomaAnn Surg Oncol200613121655166317016755
- RutkowskiPNoweckiZIDziewirskiWMelanoma without a detectable primary site with metastases to lymph nodesDermatol Surg201036686887620482725
- de VriesMSpeijersMJBastiaannetELong-term follow-up reveals that ulceration and sentinel lymph node status are the strongest predictors for survival in patients with primary cutaneous melanomaEur J Surg Oncol201137868168721636244
- KettlewellSMoyesCBrayCValue of sentinel node status as a prognostic factor in melanoma: prospective observational studyBMJ20063327555142316735303
- PlymAUllenhagGJBreivaldMLambeMBerglundAClinical characteristics, management and survival in young adults diagnosed with malignant melanoma: a population-based cohort studyActa Oncol201453568869624369746
- BayCKejsAStormHEngholmGIncidence and survival in patients with cutaneous melanoma by morphology, anatomical site and TNM stage: a Danish Populational-based Register Study 1989–2011Cancer Epidemiol2015391725468643
- de VriesEBrayFIEggermontAMCoeberghJWEuropean Network of Cancer RegistriesMonitoring stage-specific trends in melanoma incidence across Europe reveals the need for more complete information on diagnostic characteristicsEur J Cancer Prev200413538739515452451
- StormHHMichelsenEVClemmensenIHPihlJThe Danish Cancer Registry – history, content, quality and useDan Med Bull19974455355399408738
