Abstract
Objective
This study was to evaluate the risk factors of survival in patients with columnar cell variant (CCV) and encapsulated variant (ECV).
Materials and methods
The Surveillance, Epidemiology, and End Results database (1988–2013) was used to compare the characteristics of CCV and ECV with those of classic papillary thyroid carcinoma (PTC). Survival was analyzed by the Kaplan–Meier method, the log-rank test, and Cox multivariate regression. Multivariate logistic regression was used to further analyze lymph node metastases and distant metastasis. There were 765 CCV, 529 ECV, and 39,035 PTC patients. ECV tumors were similar to PTC in terms of overall survival, disease-specific survival, age, sex, and distant metastasis.
Results
Compared with PTC, CCV tumors tended to be larger, with a higher incidence rate among males and in patients ≥65 years of age. CCV was associated with higher rates of extrathyroidal extension, multifocality, lymph node examinations, and lymph node and distant metastases (p<0.0001). Significant differences were found in 10-year overall survival (97.14% vs 89.15%, p<0.0001) and disease-specific survival (99.08% vs 93.07%, p<0.0001) between PTC and CCV. In CCV, distant metastasis (hazard ratio 5.125, p<0.0001) and lymph nodal metastasis (hazard ratio 2.152, p=0.032) predicted a poor prognosis. After adjustment, distant metastasis was independently associated with age ≥65 years, and lymph nodal metastasis was independently associated with female sex (odds ratio [OR] 0.341 [0.234–0.496]), extrathyroidal extension (OR 2.453 [1.368–4.397]), multifocality (OR 2.168 [1.318–3.569]), size >20 mm, ≤40 mm (OR 1.851 [1.170–2.928]), and size >40 mm (OR 1.847 [1.088–3.136]).
Conclusion
ECV appears to have a similar prognosis to PTC, while CCV has a worse prognosis than classic PTC. Treatment with external beam radiotherapy and radioactive implants should be conducted carefully in patients with CCV.
Introduction
The incidence of thyroid cancer increased by 211% between 1975 and 2013 in the USA, largely due to the increased incidence of papillary thyroid cancer (PTC), which currently accounts for 80% of all cases of thyroid cancers. The overall survival (OS) rate has remained between 90% and 95% in recent decades. PTC is a low-risk histologic type of cancer and is associated with high disease-specific survival (DSS).Citation1–Citation4 This type of cancer has been characterized by factors, such as age, sex, tumor size, extrathyroidal extension (ETE), nodal metastasis, and distant metastasis.Citation5–Citation7
Among all subtypes of thyroid cancer, columnar cell variant (CCV) and encapsulated variant (ECV) are rare subtypes that have not been exclusively studied. CCV was first described in 1986, and although its biological behavior is still unclear,Citation8,Citation9 CCV has been characterized by a papillary morphology, the presence of pseudostratified columnar cells, and absence of sparse colloid and psammoma bodies.Citation10 CCV accounts for only 0.15%–0.4% of PTC cases but is much more aggressive than classic PTC.Citation11–Citation18 ECV is characterized by the presence of a complete fibrous capsule with tumor cells showing nuclear features similar to those of PTC. Although these morphological characteristics have been long recognized, ECV was formally recognized in the 2017 World Health Organization (WHO) classification of endocrine tumors.
Although the clinical characteristics of classic PTC are clearly defined, the clinical signs of CCV and ECV are currently ambiguous and remain controversial. Studies on CCV and ECV largely consist of case reports, and neither large sample analyses nor multicenter cross-sectional studies have been undertaken.
This study performed an analysis of rare variants of PTC among a large population. We compare the clinical and pathologic characteristics of CCV and ECV with those of classic PTC and identify risk factors associated with survival, distant metastases, and nodal metastasis.
Materials and methods
Data source and study participants
The data source for this study was the Surveillance, Epidemiology, and End Results (SEER) database of the National Cancer Institute (NCI), which provides population-based cancer registries coverinĝ28% of the US population. This article does not contain any studies with human participants or animals performed by any of the authors. The data of this article are from the SEER Program of the NCI, which is a public database that does not require ethical approval.
Cases of PTC, CCV, and ECV from 1988 to 2013 were selected from all 18 registries using ICD-O-3 codes 8260/3 (PTC), 8343/3 (ECV), and 8344/3 (CCV). The exclusion criteria were as follows: 1) the presence of secondary malignancies, 2) the presence of other primary thyroid malignancies, 3) age <18 years, and 4) a history of previous surgery for PTC.
The demographic variables of interest included sex, age at diagnosis, and race. The clinical variables of interest included surgical therapy (lobectomy or total thyroidectomy), radiation therapy (none, radioisotopes, external-beam radiation therapy [EBRT], radioactive implant, and other), and survival status (OS and DSS) as of December 31, 2013. OS and DSS were calculated as the time in years from diagnosis until death and disease-specific death, the last date of contact with the living patient, or December 31, 2013, whichever came first. The pathologic variables of interest included tumor size of the primary cancer taken as its largest dimension, multifocality, ETE, the number of lymph nodes examined, and nodal and distant metastases. ETE was defined as tumor invasion beyond the thyroid capsule.
Statistical analysis
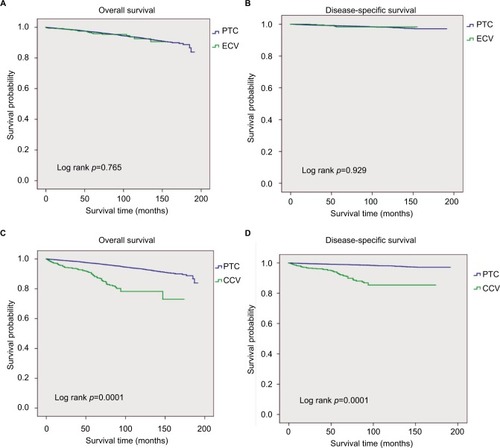
Summary statistics were used to describe the baseline characteristics of the patients (). Analysis of variance and the chi-square test were used to analyze categorical and continuous variables, respectively. OS and DSS were analyzed using the Kaplan–Meier method, and the log-rank test was used to determine whether differences in survival were statistically significant (). A Cox proportional hazards regression model was built to evaluate the effects of variables on cancer mortality in CCV patients, which was subsequently adjusted for a multivariate analysis of patient characteristics and tumor characteristics. The hazard ratios (HRs) for the relationships between each variable and DSS were calculated using a binary Cox regression model. Univariate and multivariate logistic regression models were used to evaluate independent predictors of lymph mode metastasis and distant metastasis in CCV. Variables with p<0.05 were considered statistically significant.
Table 1 Clinical characteristics and pathologic characteristics of classic PTC compared with those of the CCV and ECV
Figure 1 OS and DSS of patients of thyroid carcinoma.
Notes: (A) Kaplan–Meier analysis of OS between PTC and ECV; (B) Kaplan–Meier analysis of DSS between PTC and ECV; (C) Kaplan–Meier analysis of OS between PTC and CCV; (D) Kaplan–Meier analysis of DSS between PTC and CCV.
Abbreviations: CCV, columnar cell variant; DSS, disease-specific survival; ECV, encapsulated variant; OS, overall survival; PTC, papillary thyroid carcinoma.
Our analyses were performed with SPSS v19 (SPSS, Inc., Chicago, IL, USA) and SAS software version 9.2 (SAS Institute, Cary, NC, USA). Because SEER data reflect public and de-identified information, this study was considered exempt from institutional review board approval at our institution.
Results
There were 529 cases of ECV, 765 of CCV, and 39,035 of classic PTC diagnosed during the study period. Patients with PTC were followed for up to 26 years, while ECV and CCV patients were followed for up to 13 years. No published systematic reviews or prospective analyses have been found with regard to the use of EBRT in CCV patients, and the Database of Abstracts of Reviews and Effects yielded no results. This lack of data and the conflicting reports on EBRT in CCV prompted this summary of existing evidence to better inform clinicians.
Characteristics
The clinical and pathological characteristics of the patients are summarized in . Compared with classic PTC, CCV more frequently affected patients aged ≥65 years old (23.53% vs 11.84%, p<0.0001) and males (25.88% vs 22.51%, p=0.0272). CCV tumors tended to have a larger mean size than PTC tumors (26.40±20.00 mm vs 17.82±16.77 mm, p<0.0001), with significantly higher rates of ETE (51.24% vs 20.90%, p<0.0001) and nodal metastasis (49.41% vs 35.91%, p≤0.0001). In addition, CCV patients had more regional lymph nodes than PTC patients (70.59% vs 59.77%, p<0.0001), and CCV patients were 4 times more likely to have distant metastasis than PTC patients (3.01% vs 0.77%, p<0.0001). CCV patients were more likely to undergo total thyroidectomy (96.47% vs 94.16%, p=0.0067) than PTC patients. However, significantly lower rates of multifocality were observed among CCV patients (17.78% vs 28.16%, p<0.0001).
The age and sex of ECV and PTC patients were similar. The mean tumor size among classic PTC cases was smaller than that among ECV cases (17.82±16.77 vs 21.56±27.76, p<0.0001). Among patients whose lymph nodes were examined (41.59% vs 59.77%, p<0.0001), nodal metastases were most common among PTC patients (17.20% vs 35.91%, p<0.0001). The rate of ETE in classic PTC patients was 2.35-fold higher than ECV patients (20.90% vs 8.88%, p<0.0001). No differences were found between ECV and PTC patients with respect to the rates of radiation (radioactive iodine [RAI] 51.80% vs 53.97%, p=0.0803) and distant metastasis (0.38% vs 0.77%, p=0.3054). However, PTC patients were more likely to undergo total thyroidectomy vs lobectomy than classic ECV patients (94.16% vs 91.12%, p=0.0031).
Survival
All-cause mortality occurred in 10.98% of CCV patients (n=84), 3.97% of ECV patients (n=21), and 3.02% of PTC patients (n=1179), while disease-specific mortality occurred in 6.93% of CCV patients (n=53), 1.13% of ECV patients (n=6), and 0.98% of classic PTC patients (n=381). The 10-year DSS rates for CCV, ECV, and classic PTC patients were 93.07%, 98.87%, and 99.08%, respectively, and the univariate analysis of survival revealed no association between ECV and PTC in terms of OS and DSS. However, patients with CCV tended to have lower rates of OS and DSS than patients with PTC (10-year OS: 89.15% vs 97.14%, p<0.0001, 10-year DSS: 93.07% vs 99.08%, p<0.0001). In comparing these 2 subgroups, CCV patients exhibited significantly worse OS and DSS rates (p<0.0001; ).
Multivariate survival analyses for risk factors of 10-year DSS
Cox proportional hazards models were applied to quantify the prognostic significance of demographic features, tumor factors, and treatment, including adjustments for competing risk factors (). ECV and CCV differed in terms of 10-year DSS. The univariate and multivariate analyses of survival revealed no association between OS and DSS in ECV. An age >45 years remained a risk factor and age >65 years remained the strongest risk factor for 10-year DSS in CCV (HR=5.93 and 10.70; p=0.018, p=0.002). CCV patients with EBRT and radioactive implants, nodal metastasis, and distant metastasis had higher risks associated with 10-year DSS (HR=3.77, 2.15, 5.13, p<0.05, respectively).
Table 2 Cox multivariate regression analyses of factors associated with 10-year DSS among 765 patients with CCV, SEER (1988–2013)
Predictors of local nodal metastasis and distant metastasis
In patients with CCV, distant metastasis was independently associated with age ≥65 years (odds ratio [OR] 5.6 [1.57–20.07]). Local nodal metastasis was independently associated with female sex (OR 0.341 [0.234–0.496]), ETE (OR 2.453 [1.368–4.397]), multifocality (OR 2.168 [1.318–3.569]), size >20 mm and ≤40 mm (OR 1.851 [1.170–2.928]), and size >40 mm (OR 1.847 [1.088–3.136]) ().
Table 3 Logistic multivariate regression analyses of factors associated with nodal metastases and distant metastases among 765 patients with CCV, SEER (1988–2013)
Discussion
To our knowledge, this study is the first large population-level analysis of encapsulated and columnar cell variants of PTC. Although CCV is known to be more aggressive and ECV to be indolent compared with classic PTC, controversy remains with regard to their prognoses.Citation11,Citation12,Citation15,Citation18–Citation22 ECV was defined recently in the WHO classification of endocrine tumors.Citation20 Most cases of CCV show a poor prognosis and high mortality.Citation19 However, some cases of CCV, characterized as typically small, circumscribed or encapsulated tumors similar to ECV, have shown a more optimistic prognosis.Citation10,Citation23 Because previous studies regarding these rare variants largely consist of case reports and single-institution cohorts, we collected hundreds of cases from the SEER to define the relationships between clinicopathological characteristics and the DSS rates of these variants.
We found that some patients with CCV exhibited more aggressive features than patients with classic PTC, including ETE, lymph node examination, and nodal and distant metastases. Compared with classic PTC, ECV is characterized by lower rates of ETE, lymph nodal examination, and nodal metastasis. In our study, ECV had a similar rate of survival, whereas CCV had a lower rate of survival than classic PTC. Although no association was found between ECV and OS or DSS, our study was underpowered to detect such differences. However, in CCV patients, we found that age ≥45–64 years, age >65 years, EBRT, radioactive implants, and lymph nodal and distant metastases were associated with 10-year DSS.
Surprisingly, our survival analysis of CCV revealed that ETE, tumor size, and multifocality were not risk factors of 10-year DSS, which completely contradicts previous studies on PTC. Nevertheless, because CCV exhibits more aggressive behavior than classic PTC, we postulate that patients with CCV may experience higher rates of tumor recurrence and mortality. These results may have important clinical implications at the operative level. The management of CCV is controversial, and the current guidelines of the American Thyroid Association recommend total thyroidectomy or near-total thyroidectomy and lobectomy, central lymphadenectomy, and postoperative RAI as indicated.Citation13 Total thyroidectomy or near-total thyroidectomy and lobectomy did not result in a significant difference in survival in our study. However, the rates of definitive hypoparathyroidism and recurrent laryngeal nerve injury following total thyroidectomy and total thyroidectomy associated with routine central lymph node dissection were higher than that after lobectomy and total thyroidectomy.Citation24,Citation25 Patients have been treated by these 2 types of surgeries in our studies. In addition, a subgroup analysis indicated that operative treatment may be related to decreased effects of ETE, multifocality, and tumor size. We assumed that columnar-cell histology inherently represents a more aggressive variant of PTC,Citation26 and therefore, nodal and distant metastases were risk factors for survival in our study. Univariate analysis after multivariate adjustment revealed that male sex, ETE, multifocality, and tumors size >4 cm were associated with higher risks of nodal metastasis, whereas age >45 years was the only risk factor for distant metastasis. Therefore, due to the successful use of appropriate surgical modalities, tumor size and multifocality would not have a significant effect on survival.
EBRT is typically reserved as a last resort after surgery and RAI have been attempted.Citation21 Some studies revealed that EBRT has been traditionally used to treat incompletely resected tumors, unresectable diseases, and aggressive variants, and to reduce the risk of locoregional recurrence.Citation27,Citation28 Other retrospective reviews failed to show any differences in loco-regional control and survival between patients who had received EBRT and those who had not.Citation29 Interestingly, EBRT and radioactive implants were risk factors for 10-year DSS in CCV patients according to our analysis. Patients treated with EBRT had visibly more aggressive tumor characteristics compared with patients who had not undergone EBRT. Sometimes, the risk of recurrence depends on ETE, patient age, and tumors with a reduced iodine uptake.Citation30–Citation34 In our study, patients who underwent EBRT showed significantly higher rates of aggressive characteristics, such as age ≥65 years, lymph node metastasis, and distant metastasis. Therefore, we suspect that EBRT is limited in its ability to improve survival time and is also a risk factor for 10-year DSS. Future research on CCV is needed to further elucidate this issue.
Preoperative diagnosis of CCV is difficult,Citation35 and such diagnosis should be more clearly established. CCV tumors have unique pathologic characteristics and are composed of pseudostratified columnar cells, some of which may include neoplastic cells with elongated nuclei, hyperchromasia, and supranuclear and/or subnuclear cytoplasmic vacuolization.Citation36 Some studies demonstrated that certain molecular and immunophenotypic features were associated with the diagnosis and prognosis of CCV, such as the Ki67/Mib1 labeling index, BRAFV600E, CEA, nuclear cyclin D1, CK7, CK20, CDX2, and bcl-2.Citation9,Citation10,Citation19,Citation37 More work needs to be conducted to define the characteristics of CCV that provide the most valuable diagnostic, therapeutic, and prognostic information.
Limitations
Limitations of this study include those inherent to the SEER database, such as coding errors and limited data on CCV and ECV. CCV was first reported in the SEER database in 2001, and the mean follow-up of 10 years limits the survival analysis. Because CCV and ECV are rare tumors, our study may be underpowered to discover more subtle differences among CCV, ECV, and PTC. Despite these limitations, this is the largest study to date on this topic. Furthermore, the SEER database does not provide data regarding recurrence.
Overall, ECV and CCV are rare tumors that share various characteristics. ECV tends to be more indolent than classic PTC, whereas the CCV of papillary carcinoma shows a poor prognosis compared with conventional PTC. Early detection of CCV and aggressive intervention in patients with these tumors, especially those aged <45 years old, could lead to more favorable outcomes. Furthermore, CCV patients should be carefully treated with EBRT.
Conclusion
ECV appears to have a prognosis similar to that of classic PTC, while CCV has a worse prognosis than classic PTC. Treatment with EBRT and radioactive implants should be conducted carefully in patients with CCV.
Acknowledgments
This study used the SEER database. The interpretation and reporting of these data are the sole responsibilities of the authors. The authors acknowledge the efforts of the applied Research Program, NCI; the Office of Research, Development and Information, and the Surveillance, Epidemiology and End Results (SEER) Program tumor registries in the creation of this database.
Author contributions
SW conceived and designed the study, CJ performed data collection and analysis, TC helped with construction and manuscript writing, JL contributed to the discussion, XZ supervised this data, SH contributed to the discussion, SL interpreted the data, and JW participated in the design of the study. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- LimHDevesaSSSosaJACheckDKitaharaCMTrends in thyroid cancer incidence and mortality in the United States, 1974–2013JAMA2017317131338134828362912
- MazuratATorroniAHendrickson-RebizantJBenningHNasonRWPathakKAThe age factor in survival of a population cohort of well-differentiated thyroid cancerEndocr Connect20132315416024008393
- PontiusLNOyekunleTOThomasSMProjecting survival in papillary thyroid cancer: a comparison of the seventh and eighth editions of the American joint commission on cancer/Union for International Cancer Control Staging Systems in two contemporary national patient cohortsThyroid201727111408141628891405
- YangLShenWSakamotoNPopulation-based study evaluating and predicting the probability of death resulting from thyroid cancer and other causes among patients with thyroid cancerJ Clin Oncol201331446847423270002
- AdamMAThomasSHyslopTScheriRPRomanSASosaJAExploring the relationship between patient age and cancer-specific survival in papillary thyroid cancer: Rethinking Current Staging SystemsJ Clin Oncol201634364415442027998233
- JonklaasJNogueras-GonzalezGMunsellMNational Thyroid Cancer Treatment Cooperative Study GroupThe impact of age and gender on papillary thyroid cancer survivalJ Clin Endocrinol Metab2012976E878E88722496497
- AdamMAPuraJGoffredoPPresence and number of lymph node metastases are associated with compromised survival for patients younger than age 45 years with papillary thyroid cancerJ Clin Oncol201533212370237526077238
- EvansHLColumnar-cell carcinoma of the thyroid. A report of two cases of an aggressive variant of thyroid carcinomaAm J Clin Pathol198685177803940424
- SujoyVPintoANoséVColumnar cell variant of papillary thyroid carcinoma: a study of 10 cases with emphasis on CDX2 expressionThyroid201323671471923488912
- ChenJHFaquinWCLloydRVNoseVClinicopathological and molecular characterization of nine cases of columnar cell variant of papillary thyroid carcinomaMod Pathol201124573974921358618
- RiveraMTuttleRMPatelSShahaAShahJPGhosseinRAEncapsulated papillary thyroid carcinoma: a clinic-pathologic study of 106 cases with emphasis on its morphologic subtypes (histologic growth pattern)Thyroid200919211912719191744
- EvansHLEncapsulated papillary neoplasms of the thyroid. A study of 14 cases followed for a minimum of 10 yearsAm J Surg Pathol19871185925973618882
- HaugenBRAlexanderEKBibleKC2015American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancerThyroid20162611133
- ItoYHirokawaMUrunoTBiological behavior and prognosis of encapsulated papillary carcinoma of the thyroid: experience of a Japanese hospital for thyroid careWorld J Surg20083281789179418311502
- PisanuADeplanoDRecciaIPorcedduGUcchedduAEncapsulated papillary thyroid carcinoma: is it a distinctive clinical entity with low-grade malignancy?J Endocrinol Invest2013362788322306682
- WenigBMThompsonLDAdairCFShmooklerBHeffessCSThyroid papillary carcinoma of columnar cell type: a clinicopathologic study of 16 casesCancer19988247407539477108
- WoodfordRLNikiforovYEHuntJLEncapsulated papillary oncocytic neoplasms of the thyroid: morphologic, immunohistochemical, and molecular analysis of 18 casesAm J Surg Pathol201034111582159020924280
- SilverCEOwenRPRodrigoJPRinaldoADevaneyKOFerlitoAAggressive variants of papillary thyroid carcinomaHead Neck20113371052105920824810
- FerreiroJAHayIDLloydRVColumnar cell carcinoma of the thyroid: report of three additional casesHum Pathol19962711115611608912824
- LloydRVOsamuraRYKlöppelGRosaiJWHO Classification of Tumours of Endocrine Organs4th ed20178192
- SchneiderDFChenHNew developments in the diagnosis and treatment of thyroid cancerCA Cancer J Clin201363637439423797834
- SchroderSBockerWDralleHKortmannKBSternCThe encapsulated papillary carcinoma of the thyroid. A morphologic subtype of the papillary thyroid carcinomaCancer198454190936722747
- HuangWTYangSFWangSLChanHMChaiCYEncapsulated columnar-cell carcinoma of the thyroid: a case reportKaohsiung J Med Sci200521524124415960072
- ConzoGAveniaNAnsaldoGLSurgical treatment of thyroid follicular neoplasms: results of a retrospective analysis of a large clinical seriesEndocrine201655253053827075721
- ClaudioGErnestoTAnnaNClinical significance of prophylactic central compartment neck dissection in the treatment of clinically node-negative papillary thyroid cancer patientsWorld J Surg Oncol201614124727644091
- CarlingTOcalITUdelsmanRSpecial variants of differentiated thyroid cancer: does it alter the extent of surgery versus well-differentiated thyroid cancer?World J Surg200731591692317345120
- NixonIJSimoRNewboldKManagement of invasive differentiated thyroid cancerThyroid20162691156116627480110
- FusseyJMCrunkhornRTedlaMWeickertMOMehannaHExternal beam radiotherapy in differentiated thyroid carcinoma: a systematic reviewHead Neck201638Suppl 1E2297E230526335228
- TsangRWBrierleyJDSimpsonWJPanzarellaTGospodarowiczMKSutcliffeSBThe effects of surgery, radioiodine, and external radiation therapy on the clinical outcome of patients with differentiated thyroid carcinomaCancer19988223753889445196
- StrasserJFRabenAKoprowskiCThe role of radiation therapy in the management of thyroid cancerSurg Oncol Clin N Am200817121923218177808
- BrierleyJDTsangRWExternal beam radiation therapy for thyroid cancerEndocrin Metab Clin North Am2008372497509
- LeeNTuttleMThe role of external beam radiotherapy in the treatment of papillary thyroid cancerEndocr Relat Cancer200613497197717158749
- MazzarottoRCesaroMGLoraORubelloDCasaraDSottiGThe role of external beam radiotherapy in the management of differentiated thyroid cancerBiomed Pharmacother200054634534910989971
- BillanSCharasTExternal beam radiation in differentiated thyroid carcinomaRambam Maimonides Med J201671
- VermaRPaulPColumnar cell variant of papillary thyroid carcinoma: a diagnostic dilemma in fine-needle aspiration cytologyDiagn Cytopathol2016441081681927279270
- RottuntikarnWWangsiricharoenSRangdaengSCytomorphology and immunocytochemistry of columnar cell variant of papillary thyroid carcinomaCytopathology201728433834128470960
- HirokawaMShimizuMFukuyaTManabeTSonooHColumnar cell carcinoma of the thyroid: MIB-1 immunoreactivity as a prognostic factorEndocr Pathol199891313412114659
