Abstract
Purpose
Radical cystectomy (RC) is an effective but underused treatment for bladder cancer in elderly patients. This study performed analysis of propensity scores (PSs) to determine the outcomes of RC for elderly patients, with results generalizable at the population-based level.
Patients and methods
We conducted a population-based, retrospective cohort study of patients who underwent RC in Taiwan during 2000–2010. Multivariable logistic regression was implemented to evaluate 30- and 90-day mortality and readmission rates, length of intensive care unit (ICU) stay, length of hospital stay (LOS), and cost. Enrolled patients were divided into younger (≤75 years) and older groups (>75 years) who were matched according to their PSs.
Results
We identified 430 patients with bladder cancer who underwent RC between 2000 and 2010. Older age was not significantly associated with 30-day readmission (odds ratio [OR] = 0.80, 95% confidence interval [CI] = 0.38–1.70), 90-day readmission (OR = 1.10, 95% CI = 0.60–2.00), 30-day mortality (OR = 3.07, 95% CI = 0.31–30.0), or 90-day mortality (OR = 2.98, 95% CI = 0.91–9.70) in the PS-matched group. Similar trends were also observed for both groups regarding the mean length of ICU stay, LOS, and overall medical expenditure within the same admission.
Conclusion
No significant differences existed between the older and younger groups for 30-and 90-day mortality and readmission rates, length of ICU stay, LOS, and medical expenditure in patients undergoing RC for bladder cancer. Some healthy elderly patients may be good candidates for this extensive curative treatment.
Introduction
Because of the close association between age and incidence of cancer, it is believed that 70% of cancer diagnoses will be made in people aged 65 years or older in the US by 2030.Citation1 Bladder cancer occurs more often in elderly patients than in younger adults; those older than 70 years have a sevenfold to tenfold increased likelihood.Citation2 With populations becoming more aged, treating people with cancer will be vital in the years ahead. Radical cystectomy (RC) is the standard treatment for patients with muscle-invasive and refractory cancer.Citation3 Although extensive transurethral resection and external radiation therapy in conjunction with systemic chemotherapy have emerged as valid treatment options,Citation4 these alternatives are unlikely to provide a cure and may only extend an individual’s disease-free survival without prolonging their overall survival.Citation5 However, RC can have substantial morbidity, mainly in vulnerable older adults. This surgery is associated with an incidence of postoperative complications of up to 60% and 90-day mortality of approximately 5%–15%;Citation6 therefore, physicians tend not to administer this form of treatment in patients aged 75 years or older.Citation1 Approximately 25% of patients with bladder cancer who are 70–79 years of age undergo RC.Citation5 Nevertheless, after adjustment for tumor grade and stage, RC was associated with the greatest reduction in risk of death from bladder cancer in a previous study (the hazard ratio was 0.3 for cancer-specific survival and 0.4 for all-cause survival).Citation5
Although old age has been determined not to be a risk factor for bladder cancer after RC, detailed data regarding the potential association are lacking. Recognizing the factors that affect postoperative outcome is essential for individual risk adjustment prior to RC. Several studies have reported predictors of complications, perioperative mortality, and readmission.Citation7–Citation11 However, the data are usually obtained from tertiary referral centers, and the results may not be generalizable on a population-based level.
Recent population-based studies have reported nationwide outcomes for patients treated with RC for bladder cancer.Citation7,Citation8,Citation13,Citation14 However, current metrics for quality of care, such as the 30-day and 90-day readmission rates, length of intensive care unit (ICU) stay, length of hospital stay (LOS), and cost, are still lacking, especially for a propensity score (PS)-matched population-based study. Such data would be helpful in assessing the potential risks and benefits of RC, particularly with the current demographic shift that will lead to an increase in unhealthy and elderly patients.
This study performed PS analysis to determine the outcomes of RC for elderly patients, with results generalizable at the population-based level.
Patients and methods
Data source
This study used data obtained from the Registry of Catastrophic Illnesses Patient Database (RCIPD) extracted from the National Health Insurance Research Database of the Taiwan National Health Insurance (NHI) program. The NHI program was launched in March 1995 and provides comprehensive and universal health insurance to all citizens of Taiwan.Citation15 The RCIPD contains registration files and original medical claims data for all beneficiaries, with encryption of unique personal identification to secure patient confidentiality. The details of the RCIPD and NHI program have been provided in previous studies.Citation16,Citation17 Diagnoses were made using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes. This study was approved by the ethics review board of China Medical University (CMUH 104-REC2-115).
Sample participants
From the RCIPD, we identified patients with bladder cancer (ICD-9-CM code 188.9) who were older than 20 years and had undergone RC, including open RC and laparoscopic RC, between 2000 and 2010. The index date was the date on which the patient underwent RC. We excluded patients who were aged younger than 20 years and those with missing data for date of birth or sex. Patients with bladder cancer were classified into two age groups: younger (≤75 years) and older (>75 years). Within each group, patients were matched according to their PSs. The PS was calculated using logistic regression to estimate probabilities between different age group assignments based on the baseline variables: age, monthly income (US$), occupation, urbanization level, index year, and comorbidities of hypertension (ICD-9-CM codes 401-405), ischemic heart disease (ICD-9-CM codes 410-414), chronic obstructive pulmonary disease (ICD-9-CM codes 491, 492, and 496), asthma (ICD-9-CM code 493), and stroke (ICD-9-CM codes 430–438).
Outcome measurements
All patients with bladder cancer who underwent RC were followed from the date of RC to death, withdrawal from the insurance program, or the end of 2011. Postoperative complications were defined to involve readmission within 30 or 90 days and mortality within 30 or 90 days after discharge. We also estimated length of ICU stay, LOS, and overall admission expenditure within the same surgery admission between the younger and older groups.
Statistical analyses
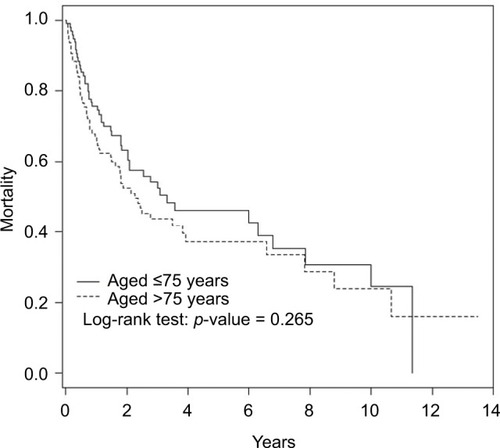
Baseline characteristics were compared between the younger and older groups by using the chi-square test for categorical variables and the two sample t-test for continuous variables. The Kaplan–Meier method was used to plot the survival curves during the follow-up period, and the log-rank test was used to assess the differences between these curves. Univariate and multivariable logistic regression analyses were used to evaluate the effects of age on the risk of 30- or 90-day readmission and 30-day or 90-day mortality, as indicated by the odds ratios (ORs) and 95% confidence intervals (CIs). All statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA). The significance level for all analyses was set to a p-value of 0.05.
Results
lists the baseline characteristics and comorbidity statuses of the patients in the nonmatched and PS-matched cohorts. We identified 430 patients with bladder cancer who underwent RC between 2000 and 2010; we included these patients in the nonmatched cohort. The mean ages of the younger and older groups were 63.3 and 79.2 years, respectively. Both groups tended to have monthly incomes <US$500 (60.5% vs. 60.4%) and worked in blue-collar jobs; comorbidities were more common in the older group, except for asthma and stroke. However, the PS-matched younger and older groups were similar in all baseline characteristics except age. The Kaplan–Meier analysis revealed that the probability of freedom from mortality was not significantly different between the younger and older groups (). presents the ORs of the postoperative complications associated with age. Older age patients were significantly associated with an increased risk of 90-day mortality (OR = 3.71, 95% CI = 1.52–9.07) compared with the younger patients; however, correlations with other postoperative complications, including 30-day readmission after discharge (OR = 0.74, 95% CI = 0.38–1.46), 90-day readmission after discharge (OR = 0.90, 95% CI = 0.54–1.49), and 30-day postoperative mortality (OR = 3.50, 95% CI = 0.78–15.7), were not observed in the nonmatched group. Similar trends were observed in the PS-matched group; however, older age was not significantly associated with 90-day mortality risk (OR = 2.98, 95% CI = 0.91–9.70) in the PS-matched group. The mean (and standard deviation [SD]) values of length of ICU stay, LOS, and overall medical expenditure within the same surgery admission in the older group were similar to those in the younger group ().
Table 1 Demographic characteristics and comorbidity in patients with bladder cancer who underwent cystectomy, with and without PS matching
Table 2 Risk of mortality associated with different age groups in patients with bladder cancer in the multivariable logistic regression model, with and without PS matching
Table 3 Length of ICU stay, LOS, and overall medical expenditure among patients with bladder cancer in different age groups, with and without PS matching
Discussion
After considering both perioperative morbidity and mortality, our study supports RC as a realistic option for treating elderly patients, because elderly patients were equally eligible for RC as younger patients. We calculated the 30-versus 90-day mortality rates of the younger and older groups as 1.04% versus 3.13% and 4.17% versus 11.5%, respectively. Therefore, the 30-day mortality may cause gross underestimation of 90-day mortality after RC in both groups. Thus, for a complete risk assessment, 90-day mortality rates may represent the most valuable calculations, rather than 30-day mortality rates. Compared with younger age, older age was significantly associated with an increased risk of 90-day mortality (OR = 3.71, 95% CI = 1.52–9.07); however, in the PS-matched group, older age was not significantly associated with the risk of 90-day mortality (OR = 2.98, 95% CI = 0.91–9.70). Therefore, age is not a factor of perioperative mortality and should not preclude elderly patients from receiving RC. In particular, compared with other treatment modalities, RC offers patients, even those older than 80 years, the greatest reduction in the risk of death from bladder cancer.Citation18–Citation21 Numerous studies have demonstrated high hospital readmission rates after RC, ranging from 25% to 41%.Citation9,Citation10,Citation22–Citation24 This study found a similar high rate of readmission. Our 30-day readmission rate was similar to that reported by Roghmann et al, who showed that most admissions after RC occurred within 30 days (19.7%).Citation12
Extending the readmission rate analysis beyond the typical 30-day window offers a more thorough comprehension of the morbidity related to RC.Citation25 Specifically, in both the younger and older groups, >30% of patients required hospital readmission within 90 days of surgery, which is higher than the approximate rate of 27% of patients with 90-day readmission shown in a previous study.Citation25 However, unlike our nationally based data, the accuracy of readmission rates derived from a single institution is limited by the researchers’ ability to capture readmissions at nonaffiliated institutions. Therefore, readmission data obtained from single-institution studies represent an underestimation of the actual readmission rate.Citation25 The present national-population-based study was free from the aforementioned limitation; therefore, compared with the single-institute study of a tertiary referral center, the 90-day readmission rate in this study was >30% in both the younger and older groups. Unexpectedly, older age was not a risk factor for 30- and 90-day readmission, because no significant difference was observed between the two groups. Because of the lack of details, we could not confirm whether these readmissions resulted from potentially preventable complications or the progression of surgical disease. Nevertheless, one study revealed that only a small percentage of readmitted patients were confirmed to have an evitable complication of their medical care.Citation26 Therefore, the reasons for readmission after RC warrant further examination.
Our results reveal that overall medical expenditure within the same surgery admission in the older group was similar to that in the younger group. Additionally, the mean (SD) values of length of ICU stay and LOS were not significantly different between the groups. To our knowledge, this is the first study to compare the overall medical expenditure for RC between elderly and younger patients with bladder cancer. This information can be a vital reference for designing a health care strategy for an aging population.
Despite its strengths, this study had limitations. The database used in this study did not include clinical information such as disease stage, disease grade, extent of lymphadenectomy, pathologic tumor characteristics, Clavien grades of postoperative complication, surgical approach (open vs. laparoscopy or robot assisted), and urinary diversion (continent or incontinent).
Conclusion
Using PS matching, we demonstrated that the 30- and 90-day mortality, readmission rate, length of ICU stay, LOS, and cost of RC for patients aged >75 years were comparable to those of their younger counterparts. Our results suggest that decisions for RC should not be based on only age because several other factors influence survival outcomes in patients. Some healthy elderly patients may be good candidates for this extensive curative treatment.
Acknowledgments
This study was supported in part by the Taiwan Ministry of Health and Welfare Clinical Trial and Research Center of Excellence (MOHW105-TDU-B-212-133019); China Medical University Hospital, Academia Sinica Taiwan Biobank, Stroke Biosignature Project (BM10501010037); NRPB Stroke Clinical Trial Consortium (MOST 105-2325-B-039-003); Tseng-Lien Lin Foundation, Taichung, Taiwan; Taiwan Brain Disease Foundation, Taipei, Taiwan; and Katsuzo and Kiyo Aoshima Memorial Funds, Japan.
Author contributions
Wei-Yu Lin and Chia-Hung Kao were involved in study conception and design. All authors carried out analysis and interpretation of data. Wei-Yu Lin and Chia-Hung Kao contributed to preparation of the manuscript. All authors contributed toward data analysis, drafting and critically revising the paper, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- WuethrichPYVidalABurkhardFCThere is a place for radical cystectomy and urinary diversion, including orthotopic bladder substitution, in patients aged 75 and older: results of a retrospective observational analysis from a high-volume centerUrol Oncol201634258e19e27
- GrieblingTLTrends in cancer of the urinary bladder and urinary tract in elderly in Denmark, 2008–2012J Urol2017197317
- IsbarnHJeldresCZiniLA population based assessment of perioperative mortality after cystectomy for bladder cancerJ Urol20091821707719447427
- KulkarniGSHermannsTWeiYPropensity score analysis of radical cystectomy versus bladder-sparing trimodal therapy in the setting of multidisciplinary bladder cancer clinicJ Clin Oncol2017352299230528410011
- ShariatSFMilowskyMDrollerMJBladder cancer in the elderlyUrol Oncol200927665366719879476
- ShabsighAKoretsRVoraKCDefining early morbidity of radical cystectomy for patients with bladder cancer using a standardized reporting methodologyEur Urol200955116417418675501
- GandagliaGVardaBSoodAShort-term perioperative outcomes of patients treated with radical cystectomy for bladder cancer included in the National Surgical Quality Improvement Program (NSQIP) databaseCan Urol Assoc J201489–10E681E68725408807
- RoghmannFTrinhQDBraunKStandardized assessment of complications in contemporary series of European patients undergoing radical cystectomyInt J Urol20142114314923906282
- StimsonCJChangSSBarocasDAEarly and late perioperative outcomes following radical cystectomy: 90-day readmissions, morbidity and mortality in a contemporary seriesJ Urol201018441296130020723939
- HollenbeckBKMillerDCTaubDIdentifying risk factors for potentially avoidable complications following radical cystectomyJ Urol20051744 pt 11231123716145376
- De NunzioCCindoloLLeonardoCAnalysis of radical cystectomy and urinary diversion complications with the Clavien classification system in an Italian real life cohortEur J Surg Oncol201339779279823562571
- RoghmannFSukumarSRaviPRadical cystectomy in the elderly: national trends and disparities in perioperative outcomes and quality of careUrol Int2014921273424052104
- BianchiMTrinhQDSunMImpact of academic affiliation on radical cystectomy outcomes in North America: a population-based studyCan Urol Assoc J2012624525023093532
- KimSPBoorjianSAShahNDContemporary trends of in-hospital complications and mortality for radical cystectomyBJU Int201211081163116822443271
- NHIRDatabase NHIRTaiwan2015 Available from: http://nhird.nhri.org.tw/en/index.htmlAccessed January 1, 2018
- HuangKWKuanYCLuoJCLinCLLiangJAKaoCHImpact of long-term gastric acid suppression on spontaneous bacterial peritonitis in patients with advanced decompensated liver cirrhosisEur J Intern Med201632919527139916
- LeeCWLinCLSungFCLiangJAKaoCHAntidepressant treatment and risk of dementia: a population-based, retrospective case-control studyJ Clin Psychiatry201677111712226845268
- DonatSMSiegristTCroninASavageCMilowskyMIHerrHWRadical cystectomy in octogenarians – does morbidity outweigh the potential survival benefits?J Urol201018362171217720399461
- KonetyBRJoslynSAFactors influencing aggressive therapy for bladder cancer: an analysis of data from the SEER programJ Urol200317051765177114532772
- SchragDMitraNXuFCystectomy for muscle-invasive bladder cancer: patterns and outcomes of care in the Medicare populationUrology20056561118112515922428
- ChappidiMRKatesMStimsonCJCauses, timing, hospital costs and perioperative outcomes of index vs nonindex hospital readmissions after radical cystectomy: implications for regionalization of careJ Urol201719729630127545575
- ShabsighAKoretsRVoraKCDefining early morbidity of radical cystectomy for patients with bladder cancer using a standardized reporting methodologyEur Urol200955116417418675501
- StitzenbergKBChangYSmithABNielsenMEExploring the burden of inpatient readmissions after major cancer surgeryJ Clin Oncol201533545546425547502
- SkolarusTAJacobsBLSchroeckFRUnderstanding hospital readmission intensity after radical cystectomyJ Urol201519351500150625451833
- LowranceWTRumohrJAChangSSClarkPESmithJAJrCooksonMSContemporary open radical Cystectomy: analysis of perioperative outcomesJ Urol200817941313131818289578
- McIntyreLKArbabiSRobinsonEFMaierRVAnalysis of risk factors for patient readmission 30 days following discharge from general surgeryJAMA Surg2016151985586127303913