Abstract
Objective
To compare the survival outcomes in locally advanced breast cancer (LABC) patients receiving post-mastectomy radiotherapy (PMRT) with and without immediate breast reconstruction.
Methods
We used the Surveillance, Epidemiology, and End Results program to include LABC patients who were treated/not treated with immediate breast reconstruction followed by PMRT between 2003 and 2010. Statistical analysis was performed using the chi-squared test, Kaplan–Meier survival analysis, and Cox regression analysis. A 1:1 propensity score matching method was performed to decrease the selection bias.
Results
We identified 1,732 patient-pairs that were completely matched. In the unmatched population, 8,198 and 1,802 patients received mastectomy only and immediate breast reconstruction, respectively. Patients who received immediate breast reconstruction had better breast cancer-specific survival (BCSS) (hazard ratio [HR] 0.880, 95% CI 0.783–0.989, P = 0.032) and overall survival (OS) (HR 0.846, 95% CI 0.758–0.943, P = 0.003) than patients who underwent mastectomy alone. However, in the matched population, there was comparable BCSS and OS between patients who received immediate breast reconstruction and mastectomy alone. Subset analysis in the matched population found that immediate breast reconstruction was associated with better BCSS (HR 0.750, 95% CI 0.614–0.917, P = 0.005) and OS (HR 0.779, 95% CI 0.644–0.942, P = 0.010) compared to patients aged <50 years who received mastectomy alone.
Conclusion
There are comparable survival outcomes in LABC patients who received immediate breast reconstruction or mastectomy alone followed by PMRT. However, patients aged <50 years had a survival advantage after immediate breast reconstruction.
Introduction
Locally advanced breast cancer (LABC) is most commonly defined as stage III disease, and mastectomy and lymphadenectomy are the standard surgical procedures for LABC, while postoperative mastectomy radiotherapy (PMRT) could significantly decrease locoregional recurrence and confer additional survival advantage.Citation1,Citation2 Patients who undergo mastectomy deal with impaired sexual characteristics and body image, which may negatively impact the quality of life. These drawbacks may be effectively compensated in some women by breast reconstruction using autologous tissue or implant, especially when performed immediately following mastectomy. Patients who received breast reconstruction may then still experience positive self-perception and natural appearance, although complications may affect the cosmetic effects.
Although several studies have indicated that immediate breast reconstruction in breast cancer is both feasible and oncologically safe, PMRT for patients who underwent immediate breast reconstruction may lead to higher rates of adverse events including reconstruction failure, capsular contracture, and overall complications.Citation3–Citation9 Patients who received implant reconstruction had a significantly higher incidence of reconstruction failure compared to autologous reconstruction after PMRT.Citation6 In addition, in patients who had not experienced reconstruction failure, PMRT after autologous reconstruction was associated with a superior patient-reported satisfaction and a higher psychosocial or physical well-being than implant reconstruction followed by PMRT.Citation3 Therefore, patients who are eligible to receive PMRT are less likely to receive immediate breast reconstruction,Citation10 and anticipation of PMRT may lead to delay or omission of breast reconstruction. However, attitudes toward breast reconstruction in the setting of planned PMRT are changing. According to the Surveillance, Epidemiology, and End Results (SEER) results program from 2000 to 2010, the proportion of immediate breast reconstruction among patients receiving PMRT increased from 13.6% to 25.1%.Citation11 However, another SEER study also found that an increase in PMRT was not associated with a decrease in those receiving reconstruction.Citation12 There are conflicting results with regard to survival outcomes in LABC patients who receive immediate breast reconstruction followed by PMRT. Some studies have indicated that no statistically significant differences were found in survival outcomes between those receiving breast reconstruction and mastectomy alone.Citation13–Citation15 In contrast, a study showed that patients who received breast reconstruction had better breast cancer-specific survival (BCSS) than patients who underwent mastectomy alone.Citation16 The heterogeneity of the population and the difference in sample size may be the main reasons for these contrasting results.
Population-based cancer registry includes a wide range of patient demographics and avoids the inherent bias observed in single institution studies, thereby allowing for greater generalization. In the current study, we used the SEER database to determine the clinical characteristics and survival outcomes of patients with LABC who received immediate breast reconstruction or mastectomy alone, followed by PMRT.
Materials and methods
Patients
The SEER database is maintained by the National Cancer Institute and includes demographics, incidence, and cancer-specific survival data for ~28% of the population in the USA.Citation17 The present study was based on the publicly available SEER database, and we have obtained the permission to access them with the reference number 11025-Nov 2016. To investigate the effect of immediate breast reconstruction (reconstruction within 4 months of mastectomy as defined by SEERCitation18,Citation19) on the long-term survival of patients, we included patients diagnosed with breast cancer between 2004 and 2010. Patients who met the following criteria were included: 1) histologically confirmed breast cancer; 2) American Joint Committee on Cancer, sixth edition, tumor–node–metastasis staging system staged T1–4N2–3M0; 3) receiving mastectomy alone or immediate breast reconstruction including reconstruction not otherwise specified, tissue, implant, or combined with tissue and implant reconstruction; 4) receiving PMRT (beam radiation) and chemotherapy; 5) variables including age, race/ethnicity, grade, estrogen receptor (ER) status, progesterone receptor (PR) status, and marital status. Patients who received preoperative or intraoperative radiotherapy were excluded. The ethics committee of the First Affiliated Hospital of Xiamen University approved this study.
The following demographic, clinicopathologic, and treatment data were collected: age and year at diagnosis, race/ethnicity, grade, T stage, N stage, hormone receptors status, marital status, and reconstruction methods. The primary survival points were BCSS and overall survival (OS). BCSS and OS were defined as the time interval from initial diagnosis until breast cancer-related death or death from any cause, respectively.
Statistical analysis
The differences in demographic and clinicopathologic variables between immediate breast reconstruction and mastectomy alone were compared using the chi-squared test. To decrease the impact of potential selection bias in the retrospective studies, a one-to-one propensity score matching (PSM) method was performed using the following variables: age, race/ethnicity, grade, T stage, N stage, ER status, PR status, and marital status.Citation20,Citation21 BCSS and OS were assessed using Kaplan–Meier survival methods and compared with a log-rank test. Cox proportional hazards regression was used to evaluate the variables and potential association with BCSS and OS. Variables with statistical significance by univariate analysis were entered into multivariate analysis. Hazard ratios (HRs) with the corresponding 95% CIs were calculated to assess the risk of death. All statistical analyses were performed using the SPSS software package, version 22.0 (IBM Corporation, Armonk, NY, USA). The level of statistical significance was defined at P <0.05.
Results
Patient characteristics
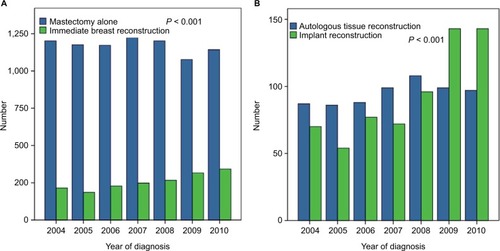
We included 10,000 breast cancer patients with stage T1–4N2–3M0 who met the inclusion criteria. These included 8,198 (82.0%) patients receiving mastectomy alone and 1,802 (18.0%) patients who received immediate breast reconstruction. In patients who received immediate breast reconstruction, 664 (36.8%) patients received autologous tissue reconstruction, 655 (36.3%) patients received implant reconstruction, and 483 (26.8%) patients had reconstruction that was not otherwise specified or combined with tissue and implant reconstruction. The number of patients undergoing immediate breast reconstruction increased from 2004 to 2010 (P < 0.001; ). In addition, more patients were likely to receive breast reconstruction with autologous tissue implantation before 2008 (55.9% vs 44.1%), while more patients were likely to receive breast reconstruction with implantation in 2009 and 2010 (59.3% vs 40.7%) (P < 0.001; ). The patient features of the entire cohort are summarized in .
Table 1 Patient characteristics before and after propensity score matching
Survival and prognostic analysis in the unmatched population
The median follow-up period was 61 months (range 3–119 months). The 5-year BCSS and OS were 78.3% and 74.4%, respectively. The 5-year BCSS in patients who received breast reconstruction and mastectomy alone was 82.4% and 77.4%, respectively (P < 0.001; ), while the 5-year OS was 80.3% and 73.1%, respectively (P < 0.001; ). There was comparable BCSS (P = 0.998) and OS (P = 0.921) in patients who received autologous tissue reconstruction or implant reconstruction.
Figure 2 Survival comparison (A, breast cancer-specific survival; B, overall survival) in unmatched population with and without immediate breast reconstruction.
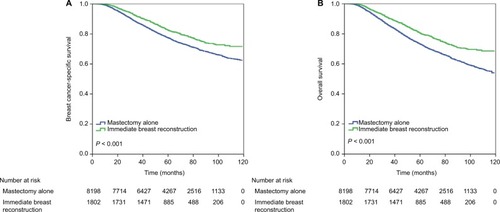
In the univariate and multivariate Cox analyses (), immediate breast reconstruction was associated with better BCSS (HR 0.880, 95% CI 0.783–0.989, P = 0.032) and OS (HR 0.846, 95% CI 0.758–0.943, P = 0.003) compared to patients who underwent mastectomy alone. Age at diagnosis, race/ethnicity, tumor grade, T stage, N stage, hormone receptor status, and marital status were also independent prognostic factors included in the multivariate analysis.
Table 2 Univariate and multivariate Cox regression analyses of prognostic factors before propensity score matching
Prognostic analysis in the matched population
A total of 1,732 pairs of patients were completely matched. The patient features of the matched population are listed in . There were comparable BCSS (P = 0.267; ) and OS (P = 0.313; ) in patients who received breast reconstruction and mastectomy alone in the matched population.
Figure 3 Survival comparison (A, breast cancer-specific survival; B, overall survival) in matched population with and without immediate breast reconstruction.
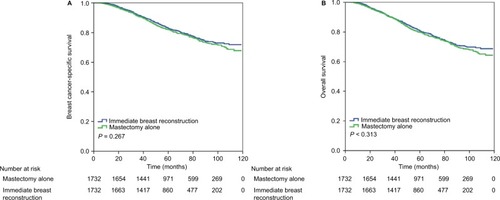
The results of univariate analyses showed that immediate breast reconstruction was not associated with a better BCSS (HR 1.088, 95% CI 0.937–1.2629, P = 0.268) or OS (HR 1.074, 95% CI 0.935–1.235, P = 0.314) compared to patients who underwent mastectomy alone (). Tumor grade, T stage, N stage, hormone receptor status, and marital status were also independent prognostic factors in the multivariate analysis of the matched population ().
Table 3 Univariate and multivariate Cox regression analyses of prognostic factors after propensity score matching
Subset analysis in the matched population
We further performed a subset analysis in the matched population, and the results showed that breast reconstruction had no effect on BCSS and OS for all the demographic and clinicopathologic variables, except in patients aged <50 years. In Kaplan–Meier survival analysis, the BCSS (P = 0.012; ) and OS (P = 0.023; ) were better in those patients who underwent immediate breast reconstruction compared to patients who received mastectomy alone.
Figure 4 Survival comparison (A, breast cancer-specific survival; B, overall survival) in matched population who are <50 years of age with and without immediate breast reconstruction.
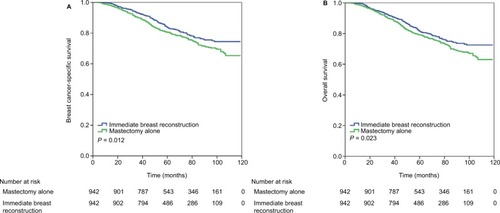
After adjustment by race/ethnicity, tumor grade, T stage, N stage, hormone receptor status, and marital status, patients who received immediate breast reconstruction still had better BCSS (HR 0.750, 95% CI 0.614–0.917, P = 0.005) and OS (HR 0.779, 95% CI 0.644–0.942, P = 0.010) than those treated with mastectomy alone ().
Table 4 Multivariate Cox regression analysis of prognostic factors after propensity score matching in patients aged <50 years
Discussion
In this study, we explored the effect of immediate breast reconstruction on LABC patients after PMRT. Our results showed that breast reconstruction significantly improved survival outcomes in unpaired patients. However, the advantage of breast reconstruction on survival disappeared in the matched group, except for patients aged <50 years.
Breast reconstruction is associated with better cosmetic results and quality of life. Anticipation of PMRT might lead to a delay or result in omission of reconstruction. However, a population-based study found that an increase in the use of PMRT was not associated with a decrease in breast reconstruction surgery.Citation12 In this study, our results showed an increased trend in immediate breast reconstruction in LABC followed by PMRT, and the number of patients who received implant reconstruction was significantly higher in 2009 and 2010 compared to the period of 2004–2008. A previous SEER study also found that the national increases in PMRT receipt in patients with tumors ≤5 cm and one to three positive nodes were not accompanied by a decrease in receipt of breast reconstruction. This may represent increasing radiation oncologists’ comfort by the prospect of irradiating to breast reconstruction, with improved cosmetic outcomes and quality of life for patients.Citation12 However, the two SEER studies including ours did not include complications after breast reconstruction or whether patient implants are reconstructed as one- or two-stage events.
Several studies have found that patients who received breast implant-based reconstruction followed by PMRT had a higher rate of postoperative morbidity including reconstructive failure, surgical site infection, repeat surgery, and total complications than their autologous tissue reconstruction counterparts.Citation22–Citation24 This might have a significantly negative effect on patient satisfaction and cosmetic outcomes.Citation25 A nationwide data found that implant reconstruction was on average of less cost than autologous reconstruction. However, implant reconstruction was associated with a significantly higher rate of reconstruction failure than autologous reconstruction of the irradiated breast (32% vs 5%), and the cumulative cost was six times more among implant reconstruction group compared to patients who underwent autologous methods because of the significant difference in the respective reconstruction failure rates.Citation6 It is worth noting that delayed implant reconstruction may minimize certain complications compared to immediate implant reconstruction.Citation26 Therefore, as the frequency of immediate breast reconstruction in breast cancer continues to increase, even in the setting of PMRT, a delay in implant reconstruction or autologous tissue reconstruction may be an optimal reconstructive choice. In addition, administration of radiotherapy before mastectomy may avoid sequencing difficulties in patients suitable for breast reconstruction.Citation27,Citation28
Although recent studies have indicated that immediate breast reconstruction is oncologically safe, this form of treatment for LABC remains controversial because of the higher rates of adverse events after administration of PMRT.Citation3–Citation9 A study from Hsieh et al included 192 patients with LABC and 62% of these patients received PMRT, with the results showing that breast reconstruction was an independent predictor for survival. The breast reconstruction group had a signifi-cantly lower risk of breast cancer-related death (P = 0.019) compared to the group that only received mastectomy.Citation16 However, a study by Lee et al included 492 stage II and III breast cancer patients who underwent chemotherapy followed by PMRT. The results showed that there was no statistically significant difference in local and distant recurrence, disease-free survival, and OS compared to the immediate reconstruction group.Citation13 Similarly, Hazard et al found no difference in locoregional recurrence, disease-free status, and OS in the setting of immediate breast reconstruction or mastectomy alone followed by PMRT.Citation14 Moreover, Soong et al demonstrated similar locoregional control and OS between the two groups.Citation15
In our study, we found that patients who underwent breast reconstructions in the unmatched populations had better survival compared to mastectomy alone, which was similar to the previous SEER study assessing stage I–IV breast cancer regardless of the use of PMRT.Citation29,Citation30 Women who underwent breast reconstruction were more likely to be younger, be married, have a higher family income and education level, have a better overall health status, have hormone receptor-positive disease, and be diagnosed at an early stage.Citation16,Citation29–Citation31 These findings were in agreement with our results. We believe that this association between breast reconstructions and survival in the unmatched population was more likely to be attributed to imbalances in socioeconomic, tumor, and treatment factors. In our study, we used the PSM method to reduce the potential selection bias in retrospective studies, and we did not find any relationship between breast reconstruction and patient survival after PSM.
Although our study lacked data on patients with local recurrence, it has been suggested that previous adipocytes may play a major role in breast cancer recurrence. Manabe et al showed that mature adipose cells can promote formation of breast carcinoma cells in a collagen gel matrix culture.Citation32 A matched cohort study also found a higher risk of local recurrence in patients undergoing the process of lipomodeling.Citation33 Therefore, autologous tissue reconstruction may present with poor outcome compared to the implant reconstruction group. However, a recent study indicated that immediate autologous tissue reconstruction in the setting of PMRT did not increase the occurrence of local and distant events, and did not decrease breast cancer-related death.Citation34 Fertsch et al used a matching analysis, and their study found no general increased risk of recurrence between the lipomodeling and control group.Citation35 In our study, we did not observe significant differences in survival outcomes between the two reconstruction methods. As all patients in our study received PMRT, we believe that this may have decreased the risk of locoregional recurrence. Therefore, the survival outcomes may not be significantly different in our study.
Women younger than 50 years have a higher likelihood of receiving mastectomy followed by breast reconstruction compared to older patients,Citation36 and this was similar to our results. In addition, our subset analysis found that breast reconstruction was associated with better survival outcomes than for patients who underwent mastectomy alone and who were younger than 50 years in the matched population. The physiologic or immunologic effects in younger reconstruction patients may be the main reason for better survival in immediate breast reconstruction group as compared to patients who received mastectomy without immediate breast reconstruction.Citation37 In the People’s Republic of China, the rate of breast reconstruction is <5%, which is significantly lower than in Western countries.Citation12,Citation38 In addition, the median age for breast cancer is 48–50 years in the People’s Republic of China compared to 64 years in the USA. In addition, mastectomy continues to account for ~90% of Chinese patients.Citation39 Therefore, our study has great significance in decision making of clinical practice for Chinese women.
Inevitably, there are several limitations in our study that should be acknowledged. First, our study was a retrospective study, which might introduce unaccounted biases. Second, the SEER database only included immediate breast reconstruction data, and patients who had undergone delayed breast reconstruction were not analyzed in our study. Some patients may have completed their reconstruction only after the follow-up time was computed. Third, we could not investigate the effect of local recurrence, cosmetic outcome, and treatment-related complications after PMRT between the two reconstruction methods. In addition, confounders such as comorbidities, body mass index, smoking, performance status, insurance type (SEER recorded the insurance status after 2007, and only 136 patients were uninsured), or clinician- and patient-related preferences can influence decision making in daily clinical practice. However, SEER database also lacks the abovementioned variables. The lack of data regarding human epidermal growth factor receptor 2 status, radiotherapy dosage, and chemotherapy regimen was another limitation.
Conclusion
In conclusion, our results suggest that there are comparable survival outcomes in LABC patients who received immediate breast reconstruction or mastectomy alone followed by PMRT, except in patients who were younger than 50 years of age. These younger patients appeared to have a survival advantage after immediate breast reconstruction. Our results demonstrate the survival outcomes in relation to immediate breast reconstruction followed by PMRT for both the physicians and the patients.
Acknowledgments
This work was partly supported by the Natural Science Foundation of Fujian Province (No. 2016J01635), the Science and Technology Planning Projects of Xiamen Science & Technology Bureau (No. 3502Z20174070), and Guangdong Medical Research Foundation (No. A2017023).
Disclosure
The authors report no conflicts of interest in this work.
References
- OvergaardMHansenPSOvergaardJPostoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. Danish Breast Cancer Cooperative Group 82b TrialN Engl J Med1997337149499559395428
- KatzAStromEABuchholzTALocoregional recurrence patterns after mastectomy and doxorubicin-based chemotherapy: implications for postoperative irradiationJ Clin Oncol200018152817282710920129
- JagsiRMomohAOQiJImpact of radiotherapy on complications and patient-reported outcomes after breast reconstructionJ Natl Cancer Inst20181102
- RicciJAEpsteinSMomohAOLinSJSinghalDLeeBTA meta-analysis of implant-based breast reconstruction and timing of adjuvant radiation therapyJ Surg Res201721810811628985836
- ChenCFHungCFLinSFChungYLDoes prosthesis-based breast reconstruction affect the clinical outcome of postmastectomy radiotherapy?Ann Plast Surg2018802S Suppl 1S7S1029369903
- AliuOZhongLChettaMDComparing health care resource use between implant and autologous reconstruction of the irradiated breast: a national claims-based assessmentPlast Reconstr Surg201713961224e1231e
- MagillLJRobertsonFPJellGMosahebiAKeshtgarMDetermining the outcomes of post-mastectomy radiation therapy delivered to the definitive implant in patients undergoing one- and two-stage implant-based breast reconstruction: a systematic review and meta-analysisJ Plast Reconstr Aesthet Surg201770101329133528743588
- ChubaPJStefaniWADulCRadiation and depression associated with complications of tissue expander reconstructionBreast Cancer Res Treat2017164364164728503719
- El-SabawiBHoALSosinMPatelKMPatient-centered outcomes of breast reconstruction in the setting of post-mastectomy radiotherapy: a comprehensive review of the literatureJ Plast Reconstr Aesthet Surg201770676878028416138
- JagsiRJiangJMomohAOTrends and variation in use of breast reconstruction in patients with breast cancer undergoing mastectomy in the United StatesJ Clin Oncol201432991992624550418
- AgarwalSKidwellKMFarbergAKozlowJHChungKCMomohAOImmediate reconstruction of the radiated breast: recent trends contrary to traditional standardsAnn Surg Oncol20152282551255925564172
- FrasierLLHoldenSHoldenTTemporal trends in postmas-tectomy radiation therapy and breast reconstruction associated with changes in national comprehensive cancer network guidelinesJAMA Oncol2016219510126539936
- LeeHHHouMFWeiSYComparison of long-term outcomes of postmastectomy radiotherapy between breast cancer patients with and without immediate flap reconstructionPLoS One2016112e014831826863006
- HazardLMiercortCGaffneyDLeavittDStewartJRLocal-regional radiation therapy after breast reconstruction: what is the appropriate target volume? A case-control study of patients treated with electron arc radiotherapy and review of the literatureAm J Clin Oncol200427655556415577432
- SoongISYauTKHoCMPost-mastectomy radiotherapy after immediate autologous breast reconstruction in primary treatment of breast cancersClin Oncol (R Coll Radiol)200416428328915214653
- HsiehTYLinYNLinSDImmediate transverse rectus abdomi-nis musculocutaneous flap reconstruction is associated with improved cancer-specific survival in locally advanced breast cancerAnn Plast Surg201473Suppl 1S31S3625003450
- Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov)SEER*Stat Database: Incidence-SEER 18 Regs Custom Data (with chemotherapy recode), Nov 2015 Sub (2000–2013) <Katrina/Rita Population Adjustment>-Linked To County Attributes-Total U.S., 1969–2014 CountiesNational Cancer Institute, DCCPS, Surveillance Research Program released July 2016, based on the November 2015 submission
- AgarwalJAgarwalSPappasLNeumayerLA population-based study of breast cancer-specific survival following mastectomy and immediate or early-delayed breast reconstructionBreast J201218322623222487264
- WuWChengSDengHWuJMaoKCaoMImpact of breast cancer subtype defined by immunohistochemistry hormone receptor and HER2 status on the incidence of immediate postmastectomy reconstructionMedicine (Baltimore)2016953e254726817902
- RosenbaumPRRubinDBConstructing a control group using multivariate matched sampling methods that incorporate the propensity scoreAm Stat19853913338
- AustinPCAn introduction to propensity score methods for reducing the effects of confounding in observational studiesMultivariate Behav Res201146339942421818162
- TsoiBZiolkowskiNIThomaACampbellKO’ReillyDGoereeRSafety of tissue expander/implant versus autologous abdominal tissue breast reconstruction in postmastectomy breast cancer patients: a systematic review and meta-analysisPlast Reconstr Surg2014133223424924469159
- El-SabawiBSosinMCareyJNNahabedianMYPatelKMBreast reconstruction and adjuvant therapy: a systematic review of surgical outcomesJ Surg Oncol2015112545846426345465
- BarryMKellMRRadiotherapy and breast reconstruction: a meta-analysisBreast Cancer Res Treat20111271152221336948
- MagillLJRobertsonFPJellGMosahebiAKeshtgarMDetermining the outcomes of post-mastectomy radiation therapy delivered to the definitive implant in patients undergoing one- and two-stage implant-based breast reconstruction: a systematic review and meta-analysisJ Plast Reconstr Aesthet Surg201770101329133528743588
- SethAKSilverHRHirschEMKimJYFineNAComparison of delayed and immediate tissue expander breast reconstruction in the setting of postmastectomy radiation therapyAnn Plast Surg201575550350725180955
- TansleyPRamseyKWongSGuerrieriMPitcherMGrinsellDNew treatment sequence protocol to reconstruct locally advanced breast cancerANZ J Surg201383963063523496238
- PaillocherNFlorczakASRichardMEvaluation of mastectomy with immediate autologous latissimus dorsi breast reconstruction following neoadjuvant chemotherapy and radiation therapy: a single institution study of 111cases of invasive breast carcinomaEur J Surg Oncol201642794995527134148
- BezuhlyMTempleCSigurdsonLJDavisRBFlowerdewGCookEFJrImmediate postmastectomy reconstruction is associated with improved breast cancer-specific survival: evidence and new challenges from the Surveillance, epidemiology, and end results databaseCancer2009115204648465419634163
- JiangYZLiuYRYuKDZuoWJShaoZMImmediate postmastectomy breast reconstruction showed limited advantage in patient survival after stratifying by family incomePLoS One2013812e8280724349366
- AgarwalSLiuJHCriseraCABuysSAgarwalJPSurvival in breast cancer patients undergoing immediate breast reconstructionBreast J201016550350920604794
- ManabeYTodaSMiyazakiKSugiharaHMature adipocytes, but not preadipocytes, promote the growth of breast carcinoma cells in collagen gel matrix culture through cancer-stromal cell interactionsJ Pathol2003201222122814517839
- PetitJYRietjensMBotteriEEvaluation of fat grafting safety in patients with intraepithelial neoplasia: a matched-cohort studyAnn Oncol20132461479148423393126
- MaaloufCBou-MerhiJKaramEPatocskaiEDaninoAMThe impact of autologous breast reconstruction using DIEP flap on the oncologic efficacy of radiation therapyAnn Chir Plast Esthet201762663063628760638
- FertschSHagouanMMunderBIncreased risk of recurrence associated with certain risk factors in breast cancer patients after DIEP-flap reconstruction and lipofilling – a matched cohort study with 200 patientsGland Surg20176431532328861370
- MorrowMScottSKMenckHRMustoeTAWinchesterDPFactors influencing the use of breast reconstruction postmastectomy: a National Cancer Database studyJ Am Coll Surg200119211811192909
- HoshawSJKleinPJClarkBDCookRRPerkinsLLBreast implants and cancer: causation, delayed detection, and survivalPlast Reconstr Surg200110761393140711335807
- ChenYChenJChenJCurrent trends of breast reconstruction after mastectomy for breast cancer patients in China: a survey reportZhonghua Zhong Liu Za Zhi20143611851857 Chinese25620484
- FanLStrasser-WeipplKLiJJBreast cancer in ChinaLancet Oncol2014157e279e28924872111