Abstract
Purpose
Gastric cancer (GC) is one of the most common malignancies and has a high mortality rate. In recent years, several nutritional or inflammatory biomarkers have been shown to effectively predict the prognosis of tumors. In this study, we intended to establish a prognostic scoring system for GC patients.
Patients and methods
Our study included a total of 501 GC patients who were diagnosed with GC stage I–III and received curative gastrectomy with D2 lymphadenectomy between January 2011 and December 2012. Survival analysis was performed using Kaplan–Meier and log-rank tests. Two Cox multivariate models, one for continuous and one for categorical variables, were established to identify independent prognostic factors. All statistical analyses were performed using SPSS 20.0.
Results
Univariate and multivariate analyses revealed that tumor-node-metastasis (TNM) stage, preoperative prognostic nutritional index (PNI), and adjuvant therapy were independent prognostic factors for GC patients. We established a new composite variable, TNM-PNI, which was confirmed to be a major prognostic factor for curative D2 resection, independent of whether adjuvant therapy was administered. GC patients with higher TNM-PNI scores always had worse cancer outcomes. In addition, we found that adjuvant therapy might be beneficial for the survival of GC patients with TNM-PNI =4 or 5.
Conclusion
Preoperative PNI plays a distinctly subsidiary role to the TNM stage when predicting patient prognosis. TNM-PNI is a novel and an effective prognostic index for GC patients with curative D2 resection and a good supplement for the National Comprehensive Cancer Network Guidelines.
Introduction
Gastric cancer (GC) is the fourth most common malignancy and the second leading cause of cancer-related death worldwide.Citation1 GC patients from China account for ~40% of the total global incidence. Surgery with adjuvant therapy is the preferred intervention for GC, and gastrectomy with D2 lymphadenectomy has become the standard procedure. This intervention is especially common in East Asia because of the high incidence rate of GC. Despite surgical intervention, the 5-year survival rate of GC patients is <40%, even after curative resection. Therefore, identifying accurate prognostic factors and an effective scoring system to predict the survival time of GC patients is imperative for improving the treatment of GC.
In recent years, nutritional and inflammatory status have been recognized as factors for predicting cancer outcomes.Citation2 Several studies have reported on preoperative biomarkers and composite indexes, such as albumin,Citation3 platelet count, body mass index (BMI), Glasgow Prognostic Score (GPS),Citation4,Citation5 neutrophil–lymphocyte ratio (NLR),Citation6–Citation8 and prognostic nutritional index (PNI).Citation9–Citation11 While all these biomarkers are easily measured, noninvasive, and effective, it is still controversial which of them represents the best predictor of GC prognosis.
In this retrospective study, we intended to investigate independent prognostic factors of GC and to establish a novel prognostic scoring system for patients who are treated with curative D2 resection. The results of this study are expected to improve the prediction of GC prognosis and guide the development of postoperative treatment strategies for surgeons.
Patients and methods
Patient selection
We retrospectively analyzed the clinicopathologic and follow-up data of 501 patients who were diagnosed with GC and received curative D2 resection at the First Affiliated Hospital of China Medical University from January 2011 to December 2012. Gastrectomy with D2 lymphadenectomy was performed according to the guidelines of the Japanese Research Society for Gastric Cancer. The inclusion criteria of patients were as follows: 1) GC was confirmed as stage I–III by histopathology, 2) curative D2 resection was performed without neoadjuvant chemo-radiotherapy, 3) postoperative adjuvant therapy regimens included chemotherapy or targeted therapy, and 4) detailed clinicopathologic and follow-up data were obtained for every patient. Furthermore, among the 501 patients, 268 stage II–III patients with adjuvant therapy and another 192 stage I–III patients without adjuvant therapy were selected to identify the prognostic value of the novel scoring system of the National Comprehensive Cancer Network (NCCN) guidelines for GC. This research was approved by the Ethics Committee of China Medical University, and written informed consent for this study was obtained from each patient.
Data collection
We collected the following data for each patient: age, gender, tumor size (longest diameter), radical degree, histological type, tumor-node-metastasis (TNM) stage, albumin level, platelet count, fibrinogen level, NLR, platelet–lymphocyte ratio (PLR), PNI, adjuvant therapy, and OS time. Routine laboratory analysis of blood was performed 7 days preoperatively. Cutoff values for biomarkers were determined by their Youden index of the receiver operating characteristic curve and the results of previous studies. Follow-up was completed by December 2017. TNM stages were classified according to the 7th edition of the American Joint Committee on Cancer (AJCC) classification system.
Definition of NLR, PLR, and PNI
NLR was calculated as neutrophil count (per mm3)/lymphocyte count (per mm3), PLR was calculated as platelet count (per mm3)/lymphocyte count (per mm3), and PNI was calculated as 10-fold albumin concentration (g/dL) plus 0.005-times total lymphocyte count (per mm3). For subsequent calculations, patients with PNI ≤49 were assigned PNI =1 and patients with PNI >49 were assigned PNI =2.
Definition of TNM-PNI
A novel prognosis scoring system, “TNM-PNI,” was established combining TNM and PNI, both of which were found to be independent prognostic factors in our analysis. We assigned a score of 1–3 to the relative TNM stage (I–III) and a score of 1–2 to PNI (1–2). Finally, based on the results of the B value and hazard ratio (HR) value in Model 2 of the Cox analysis, we calculated the TNM-PNI score for each patient according to the formula: TNM-PNI = 2 × TNM score – 1 × PNI score.
Statistical analysis
Continuous and categorical variables were expressed as mean ± SD and frequency, respectively. To identify the independent prognostic factors, we performed univariate and multivariate analyses with the Cox proportional hazards model. Two models were established in the Cox analysis, one including the continuous variables and the other including the categorical variables. Correlation analyses between preoperative PNI and other characteristics were performed by independent sample t-tests and chi-square tests. In addition, Kaplan–Meier analysis and the log-rank test were used to evaluate the difference in prognosis between TNM-PNI groups. Statistical analysis was performed using SPSS 20.0, and p<0.05 was considered to be statistically significant.
Results
Clinicopathologic characteristics
We retrospectively included 501 patients with stage I–III GC in this study. Their baseline clinicopathologic characteristics are shown in . There were 364 male (72.7%) and 137 female (27.3%) patients, and the mean age was 59.2 years. Of the 501 patients, 114 (22.8%) had stage I, 139 (27.7%) had stage II, and 248 (49.5%) had stage III. The mean follow-up period was 43.1 months. Furthermore, the 1-, 3-, and 5-year OS rates of the patients were 85.0%, 62.1%, and 53.9%, respectively. Among the 501 patients, 309 received postoperative adjuvant therapy and 86.7% (268/309) were diagnosed with stage II–III.
Table 1 General characteristics of 501 GC patients with curative D2 resection
Results of the univariate and multivariate analysis
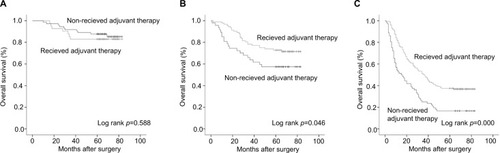
The univariate analysis revealed that age, gender, tumor size, radical degree, TNM stage, albumin, fibrinogen, NLR, PLR, and PNI might be associated with the prognosis of GC patients (p<0.05). Both multivariate models of the Cox analysis, using continuous and categorical variables, respectively, showed that TNM stage [Model 1: HR (95% CI) =2.965 (2.378–3.698), p=0.000; Model 2: HR (95% CI) =2.957 (2.369–3.690), p=0.000], PNI [Model 1: HR (95% CI) =0.972 (0.954–0.991), p=0.004; Model 2: HR (95% CI) =0.647 (0.497–0.844), p=0.001], and adjuvant therapy [Model 1: HR (95% CI) =0.569 (0.434–0.747), p=0.000; Model 2: HR (95% CI) =0.567 (0.432–0.745), p=0.000] are the independent prognostic factors of the OS for patients with curative D2 resection (). Higher TNM stage or lower preoperative PNI was always associated with worse prognosis of GC. Moreover, adjuvant therapy, as another major prognostic factor, could improve the long-term OS of stage II–III, but not that of patients with stage I in our study ().
Table 2 Univariate and multivariate survival analysis of OS in 501 GC patients with curative D2 resection
Relationship between PNI and other characteristics
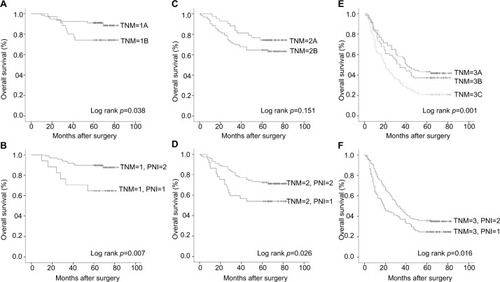
The preoperative PNI level was associated with age, tumor size, TNM stage, albumin level, fibrinogen level, NLR, and PLR (p<0.05) (). Notably, patients with a high PNI (>49) were always relatively younger, had smaller sized tumors, and presented with an earlier TNM stage compared with patients in the low-PNI group. Furthermore, we found that PNI could effectively predict the prognosis of TNM stages, especially for GC stages I and II ().
Prognostic value of TNM-PNI
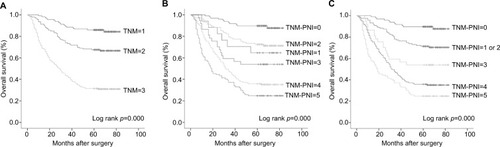
Relative to TNM stage, the TNM-PNI system showed improved accuracy in predicting prognosis (), and a higher TNM-PNI score always indicated worse OS of GC. Because the difference in prognoses did not reach statistical significance, we generalized TNM-PNI =1 and 2 as a single group (). By Cox multivariate analysis, TNM-PNI [Model 1 and Model 2: HR (95% CI) =1.812 (1.632–2.010), p=0.000] and adjuvant therapy [Model 1 and Model 2: HR (95% CI) =0.597 (0.456–0.782), p=0.000] were demonstrated to be the major independent prognostic factor for our 501 GC patients ().
Figure 3 OS curves of TNM stage and the “TNM-PNI” scoring system for GC patients with curative D2 resection. (A) TNM stage; (B) TNM-PNI scoring system; (C) adjusted TNM-PNI scoring system (generalizing TNM-PNI =1 and 2 as one group).
Abbreviations: OS, overall survival; TNM, tumor-node-metastasis; PNI, prognostic nutritional index; GC, gastric cancer.
Role of TNM-PNI for NCCN guidelines
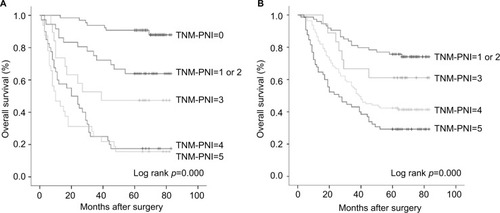
According to the NCCN guidelines for GC, for the postoperative management of D2 gastrectomy, a total of 268 patients with stage II–III were included as the adjuvant group, while the other 192 patients with stage I–III were included as the non-adjuvant group. The Cox analysis with both models identified the TNM-PNI score as the only independent prognostic factor of GC, whether adjuvant therapy was administered or not [non-adjuvant: Model 1 and Model 2: HR (95% CI) =1.923 (1.656–2.234), p=0.000; adjuvant: Model 1 and Model 2: HR (95% CI) =1.649 (1.391–1.953), p=0.000] (). As shown in , the TNM-PNI scoring system could effectively predict the prognosis of GC patients. For patients without adjuvant therapy, there was no significant difference in the prognosis between patients with TNM-PNI =4 and 5 (). However, as shown in , we found that adjuvant therapy might be beneficial for GC patients with TNM-PNI =4 or 5, as they had significantly better long-term survival rates than patients in the non-adjuvant therapy group (p<0.05).
Table 3 Multivariate survival analysis of OS in GC patients with curative D2 resection according to the NCCN guidelines
Table 4 The 1-, 3-, and 5-year survival rate of the TNM-PNI prognostic score system for GC patients with curative D2 resection according to NCCN guidelines
Figure 4 Prognostic value of “TNM-PNI” for GC patients with curative D2 resection according to NCCN guidelines. (A) The survival curve of TNM-PNI in patients without adjuvant therapy; (B) the survival curve of TNM-PNI in patients with adjuvant therapy.
Abbreviations: TNM, tumor-node-metastasis; PNI, prognostic nutritional index; GC, gastric cancer; NCCN, National Comprehensive Cancer Network.
Discussion
GC is a worldwide problem. Approximately 951,600 new GC cases and 723,100 deaths had occurred because of GC in 2012.Citation1 The TNM stage has been widely regarded as the best prognostic factor for cancers, and it has guided clinical work for decades. In our analysis, we have also verified the TNM stage as one of the independent prognostic factors that could effectively reflect the survival time of GC. However, in the clinic, we often found significant survival heterogeneity between GC patients who had the same TNM stage. Thus, in recent years, researchers have changed focus from the tumor itself to the tumor environment, particularly the nutritional and inflammatory status of patients.
Nutritional status always plays an important role in the prognosis of cancer patients, especially among older patients.Citation12 For example, albumin, a recognized nutritional index, was one of the independent predictors of OS in GC patients; and its prognostic value has even surpassed that of the TNM stage in some studies.Citation3,Citation13 Furthermore, chronic inflammation can also promote and reflect tumor progression by affecting host immunity and the antitumor response. Lymphocytes are crucial components of the immune system for their role in destroying cancer cells, and lymphocyte proliferation and metastasis can be induced by the presence of cancer cells. Tumor-infiltrating lymphocytes are important antitumor immune cells, and their distribution and infiltra tion of tumors are closely related to the oncogenesis and prognosis of tumors. Thus, PNI, a combination of albumin concentration and lymphocyte count, has been considered a good prognostic predictor for cancer patients. In this study, we performed separate Cox multivariate analyses for continuous and categorical variables and demonstrated that TNM stage, PNI, and adjuvant therapy were independent prognostic factors of GC, consistent with previous reports.
In addition to other inflammatory markers, we also found PNI to be associated with tumor size and TNM stage (). Tumor size is a manifestation of tumor burden and a prognostic factor for several tumors. GC patients with earlier TNM stage always have better nutritional and immune status. Thus, PNI, a reflection of physical condition, is always negatively correlated with tumor burden and tumor stage. We realized that PNI could be a prognostic factor in addition to the TNM stage. As shown in , PNI could separate the survival curve more effectively than the TNM stage, especially for stage I and II GC patients. Other biochemical markers may also be associated with the prognosis of cancers. Several studies have reported that platelets contribute to the multistep development of tumors and could be a therapeutic target for tumors.Citation14–Citation16 Fibrinogen is a pro-inflammatory protein that plays an important role in inflammatory responses and tumor progression; it is associated with the clinicopathologic features and prognosis of several tumors, such as breast, lung, prostate, and gastrointestinal cancers.Citation17–Citation21 In addition, some meta-analysis demonstrated that NLR and PLR could also predict the prognosis for several tumors. However, in our analysis, the biomarkers mentioned above were not independent prognostic factors for GC patients; all of them were associated with the preoperative PNI. Overall, we consider PNI to be a better prognostic biomarker for GC.
In this study, we established the TNM-PNI scoring system according to the results of multivariate analysis. We also demonstrated that it was a highly accurate and practical system for evaluating the prognosis of GC, because it reflects the tumor stage, inflammation status, and nutritional status of every patient. For GC, a higher TNM-PNI score has always indicated a worse cancer outcome. We verified that TNM-PNI was the major independent prognostic factor for GC patients with curative D2 resection, independent of whether patients received or did not receive adjuvant therapy. In addition, we recommend adjuvant therapy for stage II and III GC, but not for stage I, which is consistent with the NCCN guidelines. Furthermore, we have found that the adjuvant therapy might be more beneficial for the survival of GC patients with TNM-PNI =4 and 5, and it plays an important role in postoperative therapy for GC. Thus, our study revealed that TNM-PNI may be a good supplement for the NCCN guidelines for GC and could provide guidance for clinical work.
As far as we know, this is the first report of TNM-PNI as a novel scoring system. However, there are also some limitations to the present study. First, due to the retrospective nature of our research, additional potential prognostic indexes, such as C-reactive protein, CD4/CD8 lymphocyte count, and modified GPS could not be obtained and included in our analysis. Second, clinicopathologic data could not be obtained for some of the patients, who were, therefore, excluded from the analysis. Consequently, the sample size of this study was relatively small. Finally, our results are based on the TNM stage according to the 7th edition of the AJCC system, and it remains to be seen whether our results can be replicated for other staging systems.
Conclusion
TNM stage, preoperative PNI, and adjuvant therapy were closely related to the prognosis of GC patients. The PNI had a distinctly subsidiary role relative to the TNM stage in predicting patient survival time. Combining both factors, we established the novel TNM-PNI scoring system and demonstrated that patients with a higher TNM-PNI score always had worse survival outcomes. In conclusion, the TNM-PNI score is a highly effective prognostic factor for GC patients with curative D2 resection, and it can be a good supplement for the NCCN guidelines.
Acknowledgments
This study was funded by the Natural Science Foundation of Liaoning Province (No. 2015020500). The funders had no role in the study design, data collection and analysis, and preparation or publication of the manuscript.
Supplementary materials
Table S1 Association between preoperative PNI and clinicopathologic features of 501 GC patients with curative D2 resection
Table S2 Multivariate survival analysis of OS in 501 GC patients with curative D2 resection after establishing TNM-PNI
Disclosure
The authors report no conflicts of interest in this work.
References
- TorreLABrayFSiegelRLFerlayJLortet-TieulentJJemalAGlobal cancer statistics, 2012CA Cancer J Clin20156528710825651787
- ZitvogelLPietrocolaFKroemerGNutrition, inflammation and cancerNat Immunol201718884385028722707
- LiuBZTaoLChenYZPreoperative body mass index, blood albumin and triglycerides predict survival for patients with gastric cancerPLoS One2016116e015740127309531
- HirashimaKWatanabeMShigakiHPrognostic significance of the modified Glasgow prognostic score in elderly patients with gastric cancerJ Gastroenterol20144961040104623821018
- JiangXHikiNNunobeSPrognostic importance of the inflammation-based Glasgow prognostic score in patients with gastric cancerBr J Cancer2012107227527922713657
- GraziosiLMarinoEDe AngelisVRebonatoACavazzoniEDoniniAPrognostic value of preoperative neutrophils to lymphocytes ratio in patients resected for gastric cancerAm J Surg2015209233333725190544
- OckCYNamARLeeJPrognostic implication of antitumor immunity measured by the neutrophil-lymphocyte ratio and serum cytokines and angiogenic factors in gastric cancerGastric Cancer201720225426227147244
- ShimadaHTakiguchiNKainumaOHigh preoperative neutrophil-lymphocyte ratio predicts poor survival in patients with gastric cancerGastric Cancer201013317017620820986
- MigitaKTakayamaTSaekiKThe prognostic nutritional index predicts long-term outcomes of gastric cancer patients independent of tumor stageAnn Surg Oncol20132082647265423463091
- SunKChenSXuJLiGHeYThe prognostic significance of the prognostic nutritional index in cancer: a systematic review and meta-analysisJ Cancer Res Clin Oncol201414091537154924878931
- SunKYXuJBChenSLNovel immunological and nutritional-based prognostic index for gastric cancerWorld J Gastroenterol201521195961597126019461
- LiuXQiuHKongPZhouZSunXGastric cancer, nutritional status, and outcomeOnco Targets Ther2017102107211428442919
- SunHHeBNieZA nomogram based on serum bilirubin and albumin levels predicts survival in gastric cancer patientsOncotarget2017825413054131828476041
- XieXZengXCaoSElevated pretreatment platelet distribution width and platelet count predict poor prognosis in nasopharyngeal carcinomaOncotarget201786210608910609729285316
- FrancoATCorkenAWareJPlatelets at the interface of thrombosis, inflammation, and cancerBlood2015126558258826109205
- RachidiSWallaceKDayTAAlbergAJLiZLower circulating platelet counts and antiplatelet therapy independently predict better outcomes in patients with head and neck squamous cell carcinomaJ Hematol Oncol201476525260646
- ZhangJLiSQLiaoZHPrognostic value of a novel FPR biomarker in patients with surgical stage II and III gastric cancerOncotarget2017843751957520529088857
- WangYChenWHuCAlbumin and fibrinogen combined prognostic grade predicts prognosis of patients with prostate cancerJ Cancer20178193992400129187874
- WangHZhaoJZhangMHanLWangMXingdeLThe combination of plasma fibrinogen and neutrophil lymphocyte ratio (F-NLR) is a predictive factor in patients with resectable non small cell lung cancerJ Cell Physiol201823354216422429057536
- LiuFTGaoHWuCWZhuZMThe associationof plasma fibrinogen with clinicopathological features and prognosis in esophageal cancer patientsOncotarget2017854930299303829190975
- FanSGuanYZhaoGAnGAssociation between plasma fibrinogen and survival in patients with small-cell lung carcinomaThorac Cancer20189114615129131503