Abstract
Purpose
Tumor vessels supported by perivascular cells have been implicated in the failure of some anti-angiogenic agents. The relationship between perivascular cell coverage (PC) and bevacizumab efficacy in metastatic colorectal cancer (mCRC) was analyzed.
Patients and methods
A total of 284 consecutive mCRC patients who received first-line chemotherapy with or without bevacizumab from 2007–2014 in Sun Yat-Sen University Cancer Center were analyzed. Immunohistochemical double-stain for the perivascular cell marker alpha-smooth muscle actin and endothelial cell (cluster of differentiation 31) was performed to characterize the intratumoral microvascular density. Multispectral image capturing and computerized image analyses were used to quantify the microvessels supported by the perivascular cells. The patients were divided into high and low PC group according to a median cutoff value of 0.55.
Results
No significant differences in overall survival (OS) and progression-free survival (PFS) were noted between the high and low PC group. In the low PC group, the patients with bevacizumab treatment had favorable OS (P=0.03), but without PFS benefit. In the high PC group, neither OS nor PFS was significantly different between the B+C and C subgroup. Tumors with perineural invasion had high PC (P=0.03).
Conclusion
The data showed that a low PC value could be a predictor for bevacizumab benefit.
Introduction
Targeting tumor microvascular monoclonal antibody has been a promising therapy in many advanced solid tumors,Citation1 including metastatic colorectal cancer (mCRC).Citation2 As a standard anti-angiogenesis drug inhibiting the vascular endothelial growth factor (VEGF), bevacizumab has been widely used in mCRC.Citation3–Citation6 The combination of bevacizumab plus chemotherapy has substantially improved overall survival (OS) up to 30 months.Citation7 However, the angiogenesis pathway in mCRC is not fully understood, and evidence on selecting predictive biomarkers for treatment outcomes is insufficient.Citation8,Citation9 One possible reason is that most research focuses only on the VEGF signaling pathway,Citation10,Citation11 overlooking the integral microenvironment that is intricately regulated by multiple angiogenic-related molecules.Citation12,Citation13 Hence, it is difficult to distinguish the survival benefit of angiogenesis blockers from VEGF inhibitors.Citation14 Abnormal tumor vasculature typically presents with shattered and/or vanished lumen.Citation15,Citation16 Therefore, the lack of blood supply in the tumor vasculature and the high energy requirement of proliferating cancer cells result in a hypoxic tumor microenvironment and metabolic shift to aerobic glycolysis.Citation17,Citation18 Hypoxia and aerobic glycolysis could induce the production of large amounts of lactic acid by tumor cells, leading to the acidic microenvironment.Citation19,Citation20 Lactate dehydrogenase (LDH), the key enzyme in the production of lactic acid, may reflect the acidity of the tumor microenvironment. Our previous study suggested that the LDH in peripheral blood is a potential predictor of treatment outcomes of anti-angiogenesis therapy.Citation21 However, the LDH in peripheral blood could not accurately reflect the real situation in the tumor microenvironment. The varying cutoff concentrations and several isoforms make LDH an unsatisfactory biomarker candidate. The intricate regulators in the microenvironment will eventually act on tumor vasculature. Therefore, the features of tumor vasculature could be potential predictive markers of anti-angiogenic therapy.
The budding mode of new capillaries through the mutual cooperation of various cells in the tumor microenvironment is the most widely recognized method of angiogenesis.Citation22 With the discovery of other mechanisms of new vessel recruitment,Citation23 the heterogeneity of tumor vasculature had been gaining increasing interest.Citation24 As one of the principal constituents of blood vessels, the pericytes play crucial roles in vessel survival, maturation, stabilization,Citation19 and blood flow regulation.Citation20 The mature blood vessels are characterized by encompassing pericytes.Citation25 The hypothesis of the synergistic effect was that bevacizumab eliminated and normalized the immature tumor vessels, which could enhance blood transfusion to the tumor cells.Citation26,Citation27 Furthermore, pericytes have been reported as a homogeneous cell population in terms of derivation, distribution, phenotype, and function.Citation28
The purpose of our study was to investigate whether there was a particular microvessel characteristic in mCRC and to evaluate the relationship between this type of tumor vessel and bevacizumab efficacy, particularly the immature vessels that lack supporting pericytes.Citation15
Materials and methods
Patients
Patients who met the following inclusion criteria were enrolled: (1) pathologically diagnosed with mCRC and with clinical and/or pathological confirmations of metastasis at the Sun Yat-Sen University Cancer Center from January 2005 to March 2014 and finished the planned course of first-line treatment in this center; (2) with pathological specimens of primary tumor; and (3) an Eastern Cooperative Oncology Group (ECOG) performance status of ≤2. Patients in the chemotherapy plus bevacizumab group received bevacizumab at a dose of 5 mg/kg on day one combined with the standard first-line chemotherapy regimens including oxaliplatin-based and irinotecan-based regimens. Patients who received less than four cycles of bevacizumab were excluded because a therapeutic benefit can only be obtained from at least four cycles of bevacizumab.Citation29 Patients who lack a pathological diagnosis or complete medical history, those lost to followup, and those who have two or more kinds of asynchronous or synchronous tumor were excluded.
Double immunohistochemical staining
All specimens were fixed in formalin and embedded in paraffin blocks; the blocks were then cut into 4-µm sections. All tissue sections were double stained to assess the blood vessel endothelial cell marker cluster of differentiation 31 (CD31) and the perivascular cell marker alpha smooth muscle actin (α-SMA).
For immunohistochemical (IHC) staining, we used a Polymer Double-stain System (Mo/HRP Rb/AP, Zhong Shan Gold Bridge Biotechnology Co., Ltd, Beijing, China) according to the manufacturer’s instructions. Tissue sections were incubated simultaneously with two primary antibodies: rabbit anti-human CD31 polyclonal antibody (working dilution 1:200, Abcam, Cambridge, UK) and mouse anti-human α-SMA monoclonal antibody (working dilution 1:12,000, Sigma-Aldrich, Merck KGaA, Darmstadt, Germany). Sections were incubated with anti-rabbit multimer labeled with horseradish peroxidase (brown staining) for CD31 and with anti-mouse multimer labeled with alkaline phosphatase substrate (red staining) for α-SMA. The nuclear-specific hematoxylin was used for counterstaining.
Tumor area and multispectral imaging
We selected the five most vascularized spots (×20 objective) in all sections. Images were spectrally analyzed to quantify horseradish peroxidase-stained, alkaline phosphatase substrate-stained, and hematoxylin-stained regions using the Nuance multispectral imaging system (Cambridge Research, Woburn, MA, USA). The resulting image cubes were converted to optical density (OD) units and were mathematically unmixed into separated CD31 substrate, SMA substrate, and hematoxylin components using spectra deduced from control specimens. The component images were pseudo-colored for further analyses.
Images were analyzed on Image Pro Plus 6.0 software. The mean values of perivascular cell coverage (PC, percentage) for the five selected spots in each area were considered the final values.
Follow-up and statistical analysis
The latest follow-up was performed on June 30, 2016 through telephone interview or medical records review. OS was measured from the date of diagnosis with mCRC to the date of death. Progression-free survival (PFS) was measured from the initiation of first-line therapy to the progression. Both OS and PFS were estimated via the Kaplan–Meier method, and survival differences were analyzed via the log-rank test.
The distributions of the baseline characteristics of the patients were assessed via the Chi-squared test. The correlation between PC and clinicopathologic characteristics was assessed using Spearman rank correlations for categorical data and Wilcoxon rank-sum test and Kruskal-Wallis test for measured data. All statistical was analyses were conducted using SPSS version 22 software. Significance was set at a P-value of <0.05.
Results
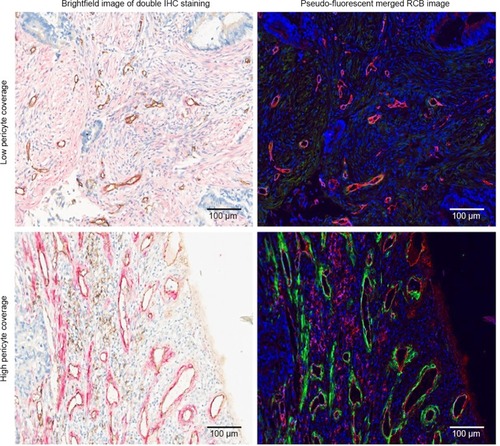
A total of 284 patients with available pathological sections were recruited in this retrospective study. Of them, 59 patients received chemotherapy combined with bevacizumab (B+C group), while 225 patients received chemotherapy alone (C group). The association between endothelial cells and perivascular cells was assessed by analyzing the co-staining of CD31 and α-SMA via Nuance multispectral imaging.Citation30 revealed the correlations between perivascular cells and endothelial cells. The blood vessels in mCRC were covered with different proportions of perivascular cells. The median valueCitation30 of PC was 0.55 and was used as the cutoff point to divide the patients into high and low PC groups. High and low PC were defined as a median PC of >0.55 and ≤0.55, respectively.
Figure 1 Double IHC staining and image analyses of mCRC tissue.
Notes: Tissue sections were stained with anti-CD31 antibody (brown in the brightfield IHC images, red in the pseudo-fluorescent merged RGB images) and anti-α-SMA antibody (red in the brightfield IHC images, green in the pseudo-fluorescent merged RGB images). Brightfield and pseudo-fluorescent RGB images are shown to highlight the intensity of the staining. Scale bars, 100 µm.
Abbreviations: IHC, immunohistochemical; mCRC, metastatic colorectal cancer; CD31, cluster of differentiation 31; RGB, red-green-blue; α-SMA, alpha-smooth muscle actin.
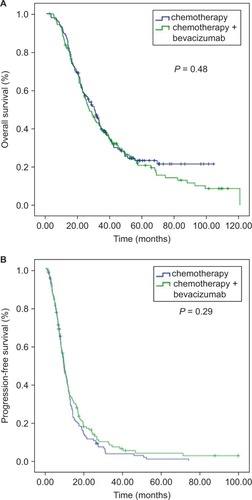
PC and patients’ survival
The median OS in the high PC group was lower than that in the PC group at 26.5 (95% CI=21.8–31.1) months vs 30.0 (95% CI=25.0–35.0) months (P=0.48, ), respectively, but the difference was not significant. The difference in PFS between the two groups also showed no significance (9.3 months in the high PC group and 9.8 months in the low PC group, P=0.29, ). The patient characteristics are shown in . All of the factors were balanced in statistical analysis.
Table 1 Patient characteristics
PC and bevacizumab effect
In the low PC cohort, the median OS of the B+C group was 48.5 (95% CI=22.9–74.1) months, while it was 26.4 (95% CI=19.0–33.7) months (P=0.03) in the C group. Meanwhile, no significant difference in median OS was noted between the B+C and C subgroups in the high PC group (26.1 months in the C group and 29.0 months in the B+C group, P=0.55, ). The patients who received bevacizumab therapy did not obtain a PFS benefit in both the low and high PC groups (9.1 and 12.4 months in the C and B+C subgroups, respectively, in the low PC group, P=0.10; 9.00 and 10.87 months in the C and B+C subgroups in the high PC group, P=0.77, ).
Figure 3 Kaplan–Meier curve analyses of OS. (A) In the low PC group, patients who received bevacizumab had better OS. (B) In the high PC group, there was no significant difference in OS in terms of bevacizumab treatment.
Abbreviations: OS; overall survival; PC, perivascular cell coverage.
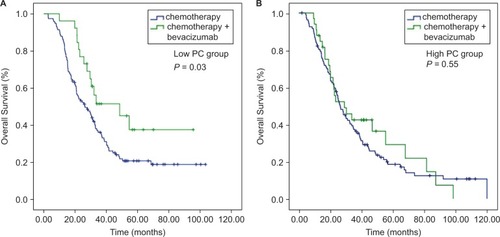
Figure 4 Kaplan–Meier curve analyses of PFS. There was no significant difference in PFS in terms of bevacizumab treatment in both the low PC group (A) and the high PC group (B).
Abbreviations: PFS, progression-free survival; PC, perivascular cell coverage.
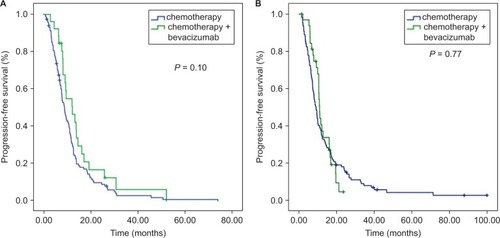
The results suggested that patients with low PC could benefit more from bevacizumab than those with high PC. Analyses of patient characteristics according to the B+C subgroup and C subgroup in the low PC cohort showed that they were equally distributed (). Meanwhile, in the high PC cohort, a higher percentage of patients in the B+C subgroup was female (P=0.01), and the number of patients with vascular (P=0.003) and perineural invasion (P=0.03) was also higher than that in the C subgroup.
Table 2 Patient characteristics in PC subgroup analyses
Correlation between PC and clinicopathologic characteristics
We analyzed the relationship between PC and clinicopathologic characteristics in mCRC and found that high PC was correlated with the occurrence of perineural invasion (P=0.03). However, there was no correlation between PC and sex, age, tumor size, primary tumor location, pathological type, T-classification, lymphatic invasion, stage, and vascular invasion in mCRC ().
Table 3 Correlation between clinicopathologic characteristics and PC
Discussion
Blockage of tumor angiogenesis is a promising approach in cancer treatment. However, due to the complexity of tumor angiogenesis, the survival benefit from bevacizumab administration is still limited in mCRC patients.Citation31,Citation32 Bevacizumab, as well as other anti-angiogenic agents targeting VEGF-A or its receptors, perhaps only inhibit the particular endothelial cells that rely on exogenous VEGF-A.Citation24 At least six well-defined tumor vessel types develop from angiogenesis and arterio-venogenesis with respect to structure and function, including glomeruloid microvascular proliferations, mother vessels, vascular malformations, capillaries, draining veins, and feeder arteries.Citation24 Although all six types of blood vessels could be induced by VEGF-A in mouse models, only the mother vessel and glomeruloid microvascular proliferations remained sensitive to anti-VEGF-A therapy.Citation33
During tumor angiogenesis, the recruitment and coverage of perivascular cells is an essential condition for vessel maturation.Citation14 Bergers and HanahanCitation34 found that maturation of the vasculature with increased PC might be responsible for the failure of anti-VEGF therapy. Suppressing pericyte migration has been reported to be better than anti-angiogenic therapy alone,Citation35 implying that suppressing pericyte migration could result in production of microvessels with low PC, which are sensitive to anti-angiogenic therapy.
Aside from inducing angiogenesis, tumors exploit multiple mechanisms to recruit blood vessels,Citation23 including vessel co-option, which is a process of hijacking the normal vessel counterpart similar to tumor invasion.Citation36 The co-opted vessels are usually supported by pericytes surrounding the endothelial cells.Citation18 Pericytes not only stabilize blood vessels,Citation37 but also induce the autocrine VEGF-A signaling that could promote endothelial cell survival.Citation38 Weisshardt et alCitation39 have reported that bevacizumab-resistant vessels in mCRC are covered by pericytes that have much longer diameters than capillary vessels, suggesting the formation of co-option vessels in the tumor. The vessel co-option has been reported as an essential mechanism for anti-angiogenic resistance in mouse neuroblastomaCitation40 and in patients with colorectal cancer liver metastases.Citation41 In addition, the pericytes have been found to be involved in vascular immunosurveillance,Citation42 and promote tumor growth via immunosuppression.Citation43 Hence, the low proportion of perivascular cells could serve as a predictive marker of anti-angiogenic therapy. In our study, we discovered a novel finding that low PC is a potential predictive marker for bevacizumab therapy.
Our study found that PC was not a prognostic factor in mCRC. In contrast, some reports have demonstrated that poor PC indicated unfavorable prognoses in patients with colorectal cancerCitation44 and breast cancer.Citation45 However, the value of PC as a prognostic marker is controversial. In clear-cell renal cell carcinoma, high PC was associated with more aggressive characteristics such as high tumor grades, high tumor stages, high necrosis rates, and poor outcome.Citation30 In the current study, we found that high PC was associated with more perineural invasion. To the best of our knowledge, the significance of the association between PC and patient prognosis in mCRC is unclear.
This study has some limitations, as follows. First, it is a retrospective and non-randomized study with a small number of patients. Second, in the low PC group, the addition of bevacizumab significantly improved OS, but not PFS. The results are similar to those of the FLEX study of non-small-cell lung cancer.Citation46 The small sample size may have been inadequate to show a statistically significant PFS difference, because bevacizumab seemed to prolong the PFS for 3.3 months in the low PC group. Third, in the high PC cohort, the proportion of patients with vascular and perineural invasion was higher in the B+C subgroup than that in the C subgroup. Both vascular and perineural invasion are poor prognostic factors that may offset the bevacizumab benefit in the high PC group, although the number of patients with such factors was small in this cohort.
Conclusion
PC is a potential predictive marker of bevacizumab therapy. Patients with low PC value could benefit more from bevacizumab treatment than those with high PC. Our findings need to be validated in large-scale prospective studies. The clinical value of PC for choosing the optimal therapeutic modality should be assessed.
Ethics approval
This study was approved by the ethics committee of the Sun Yat-Sen University Cancer Center (Approval no: GZR2015-034). Written informed consent was obtained from each patient.
Acknowledgments
We thank the participants for their cooperation in this study. This study was funded by the Natural Science Foundation of Guangdong, China (2015A030313010); Science and Technology Program of Guangzhou, China (1563000305); and National Natural Science Foundation of China (81272641 and 81572409).
Data availability
The authenticity of this article has been validated by uploading the key raw data onto the Research Data Deposit public platform (www.researchdata.org.cn), with the approval RDD number as RDDB2018000380.
Disclosure
The authors report no conflicts of interest in this work.
References
- CookKMFiggWDAngiogenesis inhibitors: current strategies and future prospectsCA Cancer J Clin201060422224320554717
- HurwitzHIFehrenbacherLHainsworthJDBevacizumab in combination with fluorouracil and leucovorin: an active regimen for first-line metastatic colorectal cancerJ Clin Oncol200523153502350815908660
- SaltzLBClarkeSDíaz-RubioEBevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: a randomized phase III studyJ Clin Oncol200826122013201918421054
- GiantonioBJCatalanoPJMeropolNJBevacizumab in combination with oxaliplatin, fluorouracil, and leucovorin (FOLFOX4) for previously treated metastatic colorectal cancer: results from the Eastern Cooperative Oncology Group Study E3200J Clin Oncol200725121539154417442997
- YangQYinCLiaoFBevacizumab plus chemotherapy as third- or later-line therapy in patients with heavily treated metastatic colorectal cancerOnco Targets Ther201582407241326366095
- BennounaJSastreJArnoldDContinuation of bevacizumab after first progression in metastatic colorectal cancer (ML18147): a randomised phase 3 trialLancet Oncol2013141293723168366
- ElezEArgilésGTaberneroJFirst-Line Treatment of Metastatic Colorectal Cancer: Interpreting FIRE-3, PEAK, and CALGB/SWOG 80405Curr Treat Options Oncol201516115226374340
- JubbAMHarrisALBiomarkers to predict the clinical efficacy of bevacizumab in cancerLancet Oncol201011121172118321126687
- LambrechtsDLenzHJde HaasSCarmelietPSchererSJMarkers of response for the antiangiogenic agent bevacizumabJ Clin Oncol20133191219123023401453
- CaoYVEGF-targeted cancer therapeutics-paradoxical effects in endocrine organsNat Rev Endocrinol201410953053925048037
- MaruDVenookAPEllisLMPredictive biomarkers for bevacizumab: are we there yet?Clin Cancer Res201319112824282723549876
- StackerSAAchenMGThe VEGF signaling pathway in cancer: the road aheadChin J Cancer201332629730223419196
- YanLMolecular targeted agents–where we are and where we are goingChin J Cancer201332522523223642906
- BellouSPentheroudakisGMurphyCFotsisTAnti-angiogenesis in cancer therapy: Hercules and hydraCancer Lett2013338221922823707856
- YaoXQianCNZhangZFTwo distinct types of blood vessels in clear cell renal cell carcinoma have contrasting prognostic implicationsClin Cancer Res200713116116917200351
- QianCNHuangDWondergemBTehBTComplexity of tumor vasculature in clear cell renal cell carcinomaCancer200911510 Suppl2282228919402071
- AdighibeOLeekRDFernandez-MercadoMWhy some tumours trigger neovascularisation and others don’t: the story thus farChin J Cancer2016351826873439
- QianCNTanMHYangJPCaoYRevisiting tumor angiogenesis: vessel co-option, vessel remodeling, and cancer cell-derived vasculature formationChin J Cancer2016351026747273
- SimonaviciusNAshendenMvan WeverwijkAPericytes promote selective vessel regression to regulate vascular patterningBlood201212071516152722740442
- HallCNReynellCGessleinBCapillary pericytes regulate cerebral blood flow in health and diseaseNature20145087494556024670647
- YinCJiangCLiaoFInitial LDH level can predict the survival benefit from bevacizumab in the first-line setting in Chinese patients with metastatic colorectal cancerOnco Targets Ther201471415142225143746
- CarmelietPJainRKMolecular mechanisms and clinical applications of angiogenesisNature2011473734729830721593862
- CarmelietPJainRKMolecular mechanisms and clinical applications of angiogenesisNature2011473734729830721593862
- NagyJAChangSHShihSCDvorakAMDvorakHFHeterogeneity of the tumor vasculatureSemin Thromb Hemost201036332133120490982
- ZhaoYYXueCJiangWPredictive value of intratumoral microvascular density in patients with advanced non-small cell lung cancer receiving chemotherapy plus bevacizumabJ Thorac Oncol201271717522011670
- SaboEBoltenkoASovaYSteinAKleinhausSResnickMBMicroscopic analysis and significance of vascular architectural complexity in renal cell carcinomaClin Cancer Res20017353353711297244
- JainRKNormalizing tumor vasculature with anti-angiogenic therapy: a new paradigm for combination therapyNat Med20017998798911533692
- PaivaAELousadoLGuerraDAPPericytes in the Premetastatic NicheCancer Res201878112779278629789421
- Bei ZhangWHZhangWHBA Potential Administration-time Dependent Effect of Bevacizumab in Improving Overall Survival and Increasing Metastasis in Metastatic Colorectal CancerChemotherapy20130201
- CaoYZhangZLZhouMPericyte coverage of differentiated vessels inside tumor vasculature is an independent unfavorable prognostic factor for patients with clear cell renal cell carcinomaCancer2013119231332422811049
- HurwitzHFehrenbacherLNovotnyWBevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancerN Engl J Med2004350232335234215175435
- HayesDFBevacizumab treatment for solid tumors: boon or bust?JAMA2011305550650821285431
- SitohyBNagyJADvorakHFAnti-VEGF/VEGFR therapy for cancer: reassessing the targetCancer Res20127281909191422508695
- BergersGHanahanDModes of resistance to anti-angiogenic therapyNat Rev Cancer20088859260318650835
- SongSEwaldAJStallcupWWerbZBergersGPDGFRbeta+ peri-vascular progenitor cells in tumours regulate pericyte differentiation and vascular survivalNat Cell Biol20057987087916113679
- QianCNHijacking the vasculature in ccRCC–co-option, remodelling and angiogenesisNat Rev Urol201310530030423459032
- SchrimpfCXinCCampanholleGPericyte TIMP3 and ADAMTS1 modulate vascular stability after kidney injuryJ Am Soc Nephrol201223586888322383695
- FrancoMRoswallPCortezEHanahanDPietrasKPericytes promote endothelial cell survival through induction of autocrine VEGF-A signaling and Bcl-w expressionBlood2011118102906291721778339
- WeisshardtPTrarbachTDürigJTumor vessel stabilization and remodeling by anti-angiogenic therapy with bevacizumabHistochem Cell Biol2012137339140122193946
- KimESSerurAHuangJPotent VEGF blockade causes regression of coopted vessels in a model of neuroblastomaProc Natl Acad Sci U S A20029917113991140412177446
- FrentzasSSimoneauEBridgemanVLVessel co-option mediates resistance to anti-angiogenic therapy in liver metastasesNat Med201622111294130227748747
- StarkKPekayvazKMassbergSRole of pericytes in vascular immunosurveillanceFront Biosci201823767781
- SenaIFGPaivaAEPrazeresPGlioblastoma-activated pericytes support tumor growth via immunosuppressionCancer Med2018741232123929479841
- MezheyeuskiABradic LindhMGurenTKSurvival-associated heterogeneity of marker-defined perivascular cells in colorectal cancerOncotarget2016727419484195827248825
- CookeVGLebleuVSKeskinDPericyte depletion results in hypoxia-associated epithelial-to-mesenchymal transition and metastasis mediated by met signaling pathwayCancer Cell2012211668122264789
- PirkerRPereiraJRSzczesnaACetuximab plus chemotherapy in patients with advanced non-small-cell lung cancer (FLEX): an open-label randomised phase III trialLancet200937396741525153119410716