Abstract
Introduction
To assess the effect of tumor laterality to cardiac-related deaths of breast cancer in the current radiation practices using a large modern population-based study.
Methods
Women diagnosed with breast cancer from 2000 to 2008 were included using the current Surveillance, Epidemiology, and End Results database. The primary outcome of this study was the cardiac-related mortality. Multivariate analysis was performed using the Cox proportional hazards model to analyze the cardiac-related mortality including demographic, clinicopathologic, and treatment factors.
Results
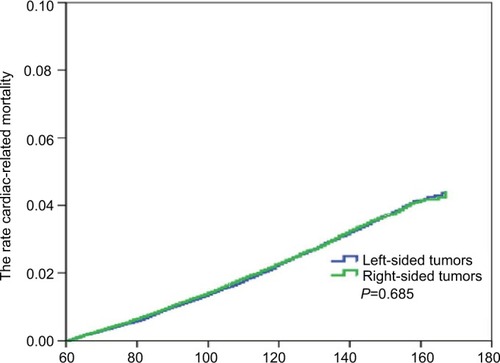
We identified 168,761 breast cancer patients, including 85,006 (50.4%) patients with left-sided tumors and 83,755 (49.6%) patients with right-sided tumors. The median follow-up period was 8.8 years. The 10-year cardiac-related mortality was 2.3% and 2.3% in left- and right-sided tumors, respectively (P=0.685). The results indicated that patients with older age, non-Hispanic Black, receipt of mastectomy, and married status were the independent adverse factors for cardiac-related mortality. However, left-sided tumors were not associated to a higher risk of cardiac-related mortality than right-sided tumors following postoperative radiotherapy (right vs left, hazard ratios 1.025, 95% CI 0.856–1.099, P=0.484). The risk of cardiac-related mortality in the entire cohort was increased with the extension of follow-up time. However, there was still not significantly different between left- and right-sided tumors. Subgroup analysis also found no association between tumor laterality and cardiac-related mortality after postoperative radiotherapy based on various demographics and treatment factors.
Conclusion
With a median follow-up of 8.8 years, no significant differences were found in cardiac-related mortality between left- and right-sided tumors under current radiation practices of breast cancer patients.
Introduction
Postoperative radiotherapy (PORT) is an important component of the comprehensive treatment of breast cancer. Long-term studies indicate that PORT following breast- conserving surgery (BCS) in eligible patients results in similar efficacy, including local tumor control and overall survival, compared to mastectomies.Citation1 In addition, the locoregional recurrence rates and survival outcomes in locally advanced breast cancers with tumors larger than 5 cm and four or more axillary lymph node metastases are improved with postoperative mastectomy radiotherapy.Citation2,Citation3 However, the administration of PORT for breast cancer may expose the heart and blood vessels to late radiotherapy-induced complications, and several recent population-based studies have indicated that PORT used in breast cancer has an increased risk of ischemic heart disease, valvular disease, and pericarditis.Citation4–Citation6 The dose to the heart has decreased with the development of radiotherapy techniques.Citation7 However, much uncertainty remains on the long-term cardiac toxicity effects of PORT.
In breast cancer patients with left-sided tumors, the heart is exposed to a significantly higher dose than in right-sided tumors.Citation7 Furthermore, the long-term cardiac toxicity due to PORT between the two tumor lateralities remains controversial. Several studies using large cohorts have found that the risk of cardiac-related mortality in left-sided tumors was significantly higher than right-sided tumors after PORT.Citation5–Citation11 However, there were also studies which showed similar cardiac-related mortality between the two groups.Citation12–Citation15 In addition, specific patients, including patients who have had previous cardiac disease or older survivors (aged 65+ years), might also be at an increased risk of cardiac-related mortality in left-sided tumors compared with right-sided tumors.Citation16,Citation17 Differences in the enrolled population, therapy duration, radiotherapy techniques, target volume, chemotherapy regimen, and follow-up time may be the main explanation for conflicting results of cardiac-related mortality in the above- mentioned studies. In the present study, we assessed the effect of tumor laterality on cardiac-related mortality in the current radiation practices using a large modern population- based database.
Materials and methods
Surveillance, Epidemiology, and End Results (SEER) database
The SEER database is maintained at the National Cancer Institute,Citation18 and contains de-identified information on approximately 28% of cancer patients in the USA. The demographics, clinicopathological features, therapeutic factors (including surgery, radiotherapy and chemotherapy), and patient-specific survival are recorded in the current SEER database. SEER database is a worldwide public database, and we have permission to access the SEER database (authorization code 10702-Nov2017). This study was approved by the Institutional Review Board of the First Affiliated Hospital of Xiamen University and performed in accordance with their guidelines.
Patients, covariates, and treatment information
Women diagnosed with breast cancer between 2000 and 2008 who met the following criteria were included: non-metastatic disease, left- or right-sided tumors, underwent BCS or mastectomy, received adjuvant beam radiotherapy following primary surgery, and followed-up more than 60 months. Patients without defined tumor laterality, who underwent preoperative radiotherapy or PORT with implants/isotopes alone, and did not undergo PORT were excluded.
We gathered demographic and clinicopathologic characteristics data including age, race/ethnicity, histological subtype, tumor stage, nodal stage, hormone receptor status, marital status, and tumor laterality. Patient staging was extrapolated to the 7th Union for International Cancer Control/American Joint Committee on Cancer Tumor-Node- Metastasis staging system. Primary and adjuvant treatments include surgical procedures, chemotherapy, and completion of the first course of PORT. The primary end-point measured in this study was the probability of cardiac-related mortality. Data on risk factors for cardiac-related mortality were collected 5 years post breast cancer diagnosis.
Statistical analyses
Differences in demographics, clinicopathology, and treatment characteristics by tumor laterality were examined by chi-squared test. In addition, we evaluated the probability of cardiac-related mortality by tumor laterality using the Kaplan–Meier method, with P-values based on log-rank tests. Multivariate analysis was performed using the Cox proportional hazards model to analyze the risk factors for cardiac-related mortality including age, race/ethnicity, marital status, surgical procedures, chemotherapy, and tumor laterality by assessment of the hazard ratios (HRs) and their corresponding 95% confidence interval (95% CI). Subgroup analysis was performed to assess the effect of different demographics and treatment factors on the risk of cardiac-related mortality in patients with left- and right-side tumors using univariate analysis. Analyses resulting in P-values of <0.05 were considered statistically significant. All analyses were performed using SPSS statistical software (version 22.0; IBM Corp., Armonk, NY, USA).
Results
We identified 168,761 patients who met the criteria described above, including 85,006 (50.4%) patients with left-sided tumors and 83,755 (49.6%) patients with right-sided tumors. The median age of the entire cohort was 58 years (range, 13–100 years). A comparison of demographic, clinicopathologic, and treatment factors by tumor laterality is shown in . The distribution of lymph nodes status (P<0.001), estrogen receptors status (P<0.001), and progesterone receptors status (P=0.016) by tumor laterality reached statistical significance. In addition, the distribution of age, race/ethnicity, histological subtypes, tumor stage, surgical procedure, chemotherapy, and marital status did not differ by tumor laterality.
Table 1 The demographic, clinicopathologic, and treatment factors by tumor laterality
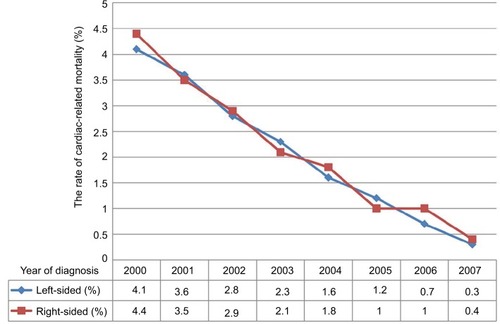
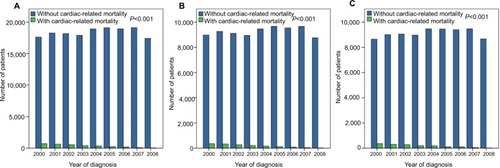
The median follow-up was 8.8 years (106 months, range, 61–167 months). A total of 3,169 patients died of heart- related disease. During the follow-up period, the 8-year, 10-year, and 13-year cardiac-related mortality rates were 1.2%, 2.2%, and 3.9%, respectively. In the entire cohort, the risk of cardiac-related mortality steadily declined over the study period (). There were also similar trends in left- and right-sided tumors (). A total of 1,588 and 1,581 patients died of heart-related disease in left- and right-sided tumors, respectively, and the 10-year heart-related disease rates were 2.3% and 2.3%, respectively (P=0.685) (). The rates of cardiac-related mortality by tumor laterality by the years of diagnosis are listed in , indicating that the risk of cardiac-related mortality was increased with the extension of follow-up time. However, there was still no significant difference between left- and right-sided tumors.
Figure 1 The cardiac-related mortality by tumor laterality during the study period.
Notes: (A) Entire cohort; (B) left-sided tumors; (C) right-sided tumors.
The multivariate Cox proportional hazards model including demographic, clinicopathologic, treatment factors, and tumor laterality was used to assess the risk of cardiac-related mortality (). The results indicated that patients with older age, non-Hispanic Black, receipt of mastectomy, and married status were the independent adverse factors for cardiac-related mortality. However, no association was found between left- and right-sided tumors and cardiac-related mortality (right vs left, HR 1.025, 95% CI 0.856–1.099, P=0.484).
Table 2 Multivariate analysis of cardiac-related mortality by tumor laterality
We further analyzed the effect of different demographics and treatment factors on the risk of cardiac-related mortality in patients with left- and right-sided tumors. The results demonstrate that left-sided tumors were not associated with a significantly higher risk of cardiac-related mortality than right-sided tumors by various demographics and treatment factors ().
Table 3 Multivariate univariate analysis of cardiac-related mortality by tumor laterality based on various demographics and treatment factors
Discussion
In our study, we performed a large modern population-based study to assess the effect of tumor laterality on cardiac-related mortality with current radiation practices of breast cancer. Our study found that the risk of cardiac-related mortality in patients with left-sided tumors between 2000 and 2008 was not significantly higher than that of patients with right-sided tumors.
The effect of tumor laterality on cardiac-related mortality following PORT remains controversial. A meta-analysis including 289,109 patients found that heart-related mortality in left-sided tumors following PORT was significantly higher than in right-sided tumors and was more apparent after ≥15 years of follow-up.Citation8 A long-term study by Bouillon et al also found that among women who had received PORT between 1954 and 1984, left-sided tumors had a 1.56-fold (95% CI 1.27–1.90) higher risk of cardiac-related mortality than right-sided tumors, even after 20 years.Citation11 In addition, the population-based case–control study also indicated a significant increase in long term cardiac-related mortality in women with left-sided tumors treated with PORT.Citation6 However, the abovementioned studies had notable flaws. The cohorts were treated within a wide timespan, from 1954 to 2002, which comes with large differences in planning and delivering radiotherapy, including therapy duration, radiotherapy techniques, fraction size, and target volume. A previous SEER study demonstrated higher cardiac-related mortality in left-sided tumors compared to right-sided tumors following PORT between 1973 and 1982. However, no evidence of heart-related mortality was found between the two groups since 1983.Citation9 Our study includes patients from 2000–2008, well within the era of modern radiotherapy, and our results suggest comparable trends of cardiac-related mortality in tumor laterality.
With the advancement of radiotherapy techniques, the risk of cardiac-related mortality in breast cancer patients may be comparable between tumor laterality. Several studies include patients in the era of modern radiotherapy, and the results demonstrate that the risk of cardiac-related mortality does not increase in patients receiving left-sided PORT compared to right-sided PORT, with the exception of women with a history of cardiac disease.Citation12,Citation15,Citation16,Citation19 A population-based study also confirmed that the 10-year cardiac-related mortality rate in left- and right-sided tumors following PORT was only 2.4% and 1.9%, respectively,Citation19 which was similar to our study. However, our study also found that the risk of cardiac-related mortality steadily declined over the study period. Furthermore, heart related deaths are independent of tumor laterality, due to the significant improvements in radiotherapy techniques and accuracy of radiation delivery. Indeed, these produce significantly less scatter and thereby decrease excessive exposure to the heart.Citation20 Moreover, the computed tomography-based target volume delineation and treatment planning could also significantly reduce the dose to heart. Therefore, modern radiotherapy techniques might further reduce the cardiac-related mortality compared to previous studies, and the survival benefits of the radiotherapy may far outweigh the risks for women being considered for breast cancer radiotherapy.
Although the modern radiotherapy techniques have advantage in dosimetry, data of cardiac dose sparing techniques regarding late cardiac events are limited due to the difficulties of long-term follow-up. There are several cardiac biomarkers to evaluate early cardiac injury including brain natriuretic peptide and N-terminal pro-B-type natriuretic peptide, which could be useful minimally invasive markers to detect early cardiac injury.Citation21,Citation22
The dose to the heart is exposed to differs between left- and right-sided tumors. A systematic review of publications between 2003 and 2013 found that the average dose of heart is exposed to in left- and right-sided tumors was 5.4 Gy (range, <0.1–28.6 Gy) and 3.3 Gy, respectively.Citation23 A practice pattern survey from 82 radiation oncology departments demonstrated that 5 Gy was a “safe” dose to the heart.Citation24 However, a recent study by Darby et al indicated a linear correlation between the risk of major coronary events and the mean dose to the heart (7.4% per Gy), with no clear threshold.Citation6 In addition, the volume of the left ventricle receiving 5 Gy may be a better predictor for acute coronary event than mean heart dose in breast cancer.Citation25 Therefore, reducing radiation exposure of the heart might further decrease the risk of acute coronary event or cardiac-related mortality after PORT of breast cancer.
In breast cancer, the internal mammary node radiation remains one of the major determinants of cardiac toxicity regardless of tumor laterality. The rate of radiation administration to internal mammary node has decreased since the 1980s;Citation9 this might be one explanation for the reductions of radiation-related cardiac mortality in left-side tumors. However, there might be more patients who received internal mammary node radiation based on the results of EORTC 22922/10925 and MA.20.Citation26,Citation27 The guidelines of the National Comprehensive Cancer Network recommend the irradiation dose to internal mammary nodes since 2016.Citation28 Although the argument against internal mammary node radiation is cardiac toxicity,Citation6 studies have indicated that the cardiac toxicity is a multifactorial process with only a small portion directly related to radiotherapy.Citation29 In addition, with advances of radiotherapy techniques in internal mammary radiation, the average dose the heart is exposed to has decreased to 1.0 Gy, which is significantly lower than 6.4 Gy for tomotherapy, 4.5 Gy for volume modulated arc therapy, and 5.3 for wide tangential irradiation.Citation30
In this study, the probability of cardiac-related mortality was significantly higher in patients undergoing PORT after mastectomy than in patients receiving BCS followed by PORT. The mean dose to the heart in BCS has declined in recent years to 2–7 and 1.5 Gy for left- and right-sided tumors, respectively.Citation31,Citation32 However, in patients with left-sided tumors who received mastectomy, the mean dose was 8.1–8.8 Gy using three-dimensional conformal radiotherapy, and 7.0–7.3 Gy using intensity modulated radiation therapy.Citation33,Citation34 Moreover, most patients undergoing PORT after mastectomy were locally advanced stages, and the probability of receiving chemotherapy for patients undergoing mastectomy in our study was significantly higher than in patients receiving BCS (84.5% vs 39.7%, P<0.001). A study from the Danish Breast Cancer Cooperative Group reported that PORT in left-sided tumors was associated with a significantly higher risk of cardiac disease compared to right-sided tumors, with the largest increases observed among women who also received anthracycline-based chemotherapy.Citation10 In addition, patients who received PORT following a mastectomy may have received additional regional nodal radiotherapy resulting in excessive exposure to the heart and increasing the risk of cardiac-related mortality. A large cohort including 70,230 stage I to III breast cancer patients between 1989 and 2005 indicated that the risk of any cardiovascular event did not change with longer follow-ups after left-sided PORT after BCS, whereas the risk of left-sided PORT following mastectomy increased with longer follow-up duration.Citation5 Therefore, the dose to the heart is exposed to should be reduced for patients who received mastectomy to decrease the risk of cardiac-related death.
Our study confirms a previous study which reveals that patients of older age, unmarried status, or African American descent are both associated with higher rates of cardiac-related mortality.Citation12 This may be explained by the baseline risks of these subgroups rather than any relation to radiotherapy.Citation35–Citation38 However, our subgroup analysis found no association between long-term cardiac-related mortality by tumor laterality and various demographics and treatment factors.
Several limitations should be acknowledged when interpreting our results. First, there is an inherent weakness of selection bias in a population-based observational study. The main advantage of our study is that it includes a large cohort of population-based patients with sufficient power to detect relatively small increases in cardiac risk. Additionally, our study includes patients from 2000, which are more reflective of the current radiation practices compared to previous studies. Second, the follow-up in our study was relatively short, with a median of 8.8 years in the total cohort. The study by Darby et alCitation39 indicated that the cardiac-related mortality in left-sided tumors following PORT did not become significantly higher compared to right-sided tumors until 10–15 years after their PORT. Therefore, the median follow- up of 8.8 years in our study may not be long enough. We plan to repeat our analysis in the next 5–10 years to investigate the long term cardiac-related mortality by tumor laterality. Third, we could only include cardiac-related mortality in our study due to the lack of information in the SEER database. Indeed, time of the diagnosis and treatment results of specific cardiovascular diseases were not included in the current SEER database. In addition, there was a lack of data for the chemotherapy, endocrine, and targeted therapy regimens given, and the details of PORT in specific patients, which may be potentially confounding factors in assessing the effect of tumor laterality on cardiac morbidity of patients.
Conclusion
In conclusion, with a median follow-up of 8.8 years, no significant differences were found in cardiac-related mortality between left- and right-sided tumors in the current radiation practices of breast cancer. Longer follow-up studies with modern adjuvant radiotherapy are needed to assess the effects of tumor laterality on cardiac-related mortality in breast cancer patients.
Acknowledgments
This work was partly supported by the Natural Science Foundation of Fujian Province (No. 2015J01563), and the Medical Innovation Program of Fujian Province (No. 2017-CXB-14).
Disclosure
The authors report no conflicts of interest in this work.
References
- Blichert-ToftMNielsenMDüringMLong-term results of breast conserving surgery vs. mastectomy for early stage invasive breast cancer: 20-year follow-up of the Danish randomized DBCG-82TM protocolActa Oncol200847467268118465335
- OvergaardMHansenPSOvergaardJPostoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. Danish Breast Cancer Cooperative Group 82b TrialN Engl J Med1997337149499559395428
- KatzAStromEABuchholzTALocoregional recurrence patterns after mastectomy and doxorubicin-based chemotherapy: implications for postoperative irradiationJ Clin Oncol200018152817282710920129
- McgalePDarbySCHallPIncidence of heart disease in 35,000 women treated with radiotherapy for breast cancer in Denmark and SwedenRadiother Oncol2011100216717521752480
- BoekelNBSchaapveldMGietemaJACardiovascular Disease Risk in a Large, Population-Based Cohort of Breast Cancer SurvivorsInt J Radiat Oncol Biol Phys20169451061107227026313
- DarbySCEwertzMMcgalePRisk of ischemic heart disease in women after radiotherapy for breast cancerN Engl J Med20133681198799823484825
- TaylorCWBrønnumDDarbySCCardiac dose estimates from Danish and Swedish breast cancer radiotherapy during 1977-2001Radiother Oncol2011100217618321376412
- SardarPKunduAChatterjeeSLong-term cardiovascular mortality after radiotherapy for breast cancer: A systematic review and meta-analysisClin Cardiol2017402738128244595
- HensonKEMcgalePTaylorCDarbySCRadiation-related mortality from heart disease and lung cancer more than 20 years after radiotherapy for breast cancerBr J Cancer2013108117918223257897
- RehammarJCJensenMBMcgalePRisk of heart disease in relation to radiotherapy and chemotherapy with anthracyclines among 19,464 breast cancer patients in Denmark, 1977-2005Radiother Oncol2017123229930528365142
- BouillonKHaddyNDelalogeSLong-term cardiovascular mortality after radiotherapy for breast cancerJ Am Coll Cardiol201157444545221251585
- Paul WrightGDrinaneJJSobelHLChungMHLeft-Sided Breast Irradiation does not Result in Increased Long-Term Cardiac-Related Mortality Among Women Treated with Breast-Conserving SurgeryAnn Surg Oncol20162341117112226530446
- SoranOVargoJAPolatAVNo association between left- breast radiation therapy or breast arterial calcification and long-term cardiac events in patients with breast cancerJ Womens Health2014231210051011
- ParkCKLiXStarrJHarrisEECardiac morbidity and mortality in women with ductal carcinoma in situ of the breast treated with breast conservation therapyBreast J201117547047621762242
- RutterCEChagparABEvansSBBreast cancer laterality does not influence survival in a large modern cohort: implications for radiation-related cardiac mortalityInt J Radiat Oncol Biol Phys201490232933425304793
- BoeroIJParavatiAJTriplettDPModern Radiation Therapy and Cardiac Outcomes in Breast CancerInt J Radiat Oncol Biol Phys201694470070826972642
- HaqueRYoodMUGeigerAMLong-term safety of radiotherapy and breast cancer laterality in older survivorsCancer Epidemiol Biomarkers Prev201120102120212621878589
- Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: Incidence – SEER 18 Regs Custom Data (with chemotherapy recode), Nov 2015 Sub (2000–2013) <Katrina/Rita Population Adjustment> – Linked To County Attributes – Total US, 1969–2014 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released July 2016, based on the November 2015 submission. Available from: www.seer.cancer.gov.
- WangWO’ConnellDStuartKBoyagesJAnalysis of 10-year cause- specific mortality of patients with breast cancer treated in New South Wales in 1995J Med Imaging Radiat Oncol201155551652522008173
- ShahCBadiyanSBerrySCardiac dose sparing and avoidance techniques in breast cancer radiotherapyRadiother Oncol2014112191624813095
- PalumboIPalumboBFravoliniMLBrain natriuretic peptide as a cardiac marker of transient radiotherapy-related damage in left-sided breast cancer patients: A prospective studyBreast201625455026547836
- D’ErricoMPGrimaldiLPetruzzelliMFN-terminal pro-B-type natriuretic peptide plasma levels as a potential biomarker for cardiac damage after radiotherapy in patients with left-sided breast cancerInt J Radiat Oncol Biol Phys2012822e239e24621640499
- TaylorCWWangZMacaulayEExposure of the Heart in Breast Cancer Radiation Therapy: A Systematic Review of Heart Doses Published During 2003 to 2013Int J Radiat Oncol Biol Phys201593484585326530753
- DumaMNMünchSOechsnerMCombsSEAre heart toxicities in breast cancer patients important for radiation oncologists? A practice pattern survey in German speaking countriesBMC Cancer201717156328835224
- van den BogaardVATaBDvan der SchaafAValidation and Modification of a Prediction Model for Acute Cardiac Events in Patients With Breast Cancer Treated With Radiotherapy Based on Three-Dimensional Dose Distributions to Cardiac SubstructuresJ Clin Oncol201735111171117828095159
- PoortmansPMColletteSKirkoveCInternal Mammary and Medial Supraclavicular Irradiation in Breast CancerN Engl J Med2015373431732726200978
- WhelanTJOlivottoIAParulekarWRRegional Nodal Irradiation in Early-Stage Breast CancerN Engl J Med2015373430731626200977
- National Comprehensive Cancer Network Available from: https://www.nccn.org/professionals/physician_gls/pdf/breast.pdfAccessed April 11, 2018
- ChargariCKirovKMBolletMACardiac toxicity in breast cancer patients: from a fractional point of view to a global assessmentCancer Treat Rev201137432133020864260
- RangerADunlopAHutchinsonKA Dosimetric Comparison of Breast Radiotherapy Techniques to Treat Locoregional Lymph Nodes Including the Internal Mammary ChainClin Oncol2018306346353
- GiordanoSHKuoYFFreemanJLRisk of cardiac death after adjuvant radiotherapy for breast cancerJ Natl Cancer Inst200597641942415770005
- PattDAGoodwinJSKuoYFCardiac morbidity of adjuvant radiotherapy for breast cancerJ Clin Oncol200523307475748216157933
- RudatVAlaradiAAMohamedAAi-YahyaKAltuwaijriSTangential beam IMRT versus tangential beam 3D-CRT of the chest wall in postmastectomy breast cancer patients: a dosimetric comparisonRadiat Oncol201162621418616
- MaCZhangWLuJDosimetric Comparison and Evaluation of Three Radiotherapy Techniques for Use after Modified Radical Mastectomy for Locally Advanced Left-sided Breast CancerSci Rep201551227426194593
- van DykeMGreerSOdomEHeart Disease Death Rates Among Blacks and Whites Aged ≥35 Years – United States, 1968-2015MMWR Surveill Summ2018675111
- SidneySSorelMEQuesenberryCPComparative Trends in Heart Disease, Stroke, and All-Cause Mortality in the United States and a Large Integrated Healthcare Delivery SystemAm J Med2018131782983629625083
- SchultzWMHayekSSSamman TahhanAMarital Status and Outcomes in Patients With Cardiovascular DiseaseJ Am Heart Assoc2017612pii: e005890
- ManfrediniRde GiorgiATiseoRMarital Status, Cardiovascular Diseases, and Cardiovascular Risk Factors: A Review of the EvidenceJ Womens Health2017266624632
- DarbySCMcgalePTaylorCWPetoRLong-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: prospective cohort study of about 300,000 women in US SEER cancer registriesLancet Oncol20056855756516054566