Abstract
Background
Many studies have evaluated the relationship between alkaline phosphatase (ALP) and the prognosis for prostate cancer (PCa). But they have not reached a widespread consensus yet. Therefore, we completed a meta-analysis to ascertain the significance of ALP and the prognosis for PCa.
Methods
A literature search was performed in the PubMed, Embase, and Web of Science databases. HRs concerning overall survival (OS), progression-free survival (PFS), and cancer-specific survival (CSS) were extracted to evaluate the impacts of ALP on the prognosis for PCa. Subgroup analyses were conducted on different study types, regions, sample sizes, and cutoff values. Sensitivity analysis was performed by removing one study in sequence.
Results
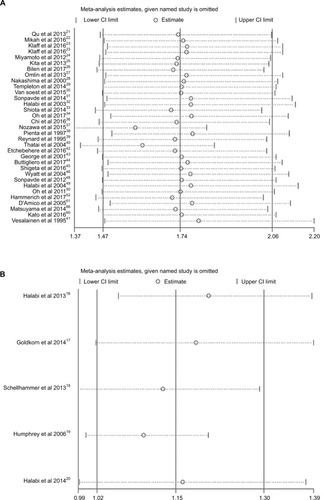
A total of 63 studies from 54 articles with 16,135 patients were included in this meta-analysis. The pooled results indicated that high baseline ALP was associated with obviously poor OS (HR=1.74, 95% CI: 1.47–2.06) and PFS (HR=1.60, 95% CI: 1.13–2.26) in patients with PCa. The pooled HR for bone-specific ALP and OS was 1.76 (95% CI: 1.45–2.15). However, no association between ALP and CSS (HR=1.002, 95% CI: 0.998–1.005) was found for PCa. The results of subgroup analyses were all in accordance with the main findings. Sensitivity analysis suggested that no single study could affect the stability of the results.
Conclusion
High serum ALP is significantly associated with poor OS and PFS except for CSS in PCa. ALP is an efficient and convenient biomarker for PCa prognosis.
Introduction
Prostate cancer (PCa) is the most common malignancy in western males.Citation1 It is estimated that 164,690 new PCa cases and 29,430 PCa-related deaths will occur in 2018 in USA.Citation1 So far, prostate-specific antigen (PSA) has been mostly used for early detection and recurrence evaluation as a biomarker. Gleason score is a classical prognostic factor but not sufficient to portray the complexity of clinical prognosis.Citation2 The heterogeneous genomic property of PCa can lead to the difficulty in survival prognosis and therapy monitoring. Therefore, there is an urgent need for novel effective parameters to predict outcomes for treatment decision. Recently, a number of biomarkers about PCa have been investigated and established in patient cohort studies.Citation3–Citation6 In comparison with cancer tissues, serum is an ideal source of biomarkers because of the convenience in routine clinical measurement.Citation7 Scientists have been trying for decades to seek the biomarkers among the different kinds of molecules such as proteins, noncoding RNAs, and chemical compounds.Citation8 Interestingly, we notice that alkaline phosphatase (ALP), a classical parameter, also has a great potential in the prognosis of PCa.
The enzyme ALP can physiologically dephosphorylate compounds under alkaline pH environment.Citation9 Serum ALP level is a widely used parameter for liver disease, bone disease burden, and treatment effects.Citation10 It is acknowledged that the elevation in ALP level is positively related to the rise of bone activity like osteosarcoma.Citation11 Therefore, we speculate that bone metastatic cancer may also lead to the rising of serum ALP, given that bone is the most common metastatic site of PCa. Over 85% patients died from bone metastasis among PCa-related deaths.Citation12 So, can we identify the relationship between ALP and different survival outcomes in patients with PCa?
Up to now, the prognostic performance of ALP in patients with PCa has been discussed in many studies; however, these studies have yielded some conflicting conclusions. The aim of this study was to quantitatively and comprehensively derive a more precise prognostic estimation of ALP in patients with PCa by a meta-analysis.
Methods
Search strategy
This meta-analysis adhered to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).Citation13 A comprehensive literature search in the PubMed, Embase, and Web of Science was conducted from the databases onset to February 5, 2018. The key words were as follows: (“prostate neoplasms[MeSH]” OR “prostate cancer”) AND “alkaline phosphatase” or “ALP” AND (“prognosis[MeSH]” OR “survival” OR “outcome”). The language of studies was not restricted. Additional relevant publications were also manually searched based on the reference lists.
Study selection
Inclusion and exclusion criteria
Studies were included only if they met the following criteria: 1) clinical cohort/trial evaluated the prognostic ability of ALP in PCa; 2) studies compared ALP with other prognostic models and reported survival outcomes such as overall survival (OS), progression-free survival (PFS), and cancer-specific survival (CSS); 3) reported original HR with 95% CI or the HR could be calculated from sufficient data; 4) articles with the most complete information if there were several studies among overlapping cohorts or time periods.
The exclusion criteria were 1) duplicate publications; 2) studies based on less than 20 patients; 3) laboratory studies, animal studies, letters, or review articles.
Assessment of study quality
Two investigators (DL and XH) independently reviewed all the relevant articles, then evaluated the methodological quality of observational studies using Newcastle–Ottawa Quality Assessment Scale (NOS) assessment tool, including selection, comparability, and outcomes.Citation14 The Jadad composite scale was utilized to assess randomized controlled trials (RCTs).Citation15 The NOS score ≥7 or Jadad score ≥4 indicated high quality. Disagreements in data collection and quality assessment were resolved through consensus by involving a third author (HL).
Data extraction
The baseline and outcome data were obtained from each study: first author’s surname, year of publication, study design, country, sample size, age, PSA level, cutoff value, follow-up time, outcomes, and HRs with 95% CI. If the HRs of both univariate and multivariate analysis were available, only the latter was used.
Statistical analysis
HRs with 95% CI from all eligible studies were pooled via a meta-analysis to access the strength of ALP to survival endpoints. The Cochran Q test was used to determine the heterogeneity among studies. A P value <0.10 indicated heterogeneity. The inconsistency (I2) was also calculated to evaluate heterogeneity. An I2 value >50% indicated the presence of statistical heterogeneity. The random-effect model (DerSimonian and Laird method) was used to calculate pooled results when there was heterogeneity among included studies; otherwise, the fixed-effect model was used. To seek deeper relationship between ALP and OS, we conducted subgroup analyses on study type, cutoff value, sample size, and region of study. Furthermore, to test the reliability of the results, sensitivity analysis was conducted by removing each single study in turn. Begg’s test with funnel plots was used to measure publication bias. The P value >0.05 indicated no potential publication bias. The Stata 12.0 software (StataCorp, College Station, TX, USA) was used to perform all the statistical analyses. A two-sided P value <0.05 was considered as statistically significant.
Results
Studies selection and evaluation
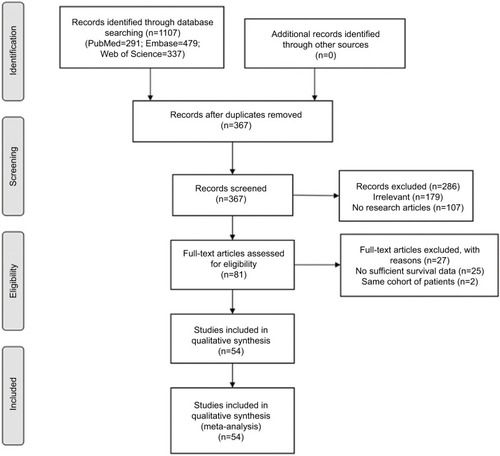
The flowchart of articles searching process is shown in . A total of 1,107 relevant citations were initially retrieved by the search strategy as described above in PubMed, Embase, and Web of Science. Seven hundred forty duplicate articles were removed. Among the remaining 367 articles, 286 were further excluded for unrelated information and not clinical research articles. Eighty-one potential articles were screened carefully, 27 articles were ruled out because of lack of essential data of survival outcome or overlapping cohorts. If there were multiple outcomes in the same article, we considered them as different studies. Finally, 63 studies from 54 articlesCitation16–Citation69 published between 1995 and 2017 encompassing 16,135 patients were included in the meta-analysis, with the sample size ranging from 30 to 1,183 patients (). The characteristics of the included studies are summarized in . The median length of follow-up varied from 8.3 to 63.4 months. Prognostic outcomes were quantitatively synthesized, including OS, CSS, and PFS. A total of 36 observational studies and five RCTs had available data for the OS analysis, while seven studies reported HRs for CSS, and nine studies reported HRs for PFS. The quality assessment results of the 54 eligible articles shown in Table S1 revealing the NOS score were equal or greater than 6 in all 48 observational studies and the Jadad score was over 4 in all six RCTs.
Table 1 Baseline characteristics of included studies
Overall analysis
Meta-analysis on OS
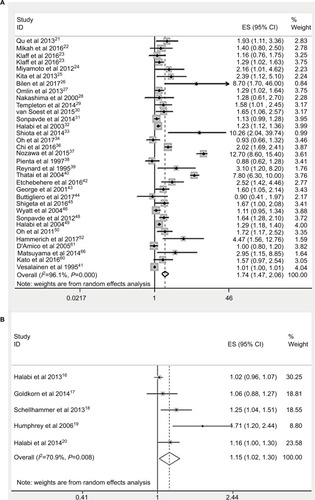
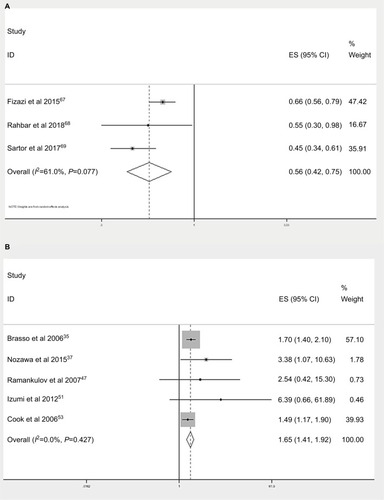
There were 33 observational studies presenting the data of ALP and OS. The random effects model was used to analyze the relationship between them. The pooled HR was 1.74 (95% CI: 1.47–2.06, ) with significant heterogeneity between studies (I2=96.1%, P<0.001), which demonstrated a significant relationship between ALP and OS. However, the pooled HR was 1.15 (95% CI: 1.02–1.30, ), which demonstrates a significant relationship among five RCTs. There were three studies comparing the decrease in serum ALP level and OS, whose pooled HR was 0.56 (95% CI: 0.42–0.75, ). Besides, five studies investigated the relationship between bone-specific ALP (BAP) and OS in patients with PCa. The pooled HR for BAP and OS is 1.65 (95% CI: 1.41–1.92, ).
Meta-analysis on CSS
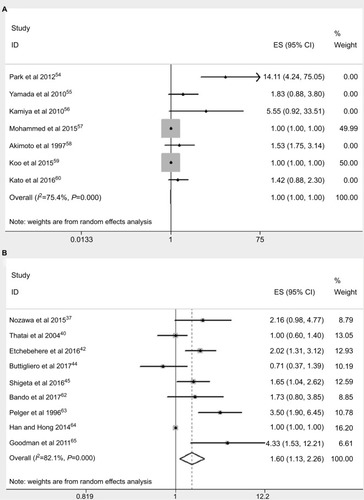
Seven studies provided sufficient data on ALP and CSS outcome. The pooled HR was 1.002 (95% CI: 0.998–1.005) via a random effects model, and the potential heterogeneity among studies was observed (I2=75.4%, P<0.001, ).
Meta-analysis on PFS
Nine studies reported the data concerning the association between ALP and PFS. Meta-analysis adopting the random effects model revealed that elevated ALP was significantly associated with shorter PFS (HR=1.60, 95% CI: 1.13–2.26) with potential heterogeneity (I2=82.1%, P<0.001, ).
Subgroup analyses
Moreover, we conducted a subgroup meta-analysis on different study designs. Although the main results were not affected by different study design, heterogeneity still existed in both prospective cohorts (HR=1.76, 95% CI: 1.42–2.19, Figure S1A) and retrospective studies (HR=1.58, 95% CI: 1.24–2.00, Figure S1B). In epidemiological studies, ethnicity difference was usually recognized as a critical source of bias. Notably, we also found the elevated serum ALP was significantly associated with poor OS among the studies in Asia (Figure S1C), Europe (Figure S1D), and North America (Figure S1E). Furthermore, we performed subgroup analysis in different cutoff values (Figure S1F, G) and sample sizes (Figure S1H, I). To sum up, the pooled HRs indicated that higher ALP was significantly associated with poorer OS in all subgroups of patients with PCa ().
Table 2 Summary of the subgroup analysis results of ALP and OS prognosis for PCa
Sensitivity analysis
The sensitivity analysis was performed by the sequential deletion of any individual article to measure the effects of each individual study. The results showed that the overall HRs were not significantly influenced by individual study, as shown in , indicating the robustness of the results in our meta-analysis.
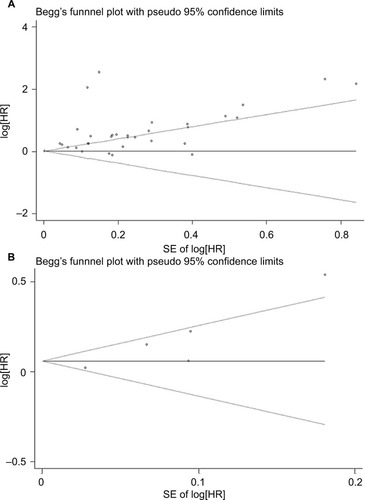
Assessment of publication bias
Begg’s test was performed to evaluate the publication bias of the inclusion studies (). The P-values of Begg’s test for OS (observational studies and RCTs) were 0.747 and 0.086, respectively, indicating that there was no significant publication bias.
Discussion
Serum ALP level is a simple and rapid laboratory test in routine clinical practice. An ideal prognostic biomarker can be used to determine prognosis, monitor response to therapy, and postoperative surveillance.Citation70 The high ALP level has been reported related to the poor survival in colorectal cancer.Citation71 The elevation of ALP is also an independent risk factor in the bone metastasis of gastric cancer and bladder cancer.Citation72,Citation73 However, the underlying mechanisms of ALP in patients with PCa remain unclear. A possible explanation is that when the PCa starts metastasis, ALP reflects bone turnover, osteoblast activity, and the osteoid formation in adjacent bone tissues.Citation11 Thus, ALP may be an indicator of bone metastatic tumor load.
In this meta-analysis, based on the existing data from 63 included studies, the pooled results indicated that high baseline ALP was associated with obviously poor OS and PFS (HR=1.60, 95% CI: 1.13–2.26) in patients with PCa. As presented in , most included studies used multivariate cox model to explore ALP and survival. After being adjusted for other factors such as tumor stage/grade, PSA, Gleason score, hemoglobin, and metastasis, the original results of ALP were objective and reliable. The meta-analysis on both observational studies (HR=1.74, 95% CI: 1.47–2.06) and RCTs (HR=1.15, 95% CI: 1.02–1.30) reached the consistent conclusions about ALP and OS. In addition, high serum BAP was also significantly related to poor OS (HR=1.76, 95% CI: 1.42–2.15). However, our result revealed that there was no association between ALP and CSS in patients with PCa (HR=1.002, 95% CI: 0.998–1.005). We hypothesize that ALP is more sensitive in reflecting bone metastasis, so, high serum ALP is significantly associated with PFS of PCa. PCa patients with bone metastasis and other underlying diseases may lead to poorer OS. Whereas the seven studies about CSS () were all retrospective in the study design. The sample size was also relatively smaller for CSS than OS. Thus, we should carefully interpret the result of ALP and CSS. The results of subgroup analyses on different study types, regions, cutoff values, and sample sizes were all in accordance with the main findings. The sensitivity analysis and publication bias tests’ outcomes also supported our results. Therefore, we may recommend ALP as a valuable prognostic marker for PCa treatment decision and adjustment. Compared with the positron emission tomography-computed tomography, ALP combined with bone scintigraphy may also be useful to assess the metastatic burden and survival possibility of PCa with a remarkably less expensive cost.
To our knowledge, this is the first meta-analysis on ALP and the prognosis of PCa. However, there are still a couple of limitations to be stated. First, although the language was not restricted during the searching process, all the included studies were in English, which might lead to language bias. Second, although sensitivity analysis supported the stability of our results, the findings should be cautiously interpreted. Heterogeneity among studies was found in overall and subgroup analyses. It was probably owing to multivariate factors in some included studies. Third, the data of ALP on other prognostic clinical parameters such as metastasis and all-cause mortality are lacking at present. Meanwhile, the retrospective design in 23 included studies () may cause potential recall bias. Thus, more large-scale prospective studies are warranted to testify the prognostic ability of ALP in PCa in the future. Moreover, BAP will also be a potential prognostic marker in PCa, which needs verification as well.
Conclusion
In spite of the limitations mentioned above, the results of this study present the conclusion that high serum ALP is significantly associated with poor OS and PFS of PCa, but there is no obvious relation between ALP and CSS. ALP level is an efficient and convenient biomarker for PCa prognosis.
Acknowledgments
This study was supported by the Natural Science Foundation of Liaoning Province (program No.: 2015020275)
Author contributions
YS and BH were involved in project development; DL and HL helped to collect and manage data; DL, HL, and XH analyzed the data; DL wrote/edited the manuscript; YS and BH helped in critical revision of the manuscript. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- SiegelRLMillerKDJemalACancer statistics, 2018CA Cancer J Clin201868173029313949
- LiuYThe context of prostate cancer genomics in personalized medicineOncol Lett20171353347335328521441
- LiDYHaoXYMaTMDaiHXSongYSThe prognostic value of platelet-to-lymphocyte ratio in urological cancers: a meta-analysisSci Rep2017711538729133845
- LiDLvHHaoXDongYDaiHSongYPrognostic value of bone scan index as an imaging biomarker in metastatic prostate cancer: a meta-analysisOncotarget2017848844498445829137438
- GraffREPetterssonALisRTDietary lycopene intake and risk of prostate cancer defined by ERG protein expressionAm J Clin Nutr2016103385186026817504
- CochettiGPoliGGuelfiGBoniAEgidiMGMeariniEDifferent levels of serum microRNAs in prostate cancer and benign prostatic hyperplasia: evaluation of potential diagnostic and prognostic roleOnco Targets Ther201697545755328008272
- ZhangMChenLYuanZCombined serum and EPS-urine proteomic analysis using iTRAQ technology for discovery of potential prostate cancer biomarkersDiscov Med20162212228129528009970
- SalviSGurioliGde GiorgiUCell-free DNA as a diagnostic marker for cancer: current insightsOnco Targets Ther201696549655927822059
- SharmaUPalDPrasadRAlkaline phosphatase: an overviewIndian J Clin Biochem201429326927824966474
- FanYJinXJiangMFangNElevated serum alkaline phosphatase and cardiovascular or all-cause mortality risk in dialysis patients: A meta-analysisSci Rep2017711322429038525
- RenH-YSunL-LLiH-YYeZ-MPrognostic significance of serum alkaline phosphatase level in osteosarcoma: a meta-analysis of published dataBiomed Res Int201520151016083526618165
- GrootMTBoeken KrugerCGPelgerRCUyl-de GrootCACosts of prostate cancer, metastatic to the bone, in The NetherlandsEur Urol200343322623212600424
- MoherDLiberatiATetzlaffJAltmanDGPRISMA GroupPreferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA StatementPLoS Med200967e100009719621072
- StangACritical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analysesEur J Epidemiol201025960360520652370
- JadadARMooreRACarrollDAssessing the quality of reports of randomized clinical trials: Is blinding necessary?Control Clin Trials19961711128721797
- HalabiSLinCYSmallEJPrognostic model predicting metastatic castration-resistant prostate cancer survival in men treated with second-line chemotherapyJ Natl Cancer Inst2013105221729173724136890
- GoldkornAElyBQuinnDICirculating tumor cell counts are prognostic of overall survival in SWOG S0421: a phase III trial of docetaxel with or without atrasentan for metastatic castration-resistant prostate cancerJ Clin Oncol201432111136114224616308
- SchellhammerPFChodakGWhitmoreJBSimsRFrohlichMWKantoffPWLower baseline prostate-specific antigen is associated with a greater overall survival benefit from sipuleucel-T in the Immunotherapy for Prostate Adenocarcinoma Treatment (IMPACT) trialUrology20138161297130223582482
- HumphreyPAHalabiSPicusJPrognostic significance of plasma scatter factor/hepatocyte growth factor levels in patients with metastatic hormone-refractory prostate cancer: results from cancer and leukemia group B 150005/9480Clin Genitourin Cancer20064426927416729910
- HalabiSLinCYKellyWKUpdated prognostic model for predicting overall survival in first-line chemotherapy for patients with metastatic castration-resistant prostate cancerJ Clin Oncol201432767167724449231
- QuYyDaiBKongYYPrognostic factors in Chinese patients with metastatic castration-resistant prostate cancer treated with docetaxel-based chemotherapyAsian J Androl201315111011523147466
- MikahPKrabbeLMEminagaODynamic changes of alkaline phosphatase are strongly associated with PSA-decline and predict best clinical benefit earlier than PSA-changes under therapy with abiraterone acetate in bone metastatic castration resistant prostate cancerBMC Cancer201616121426975660
- KlaffRVarenhorstEBerglundAClinical presentation and predictors of survival related to extent of bone metastasis in 900 prostate cancer patientsScand J Urol201650535235927603423
- MiyamotoSItoKMiyakuboMImpact of pretreatment factors, biopsy Gleason grade volume indices and post-treatment nadir PSA on overall survival in patients with metastatic prostate cancer treated with step-up hormonal therapyProstate Cancer Prostatic Dis2012151758621986985
- KitaYShimizuYInoueTKambaTYoshimuraKOgawaOReduced-dose docetaxel for castration-resistant prostate cancer has no inferior impact on overall survival in Japanese patientsInt J Clin Oncol201318471872322791141
- BilenMAHessKRSubudhiSKClinical predictors of survival in patients with castration-resistant prostate cancer receiving sipuleucel-T cellular immunotherapyCancer Chemother Pharmacol201780358358928730293
- OmlinAPezaroCMukherjiDImproved survival in a cohort of trial participants with metastatic castration-resistant prostate cancer demonstrates the need for updated prognostic nomogramsEur Urol201364230030623313031
- NakashimaJOzuCNishiyamaTPrognostic value of alkaline phosphatase flare in patients with metastatic prostate cancer treated with endocrine therapyUrology200056584384711068314
- TempletonAJPezaroCOmlinASimple prognostic score for metastatic castration-resistant prostate cancer with incorporation of neutrophil-to-lymphocyte ratioCancer2014120213346335224995769
- van SoestRJNieuweboerAJMde MorréeESThe influence of prior novel androgen receptor targeted therapy on the efficacy of cabazitaxel in men with metastatic castration-resistant prostate cancerEur J Cancer201551172562256926278646
- SonpavdeGPondGRArmstrongAJPrognostic impact of the neutrophil-to-lymphocyte ratio in men with metastatic castration-resistant prostate cancerClin Genitourin Cancer201412531732424806399
- HalabiSSmallEJKantoffPWPrognostic model for predicting survival in men with hormone-refractory metastatic prostate cancerJ Clinic Oncol200321712321237
- ShiotaMYokomizoAAdachiTThe oncological outcomes and risk stratification in docetaxel chemotherapy for castration-resistant prostate cancerJpn J Clin Oncol201444986086724951829
- OhWKMiaoRVekemanFPatient characteristics and overall survival in patients with post-docetaxel metastatic castration-resistant prostate cancer in the community settingMed Oncol201734916028795333
- BrassoKChristensenIJJohansenJSPrognostic value of PINP, bone alkaline phosphatase, CTX-I, and YKL-40 in patients with metastatic prostate carcinomaProstate200666550351316372331
- ChiKNKheohTRyanCJA prognostic index model for predicting overall survival in patients with metastatic castration-resistant prostate cancer treated with abiraterone acetate after docetaxelAnn Oncol201627345446026685010
- NozawaMHaraIMatsuyamaHSignificance of baseline bone markers on disease progression and survival in hormone-sensitive prostate cancer with bone metastasisWorld J Urol20153391263126825354720
- PientaKJRedmanBGBandekarRA phase II trial of oral estramustine and oral etoposide in hormone refractory prostate cancerUrology19975034014079301705
- ReynardJMPetersTJGillattDProstate-specific antigen and prognosis in patients with metastatic prostate cancer - a multivariable analysis of prostate cancer mortalityBr J Urol19957545075157540483
- ThataiLCBanerjeeMLaiZVaishampayanURacial disparity in clinical course and outcome of metastatic androgen-independent prostate cancerUrology200464473874315491712
- VesalainenSLipponenPTaljaMSyrjänenKBiochemical parameters as prognostic factors in prostatic adenocarcinomaActa Oncol19953415359
- EtchebehereECMiltonDRAraujoJCSwanstonNMMacapinlacHARohrenEMFactors affecting 223Ra therapy: clinical experience after 532 cycles from a single institutionEur J Nucl Med Mol Imaging201643182026416392
- GeorgeDJHalabiSShepardTFPrognostic significance of plasma vascular endothelial growth factor levels in patients with hormone-refractory prostate cancer treated on Cancer and Leukemia Group B 9480Clin Cancer Res2001771932193611448906
- ButtiglieroCPisanoCTucciMPrognostic impact of pretreatment neutrophil-to-lymphocyte ratio in castration-resistant prostate cancer patients treated with first-line docetaxelActa Oncol201756455556228068151
- ShigetaKKosakaTKitanoSHigh absolute monocyte count predicts poor clinical outcome in patients with castration-resistant prostate cancer treated with docetaxel chemotherapyAnn Surg Oncol201623124115412227364499
- WyattRBSanchez-OrtizRFWoodCGRamirezELogothetisCPettawayCAPrognostic factors for survival among Caucasian, African-American and Hispanic men with androgen-independent prostate cancerJ Natl Med Assoc200496121587159315622688
- RamankulovALeinMKristiansenGLoeningSAJungKPlasma osteopontin in comparison with bone markers as indicator of bone metastasis and survival outcome in patients with prostate cancerProstate200767333034017192877
- SonpavdeGPondGRBerryWRSerum alkaline phosphatase changes predict survival independent of PSA changes in men with castration-resistant prostate cancer and bone metastasis receiving chemotherapyUrol Oncol201230560761320888271
- HalabiSSmallEJVogelzangNJBarrierRCGeorgeSLGilliganTDImpact of race on survival in men with metastatic hormone-refractory prostate cancerUrology200464221221715302462
- OhWKVargasRJacobusSElevated plasma tissue inhibitor of metalloproteinase-1 levels predict decreased survival in castration-resistant prostate cancer patientsCancer2011117351752520862742
- IzumiKMizokamiAItaiSIncreases in bone turnover marker levels at an early phase after starting zoledronic acid predicts skeletal-related events in patients with prostate cancer with bone metastasisBJU Int2012109339440021599822
- HammerichKHDonahueTFRosnerILAlkaline phosphatase velocity predicts overall survival and bone metastasis in patients with castration-resistant prostate cancerUrologic Oncology201735460.e21e28
- CookRJColemanRBrownJMarkers of bone metabolism and survival in men with hormone-refractory metastatic prostate cancerClin Cancer Res200612113361336716740758
- ParkJMNamJSNaWPrognostic value of body mass index in Korean patients with castration-resistant prostate cancerKorean J Urol2012531176176523185667
- YamadaYNaruseKNakamuraKInvestigation of risk factors for prostate cancer patients with bone metastasis based on clinical dataExp Ther Med20101463563922993586
- KamiyaNSuzukiHYanoMImplications of serum bone turnover markers in prostate cancer patients with bone metastasisUrology20107561446145120206975
- MohammedAAEl-TanniHGhanemHMImpact of body mass index on clinico-pathological parameters and outcome in patients with metastatic prostate cancerJ Egypt Natl Canc Inst201527315515926227217
- AkimotoSInomiyaHAkakuraKShimazakiJItoHPrognostic factors in patients with prostate cancer refractory to endocrine therapy: univariate and multivariate analyses including doubling times of prostate-specific antigen and prostatic acid phosphataseJpn J Clin Oncol19972742582629379515
- KooKCParkSUKimKHPredictors of survival in prostate cancer patients with bone metastasis and extremely high prostate-specific antigen levelsProstate Int201531101526157761
- KatoMTsuzukiTKimuraKThe presence of intraductal carcinoma of the prostate in needle biopsy is a significant prognostic factor for prostate cancer patients with distant metastasis at initial presentationMod Pathol201629216617326743470
- D’AmicoAVChenMHCoxMCDahutWFiggWDProstate-specific antigen response duration and risk of death for patients with hormone-refractory metastatic prostate cancerUrology200566357157616140080
- BandoYHinataNTerakawaTActivity of cabazitaxel in patients with metastatic castration-resistant prostate cancer after treatment with single or dual regimens of novel androgen receptor-targeting agentsMed Oncol201734916328819719
- PelgerRCLycklamaANijeholtGAZwindermanAHPapapoulosSEHamdyNAThe flare in serum alkaline phosphatase activity after orchiectomy: a valuable negative prognostic index for progression-free survival in prostatic carcinomaJ Urol199615611221268648772
- HanKSHongSJSerum alkaline phosphatase differentiates prostate-specific antigen flare from early disease progression after docetaxel chemotherapy in castration-resistant prostate cancer with bone metastasisJ Cancer Res Clin Oncol2014140101769177624858569
- GoodmanOBSymanowskiJTLoudyiAFinkLMWardDCVogel-zangNJCirculating tumor cells as a predictive biomarker in patients with hormone-sensitive prostate cancerClin Genitourin Cancer201191313821705286
- MatsuyamaHShimabukuroTHaraICombination of hemoglobin, alkaline phosphatase, and age predicts optimal docetaxel regimen for patients with castration-resistant prostate cancerInt J Clin Oncol201419594695424272390
- FizaziKMassardCSmithMBone-related parameters are the main prognostic factors for overall survival in men with bone metastases from castration-resistant prostate cancerEur Urol2015681425025449207
- RahbarKBoegemannMYordanovaAPSMA targeted radio-ligand therapy in metastatic castration resistant prostate cancer after chemotherapy, abiraterone and/or enzalutamide. A retrospective analysis of overall survivalEur J Nucl Med Mol Imaging2018451121929026946
- SartorOColemanRENilssonSAn exploratory analysis of alkaline phosphatase, lactate dehydrogenase, and prostate-specific antigen dynamics in the phase 3 ALSYMPCA trial with radium-223Ann Oncol20172851090109728453701
- NowsheenSAzizKPanayiotidisMIGeorgakilasAGMolecular markers for cancer prognosis and treatment: have we struck gold?Cancer Lett20123271–214215222120674
- LiuFZhaoJXieJPrognostic risk factors in patients with bone metastasis from colorectal cancerTumour Biol201637121612716134
- LimSMKimYNParkKHBone alkaline phosphatase as a surrogate marker of bone metastasis in gastric cancer patientsBMC Cancer201616138527377907
- HuangPLanMPengAFSerum calcium, alkaline phosphatase and hemoglobin as risk factors for bone metastases in bladder cancerPLoS One2017129e018383528902911