Abstract
Background
Elevated plasma fibrinogen levels have been associated with tumor progression in several malignancies. Our study aims to characterize the clinical significance of elevated plasma fibrinogen levels in patients with hepatocellular carcinoma (HCC).
Materials and methods
Relevant published articles were systematically searched in electronic databases including PubMed, Embase, and Web of Science. The pooled differences in plasma fibrinogen levels among HCC, cirrhotic, and control groups were expressed as weighted mean differences (WMDs) and their corresponding 95% CIs. The associations between elevated fibrinogen and overall survival (OS) and disease-free survival (DFS)/recurrence-free survival (RFS) were expressed as HRs and their 95% CIs, whereas the associations between elevated fibrinogen and various types of clinical characteristic of patients with HCC were expressed as ORs and their corresponding 95% CIs.
Results
Results showed that the plasma fibrinogen levels in patients with HCC were not significantly different than that in healthy controls (WMD = 0.50, 95% CI = [−0.82, 1.82], P = 0.457) or patients with cirrhosis (WMD = −0.62, 95% CI = [−1.56, 0.33], P = 0.200). However, our results showed that compared to those with normal levels, patients with HCC and elevated plasma fibrinogen levels showed poorer OS (HR = 2.08, 95% CI = [1.67, 2.59], P < 0.0001) and DFS/RFS (HR = 1.90, 95% CI = [1.52, 2.37], P < 0.0001). Results of trial sequential analysis of the OS indicated that currently available studies were sufficient to validate the negative prognostic value of elevated plasma fibrinogen in patients with HCC. Clinicopathological analyses showed that high plasma fibrinogen levels were associated with tumor progression as indicated by advanced tumor stage, larger tumor size, increased tumor number, and the presence of vascular invasion.
Conclusion
Elevated plasma fibrinogen levels are associated with poor prognosis and advanced tumor progression. Plasma fibrinogen may serve as a negative prognostic biomarker in patients with HCC.
Introduction
Hepatocellular carcinoma (HCC) is a primary malignancy of the liver and is now the second leading cause of cancer deaths worldwide, following lung cancer.Citation1 The global incidence of HCC is still on the rise with the highest prevalence in East Asia,Citation1 where the mortality rate is 33.5 per 100,000 people.Citation2 The majority of HCC cases occur with underlying chronic hepatitis B or C viral infection and cirrhosis.Citation3,Citation4 The other main risk factors for HCC are alcohol intoxication and aflatoxin.Citation3,Citation5 Current treatment modalities include radical therapies (eg, surgical resection, liver transplantation, radiofrequency ablation) and adjuvant therapies (eg, transarterial chemoembolization [TACE], systemic chemotherapy, sorafenib). Although these methods have significantly improved the long-term survival of patients with HCC, the overall prognosis is largely limited by the extent of liver dysfunction.Citation6 Although various tumor staging systems are available to predict prognosis, they too have major limitations. For instance, the Milan criteria are solely based on the preoperative imaging without consideration of molecular signaturesCitation7 and biopsy has the risk of introducing tumor cell seeding.Citation8 Therefore, it would be useful to identify effective preoperative prognostic biomarkers that may facilitate outcome prediction and indicate the requirement for aggressive therapy in high-risk patients with HCC.
To date, the most common serum biomarker used by clinicians to diagnose HCC is alpha-fetoprotein (AFP). However, the reliability of AFP is questionable due to its lack of sensitivity and specificity.Citation9 In addition, AFP marker is less valuable in the early stages of HCC when the tumor size is less than 3 cm.Citation10 Therefore, new and more effective prognostic serum biomarkers are needed to improve clinical outcomes.
Fibrinogen is a 340-kDa soluble plasma glycoprotein synthesized in the liver by hepatocytes. It is an important coagulation factor. In the coagulation cascade, fibrinogen is enzymatically converted to fibrin by activated thrombin and subsequently forms a clot. In situations such as tissue injury, infection, and inflammation, fibrinogen concentrations are rapidly elevated.Citation11,Citation12 Recently, emerging evidence has associated the elevation of fibrinogen level with tumor progression in several malignancies, such as breast cancer,Citation13 gallbladder cancer,Citation14 gastric cancer,Citation15 colorectal cancer,Citation16 and lung cancer.Citation17 Few studies have also reported that patients with HCC and elevated pretreatment plasma fibrinogen levels have poor outcomes.Citation18,Citation19 However, these studies were limited in size, varied in cutoff concentrations, or administered heterogenous treatments, and the correlations between elevated fibrinogen and clinicopathological parameters of HCC were unclear. In addition, there are conflicting findings on the levels of plasma fibrinogen in HCC patients compared to that in control or cirrhotic groups. Several studies reported that HCC patients showed higher levels of pretreatment plasma fibrinogen compared to healthy controls or cirrhotic patients.Citation20–Citation22 However, Basili et alCitation23 and Liu et alCitation24 found no significant difference in the plasma fibrinogen levels between HCC and control or cirrhotic groups, and Hessien et alCitation25 indicated lower levels of fibrinogen in HCC patients compared to that in control and cirrhotic patients. Therefore, our present study aims to summarize the currently available studies to examine 1) whether the pretreatment plasma fibrinogen levels were significantly different among HCC, cirrhotic, and healthy subjects; 2) the association between elevated plasma fibrinogen and prognosis in patients with HCC; and 3) the association between elevated fibrinogen levels and tumor progression in patients with HCC. To the best of our knowledge, no meta-analysis has been performed to assess elevated plasma fibrinogen risk in patients with HCC.
Materials and methods
This meta-analysis was conducted in accordance with the PRISMA guidelines. The studies included in this meta-analysis are previously published, and therefore, ethical approval and informed consent are not required.
Literature search strategy
Relevant published literatures were systematically searched in electronic databases including PubMed, Embase, and Web of Science. The last update was September 2017. The keywords used included “Fibrinogen”, “liver neoplasm”, and “hepatocellular carcinoma”. Specifically, the keywords used in PubMed were (Fibrinogen) AND (neoplasm, liver [MeSH Terms] OR hepatocellular carcinoma). In Embase, the keywords used were Quick search: Fibrinogen AND (liver neoplasm OR hepatocellular carcinoma). In Web of Science, the keywords used were Fibrinogen AND (liver neoplasm OR hepatocellular carcinoma) [Topic]. There were no restrictions to the search process in terms of language, date, research design, or publication status.
Study selection criteria
Studies were included when they met the following inclusion criteria:
diagnosis of HCC was proven by pathological methods;
pretreatment plasma fibrinogen was measured in all participants;
mean and SD of pretreatment plasma fibrinogen levels were reported in patients with HCC, cirrhosis, and/or healthy controls;
complete clinicopathological characteristics were evaluated prior to treatment; and
outcomes included overall survival (OS), disease-free survival (DFS), and/or recurrence-free survival (RFS).
Studies were excluded when they met the following exclusion criteria:
experiments were performed in vitro or in vivo;
study designs were case reports and reviews;
fibrinogen peptide chains, mRNA or protein expression, or fibrinogen degradation products were measured;
conference proceedings that contained only summaries;
articles were not in English or Chinese; and
literature with data that could not be extracted.
Outcomes of interest
The primary outcomes of interest were OS, DFS, and RFS. Another outcome of interest was the association between fibrinogen levels and clinicopathological parameters. Other outcomes of interest were pretreatment plasma fibrinogen levels of HCC, cirrhotic, and/or healthy subjects.
Data extraction and quality assessment
Two independent researchers performed literature selection, evaluation, and extraction. Data on the following characteristics were retrieved: first author; year of publication; country in which the study was conducted; number of HCC, cirrhotic, and control subjects enrolled; age; sex; pretreatment plasma fibrinogen level measurements and methods; plasma fibrinogen cutoff values; methods used to determine cutoff values; treatments received; and follow-up period. Discrepancies were resolved by discussion to consensus. If both univariate and multivariate outcomes were provided in an article, we chose the latter. Efforts were made to contact the corresponding authors for any information not reported in the article.
The Newcastle–Ottawa Scale (NOS) was used to assess the quality of the studies included. NOS employs a “star” rating system that evaluates eight items, which are categorized into three domains: selection (four items: maximum one star each), comparability (one item: maximum two stars), and outcome (three items: maximum one star each). The NOS assessment, which ranges from 0 (worst) to 9 (best) stars, provides a semiquantitative appraisal for the overall quality of each study. Studies with scores of 6 or higher were regarded as high quality.
Statistical analyses
All statistical analyses were performed using Stata 13.1 (StataCorp LP, College Station, TX, USA). The pooled differences in plasma fibrinogen levels among HCC, cirrhotic, and control groups were expressed as weighted mean differences (WMDs) and their corresponding 95% CIs. The associations between elevated fibrinogen and OS or DFS/RFS were expressed as the HRs and their corresponding 95% CIs, and the associations between elevated fibrinogen and various types of clinical characteristics of patients with HCC were expressed as ORs and their corresponding 95% CIs. Heterogeneity among studies was assessed using Cochran’s Q test and Higgins I2 statistic.Citation26 If no significant heterogeneity was indicated among studies (P > 0.1, I2 < 50%), a fixed effect model was applied for analysis.Citation27 Otherwise, the random effect model was adopted.Citation28 Sensitivity analysis was performed using sequential omission of individual studies to evaluate the influence of an individual study on the overall pooled estimates. If the pooled estimates were affected after removal, it indicated that the results were inconsistent. Egger’s linear regression tests were used to assess for publication bias, and any indication of publication bias was further tested with trim and fill analysis. P < 0.05 indicated significant bias.
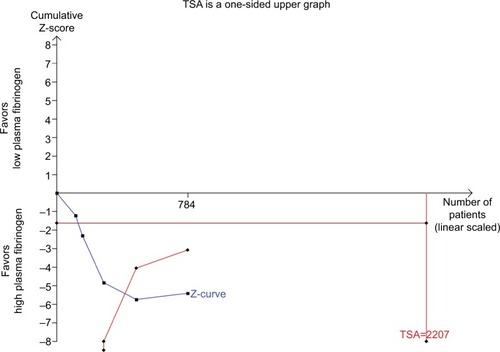
Trial sequential analysis (TSA) was conducted to minimize type I error, evaluate required information size, and assess whether current available studies were sufficient for a firm conclusion. The required information size refers to the required number of participants to produce statistically significant result in meta-analysis. The diversity-adjusted required information size of 784 patients was calculated on the basis of type I error of 5%, type II error of 20%, the control event proportion of 40%, and a relative risk reduction of 20% in outcomes. When the cumulative Z-curve crossed the trial sequential monitoring boundary for benefit, harm or futility, or the required information size, this result suggests conclusive evidence within this meta-analysis. Otherwise, more clinical studies are warranted to reach a consistent conclusion.
Results
Study selection process
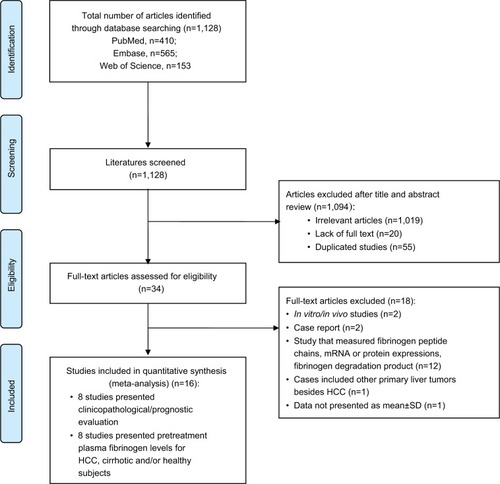
depicts the fully detailed process of article search and selection. The electronic database searches yielded a total of 1,128 potential articles (PubMed = 410, Embase = 565, and Web of Science = 153). The titles and abstracts were screened, and 1,094 articles were excluded because they covered irrelevant research topics (n = 1,019), lacked full text (n = 20), or were duplicates (n = 55). Thirty-four full-text articles were retrieved for detailed evaluation. Eighteen articles were eliminated due to the following reasons: in vivo/in vitro study (n = 2); case report (n = 2); study that measured fibrinogen peptide chains, mRNA or protein expression, or fibrinogen degradation product (n = 12); cases that included other primary liver tumor besides HCC (n = 1); and data not presented as mean ± SD (n = 1). A total of 16 articles were included in this study: eight articles measured and compared the plasma fibrinogen levels among HCC, cirrhotic, and healthy subjects, and eight articles studied the clinicopathological and prognostic value of plasma fibrinogen in HCC.
Figure 1 Flow chart of article search and selection.
Note: PLoS Medicine (OPEN ACCESS) Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. doi:10.1371/journal.pmed1000097.Citation55
Abbreviation: HCC, hepatocellular carcinoma.
Study characteristics and quality assessment
Eight studies that reported OS, DFS, or RFS were included in the meta-analysis to assess the prognostic value of plasma fibrinogen in patients with HCC. The main characteristics of the included studies are presented in . All studies were conducted in Asia, involving a total of 1,961 patients with HCC. Pretreatment plasma fibrinogen levels were measured using Clauss assay or serum biochemistry method. The cutoff values for plasma fibrinogen level were determined by different methods, including receiver operating characteristics (ROC), clinical reference range, or median. The cutoff values divided patients with HCC into an elevated plasma fibrinogen group and a normal plasma fibrinogen group. All patients with HCC also received either curative treatment or palliative treatment. In addition, eight studies were included to examine the pretreatment plasma fibrinogen levels in HCC, cirrhotic, and/or healthy subjects. Six studies presented plasma fibrinogen levels in patients with HCC and healthy controls, three studies presented data for patients with cirrhosis and controls, and six studies presented data for patients with HCC and patients with cirrhosis. The details of the studies are provided in .
We also used the NOS to evaluate the quality of the eight studies that reported OS, DFS, and RFS. All of the studies scored between 8 and 9, indicating that the quality of the included studies was high ().
Table 1 Study characteristics of the included studies for prognostic analysis
Table 2 Baseline plasma fibrinogen levels of HCC, cirrhotic, and healthy subjects
Table 3 Quality assessment of the included studies for prognostic evaluation
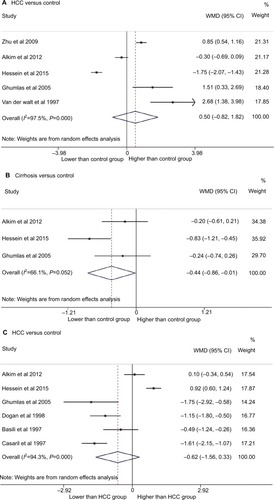
Plasma fibrinogen levels among HCC, cirrhotic, and healthy subjects
We examined the plasma fibrinogen levels in HCC, cirrhotic, and healthy subjects. A random effect model showed no significant difference in the plasma fibrinogen levels among patients with HCC and healthy controls (WMD = 0.50, 95% CI = [−0.82, 1.82], P = 0.457; ). However, compared to healthy individuals, patients with cirrhosis had significantly lower plasma fibrinogen levels (WMD = −0.44, 95% CI = [−0.86, −0.01], P = 0.043; ). The plasma fibrinogen levels were not significantly different between patients with HCC and patients with cirrhosis (WMD = −0.62, 95% CI, [−1.56, 0.33], P = 0.200; ).
Figure 2 Forest plot for plasma fibrinogen levels in (A) patients with HCC compared to that in healthy controls, (B) cirrhotic patients compared to healthy controls, and (C) patients with HCC compared to patients with cirrhosis.
Abbreviations: HCC, hepatocellular carcinoma; WMD, weighted mean difference.
Association between plasma fibrinogen and HCC prognosis
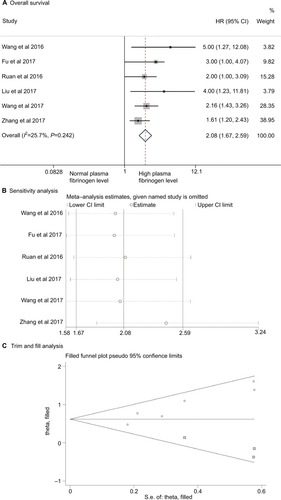
Correlation between elevated plasma fibrinogen and OS
Meta-analysis of the six OS-related studies showed little heterogeneity among studies (I2 = 25.7%, P = 0.242). A fixed effect model showed that patients with HCC and high pretreatment plasma fibrinogen levels had significantly poorer OS compared to those with normal fibrinogen levels (HR = 2.08, 95% CI = [1.67, 2.59], P < 0.0001; ). Sensitivity analysis showed that the pooled result was relatively stable (). Egger’s test (P = 0.008) showed the presence of publication bias. Further, trim and fill analysis showed that after adjusting for three studies, the recalculated pooled HR for OS was 1.85 (95% CI = [1.51, 2.27]; ), which was not significantly changed from the initial estimate (HR = 2.08, 95% CI = [1.67, 2.59]). Our data suggest that the presence of publication bias has no significant effect on the overall finding.
Figure 3 Association of elevated plasma fibrinogen level with overall survival in patients with hepatocellular carcinoma.
Notes: (A) Forest plot of HRs for overall survival. (B) Sensitivity analysis of overall survival. (C) Trim and fill analysis for the overall survival. The squares represent the adjusted studies.
We also performed TSA meta-analysis on the OS results. Although the number of participants had not reached the required information size, our TSA showed that the cumulative Z-curve crossed the trial sequential monitoring boundary for harm, confirming the poorer survival rate among patients with HCC and high levels of plasma fibrinogen. Our results suggest that currently available studies are sufficient to conclude the negative prognostic value of elevated plasma fibrinogen in patients with HCC ().
Figure 4 TSA of the association between elevated plasma fibrinogen levels and overall survival in patients with hepatocellular carcinoma.
Notes: The diversity-adjusted required information size of 784 patients was calculated on the basis of type I error of 5%, type II error of 20%, the control event proportion of 40%, and a relative risk reduction of 20% in outcomes. The cumulative Z-curve crossed the trial sequential monitoring boundary for harm, confirming the poorer survival rate in patients with hepatocellular carcinoma and high plasma fibrinogen.
Abbreviation: TSA, trial sequential analysis.
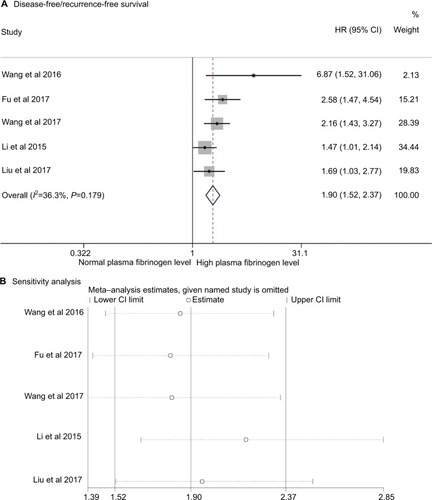
Correlation between elevated plasma fibrinogen and DFS/RFS
Meta-analysis of the 5 DFS-/RFS-related studies showed low heterogeneity among studies (I2 = 36.3%, P = 0.179). A fixed effect model showed that patients with HCC and high pretreatment plasma fibrinogen levels had significantly poorer outcomes compared to those with normal fibrinogen levels (HR = 1.90, 95% CI = [1.52, 2.37], P < 0.0001; ). Sensitivity analysis showed that the pooled result was relatively stable (). Egger’s test (P = 0.095) showed no publication bias.
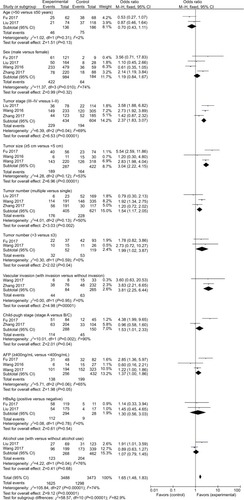
Association between plasma fibrinogen and clinicopathological parameters of HCC
Clinicopathological analyses showed that elevated plasma fibrinogen levels were significantly associated with advanced tumor stage (stage III–IV vs stage I–II, OR = 2.37, 95% CI = [1.83, 3.07], P < 0.00001), larger tumor size (≥5 vs <5 cm, OR = 3.04, 95% CI = [2.22, 4.15], P < 0.00001), increased tumor number (multiple vs single, OR = 1.54, 95% CI = [1.17, 2.05], P = 0.002; >3 vs ≤3 tumor nodules, OR = 1.99, 95% CI = [1.02, 3.87], P = 0.04), and vascular invasion (OR = 3.81, 95% CI = [2.25, 6.44], P < 0.00001). Plasma fibrinogen levels were significantly higher in patients with HCC and mild cirrhosis (Child A) compared to those with moderate or advanced cirrhosis (Child B/C) (Child A vs Child B/C, OR = 1.53, 95% CI = [1.01, 2.33], P = 0.04). Higher plasma fibrinogen was also marginally associated with increased serum AFP level (OR = 1.37, 95% CI = [1.00, 1.86], P = 0.05). No significant association was found when evaluating age, sex, hepatitis B surface antigen (HBsAg), and alcohol use. The correlations between plasma fibrinogen and the clinical features of HCC are depicted in and summarized in .
Table 4 Overall analysis of the association between elevated plasma fibrinogen levels and clinical features of patients with hepatocellular carcinoma
Figure 6 Association between elevated plasma fibrinogen levels and clinicopathological parameters including age (>50 vs ≤50 years), sex (male vs female), tumor stage (III–IV vs I–II), tumor size (≥5 vs <5 cm), tumor number (multiple vs single; >3 vs ≤3), vascular invasion (with vs without invasion), Child-Pugh stage (A vs B/C), serum AFP level (≥400 vs <400 ng/mL), HBsAg (positive vs negative), and alcohol use (with vs without alcohol use).
Abbreviations: AFP, alpha-fetoprotein; HBsAg, hepatitis B surface antigen.
Discussion
In this meta-analysis, we identified eight studiesCitation20–Citation23,Citation25,Citation29–Citation31 that examined the pretreatment plasma fibrinogen levels in HCC, cirrhotic, and/or healthy subjects. We observed that patients with cirrhosis had significantly lower plasma fibrinogen levels compared to healthy controls (WMD = −0.44, 95% CI = [−0.86, −0.01], P = 0.043). Fibrinogen is a product of hepatocytes. Therefore, patients with cirrhosis and compromised liver function may generally have less plasma fibrinogen levels than healthy counterparts.Citation25,Citation29 However, our WMD analyses showed that the pretreatment plasma fibrinogen levels in HCC cases were not significantly elevated when compared with that in healthy subjects (WMD = 0.50, 95% CI = [−0.82, 1.82], P = 0.457) or patients with cirrhosis (WMD = −0.62, 95% CI = [−1.56, 0.33], P = 0.200). Therefore, plasma fibrinogen level is not usable as a diagnostic marker for HCC detection.
On the other hand, our prognostic value analyses, which included eight studiesCitation18,Citation19,Citation24,Citation32–Citation36 with a total number of 1,961 patients with HCC, demonstrated that those patients with HCC and elevated fibrinogen levels are more likely to experience poorer OS (HR = 2.08, 95% CI = [1.67, 2.59], P < 0.0001) and recurrence (HR = 1.90, 95% CI = [1.52, 2.37], P < 0.0001). Furthermore, TSA indicated that currently available studies are sufficient to validate the negative prognostic value of elevated plasma fibrinogen levels in patients with HCC. Our clinicopathological analyses also indicated that patients with HCC and elevated plasma fibrinogen levels are likely to be associated with a higher pathological stage including advanced tumor stage, larger tumor size, increased tumor number, and the presence of vascular invasion, implicating that plasma fibrinogen level is closely related to tumor progression.
In addition to our analysis, recent studies also indicated a positive correlation between elevated plasma fibrinogen levels and poorer prognosis in other solid tumors including esophageal carcinoma,Citation37–Citation39 small cell lung carcinoma,Citation40 non-small cell lung carcinoma,Citation41 upper urinary tract urothelial carcinoma,Citation42,Citation43 epithelial ovarian cancer,Citation44 colorectal cancer,Citation45 renal cell carcinoma,Citation46,Citation47 and gastric cancer.Citation48,Citation49 There are several theories that may explain this association: 1) tumor progression is usually coupled with elevated inflammatory responses and leukocyte infiltration into tumor stroma. Infiltrated leukocytes may convert fibrinogen into fibrin matrix, which encapsulates the tumor cells and promotes tumor angiogenesis;Citation50 2) fibrinogen may serve as an extracellular matrix protein that regulates the growth of cancer cells by binding to growth factors (eg, vascular endothelial growth factor, fibroblast growth factor-2, platelet-derived growth factor) and promote cellular adhesion, proliferation, and metastasis; andCitation51–Citation53 3) fibrinogen promotes the adhesion of tumor cells to platelets, which leads to platelet aggregation and thrombin formation around tumor cells. The tumor-associated platelets and thrombin protect tumor cells against the attack of natural killer cells.Citation54 Moreover, in vitro studies also suggested that high levels of fibrinogen induced epithelial–mesenchymal transition, which is a hallmark for cancer invasion and metastasis.Citation14
As a plasma biomarker, fibrinogen has its advantages: blood sampling is a minimally invasive method that patients tolerate well, and it allows replicated sampling for long-term surveillance. Plasma fibrinogen levels can be determined easily by using routine coagulation parameters tested in the laboratory, which is rapid and cost-effective compared to other measurements, such as serum AFP level. Similar to serum AFP level, which has been identified as a significant prognostic marker in HCC, fibrinogen may also achieve similar accuracy for predicting clinical outcomes. In fact, Fu et alCitation33 found that subgroups with negative AFP levels or less aggressive clinicopathology but with elevated plasma fibrinogen levels still demonstrated poorer survival outcomes, suggesting that plasma fibrinogen could be a better prognostic biomarker compared to AFP, although further studies are warranted.
Most importantly, the examination of pretreatment plasma fibrinogen levels may help clinicians identify and provide more aggressive treatments to the appropriate group of patients to improve clinical outcomes. By comparing the normal- and high-fibrinogen groups, Zhang and LongCitation19 found that patients with HCC and elevated plasma fibrinogen levels had poorer responses to TACE, a recommended adjuvant therapy for intermediate and advanced HCC. The poor response to TACE treatment in high-fibrinogen groups requires further examination due to its small sample size, and it is not one of our primary outcomes due to the limited number of studies available.
Aside from the limited studies available, there are several other limitations in our analyses. The association between the elevated plasma fibrinogen levels and poor survival outcomes could potentially be overestimated because all included studies are published studies. Positive results are always favored for publication when compared to negative results; thus exaggerating the effect of the group tested. There are variations in the plasma fibrinogen measurement methods, the cutoff values, tumor stages, and treatments received among all included studies; however, analysis suggested little heterogeneity among studies. Moreover, all patients included in the prognostic evaluation were Asians, which may not reflect as general phenomena in other ethnic populations. All of these factors could have influenced the outcome of our evaluation.
Conclusion
From our analyses of eight high-quality studies, we conclude that patients with HCC and elevated plasma fibrinogen levels have poor survival outcomes. High plasma fibrinogen levels are associated with heavier tumor burden and advanced tumor progression. Therefore, plasma fibrinogen level may serve as a prognostic biomarker in HCC.
Acknowledgments
This work was supported by the Guangdong Provincial Science and Technology Projects (No. 2017A020211031 and No. 2016ZC0145), Guangzhou Medical University Science and Technology Project (No. 201624), China National Natural Science Fund Project (81673206), Key Scientific and Technological Program of Guangzhou City (201508020262), and Guangdong Provincial Medical Science Funding Project (No. A2015243).
Author contributions
GH, HJ, ZJ, and XZ conceived and designed the study. GH, HJ, and YL searched the database and checked them according to the eligible criteria and exclusion criteria. YW and WC analyzed the data. BS and YL designed the methodology. ZJ and XZ supervised the planning and execution of the research activity. GH and HJ wrote the paper. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- MazzantiRArenaUTassiRHepatocellular carcinoma: where are we?World J Exp Med201661213626929917
- CicaleseLHepatocellular Carcinoma Available from: https://emedicine.medscape.com/article/197319-overviewAccessed January 24, 2018
- BoschFXRibesJDíazMClériesRPrimary liver cancer: worldwide incidence and trendsGastroenterology20041275 Suppl 1S5S1615508102
- ZhangDYFriedmanSLFibrosis-dependent mechanisms of hepatocarcinogenesisHepatology201256276977522378017
- DonatoFTaggerAGelattiUAlcohol and hepatocellular carcinoma: the effect of lifetime intake and hepatitis virus infections in men and womenAm J Epidemiol2002155432333111836196
- Huitzil-MelendezFDCapanuMO’ReillyEMAdvanced hepatocellular carcinoma: which staging systems best predict prognosis?J Clin Oncol201028172889289520458042
- MazzaferroVRegaliaEDociRLiver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosisN Engl J Med1996334116937008594428
- de SioICastellanoLCalandraMdel Vecchio-BlancoCSubcutaneous needle-tract seeding after fine needle aspiration biopsy of pancreatic liver metastasisEur J Ultrasound2002151–2656812044855
- ChauhanRLahiriNTissue-LNTissue- and serum-associated biomarkers of hepatocellular carcinomaBiomark Cancer20168Suppl 1375527398029
- WangCSLinCLLeeHCUsefulness of serum des-gamma-carboxy prothrombin in detection of hepatocellular carcinomaWorld J Gastroenterol200511396115611916273636
- MosessonMWFibrinogen and fibrin structure and functionsJ Thromb Haemost2005381894190416102057
- TennentGABrennanSOStangouAJO’GradyJHawkinsPNPepysMBHuman plasma fibrinogen is synthesized in the liverBlood200710951971197417082318
- WenJYangYYeFThe preoperative plasma fibrinogen level is an independent prognostic factor for overall survival of breast cancer patients who underwent surgical treatmentBreast201524674575026482138
- ShuYJWengHBaoRFClinical and prognostic significance of preoperative plasma hyperfibrinogenemia in gallbladder cancer patients following surgical resection: a retrospective and in vitro studyBMC Cancer20141456625096189
- LeeSELeeJHRyuKWPreoperative plasma fibrinogen level is a useful predictor of adjacent organ involvement in patients with advanced gastric cancerJ Gastric Cancer2012122818722792520
- YamashitaHKitayamaJTaguriMNagawaHEffect of preoperative hyperfibrinogenemia on recurrence of colorectal cancer without a systemic inflammatory responseWorld J Surg20093361298130519347392
- JiangHGLiJShiSBValue of fibrinogen and D-dimer in predicting recurrence and metastasis after radical surgery for non-small cell lung cancerMed Oncol20143172224861920
- KinoshitaAOnodaHImaiNElevated plasma fibrinogen levels are associated with a poor prognosis in patients with hepatocellular carcinomaOncology201385526927724217119
- ZhangXLongQElevated serum plasma fibrinogen is associated with advanced tumor stage and poor survival in hepatocellular carcinoma patientsMedicine20179617e669428445272
- CasarilMCapraFMarchioriLSerum copper and ceruloplasmin in early and in advanced hepatocellular carcinoma: diagnostic and prognostic relevanceTumori19897554985022557694
- DoğanUBCindorukMDumluSUnlüRUnalSDiagnostic value of serum copper, zinc and plasma fibrinogen in cirrhotic patients with and without hepatocellular carcinomaItal J Gastroenterol Hepatol19972954764779494860
- ZhuWLFanBLLiuDLZhuWXAbnormal expression of fibrinogen gamma (FGG) and plasma level of fibrinogen in patients with hepatocellular carcinomaAnticancer Res20092972531253419596924
- BasiliSAndreozziPVieriMLipoprotein (a) serum levels in patients with hepatocarcinomaClin Chim Acta19972621–253609204209
- LiuZGuoHGaoFFibrinogen and D-dimer levels elevate in advanced hepatocellular carcinoma: High pretreatment fibrinogen levels predict poor outcomesHepatol Res201747111108111727914119
- HessienMAyadMIbrahimWMUlarabBIMonitoring coagulation proteins during progression of liver diseaseIndian J Clin Biochem201530221021625883431
- HigginsJPThompsonSGDeeksJJAltmanDGMeasuring inconsistency in meta-analysesBMJ2003327741455756012958120
- MantelNHaenszelWStatistical aspects of the analysis of data from retrospective studies of diseaseJ Natl Cancer Inst195922471974813655060
- DersimonianRLairdNMeta-analysis in clinical trialsControl Clin Trials1986731771883802833
- AlkimHAyazSSasmazNOguzPSahinBHemostatic abnormalities in cirrhosis and tumor-related portal vein thrombosisClin Appl Thromb Hemost201218440941522166587
- Al GhumlasAKAbdel GaderAGAl FalehFZHaemostatic abnormalities in liver disease: could some haemostatic tests be useful as liver function tests?Blood Coagul Fibrinolysis200516532933515970716
- van der WaltJAGompertsEDKewMCHemostatic factors in primary hepatocellular cancerCancer197740415931603198099
- WangGYJiangNYiHMPretransplant level is a novel prognostic predictor for hepatocellular carcinoma recurrence and patient survival following liver transplantationAnn Transplant20162112513026903139
- FuSJJiFHanMPrognostic value of combined preoperative fibrinogen and neutrophil-lymphocyte ratio in patients with hepatocellular carcinoma after liver transplantationOncotarget2017834301431227935864
- WangXPMaoMJHeZLA retrospective discussion of the prognostic value of combining prothrombin time(PT) and fibrinogen(Fbg) in patients with hepatocellular carcinomaJ Cancer20178112079208728819409
- RuanDYLinZXWangTTNomogram for preoperative estimation of long-term survival of patients who underwent curative resection with hepatocellular carcinoma beyond Barcelona clinic liver cancer stage A1Oncotarget2016738613786138927542216
- LiYRuanDYYiHMWangGYYangYJiangNA three-factor preoperative scoring model predicts risk of recurrence after liver resection or transplantation in hepatocellular carcinoma patients with preserved liver functionHepatobiliary Pancreat Dis Int201514547748426459723
- LiuFTGaoHWuCWZhuZMThe association of plasma fibrinogen with clinicopathological features and prognosis in esophageal cancer patientsOncotarget2017854930299303829190975
- LvGYYuYAnLSunXDSunDWPreoperative plasma fibrinogen is associated with poor prognosis in esophageal carcinoma: a meta-analysisClin Transl Oncol201820785386129134563
- MatsudaSTakeuchiHKawakuboHPrognostic impact of change in the fibrinogen and albumin score during preoperative treatment in esophageal cancer patientsWorld J Surg201741112788279528608015
- FanSGuanYZhaoGAnGAssociation between plasma fibrinogen and survival in patients with small-cell lung carcinomaThorac Cancer20189114615129131503
- ChenPWangCChengBPlasma fibrinogen and serum albumin levels (FA score) act as a promising prognostic indicator in non-small cell lung cancerOnco Targets Ther2017103107311828790844
- CuiJYuMZhangNPrognostic scores based on the preoperative plasma fibrinogen and serum albumin level as a prognostic factor in patients with upper urinary tract urothelial carcinomaOncotarget2017840689646897328978171
- ZhangBSongYJinJPreoperative plasma fibrinogen level represents an independent prognostic factor in a Chinese cohort of patients with upper tract urothelial carcinomaPLoS One2016113e015019326930207
- LuoYKimHSKimMLeeMSongYSElevated plasma fibrinogen levels and prognosis of epithelial ovarian cancer: a cohort study and meta-analysisJ Gynecol Oncol2017283e3628382799
- HongTShenDChenXWuXHuaDPreoperative plasma fibrinogen, but not D-dimer might represent a prognostic factor in non-metastatic colorectal cancer: a prospective cohort studyCancer Biomark201719110311128269756
- TianYHongMJingSClinical and prognostic effect of plasma fibrinogen in renal cell carcinoma: a meta-analysisBiomed Res Int201720179591506828154828
- PengDHeZSLiXSA novel predictor of survival with renal cell carcinoma after nephrectomyJ Endourol201731439740428121179
- YuXHuFYaoQLiCZhangHXueYSerum fibrinogen levels are positively correlated with advanced tumor stage and poor survival in patients with gastric cancer undergoing gastrectomy: a large cohort retrospective studyBMC Cancer20161648027418164
- YuWWangYShenBAn elevated preoperative plasma fibrinogen level is associated with poor overall survival in Chinese gastric cancer patientsCancer Epidemiol201642394527010728
- DvorakHFHarveyVSEstrellaPBrownLFMcdonaghJDvorakAMFibrin containing gels induce angiogenesis. Implications for tumor stroma generation and wound healingLab Invest19875766736862447383
- SahniASimpson-HaidarisPJSahniSKVadayGGFrancisCWFibrinogen synthesized by cancer cells augments the proliferative effect of fibroblast growth factor-2 (FGF-2)J Thromb Haemost20086117618317949478
- SahniAFrancisCWVascular endothelial growth factor binds to fibrinogen and fibrin and stimulates endothelial cell proliferationBlood200096123772377811090059
- WitschESelaMYardenYRoles for growth factors in cancer progressionPhysiology20102528510120430953
- ZhengSShenJJiaoYPlatelets and fibrinogen facilitate each other in protecting tumor cells from natural killer cytotoxicityCancer Sci2009100585986519302289
- MoherDLiberatiATetzlaffJAltmanDGThe PRISMA GroupPreferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA StatementPLoS Med200967e100009719621072