Abstract
Background
The association between metabolic syndrome (MS) and bladder cancer (BC) was not fully investigated, and most primary studies and pooled analyses were only focused on certain specific components.
Objective
To further investigate this issue and obtain more precise findings, we conducted this updated evidence synthesis of published studies, which involved not only MS components but also the MS in its entirety.
Materials and methods
We searched the PubMed, EMBASE, and Web of Science databases for observational studies on the association between BC susceptibility and/or mortality, and MS and its components. We extracted data from included studies, evaluated heterogeneity, and performed meta-analytic quantitative syntheses.
Results
A total of 95 studies with 97,795,299 subjects were included in the present study. According to the results, MS significantly increased the risk of BC (risk ratio [RR]=1.11, 95% CI=1.00–1.23); diabetes significantly increased the risk of BC (RR=1.29, 95% CI=1.19–1.39) and associated with poor survival (RR=1.24, 95% CI=1.08–1.43). Excessive body weight was associated with increased susceptibility (RR=1.07, 95% CI=1.02–1.12), recurrence (RR=1.46, 95% CI=1.18–1.81), and mortality (RR=1.17, 95% CI=1.00–1.37). As indicated by cumulative meta-analysis, sample size was inadequate for the association between BC susceptibility and MS, the association between BC recurrence and excessive body weight, and the association between BC survival and diabetes. The sample size of the meta-analysis was enough to reach a stable pooled effect for other associations.
Conclusion
Diabetes and excessive body weight as components of MS are associated with increased susceptibility and poor prognosis of BC. Uncertainty remains concerning the impact of overall MS, hypertension, and dyslipidemia on BC susceptibility and prognosis, for which further investigations are needed.
Introduction
Metabolic syndrome (MS) is defined by a collection of biochemical and physiologic abnormalities associated with the development of cardiovascular disease (CVD) and type 2 diabetes. Abdominal obesity, atherogenic dyslipidemia, high blood pressure, and insulin resistance are major components of MS.Citation1 According to the US National Health and Nutrition Examination Survey data, the overall MS prevalence among adults was 21.8% during 1988–1994, and it had increased up to 34.7% by the end of 2012. The prevalence of MS also increases with age, from 18.3% among those aged 20–39 years to 46.7% among those aged 60 years or more. Almost half of the US population will be diagnosed of MS throughout their life as the population-aging continues.Citation2,Citation3 The MS was previously identified as a strong contributor to cardiovascular morbidity and mortality; in addition, it has also been recognized as a potential etiologic factor for the development and progression of multiple types of cancers.Citation4 Bladder cancer (BC) is the most common malignancy that affects the urinary tract. Evidence from epidemiologic investigations, clinical studies, and pooled analyses suggests that the MS may increase the risk, recurrence, and mortality of BC. However, most primary studies and pooled analyses only focused on certain specific MS components, such as diabetes and excessive body weight, but not the overall MS; as a result, the impact of MS on the carcinogenesis and prognosis of BC patients remains unclear. On the other hand, the stability of pooled effects (robustness to inclusion of additional studies), which could be investigated using cumulative meta-analysis, was left unexamined in previous meta-analysis. Therefore, in order to further investigate this issue and obtain more precise findings, an updated summarization of published studies, which integrates pooled analysis and stability examination and involves not only MS components but also the MS in its entirety, needs to be performed. To this end, we conducted the present comprehensive evidence synthesis incorporating pooled analysis and cumulative meta-analysis, to summarize all published studies to date, concerning the association between MS, its components, and BC in terms of susceptibility and prognosis.
Materials and methods
Literature search strategy
To identify observational studies on the association between BC risk and prognosis, we searched literature databases including the PubMed, EMBASE, and Web of Science. All possible combinations of the following search terms were used for the search: “bladder cancer”, “urothelial carcinoma”, “metabolic syndrome”, “diabetes”, “overweight”, “obesity”, “hypertension”, “dyslipidemia”, “risk”, “susceptibility”, “survival”, “recurrence”, and “prognosis”. The time limit for the search was between the establishment of the database and 31 March 2018. No language limits were applied to the search. The references of previous meta-analyses on similar topics were also screened for potential relevant studies.
Study selection and data extraction
Eligible studies were selected according to the predefined selection criteria. Included studies should be observational studies and provided data on the association between BC susceptibility and/or survival, and MS or any of its known components. Two authors independently reviewed the literature search results and selected studies for inclusion. Any discrepancies were resolved by discussion with a third author.
The following data were extracted from the included studies: surname of the first author, year of publication, country of origin, research design, sample size, exposures examined (MS and/or its components), outcomes analyzed (susceptibility and/or prognosis), and data of effect sizes measuring the association between exposures and outcomes. Two authors independently conducted data extraction, and any discrepancies were resolved by discussion or consulting with a third author.
Statistical analysis
Quantitative evidence syntheses using a fixed effects or random effects meta-analytic model were performed. When significant heterogeneity among studies was detected, a fixed effects model was used, otherwise a random effects model was used. Leave-one-out sensitivity analysis was performed to identify influential studies for a given meta-analysis. Subgroup analysis by gender was performed concerning the association between MS and BC susceptibility, and subgroup analysis by degree of excessive body weight (overweight vs obesity) was performed for the association between excessive body weight and BC risk, recurrence, and mortality. Z-test was performed to examine if the difference between pooled effects across subgroups was significant. Cumulative meta-analyses by chronologic order were performed to examine if a stable pooled effect was reached in meta-analysis. Publication bias was investigated by funnel graphs and Egger’s test, and trim-and-fill analysis was performed when significant publication bias was detected.
Results
Basic characteristics of included studies
The primary literature search identified 884 publications. After comprehensive screening according to the selection criteria, a total of 95 studies were included in the present evidence synthesis. Among the included studies, 74 were cohort studies, 16 were case–control studies, and five were cross-sectional studies. The basic characteristics of the included studies are shown in Table S1.
Association between MS and BC susceptibility and prognosis
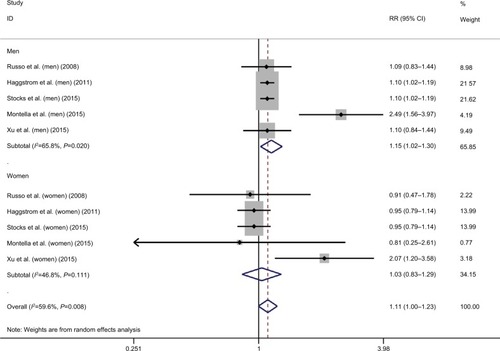
As to the correlation between overall MS and susceptibility of BC, a total of five studies were included, among which significant heterogeneity was detected (I2=59.6, P=0.008).Citation5–Citation9 Based on the results of pooled analysis, MS significantly increased the risk of BC (risk ratio [RR]=1.11, 95% CI=1.00–1.23; ). Sensitivity analysis showed that the study by Montella et al was influential and was a potential source of observed heterogeneity.Citation8 According to the subgroup analysis by gender, MS significantly increased the incidence of BC in males (RR=1.15, 95% CI=1.02–1.30; ), but not in females (RR=1.03, 95% CI=0.83–1.29; ). However, the observed subgroup difference was not statistically significant (Z=0.88, P=0.38).
Figure 1 Meta-analysis on the association between bladder cancer susceptibility and metabolic syndrome.
Abbreviation: RR, risk ratio.
Only one study that investigated the association between MS and BC mortality was found, in which a strong positive correlation between MS and BC mortality was reported (RR=4.03, 95% CI=2.03–8.01).Citation10
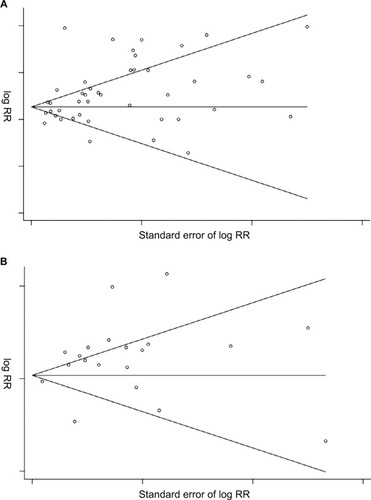
According to the results of cumulative meta-analysis by year of publication, stable pooled effects were not yet reached in both overall meta-analysis and subgroup analysis by gender, regarding the association between MS and BC susceptibility (Figure S1).
Association between diabetes and BC susceptibility and prognosis
In terms of the correlation between diabetes and risk of BC, a total of 41 studies were included, among which significant heterogeneity was detected (I2=89.8%; P<0.001).Citation11–Citation51 Based on the results of pooled analysis, diabetes significantly increased the risk of BC (RR=1.29, 95% CI=1.19–1.39; ). Sensitivity analysis revealed that the study by Lee et al was influential, which was a potential source of observed heterogeneity.Citation39
Figure 2 Meta-analysis on the association between bladder cancer susceptibility (A), mortality (B), and diabetes.
Abbreviation: RR, risk ratio.
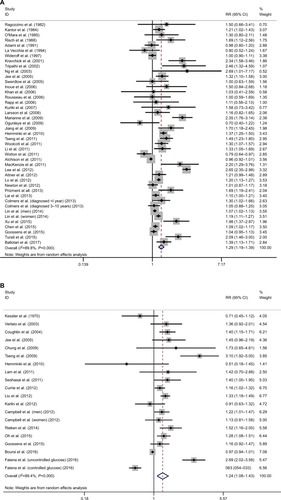
In terms of the correlation between diabetes and mortality of BC patients, a total of 18 studies were included.Citation21,Citation32,Citation49,Citation52–Citation67 Significant heterogeneity was detected (I2=89.4%; P<0.001). The results of pooled analysis showed that diabetes was significantly associated with poor survival in BC patients (RR=1.24, 95% CI=1.08–1.43; ). Sensitivity analysis revealed that the studies by Faiena et alCitation66 and Tseng et alCitation55 were influential, as potential sources of observed heterogeneity.
According to the results of cumulative meta-analysis by year of publication, a stable pooled effect was reached in meta-analysis regarding the association between diabetes and BC susceptibility (Figure S2A), but not the association between diabetes and BC mortality (Figure S2B).
Association between excessive body weight and BC susceptibility and prognosis
In terms of the association between excessive body weight and risk of BC, a total of 18 studies were included in the overall meta-analysis of both overweight and obesity, among which significant heterogeneity was detected (s=64.6, P<0.001).Citation6,Citation19,Citation28,Citation68–Citation82 Excessive body weight was significantly associated with increased risk of BC (RR=1.07, 95% CI=1.02–1.12; ). Sensitivity analysis revealed that the studies by Samanic et alCitation72, Koebnick et alCitation77, and Häggström et alCitation6 were influential and were potential sources of observed heterogeneity. The overall meta-analysis investigating the association between excessive body weight and BC recurrence indicated increased risk of recurrence in BC patients with excessive body weight (RR=1.46, 95% CI=1.18–1.81; ). Significant heterogeneity was detected (I2=85.5, P<0.001) among the included 11 studies.Citation83–Citation93 Sensitivity analysis revealed that the study by Kluth et al was influential, a potential source of observed heterogeneity.Citation90 The overall meta-analysis investigating association between excessive body weight and BC survival indicated unfavorable survival of BC patients with excessive body weight (RR=1.17, 95% CI=1.00–1.37; ). Significant heterogeneity was detected (I2=88.2, P<0.001) among the included six studies.Citation87,Citation90,Citation92,Citation94–Citation96 Sensitivity analysis revealed that the studies by Chromecki et al and Dabi et al were influential and were potential sources of observed heterogeneity.Citation87,Citation92
Figure 3 Meta-analysis on the association between bladder cancer susceptibility (A), recurrence (B), mortality (C), and excessive body weight.
Abbreviation: RR, risk ratio.
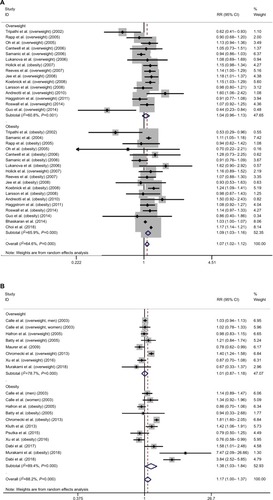
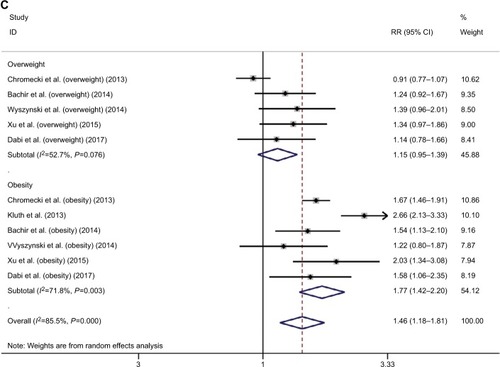
According to subgroup analysis by the degree of excessive body weight, overweight did not have a significant impact on the susceptibility of BC (RR=1.04, 95% CI=0.96–1.13), but obesity was significantly associated with increased risk of BC (RR=1.09, 95% CI=1.03–1.16). Similar results were revealed in subgroup analysis for prognosis. Overweight did not have a significant impact on recurrence and mortality of BC (recurrence: RR=1.15, 95% CI=0.95–1.39; mortality: RR=1.01, 95% CI=0.87–1.18), but obesity was associated with an increased recurrence risk and poor survival in BC patients (recurrence: RR=1.46, 95% CI=1.18–1.81; mortality: RR=1.38, 95% CI=1.03–1.84). However, the observed subgroup differences were all statistically nonsignificant (susceptibility: Z=0.93, P=0.35; recurrence: Z=1.64, P=0.10; mortality: Z=1.88, P=0.06). Significant heterogeneity was detected in each subgroup analysis ().
According to the results of cumulative analysis by chronologic order, a stable pooled effect was reached in meta-analysis regarding the association between excessive body weight and BC susceptibility (Figure S3A) and subgroup analysis by severity (Figure S3B). In contrast, instability was detected for recurrence (Figure S3C, D). An almost stable pooled effect was reached in meta-analysis for mortality (Figure S3E, F).
Association between hypertension, dyslipidemia, and BC susceptibility and prognosis
A quantitative evidence synthesis regarding the association between hypertension and BC risk or mortality cannot be performed due to limited number of relevant studies. Stocks’ study revealed that every 10 mmHg blood pressure increment brought significant increase in BC susceptibility and mortality in males (susceptibility: RR=1.12, 95% CI=1.04–1.21; mortality: RR=1.26, 95% CI=1.05–1.51); in contrast, similar effects were not observed among females (susceptibility: RR=0.95, 95% CI=0.81–1.11; mortality: RR=1.14, 95% CI=0.82–1.59).Citation97 Batty’s study reported no significant association between increased systolic or diastolic blood pressure BC (high systolic blood pressure: RR=1.06, 95% CI=0.96–1.18; high diastolic blood pressure: RR=1.08, 95% CI=0.92–1.27).Citation98 In Tai’s study, investigators reported a nonsignificant association between hypertension and BC recurrence (HR=1.3, 95% CI=0.88–1.93).Citation99
Concerning the association between dyslipidemia and BC, only two studies were identified in our literature search, in which inconsistent findings were reported. A retrospective study with 2,070 Chinese participants revealed a non-significant correlation between hypertriglyceridemia and BC susceptibility (adjusted OR=1.3, 95% CI=0.88–1.93).Citation9 However, another study by Stocks et al reported a significant association between hypertriglyceridemia and both BC susceptibility (HR=1.18, 95% CI=1.06–1.32) and mortality (HR=1.72, 95% CI=1.39–2.12).Citation7
Publication bias
No significant publication bias was detected except for the meta-analyses regarding the association between diabetes and BC susceptibility (P=0.015; ) and mortality (P=0.036; ). The trim-and-fill adjusted pooled RR and 95% CI was 1.28 (1.19–1.38) and 1.11 (0.97–1.28), respectively.
Discussion
The prevalence of MS continues to increase worldwide. According to the US National Cholesterol Education Program’s Adult Treatment Panel III report, MS has been identified as a multiplex risk factor for CVD that deserves more clinical attention.Citation1 On the other hand, we should also spare attention on the probable association between MS and BC, which is a common and costly malignancy.Citation100 In this comprehensive evidence synthesis of 95 studies involving 97,795,299 participants, we confirmed that MS and its components did confer contributing effects on the development and mortality of BC. In a Northern Italy prospective cohort of 407,157 subjects in the Reggio Emilia diabetes registry project, diabetes was associated with increases in the incidence of all cancers, including BC.Citation101 Our pooled analysis also reported a positive association between diabetes and BC. Our findings indicated that diabetes was the strongest single risk factor among the components of MS, which significantly increased the risk of BC and overall mortality. Our findings were similar to those reported in Fang et al’s meta-analysis and identified a stronger association compared with Xu et al’s meta-analysis.Citation102,Citation103 The underlying mechanisms between this association have been proposed. First, insulin may play a role as growth factor by exerting mitosis-promoting effects. Insulin binds and activates the insulin-like growth factor-1 (IGF-1) receptor and triggers the downstream pathways having potent mitogenic and transforming activity.Citation104 Increased insulin and IGF-1 in patients with MS may contribute to cancer progression and facilitate the growth of tumors by binding to the overexpressed insulin receptor in many cancers.Citation105 In addition, an association between insulin resistance and aberrant level of proinflammatory cytokine tumor necrosis factor a, which may induce development and progression of many tumors, has been reported.Citation106,Citation107 This could explain the increased cancer risk in adults with type 2 diabetes.Citation108,Citation109 Second, diabetes was associated with mitochondrial malfunction, which will lead to insufficient DNA repair. Moreover, mitochondria malfunction will increase the production of ROS, raising oxidative stress.Citation110 Third, diabetes, especially under conditions of poor metabolic control, causes a permanent proinflammatory state. This will consume intracellular antioxidant capacity, predisposing susceptible cells to carcinogenesis and cancer progression.Citation111 This could explain why uncontrolled diabetes was significantly associated with higher overall mortality, as reported in both Tai and Faiena’s studies.Citation66,Citation99 On the other hand, it has been suggested that antidiabetic drugs, such as metformin, may influence cancer risk among diabetic patients.Citation108
Obesity has been previously reported to be associated with a higher incidence and mortality of cancer.Citation112,Citation113 In the present meta-analysis, we observed a positive correlation between obesity and BC risk, BC survival, and recurrence; in contrast, overweight was not significantly associated with BC risk, BC survival, or recurrence. Overall, it seems that there was a positive correlation between body weight and BC risk, jBC survival or recurrence, with a possible dose–response effect. Similar to our findings, previous meta-analyses had revealed that each 1 kg/m2 increase in body mass index (BMI) was related to a 1.3% increase in risk of BC recurrence and each 5 kg/m2 increase in BMI was related to a 4.2% increase in BC incidence.Citation114,Citation115 A meta-analysis by Qin et al also confirmed that obesity was associated with an increased risk for BC, which was consistent with our results.Citation116 However, a meta-analysis by Lin et al reported that obesity was not significantly associated with BC overall survival, which was partially different from our observations.Citation115 The mechanism for the potential effects of excessive body weight on the BC risk and outcome has not been fully clarified. A frequently proposed hypothesis is that excessive body weight may cause metabolic and hormone changes, including hyperinsulinemia, leptin level elevation, and adiponectin reduction, which may promote carcinogenesis and progression of certain cancers.Citation117,Citation118 Moreover, obesity is generally accompanied by unrestrained diet and physical inactivity, and previous studies have proved that excessive calorie intake and physical inactivity may influence cancer development and progression.Citation113
Unlike obesity and diabetes, the role of hypertension and hyperlipidemia in BC development and progression has not been well investigated. Existing studies concerning hypertension and BC have not reached an unified conclusion. In Stocks et al’s study, blood pressure increment was significantly associated with BC incidence and mortality in men, whereas other studies did not find a significant association between hypertension and BC. Interestingly, even Stocks et al did not find the same correlation in women.Citation97–Citation99 A link between hypertension and cancer may be mediated via proliferative abnormalities in vascular smooth muscle cells. However, it needs more proof to clarify the correlation between hypertension and BC, and the underlying mechanism as well.Citation119 A case–control study in China revealed that hypertriglyceridemia was significantly associated with BC risk, while there was no positive correlation between low high-density lipoprotein-cholesterol and BC risk.Citation120 The association between hypertriglyceridemia and BC also needs further investigations.
In our meta-analysis, we found overall that MS significantly increased the risk and mortality of BC, but this effect was only observed among male subjects. This finding is consistent with those of Esposito et al’s and Cantiello et al’s meta-analyses, which also indicated that MS was associated with higher risk of BC in men.Citation4,Citation121 However, Cantiello et al’s work reported a nonsignificant association between MS and BC prognosis, and this was different from our observation.Citation121
For the first time we investigated whether the sample size was large enough to support conclusions with confidence. We need additional samples (primary studies) for the association between BC susceptibility and MS, the association between BC recurrence and excessive body weight, and the association between BC survival and diabetes. The sample size was adequate to reach a stable pooled effect regarding other associations. To the best of our knowledge, the present study is the most recent evidence synthesis connecting BC and MS, which included nearly 100 studies with nearly 100,000,000 participants, examined the overall MS and individual components, evaluated both susceptibility and prognosis, and explored adequacy of sample size by cumulative meta-analysis; however, our work also has certain limitations. First, significant heterogeneity was detected for most of the pooled analysis. In addition to the effect by influential studies identified by sensitivity analysis, the variation in race, sample size, and study design could also be the potential sources of the observed heterogeneity. Second, the publication bias was detected for certain analyses, and we performed trim- and-fill adjustment as complementary information.
Conclusions
Certain components of MS, that is, diabetes and excessive body weight, are associated with increased susceptibility and poor prognosis of BC. Uncertainty remains concerning the impact of overall MS, hypertension, and dyslipidemia on BC susceptibility and prognosis, for which further investigations are needed.
Disclosure
The authors report no conflicts of interest in this work.
References
- GrundySMBrewerHBCleemanJIDefinition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association Conference on scientific issues related to definitionCirculation2004109343343814744958
- FordESGilesWHDietzWHPrevalence of the metabolic syndrome among us adults: findings from the third national health and nutrition examination survey20022873356359
- AguilarMBhuketTTorresSLiuBWongRJPrevalence of the metabolic syndrome in the United States, 2003–2012JAMA2015313191973197425988468
- EspositoKChiodiniPColaoALenziAGiuglianoDMetabolic syndrome and risk of cancer: a systematic review and meta-analysisDiabetes Care201235112402241123093685
- RussoAAutelitanoMBisantiLMetabolic syndrome and cancer riskEur J Cancer200844229329718055193
- HäggströmCStocksTRappKMetabolic syndrome and risk of bladder cancer: prospective cohort study in the metabolic syndrome and cancer project (Me-Can)Int J Cancer201112881890189820568111
- StocksTBjørgeTUlmerHMetabolic risk score and cancer risk: pooled analysis of seven cohortsInt J Epidemiol20154441353136325652574
- MontellaMdi MasoMCrispoAMetabolic syndrome and the risk of urothelial carcinoma of the bladder: a case-control studyBMC Cancer20151572026475132
- XuSZhangGMGuanFJThe association between metabolic syndrome and the risk of urothelial carcinoma of the bladder: a case-control study in ChinaWorld J Surg Oncol201513123626246367
- ShaNXuHChenTThe evaluation of the association between the metabolic syndrome and tumor grade and stage of bladder cancer in a Chinese populationOnco Targets Ther201691175117927022277
- RagozzinoMMeltonLJChuCPPalumboPJSubsequent cancer risk in the incidence cohort of Rochester, Minnesota, residents with diabetes mellitusJ Chronic Dis198235113197068798
- KantorAFHartgePHooverRNNarayanaASSullivanJWFraumeniJFUrinary tract infection and risk of bladder cancerAm J Epidemiol198411945105156711540
- O’MaraBAByersTSchoenfeldEDiabetes mellitus and cancer risk: a multisite case-control studyJ Chronic Dis19853854354413998058
- RischHABurchJDMillerABHillGBSteeleRHoweGRDietary factors and the incidence of cancer of the urinary bladderAm J Epidemiol19881276117911913369417
- AdamiHOMclaughlinJEkbomACancer risk in patients with diabetes mellitusCancer Causes Control1991253073141932543
- La VecchiaCNegriEFranceschiSD’AvanzoBBoylePA case-control study of diabetes mellitus and cancer riskBr J Cancer19947059509537947103
- WideroffLGridleyGMellemkjaerLCancer incidence in a population-based cohort of patients hospitalized with diabetes mellitus in DenmarkJ Natl Cancer Inst19978918136013659308706
- KravchickSGalRCytronSIncreased incidence of diabetes mellitus in the patients with transitional cell carcinoma of urinary bladderPathol Oncol Res200171565911349222
- TripathiAFolsomARAndersonKEIowa Women’s Health StudyRisk factors for urinary bladder carcinoma in postmenopausal women. The Iowa Women’s Health StudyCancer200295112316232312436437
- NgYHusainIWaterfallNDiabetes mellitus and bladder cancer--an epidemiological relationship?Pathol Oncol Res200391303112704444
- JeeSHOhrrHSullJWYunJEJiMSametJMFasting serum glucose level and cancer risk in Korean men and womenJAMA2005293219420215644546
- SwerdlowAJLaingSPQiaoZCancer incidence and mortality in patients with insulin-treated diabetes: a UK cohort studyBr J Cancer200592112070207515886700
- InoueMIwasakiMOtaniTSasazukiSNodaMTsuganeSDiabetes mellitus and the risk of cancer: results from a large-scale population-based cohort study in JapanArch Intern Med2006166171871187717000944
- KhanMMoriMFujinoYSite-specific cancer risk due to diabetes mellitus history: evidence from the Japan Collaborative Cohort (JACC) StudyAsian Pac J Cancer Prev20067225325916839219
- RousseauMCParentMEPollakMNSiemiatyckiJDiabetes mellitus and cancer risk in a population-based case-control study among men from Montreal, CanadaInt J Cancer200611882105210916284945
- RappKSchroederJKlenkJFasting blood glucose and cancer risk in a cohort of more than 140,000 adults in AustriaDiabetologia200649594595216557372
- KurikiKHiroseKTajimaKDiabetes and cancer risk for all and specific sites among Japanese men and womenEur J Cancer Prev2007161838917220709
- LarssonSCAnderssonSOJohanssonJEWolkADiabetes mellitus, body size and bladder cancer risk in a prospective study of Swedish menEur J Cancer200844172655266018707871
- Ulcickas YoodMOliveriaSACampbellUBKoroCEIncidence of cancer in a population-based cohort of patients with type 2Diabetes200931216
- OgunleyeAAOgstonSAMorrisADEvansJMA cohort study of the risk of cancer associated with type 2 diabetesBr J Cancer200910171199120119690547
- JiangXCastelaoJEGroshenSUrinary tract infections and reduced risk of bladder cancer in Los AngelesBr J Cancer2009100583483919174821
- HemminkiKLiXSundquistJSundquistKRisk of cancer following hospitalization for type 2 diabetesOncologist201015654855520479278
- TsengCHDiabetes and risk of bladder cancer: a study using the National Health Insurance database in TaiwanDiabetologia20115482009201521544514
- WoolcottCGMaskarinecGHaimanCAHendersonBEKolonelLNDiabetes and urothelial cancer risk: the Multiethnic Cohort studyCancer Epidemiol201135655155421470936
- LiCBalluzLSFordESOkoroCATsaiJZhaoGAssociation between diagnosed diabetes and self-reported cancer among U.S. adults: findings from the 2009 Behavioral Risk Factor Surveillance SystemDiabetes Care20113461365136821505205
- WottonCJYeatesDGGoldacreMJCancer in patients admitted to hospital with diabetes mellitus aged 30 years and over: record linkage studiesDiabetologia201154352753421116605
- AtchisonEAGridleyGCarreonJDLeitzmannMFMcglynnKARisk of cancer in a large cohort of U.S. veterans with diabetesInt J Cancer2011128363564320473855
- MackenzieTZensMSFerraraASchnedAKaragasMRDiabetes and risk of bladder cancer: evidence from a case-control study in New EnglandCancer201111771552155621425156
- LeeMYLinKDHsiaoPJShinSJThe association of diabetes mellitus with liver, colon, lung, and prostate cancer is independent of hypertension, hyperlipidemia, and gout in Taiwanese patientsMetabolism201261224224921820134
- AttnerBLandin-OlssonMLithmanTNoreenDOlssonHCancer among patients with diabetes, obesity and abnormal blood lipids: a population-based register study in SwedenCancer Causes Control201223576977722467266
- LoSFChangSNMuoCHModest increase in risk of specific types of cancer types in type 2 diabetes mellitus patientsInt J Cancer2013132118218822510866
- NewtonCCGapsturSMCampbellPTJacobsEJType 2 diabetes mellitus, insulin-use and risk of bladder cancer in a large cohort studyInt J Cancer201313292186219123024033
- PrizmentAEAndersonKEYuanJMFolsomARDiabetes and risk of bladder cancer among postmenopausal women in the Iowa Women’s Health StudyCancer Causes Control201324360360823296458
- LaiGYParkYHartgePHollenbeckARFreedmanNDThe association between self-reported diabetes and cancer incidence in the NIH-AARP Diet and Health StudyJ Clin Endocrinol Metab2013983E497E50223408570
- ColmersINMajumdarSRYasuiYBowkerSLMarraCAJohnsonJADetection bias and overestimation of bladder cancer risk in type 2 diabetes: a matched cohort studyDiabetes Care201336103070307523990517
- LinCCChiangJHLiCICancer risks among patients with type 2 diabetes: a 10-year follow-up study of a nationwide population-based cohort in TaiwanBMC Cancer20141438124884617
- XuHLFangHXuWHCancer incidence in patients with type 2 diabetes mellitus: a population-based cohort study in ShanghaiBMC Cancer20151585226541196
- ChenHFChenSWChangYHLiCYCyLRisk of malignant neoplasms of kidney and bladder in a cohort study of the diabetic population in Taiwan with age, sex, and geographic area stratificationsMedicine20159438e149426402804
- GoossensMEZeegersMPBazelierMTde BruinMLBuntinxFde VriesFRisk of bladder cancer in patients with diabetes: a retrospective cohort studyBMJ Open201556e7470
- TuratiFPoleselJdi MasoMDiabetes mellitus and the risk of bladder cancer: an Italian case–control studyBr J Cancer2015113112713025996204
- BallotariPVicentiniMManicardiVDiabetes and risk of cancer incidence: results from a population-based cohort study in northern ItalyBMC Cancer201717170329070034
- KesslerIICancer mortality among diabeticsJ Natl Cancer Inst197044367368611515436
- VerlatoGZoppiniGBonoraEMuggeoMMortality from site-specific malignancies in type 2 diabetic patients from VeronaDiabetes Care20032641047105112663571
- CoughlinSSCalleEETerasLRPetrelliJThunMJDiabetes mellitus as a predictor of cancer mortality in a large cohort of US adultsAm J Epidemiol2004159121160116715191933
- ChungHChenSLiMPOD-11.08: Diabetes and risk of death from cancer of the prostate, kidney, and urinary bladderUrology2009744S36S37
- TsengCHChongCKTsengCPChanTTAge-related risk of mortality from bladder cancer in diabetic patients: a 12-year follow-up of a national cohort in TaiwanAnn Med200941537137919191082
- LamEKBattyGDHuxleyRRAssociations of diabetes mellitus with site-specific cancer mortality in the Asia-Pacific regionAnn Oncol201122373073820705912
- Rao Kondapally SeshasaiSKaptogeSThompsonADiabetes mellitus, fasting glucose, and risk of cause-specific deathN Engl J Med2011364982984121366474
- CurrieCJPooleCDJenkins-JonesSGaleEAJohnsonJAMorganCLMortality after incident cancer in people with and without type 2 diabetes: impact of metformin on survivalDiabetes Care201235229930422266734
- LiuXJiJSundquistKSundquistJHemminkiKThe impact of type 2 diabetes mellitus on cancer-specific survival: a follow-up study in SwedenCancer201211851353136121800292
- KarlinNJDueckACCookCBCancer with diabetes: prevalence, metabolic control, and survival in an academic oncology practiceEndocr Pract201218689890522982797
- CampbellPTNewtonCCPatelAVJacobsEJGapsturSMDiabetes and cause-specific mortality in a prospective cohort of one million U.S. adultsDiabetes Care20123591835184422699290
- RiekenMXylinasEKluthLEffect of diabetes mellitus and metformin use on oncologic outcomes of patients treated with radical cystectomy for urothelial carcinomaUrol Oncol201432149.e714
- OhJJKangMYJoJKAssociation between diabetes mellitus and oncological outcomes in bladder cancer patients undergoing radical cystectomyInt J Urol201522121112111726290403
- BoursiBGiantonioBJLewisJDHaynesKMamtaniRYangYXSerum glucose and hemoglobin A1C levels at cancer diagnosis and disease outcomeEur J Cancer201659909827017290
- FaienaIDombrovskiyVYSultanRCSalmasiAHSingerEAWeissREEffect of uncontrolled diabetes on outcomes after cystectomy in patients with bladder cancer: a population-based studyClin Genitourin Cancer2016145e509e51426997576
- HwangECKimYJHwangISImpact of diabetes mellitus on recurrence and progression in patients with non-muscle invasive bladder carcinoma: a retrospective cohort studyInt J Urol2011181176977621914000
- SamanicCGridleyGChowWHLubinJHooverRNFraumeniJFObesity and cancer risk among white and black United States veteransCancer Causes Control2004151354414970733
- RappKSchroederJKlenkJObesity and incidence of cancer: a large cohort study of over 145,000 adults in AustriaBr J Cancer20059391062106716234822
- OhSWYoonYSShinSAEffects of excess weight on cancer incidences depending on cancer sites and histologic findings among men: Korea National Health Insurance Corporation StudyJ Clin Oncol200523214742475416034050
- CantwellMMLaceyJVSchairerCSchatzkinAMichaudDSReproductive factors, exogenous hormone use and bladder cancer risk in a prospective studyInt J Cancer2006119102398240116894568
- SamanicCChowWHGridleyGJarvholmBFraumeniJFRelation of body mass index to cancer risk in 362,552 Swedish menCancer Causes Control200617790190916841257
- LukanovaABjörOKaaksRBody mass index and cancer: results from the Northern Sweden Health and Disease CohortInt J Cancer2006118245846616049963
- HolickCNGiovannucciELStampferMJMichaudDSProspective study of body mass index, height, physical activity and incidence of bladder cancer in US men and womenInt J Cancer2007120114014617036323
- ReevesGKPirieKBeralVCancer incidence and mortality in relation to body mass index in the Million Women Study: cohort studyBMJ20073357630113417986716
- JeeSHYunJEParkEJBody mass index and cancer risk in Korean men and womenInt J Cancer200812381892189618651571
- KoebnickCMichaudDMooreSCBody mass index, physical activity, and bladder cancer in a large prospective studyCancer Epidemiol Biomarkers Prev20081751214122118483344
- AndreottiGHouLBeane FreemanLEBody mass index, agricultural pesticide use, and cancer incidence in the Agricultural Health Study cohortCancer Causes Control201021111759177520730623
- RoswallNFreislingHBueno-de-MesquitaHBAnthropometric measures and bladder cancer risk: a prospective study in the EPIC cohortInt J Cancer2014135122918292924771290
- GuoLLiNWangGBody mass index and cancer incidence: a prospective cohort study in northern ChinaZhonghua Liu Xing Bing Xue Za Zhi201435323123624831616
- BhaskaranKDouglasIForbesHdos-Santos-SilvaILeonDASmeethLBody-mass index and risk of 22 specific cancers: a population-based cohort study of 5.24 million UK adultsLancet2014384994575576525129328
- ChoiJBLeeEJHanKDHongSHHaUSEstimating the impact of body mass index on bladder cancer risk: stratification by smoking statusSci Rep20188194729343838
- CalleEERodriguezCWalker-ThurmondKThunMJOverweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adultsN Engl J Med2003348171625163812711737
- HafronJMitraNDalbagniGBochnerBHerrHDonatSMDoes body mass index affect survival of patients undergoing radical or partial cystectomy for bladder cancer?J Urol200517351513151715821470
- BattyGDShipleyMJJarrettRJBreezeEMarmotMGSmithGDObesity and overweight in relation to organ-specific cancer mortality in London (UK): findings from the original Whitehall studyInt J Obes2005291012671274
- MaurerTMaurerJRetzMInfluence of body mass index on operability, morbidity and disease outcome following radical cystectomyUrol Int200982443243919506411
- ChromeckiTFChaEKFajkovicHObesity is associated with worse oncological outcomes in patients treated with radical cystectomyBJU Int2013111224925522727036
- XuXZhouLMiaoRAssociation of cancer mortality with postdiagnosis overweight and obesity using body mass indexOncotarget2016745023502926657291
- MurakamiYMatsumotoKIkedaMImpact of body mass index on the oncological outcomes of patients with upper and lower urinary tract cancers treated with radical surgery: a multi-institutional retrospective studyAsia Pac J Clin Oncol2018144310317
- KluthLAXylinasECrivelliJJObesity is associated with worse outcomes in patients with T1 high grade urothelial carcinoma of the bladderJ Urol2013190248048623376707
- PsutkaSPBoorjianSAMoynaghMRMortality after radical cystectomy: impact of obesity versus adiposity after adjusting for skeletal muscle wastingJ Urol201519351507151325464002
- DabiYRouscoffYAnractJImpact of body mass index on the oncological outcomes of patients treated with radical cystectomy for muscle-invasive bladder cancerWorld J Urol201735222923527272203
- DabiYEl MriniMDuquesnesIImpact of body mass index on the oncological outcomes of patients treated with radical nephroureterectomy for upper tract urothelial carcinomaWorld J Urol2018361657129032451
- BachirBGAprikianAGIzawaJIEffect of body mass index on the outcomes of patients with upper and lower urinary tract cancers treated by radical surgery: results from a Canadian multicenter collaborationUrol Oncol201432444144824412632
- WyszynskiATanyosSAReesJRBody mass and smoking are modifiable risk factors for recurrent bladder cancerCancer2014120340841424122218
- XuTZhuZWangXImpact of body mass on recurrence and progression in Chinese patients with Ta, T1 urothelial bladder cancerInt Urol Nephrol20154771135114126009259
- StocksTvan HemelrijckMManjerJBlood pressure and risk of cancer incidence and mortality in the Metabolic Syndrome and Cancer ProjectHypertension201259480281022353615
- BattyGDShipleyMJMarmotMGDavey SmithGDaveySGWhite-hall StudyBlood pressure and site-specific cancer mortality: evidence from the original Whitehall studyBr J Cancer20038971243124714520454
- TaiYSChenCHHuangCYDiabetes mellitus with poor glycemic control increases bladder cancer recurrence risk in patients with upper urinary tract urothelial carcinomaDiabetes Metab Res Rev201531330731425363092
- BottemanMFPashosCLRedaelliALaskinBHauserRThe health economics of bladder cancer: a comprehensive review of the published literaturePharmacoeconomics200321181315133014750899
- BallotariPVicentiniMManicardiVDiabetes and risk of cancer incidence: results from a population-based cohort study in northern ItalyBMC Cancer201717170329070034
- FangHYaoBYanYDiabetes mellitus increases the risk of bladder cancer: an updated meta-analysis of observational studiesDiabetes Technol Ther2013151191492224180357
- XuYHuoRChenXYuXDiabetes mellitus and the risk of bladder cancer: a PRISMA-compliant meta-analysis of cohort studiesMedicine20179646e858829145273
- KaaksRLukanovaAEnergy balance and cancer: the role of insulin and insulin-like growth factor-IProc Nutr Soc20016019110611310428
- FrascaFPandiniGScaliaPInsulin receptor isoform A, a newly recognized, high-affinity insulin-like growth factor II receptor in fetal and cancer cellsMol Cell Biol19991953278328810207053
- KernPARanganathanSLiCWoodLRanganathanGAdipose tissue tumor necrosis factor and interleukin-6 expression in human obesity and insulin resistanceAm J Physiol Endocrinol Metab20012805E745E75111287357
- SzlosarekPCharlesKABalkwillFRTumour necrosis factor-alpha as a tumour promoterEur J Cancer200642674575016517151
- VigneriPFrascaFSciaccaLPandiniGVigneriRDiabetes and cancerEndocr Relat Cancer20091641103112319620249
- VigneriRDiabetes: diabetes therapy and cancer riskNat Rev Endocrinol200951265165219924151
- CebiogluMSchildHHGolubnitschajaODiabetes mellitus as a risk factor for cancer: stress or viral etiology?Infect Disord Drug Targets200882768718537703
- FedericoAMorgilloFTuccilloCCiardielloFLoguercioCChronic inflammation and oxidative stress in human carcinogenesisInt J Cancer2007121112381238617893868
- AdamiHOTrichopoulosDObesity and mortality from cancerN Engl J Med2003348171623162412711736
- VigneriPFrascaFSciaccaLFrittittaLVigneriRObesity and cancerNutr Metab Cardiovasc Dis20061611716399485
- SunJWZhaoLGYangYMaXWangYYXiangYBObesity and risk of bladder cancer: a dose-response meta-analysis of 15 cohort studiesPLoS One2015103e119313
- LinYWangYWuQAssociation between obesity and bladder cancer recurrence: a meta-analysisClin Chim Acta2018480414629408169
- QinQXuXWangXZhengXYObesity and risk of bladder cancer: a meta-analysis of cohort studiesAsian Pac J Cancer Prev20131453117312123803089
- ClearyMPGrossmannMEMinireview: obesity and breast cancer: the estrogen connectionEndocrinology200915062537254219372199
- HuXJunejaSCMaihleNJClearyMPLeptin--a growth factor in normal and malignant breast cells and for normal mammary gland developmentJ Natl Cancer Inst200294221704171112441326
- LindgrenAPukkalaENissinenATuomilehtoJBlood pressure, smoking, and the incidence of lung cancer in hypertensive men in North Karelia, FinlandAm J Epidemiol2003158544244712936899
- XuSZhangGMGuanFJThe association between metabolic syndrome and the risk of urothelial carcinoma of the bladder: a case-control study in ChinaWorld J Surg Oncol20151323626246367
- CantielloFCicioneASaloniaAAssociation between metabolic syndrome, obesity, diabetes mellitus and oncological outcomes of bladder cancer: a systematic reviewInt J Urol2015221223225345683