Abstract
Triple-negative breast cancer (TNBC) is a heterogeneous disease with poorer outcomes compared to other breast cancer subtypes. Contributing to the worse prognosis in TNBC is the higher rates of relapse and rapid progression after relapse. Advances in targeted therapeutics and conventional chemotherapy for TNBC have been stymied due to the lack of specific targets. Moreover, the responses to chemotherapy in TNBC lack durability, partially accounting for the higher rates of relapse. Immunotherapy, notably immune-checkpoint blockade, has shown to improve survival and maintain robust antitumor responses in both hematologic and solid malignancies. Unlike lung cancer, melanoma, and bladder cancer, most breast cancers are not inherently immunogenic and typically have low T cell infiltration. However, among breast cancer subtypes, TNBC is characterized by greater tumor immune infiltrate and higher degree of stromal and intratumoral tumor-infiltrating lymphocytes (TILs), a predictive marker for responses to immunotherapy. Moreover, in TNBC, the high number of stromal TILs is predictive of more favorable survival outcomes and response to chemotherapy. Immunotherapy is being extensively explored in TNBC and clinical trials are showing some promising results. This article focuses on the rationale for immunotherapy in TNBC, to explore and discuss preclinical data, results from early clinical trials, and to summarize some ongoing trials. We will also discuss the potential application of immunotherapy in TNBC from a clinician’s perspective.
Introduction
Triple-negative breast cancer (TNBC) is a subtype of breast cancer characterized by absence of estrogen receptor (ER), progesterone receptor, and human epidermal growth factor receptor 2 (HER2) and represents about 15%–20% of all breast cancer.Citation1 TNBC patients often present with visceral involvement and typically show rapid progression and thus providing limited window of treatment opportunity. Tremendous advances have occurred in other subtypes of breast cancer such as HER2+ tumors with the development of targeted agents against the HER2 receptor. Monoclonal antibodies, such as trastuzumab and pertuzumab and drug–antibody conjugates, like T-DM1, have changed the management of HER2+ breast cancer.Citation2 ER+ breast cancers have agents that block estrogen signaling through either aromatase inhibition or selective ER modulation. Coupling the anti-estrogen therapy with newly approved cyclin-dependent kinase inhibitors, like palbociclib, ribociclib, and abemaciclib, has shown improvements in progression-free survival.Citation3,Citation4 In an effort to discover actionable targets and drug development, TNBC has been further stratified into molecular subtypes.Citation5 Gene expression profiling has revealed six distinct molecular subtypes, including two basal-like, an immunomodulatory, a mesenchymal, a mesenchymal stem-like, and a luminal androgen receptor.Citation5 These molecular subtypes could be utilized in identifying personalized treatment strategies as they appear to have both predictive and prognostic value.Citation5
Tumor-infiltrating lymphocytes (TILs), present both intratumorally and in adjacent stromal tissues, have predictive and prognostic roles in breast cancer. Within breast cancer, increased TILs at diagnosis have been significantly associated with pathologic complete responses with neoadjuvant chemotherapy.Citation6,Citation7 Interestingly, the improved overall survival in the context of neoadjuvant therapy was only seen in TNBC and HER2+ breast cancer and this improved prognosis was inversely associated with disease stage.Citation6,Citation7 This subtype-specific disparity in overall survival may be due to elevated TILs in TNBC compared to other breast cancer subtypes.Citation8 In the context of HER2+ breast cancer, increased levels of TILs have been associated with improved response to the anti-HER2 antibody, trastuzumab.Citation9 In subsequent work, a high degree of TILs found in majority of TNBC have been correlated with higher likelihood of benefit from adjuvant and neoadjuvant chemotherapy, with lower risk of disease relapse.Citation9–Citation13 This association of TILs in TNBC with therapeutic response and both overall and disease-free survival underscores the prognostic value of antitumor immunity in treating patients with TNBC. The presence of TILs also serves as a predictive marker of immunotherapy response, making the examination of immunotherapy in TNBC particularly intriguing.Citation14 However, important consideration should be made for TNBC subtypes, with IM and basal-like subtypes possessing elevated infiltration of immune cells, antigen-presenting cells, and activation of immune pathways.Citation15 Additionally, basal-like TNBC subtypes are known to have high frequency of BRCA1 and BRCA2 mutations and hence unstable genetics, another predictive marker for immunotherapy response.Citation5,Citation14
The immune system not only plays a role in tumor initiation and progression, but also participates in recognition and destruction of cancer cells. The antitumor immune response dampens development/progression through tumor-directed immune responses involving cytolytic T lymphocytes.Citation16,Citation17 For progression to occur, tumors must evade the cytotoxic anti-tumor response through a diverse array of mechanisms. The evasion of immune activation is recognized as a hallmark of cancer and can involve chronic activation of humoral immunity, infiltration by Th2 T cells, protumor-polarized innate inflammatory cells, downregulation of tumor-specific anti gens, expression of negative immune checkpoints by tumors, and the absence of major histocompatibility complexes (MHC) on the surface of tumors cells.Citation14,Citation16,Citation17 Ultimately, these mechanisms act in concert to moderate antitumor response and promote tumor development and disease progression.Citation18
Manipulation of the immune system represents an attractive strategy for TNBC, a breast cancer subtype that has not seen substantial advances in clinical management. Immune-checkpoint inhibitors have yielded promising results in both advanced and early-stage disease of TNBC patients and are expected to substantially improve the overall prognosis of TNBC. A focus of the field in translating immunotherapies from immunogenic tumors, like melanoma or renal cancers, to the majority of solid tumors is the identification of patients who would benefit most from immunotherapy and identification of agents to prime the tumor microenvironment.Citation14 Of particular interest in the clinical management of TNBC would be the use of radiation or chemotherapy to augment responses to immunotherapy. Radiation increases mutational load of tumors, optimizes antigen presentation, and may act to decrease immune suppressors in the tumor microenvironment, priming the tumor for immunotherapy.Citation19–Citation23 In addition to radiation, recent investigation into the use of platinum-based chemotherapy before the induction of immunotherapy in lung cancer has shown superior response and progression-free survival compared to the standard of care.Citation24,Citation25 In this review, we will comprehensively summarize early and ongoing clinical trials of immunotherapy in TNBC. Our goal is to offer a clinical prospective on the potential promise and perils of translating immunotherapies into TNBC and likely some other nonimmunogenic solid cancers.
Immunotherapy
Immunotherapy works through stimulation of the immune system by active immunization with cancer vaccines, or passive immunization through tumor-specific antibodies and immune modulators, like immune-checkpoint inhibitors.
Immune-checkpoint inhibitors
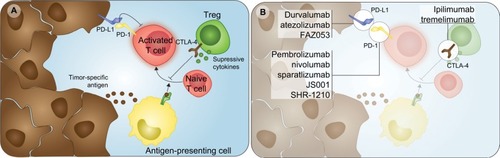
Immune checkpoints are a diverse set of regulatory points for the adaptive immune system, with roles in self-tolerance and antitumor immunity (). Physiologically, these checkpoints function in either the negative or positive regulation of the immune response, coordinating the magnitude and type of response.Citation26 The majority of published clinical trials using immune-checkpoint blockade have focused on antibodies that target cytotoxic T lymphocyte-associated antigen 4 (CTLA-4) and the programmed cell death protein 1 pathway (PD-1/PD-L1). As negative regulators of immune activation, the presence of CTLA-4 and PD-1 in the tumor microenvironment prevents a comprehensive antitumor immune response.Citation26 Monoclonal antibodies targeting PD-1/PD-L1 or CTLA-4 are thought to function by removing the inhibition of the antitumor immune response.Citation26 A visual summary of agents targeting these two immune checkpoints that are currently being investigated in TNBC is available in .
Figure 1 General mechanisms and agents targeting immune checkpoints in TNBC.
Notes: (A) Major immune cell players and interactions in the tumor microenvironment regulated by immune checkpoints. (B) Current therapies targeting PD-L1, PD-1, and CTLA-4 immune checkpoints under investigation in triple-negative breast cancer.
Abbreviations: CTLA-4, cytotoxic T lymphocyte-associated antigen 4; PD-1, programmed cell death protein 1; PD-L1, programmed death ligand 1; TNBC, triple-negative breast cancer; Treg, regulatory T cell.
PD-1 is expressed on the surface of lymphocytes and antigen-presenting cells. In the context of antitumor immunity, the binding of PD-1 on T cells with the ligands, PD-L1 or PD-L2, functions to suppress signals downstream of T-cell-receptor activation.Citation27,Citation28 With a lower side effect profile compared to anti-CTLA-4 and a wider range of approvals by the Food and Drug Administration (FDA), agents targeting PD-1 or PD-L1 have become a focus of moving immune-checkpoint blockade into many tumors. Several agents, such as pembrolizumab (anti-PD-1), nivolumab (anti-PD-1), atezolizumab (anti-PD-L1), avelumab (anti-PD-L1), and durvalumab (anti-PD-L1), have shown to be effective in various malignancies and are approved for treatment in melanoma, non-small-cell lung cancer, Hodgkin’s lymphoma, bladder cancer, gastroesophageal cancer, primary mediastinal large B-cell lymphoma, cervical cancer, renal cancer, and head and neck cancer.Citation29 Recent unprecedented approval of pembroli-zumab in metastatic cancers with microsatellite instability or deficiency in DNA mismatch repair irrespective of the tissue of origin emphasizes the importance of mutational burden in response to immune-checkpoint blockade.Citation30,Citation31
PD-L1 expression has been found in 20%–50% of all breast cancer subtypes and its expression has been associated with higher histologic grades, larger tumors, and absence of hormone receptors.Citation32 Higher PD-L1 expression has been observed in TNBCs as compared to non-TNBCs.Citation33–Citation35 This increased expression may be a result of genomic amplification of 9p24.1, containing CD274 (PD-L1) and PDCD1LG2 (PD-L2) in a subset of TNBC, but not ER+ tumors.Citation36 Across a number of malignancies, the expression of PD-L1 has been associated with increased TILs and response to anti-PD-L1 immune-checkpoint blockade.Citation37–Citation44 In the context of the latter, PD-L1 staining in melanoma and lung cancer has been used to identify patients that would likely benefit from anti-PD-1/PD-L1 therapies.Citation45 Interestingly, the presence of PD-1+ lymphocytes and PD-L1 expression in breast cancer has been linked to poor prognosis in several reports.Citation33,Citation34 However, the immunohistochemical (IHC) staining of PD-1/PD-L1 was also tied to increased tumor stage, nodal involvement, triple-negative status, and Ki-67 proliferative marker staining, all independent poor prognostic indicators.Citation33,Citation34 More recently, the expression of PD-L1 in breast cancer, and specifically in basal-like TNBC, has been associated with longer overall and disease-free survival.Citation46,Citation47 The use of PD-L1 staining to segregate TNBC patients may be useful with increasing single-agent response rates from 5%–8.8%Citation48,Citation49 to 18.5%–26%Citation50–Citation52 with the use of PD-L1 IHC staining as inclusion criteria.
Pembrolizumab
Receiving the initial FDA approval for unresectable or metastatic melanoma in 2014, pembrolizumab is one of the most studied of the immune-checkpoint therapies. Highlighting this fact was the presentation of clinical trial results in 25 tumor types at the 2018 annual meeting of the American Society of Clinical Oncology (ASCO). In 2016, the KEYNOTE-012 trial, Phase Ib study reported efficacy with acceptable safety profile when pembrolizumab was given 10 mg/kg every 2 weeks to patients with heavily pretreated, advanced TNBC.Citation50 Among the 27 patients who were evaluated for antitumor activity, the overall response rate was 18.5%, with median response time of 17.9 weeks.Citation50 A single-agent Phase II study examining a 200 mg dose given once every 3 weeks is ongoing. The KEYNOTE-086 trial is currently investigating the use of pembrolizumab in metastatic TNBC (NCT02447003) at 200 mg every 3 weeks. In the oral session at the 2017 ASCO meeting, cohort A and B were presented.Citation48,Citation52 Cohort A consisted of TNBC patients that progressed on at least one systemic therapy. In this 170-patient cohort, 8 (4.7%) responded and 13 (7.6%) achieved disease control, to include stable disease, partial response, and complete response, for 24 weeks or longer.Citation47 Additionally, one patient (0.6%) had a complete response to pembrolizumab monotherapy, and 27% had an initial reduction in target lesion.Citation47 Cohort B of the KEYNOTE-086 trial consisted of metastatic TNBC with PD-L1+ tumors, as defined by an IHC-based composite score, with no prior systemic therapy. In this cohort, objective responses were seen in 23% of 52 patients.Citation52 The increased response in cohort B may be a result of the use of pembrolizumab as a first-line therapy and the use of PD-L1+ tumors as an inclusion criterion, with only 58% of the enrolled patients possessing a combined positive PD-L1 composite score of greater than 1.Citation52
Similar to recent success of combinatorial platinum and anti-PD-1 therapy in lung cancer,Citation24,Citation25 the use of DNA damaging agents may improve response by inducing cancer cell death and releasing tumor-specific antigens. In locally advanced breast cancer, the addition of pembrolizumab to standard neoadjuvant chemotherapy (paclitaxel followed by doxorubicin and cyclophosphamide) increased the rate of pathologic complete response approximately threefold in the I-SPY 2 trial.Citation53 The addition of pembrolizumab to chemotherapy had a complete pathologic response of 60% vs 20% with chemotherapy-alone arm.Citation53 Initial data on a small cohort of patients in the KEYNOTE-173 presented at ASCO 2017 suggested improved objective response rate of 100% with combination of pembrolizumab and carboplatin vs 80% in another experimental group (nab-paclitaxel + pembrolizumab).Citation54 In spontaneous tumor models of BRCA1-mutated TNBC, the use of cisplatin inhibited tumor growth and functioned additively with anti-PD-L1 and anti-CTLA-4 combinatorial therapy.Citation55 A similar strategy of the use of poly-ADP ribose polymerase (PARP) inhibitors, selective single-strand DNA inhibitors, in BRCA-mutated TNBC and ovarian cancer found a 45% objective response rate in combination with pembrolizumab,Citation56 compared to the single-agent Phase I trial of the same PARP inhibitor (niraparib) response rate of 16.7%, suggesting the combination of the two may function synergistically.Citation57
Anti-PD-L1 therapies
Initial phase I findings of the anti-PD-L1 monoclonal antibody (MPDL3280A, atezolizumab) in metastatic TNBC were also recently reported. Of the nine patients evaluable for efficacy, the overall response rate was 33% (one complete and two partial responders) among advance TNBC patients, 90% of whom were previously treated with more than two prior regimens and one-third of whom enrolled had visceral metastases.Citation58 Similarly, a larger-scale Phase Ib study involving 168 patients, with 57 TNBC patients, who previously received taxane and anthracycline therapies, was used to evaluate the anti-PD-L1 agent (avelumab).Citation49 Across the entire cohort, the objective response rate was 5.4% with an additional 40 patients developing stable disease.Citation49 Importantly, TNBC patients with PD-L1 expression on immune cells had the clinical response as high as 44.4% vs 2.6% in those TNBC patients without the PD-L1-positive immune cells.Citation49 Similar response rate of 48.4% was seen using durvalumab in conjunction with neoadjuvant GeparNeuvo (NCT02685059).Citation59 The variable expression patterns of PD-L1 in a tumor led to investigations into antibody–drug conjugates (ADC) of anti-PD-L1 with monomethyl auristatin, an antimitotic drug.Citation60 Using an anti-PD-L1 antibody with enhanced activity for glycosylated PD-L1, Li et al demonstrated that the use of the ADC enhances efficacy of immunotherapy and increases bystander-killing of adjacent tumor cells.Citation60
Combination of checkpoint blockade
CTLA-4 functions earlier in the T cell activation process and is a major suppressive mechanism of the regulatory T cell (Treg).Citation26,Citation61 Recent research has suggested that depletion of Tregs by anti-CTLA-4 therapy is one of the major reasons leading to therapeutic responses.Citation62,Citation63 The nonredundant function of PD-1 and CTLA-4 in eliciting and maintaining immune cell activation led to combinatory therapy blocking the two immune checkpoints. In both melanoma and lung cancer, the use of nivolumab and ipilimumab (anti-CTLA-4) antibody has demonstrated better responses compared to nivolumab or chemotherapy alone.Citation64,Citation65 Interestingly, the efficacy of such combination relies on cancer types. In lung cancer the combination of nivolumab and ipilimumab did not perform any better than nivolumab alone in progression-free and overall survival regardless of PD-L1 staining.Citation65 This has not slowed down the exploration of combinatorial anti-CTLA-4/PD-1 trials, with an ongoing Phase I/II open-label trial of nivolumab plus ipilimumab vs nivolumab alone for patients with metastatic solid tumors, which include those with TNBC (NCT01928394). Additionally, a single-arm Phase II study of durvalumab in combination with the anti-CTLA-4, tremelimumab, is recruiting metastatic HER2-breast cancer patients (NCT02536794).
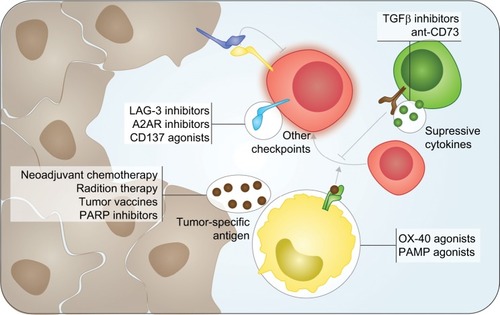
The combination of immune-checkpoint blockade with other drugs or targeting other immune checkpoints is moving forward in breast cancer (). LAG-3 is another negative checkpoint that binds to MHC II receptors and modulates antigen-presenting cells; IMP321 (LAG-3Ig), a competitive inhibitor for LAG-3/MHC II receptor binding, when combined with paclitaxel had objective response rate of 50% as a first-line therapy.Citation66 Targeting LAG-3 is the basis of several clinical trials in breast cancer, being used as an adjuvant to paclitaxel (NCT02614833) and in conjunction with anti-PD-1 therapy in TNBC (NCT02460224 and NCT03250832). Preliminary results of anti-PD-1 with anti-LAG-3 therapy found an objective response of 40% in TNBC.Citation67 In contrast, OX-40 is a positive immune-checkpoint functioning in maintaining T cell proliferation after receptor activation and suppressing Treg function.Citation68,Citation69 A Phase I/II trial into the combination of agonistic monoclonal antibody combined with either anti-PD-1 or anti-CTLA-4 therapies is recruiting advanced cancers including TNBC (NCT03241173). With a similar rationale, NKTR-214, a CD122 agonist, is being evaluated in TNBC with initial result of a 33% response rate when paired with anti-PD-1 therapy.Citation70 In contrast, the targeting of tumor-associated macrophages with anti-CSF1 and anti-PD-1 therapy had an objective response rate of 3.3% in a Phase Ib trial, underscoring the importance of selecting the right combinatorial agents for immune-checkpoint blockade.Citation71 Comprehensive summaries of the diverse range of related Phase I and II trials are listed as in the neoadjuvant () and adjuvant () settings. Additionally, small-molecule inhibitors against growth factors, PARP inhibitors, other immune checkpoints, and/or radiotherapy are currently recruiting advanced-stage TNBC patients in combination with anti-PD-1/PD-L1 or anti-CTLA-4 antibodies ().
Table 1 Clinical trials using immunotherapy with neoadjuvant chemotherapy
Table 2 Clinical trials using adjuvant immunotherapy
Table 3 Immunotherapy in combination with various agents under investigation in advanced triple-negative disease
Figure 2 Emerging immunotherapy targets and combinatorial agents in TNBC.
Notes: Current trials focus on modulating the tumor microenvironment by increasing mutational burden in tumors, stimulating antigen-presenting cells, decreasing suppressive functions of Tregs, and targeting other negative immune checkpoints on effector T cells.
Abbreviations: PAMP, pathogen-associated molecular pattern; PARP, poly-ADP ribose polymerase; TGFβ, transforming growth factor beta; TNBC, triple-negative breast cancer; Treg, regulatory T cell.
Combining radiotherapy/cryotherapy with immune-checkpoint blockade
Radiotherapy has potential to increase tumor mutation burden and increase tumor immunogenicity.Citation21–Citation23 The combination of radiotherapy with immune-checkpoint blockade has been studied in several tumor types like prostate cancer, lung cancer, sarcoma, and melanoma.Citation21,Citation23,Citation72,Citation73 The combination of local radiation to primary breast tumor with CTLA-4 blockade and PD-1/PD-L1 blockade has shown synergistic activity in preclinical murine models.Citation19,Citation20 Current investigations into the use of combinatorial radiotherapy and immune-checkpoint blockade include a Phase II trial of pembrolizumab plus radiotherapy in metastatic TNBC (NCT02730130). This trial focuses on the benefit or harm of radiation concurrently with pembrolizumab. Similarly, a Phase II trial of nivolumab after radiotherapy induction or chemotherapy (low-dose doxorubicin, cyclophosphamide, or cisplatin) in patients with metastatic TNBC (NCT02499367) is being sponsored by the Netherlands Cancer Institute. Recent Phase II findings by the group have called into question of pairing these therapies with immune-checkpoint blockade, with an initial report that irradiation and/or cyclophosphamide halved the response rate compared to nivolumab alone.Citation74 Other combinatory pilot studies have started, including the combination of stereotactic radiosurgery for oligometastatic breast cancer with pembrolizumab (NCT02303366) and the combination of hypofractionated radiotherapy with pembrolizumab in patients with advanced cancers, including breast cancer (NCT02303990).
Cancer vaccine
Cancer vaccines constitute another novel strategy in cancer immunotherapy. Therapeutic cancer vaccines have potential to elicit immune response against tumor-specific and tumor-associated antigens. Cancer vaccines include monovalent vaccines that provide a single tumor-associated antigen (TAA) target for the immune system and polyvalent peptide vaccines that provide multiple TAA targets. Cellular vaccines are mod ified tumor cells or antigen-presenting cells. A current list of clinical trials in TNBC using tumor vaccines or oncolytic viruses with checkpoint blockade is summarized in . The use of polyvalent and antigen-specific vaccines offers the potential of truly precision therapy by using the mutations or drivers of a tumor to elicit an immune response. In high-risk breast cancers that include TNBC, cancer vaccines could play a role in preventing relapse; however, to date, multiple cancer vaccine trials have failed to show improvement in clinical outcome. Notably in a phase III trial of metastatic breast cancer, the targeting of sialyl-Tn, a carbohydrate antigen found on glycoproteins, demonstrated no improvements in progression-free interval or overall survival.Citation75 In a follow-up analysis of results from the same trial, the authors did identify improvement in progression-free interval, overall survival, and antibody titer response in a subset of the patients receiving concomitant endocrine therapy.Citation76
Table 4 Cancer vaccine and immunotherapy clinical trials currently being conducted
The use of antigen-specific vaccine strategies provides a selection pressure for tumors to evolve mechanisms to evade the narrow epitope targeting.Citation77 One way of possibly overcoming this evasion is the use of personalized vaccines based on neoantigen fitness, or the likelihood of the antigen to be presented by the MHC and activate T cells. Although a number of barriers exist to prevent personalized vaccine usage for broad spectrum of patients in real time, the selection of multiple antigens based on the predicted ability to activate the antitumor immune system has shown promise in melanoma.Citation78–Citation82 When paired with anti-PD-1 therapy, the vaccines work synergistically with immune-checkpoint blockade.Citation79,Citation81 Similarly, the use of polyvalent vaccines derived from multiple antigens of the tumor or cell line has shown positive results in colorectal cancer,Citation83 prostate cancer,Citation84 follicular lymphoma,Citation85 and lung cancer.Citation86 The high rates of genomic instability within TNBC make the neoantigen fitness-based and polyvalent vaccination strategies intriguing.
Another avenue is the immunization of tumors with virus, such as the use of vaccinia virus modified to express MUC1 and interleukin 2.Citation87 The viral-mediated expression of MUC1, a nonspecific tumor antigen, to elicit an antitumor immune response mirrors the sialyl-Tn vaccination strategy.Citation75 Although partial tumor regression occurred in only 2 of the 31 patients with metastatic breast cancer, 14 patients developed stable disease.Citation87 A similar strategy of creating a tumor-specific antigen using a virus is being investigated in using a Modified Vaccinia Ankara virus to re-express wild-type p53 in combination with pembrolizumab.Citation88 Additionally, several small pilot studies of the oncolytic herpes simplex virus, HF10, demonstrated significant histopathologic response and reduction in tumor size of 30%–100%.Citation89,Citation90 The use of HF10 is currently being investigated in combination with chemotherapy for treatment of patients with unresectable pancreatic cancer (NCT03252808). Like these cancer-specific viral inoculations, newer vaccine approaches are on the horizon that can simultaneously vaccinate and use immune-checkpoint blockers to therapeutically block immune-suppressive pathway, which may increase the objective response rates.
Conclusion
TNBC remains the breast cancer subtype with the worse outcomes. Despite the progress made across many other cancers and other subtypes of breast cancer, effective treatment for advanced TNBC remains elusive. Immunotherapy with checkpoint inhibitors has shown promise, but response rates are very modest as single agent in advanced TNBCs. We have seen durable response in early-phase trials with anti-PD1 or anti-PD-L1, but response rates are up to 10% in unselected TNBC patients and improves only slightly to 20%–30% when patients are selected based on IHC-based PD-L1+ tumors.Citation48–Citation52
TILs appear to be higher in TNBC and multiple series of investigations have shown that higher TILs are associated with improved overall survival and higher response rate.Citation9–Citation13 The immunogenic microenvironment is associated with a better prognosis as a result of a higher likelihood of benefit from chemotherapy and possibly from immunotherapy, whereas cold immune microenvironment carries greater risk of relapse and lower benefit from chemotherapy and possibly immuno-therapy.Citation6,Citation7,Citation14 Identifying the subset of TNBC who will benefit most from available means of immune modulation should remain the priority while new targets and drugs are being developed. Biomarker-based patient identification, such as BRCA mutation, mutations in homologous recombination, and PD-L1 IHC testing, may improve clinical responses, but effort needs to focus on improving the development and standardization of valuable biomarkers of response.Citation49,Citation55,Citation56
Akin to the identification of biomarkers for immunotherapy response in TNBC, investigations are currently underway for combinatorial agents used as short-term induction treatment to increase immunogenicity in TNBC. Careful consideration of combination strategies, like the use of PARP inhibitors or specific chemotherapies, could be a highly successful strategy for immunotherapy in TNBC.
The development and early-phase trials into new immune checkpoints and tumor vaccine strategies for TNBC are compounding the excitement in the field. For a cancer that has not seen substantial advances in clinical management in recent decades, immunotherapy gives us a hope for durable clinical response for patients with TNBC. New agents and new combinations of immunotherapies may unlock the key to truly personalized cancer medicine. Belying the promise of immunotherapy in TNBC is a number of steps required to translate these therapies into meaningful outcomes and ultimately could turn out to be a hype. Specifically, efforts focused on understanding biology, biomarker selection, and strategies to enhance immunotherapy response are vital to the success of immunotherapy in TNBC and cancers in general.
Abbreviations
| TNBC | = | triple-negative breast cancer |
| TILs | = | tumor-infiltrating lymphocytes |
| ER | = | estrogen receptor |
| PR | = | progesterone receptor |
| HER2 | = | human epidermal growth factor receptor 2 |
| MHC | = | major histocompatibility complexes |
| CTLA-4 | = | cytotoxic T lymphocyte-associated antigen 4 |
| PD-1 | = | programmed cell death protein 1 |
| IHC | = | immunohistochemical |
| ASCO | = | American Society of Clinical Oncology |
| PARP | = | poly-ADP ribose polymerase |
| ADC | = | antibody–drug conjugates |
| Treg | = | regulatory T cell |
| TAA | = | tumor-associated antigen |
Acknowledgments
The authors are supported by the National Cancer Institute of the National Institutes of Health under award numbers R01s CA200673 (WZ), CA203834 (WZ), and F30 fellowship CA206255 (NB).
Disclosure
The authors report no conflicts of interest in this work.
References
- Cancer Genome Atlas NetworkComprehensive molecular portraits of human breast tumoursNature20124907418617023000897
- DawoodSBroglioKBuzdarAUHortobagyiGNGiordanoSHPrognosis of women with metastatic breast cancer by HER2 status and trastuzumab treatment: an institutional-based reviewJ Clin Oncol2010281929819933921
- CristofanilliMTurnerNCBondarenkoIFulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): final analysis of the multicentre, double-blind, phase 3 randomised controlled trialLancet Oncol201617442543926947331
- DiPippoAJPatelNKBarnettCMCyclin-dependent kinase inhibitors for the treatment of breast cancer: past, present, and futurePharmaco-therapy2016366652667
- LehmannBDBauerJAChenXIdentification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapiesJ Clin Invest201112172750276721633166
- LoiSTumor-infiltrating lymphocytes, breast cancer subtypes and therapeutic efficacyOncoimmunology201327e2472024073365
- AdamsSGrayRJDemariaSPrognostic value of tumor-infiltrating lymphocytes in triple-negative breast cancers from two phase III randomized adjuvant breast cancer trials: ECOG 2197 and ECOG 1199J Clin Oncol201432272959296625071121
- García-TeijidoPCabalMLFernándezIPPérezYFTumor-infiltrating lymphocytes in triple negative breast cancer: the future of immune targetingClin Med Insights Oncol201610Suppl 1313927081325
- LoiSMichielsSSalgadoRTumor infiltrating lymphocytes are prognostic in triple negative breast cancer and predictive for trastuzumab benefit in early breast cancer: results from the FinHER trialAnn Oncol20142581544155024608200
- AdamsSGoldsteinLJSparanoJADemariaSBadveSSTumor infiltrating lymphocytes (TILs) improve prognosis in patients with triple negative breast cancer (TNBC)Oncoimmunology201549e98593098593326405612
- DenkertCvon MinckwitzGDarb-EsfahaniSAbstract S1-09: evaluation of tumor-infiltrating lymphocytes (TILs) as predictive and prognostic biomarker in different subtypes of breast cancer treated with neoadjuvant therapy – a metaanalysis of 3771 patientsCancer Res2017774 SupplementS109
- LoiSSirtaineNPietteFPrognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02-98J Clin Oncol201331786086723341518
- DieciMVCriscitielloCGoubarAPrognostic value of tumor-infiltrating lymphocytes on residual disease after primary chemotherapy for triple-negative breast cancer: a retrospective multicenter studyAnn Oncol201425361161824401929
- BorcherdingNKolbRGullicksrudJVikasPZhuYZhangWKeeping tumors in check: a mechanistic review of clinical response and resistance to immune checkpoint blockade in cancerJ Mol Biol2018430142014202929800567
- VinayakSGrayRJAdamsSAssociation of increased tumor-infiltrating lymphocytes (TILs) with immunomodulatory (IM) triple-negative breast cancer (TNBC) subtype and response to neoadjuvant platinum-based therapy in PrECOG0105J Clin Oncol20173215_suppl1000
- HanahanDWeinbergRAHallmarks of cancer: the next generationCell2011144564667421376230
- de VisserKECoussensLMThe inflammatory tumor microenvironment and its impact on cancer developmentContrib Microbiol20061311813716627962
- HagerlingCCasbonAJWerbZBalancing the innate immune system in tumor developmentTrends Cell Biol201525421422025444276
- SharabiABNirschlCJKochelCMStereotactic radiation therapy augments antigen-specific pd-1-mediated antitumor immune responses via cross-presentation of tumor antigenCancer Immunol Res20153434535525527358
- DemariaSKawashimaNYangAMImmune-mediated inhibition of metastases after treatment with local radiation and CTLA-4 blockade in a mouse model of breast cancerClin Cancer Res2005112 Pt 172873415701862
- Twyman-Saint VictorCRechAJMaityARadiation and dual checkpoint blockade activate non-redundant immune mechanisms in cancerNature2015520754737337725754329
- SharabiABLimMDeweeseTLDrakeCGRadiation and checkpoint blockade immunotherapy: radiosensitisation and potential mechanisms of synergyLancet Oncol20151613e498e50926433823
- TakahashiYYasuiTTamariKRadiation enhanced the local and distant anti-tumor efficacy in dual immune checkpoint blockade therapy in osteosarcomaPLoS One20171212e018969729253865
- LangerCJGadgeelSMBorghaeiHCarboplatin and pemetrexed with or without pembrolizumab for advanced, non-squamous non-small-cell lung cancer: a randomised, phase 2 cohort of the open-label KEYNOTE-021 studyLancet Oncol201617111497150827745820
- GandhiLRodríguez-AbreuDGadgeelSPembrolizumab plus chemotherapy in metastatic non-small-cell lung cancerN Engl J Med2018378222078209229658856
- PardollDMThe blockade of immune checkpoints in cancer immunotherapyNat Rev Cancer201212425226422437870
- ChemnitzJMParryRVNicholsKEJuneCHRileyJLSHP-1 and SHP-2 associate with immunoreceptor tyrosine-based switch motif of programmed death 1 upon primary human T cell stimulation, but only receptor ligation prevents T cell activationJ Immunol2004173294595415240681
- SheppardKAFitzLJLeeJMPD-1 inhibits T-cell receptor induced phosphorylation of the ZAP70/CD3zeta signalosome and downstream signaling to PKCthetaFEBS Lett20045741–3374115358536
- HargadonKMJohnsonCEWilliamsCJImmune checkpoint blockade therapy for cancer: an overview of FDA-approved immune checkpoint inhibitorsInt Immunopharmacol201862293929990692
- LeDTUramJNWangHPD-1 blockade in tumors with mismatch-repair deficiencyN Engl J Med2015372262509252026028255
- LeDTDurhamJNSmithKNMismatch repair deficiency predicts response of solid tumors to PD-1 blockadeScience2017357634940941328596308
- GhebehHMohammedSAl-OmairAThe B7-H1 (PD-L1) T lymphocyte-inhibitory molecule is expressed in breast cancer patients with infiltrating ductal carcinoma: correlation with important high-risk prognostic factorsNeoplasia20068319019816611412
- MuenstSSoysalSDGaoFObermannECOertliDGillandersWEThe presence of programmed death 1 (PD-1)-positive tumor-infiltrating lymphocytes is associated with poor prognosis in human breast cancerBreast Cancer Res Treat2013139366767623756627
- MuenstSSchaerliARGaoFExpression of programmed death ligand 1 (PD-L1) is associated with poor prognosis in human breast cancerBreast Cancer Res Treat20141461152424842267
- MittendorfEAPhilipsAVMeric-BernstamFPD-L1 expression in triple-negative breast cancerCancer Immunol Res20142436137024764583
- BarrettMTAndersonKSLenkiewiczEGenomic amplification of 9p24.1 targeting JAK2, PD-L1, and PD-L2 is enriched in high-risk triple negative breast cancerOncotarget2015628264832649326317899
- TaubeJMAndersRAYoungGDColocalization of inflammatory response with B7-h1 expression in human melanocytic lesions supports an adaptive resistance mechanism of immune escapeSci Transl Med20124127127ra37
- TaubeJMKleinABrahmerJRAssociation of PD-1, PD-1 ligands, and other features of the tumor immune microenvironment with response to anti-PD-1 therapyClin Cancer Res201420195064507424714771
- TaubeJMYoungGDMcMillerTLDifferential expression of immune-regulatory genes associated with PD-L1 display in melanoma: Implications for PD-1 pathway blockadeClin Cancer Res201521173969397625944800
- TumehPCHarviewCLYearleyJHPD-1 blockade induces responses by inhibiting adaptive immune resistanceNature2014515752856857125428505
- AnsellSMLesokhinAMBorrelloIPD-1 blockade with nivolumab in relapsed or refractory Hodgkin’s lymphomaN Engl J Med2015372431131925482239
- BrahmerJReckampKLBaasPNivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancerN Engl J Med201537321627163926412456
- PassigliaFBronteGBazanVPD-L1 expression as predictive biomarker in patients with NSCLC: a pooled analysisOncotarget2016715197381974726918451
- InoueHParkJHKiyotaniKIntratumoral expression levels of PD-L1, GZMA, and HLA-A along with oligoclonal T cell expansion associate with response to nivolumab in metastatic melanomaOncoimmunology201659e120450727757299
- GandiniSMassiDMandalàMPD-L1 expression in cancer patients receiving anti PD-1/PD-L1 antibodies: a systematic review and meta-analysisCrit Rev Oncol Hematol2016100889826895815
- SunWYLeeYKKooJSExpression of PD-L1 in triple-negative breast cancer based on different immunohistochemical antibodiesJ Transl Med201614117327286842
- SabatierRFinettiPMamessierEPrognostic and predictive value of PDL1 expression in breast cancerOncotarget2015675449546425669979
- AdamsSSchmidPRugoHSPhase 2 study of pembrolizumab (pembro) monotherapy for previously treated metastatic triple-negative breast cancer (mTNBC): KEYNOTE-086 cohort AJ Clin Oncol20173515_suppl1008
- DirixLTakacsINikolinakosPAvelumab (MSB0010718C), an anti-PD-L1 antibody, in patients with locally advanced or metastatic breast cancer: a phase Ib JAVELIN solid tumor trialSan Antonio Breast Cancer Symposium2014S14
- NandaRChowLQDeesECPembrolizumab in patients with advanced triple-negative breast cancer: Phase Ib KEYNOTE-012 studyJ Clin Oncol201634212460246727138582
- SchmidPAtezolizumab in metastatic TNBC (mTNBC): long-term clinical outcomes and biomarker analysesAACR Proceedings2017 #2986
- AdamsSLoiSToppmeyerDPhase 2 study of pembrolizumab as first-line therapy for PD-L1-positive metastatic triple-negative breast cancer (mTNBC): preliminary data from KEYNOTE-086 cohort BJ Clin Oncol20173515_suppl1088
- NandaRLiuMCYauCPembrolizumab plus standard neoadjuvant therapy for high-risk breast cancer (BC): results from I-SPY 2J Clin Oncol20173515_suppl50628029304
- SchmidPParkYHMuñoz-CouseloEPembrolizumab (pembro) + chemotherapy (chemo) as neoadjuvant treatment for triple negative breast cancer (TNBC): preliminary results from KEYNOTE-173PASCO20173515_suppl556
- NolanESavasPPolicheniANCombined immune checkpoint blockade as a therapeutic strategy for BRCA1-mutated breast cancerSci Transl Med20179393eaal492228592566
- KonstantinopoulosPAWaggonerSEVidalGATOPACIO/Keynote-162 (NCT02657889): a phase 1/2 study of niraparib + pembrolizumab in patients (pts) with advanced triple-negative breast cancer or recurrent ovarian cancer (ROC)—results from ROC cohortJ Clin Oncol20183615_suppl106
- SandhuSKSchelmanWRWildingGThe poly (ADP-ribose) polymerase inhibitor niraparib (MK4827) in BRCA mutation carriers and patients with sporadic cancer: a phase 1 dose-escalation trialLancet Oncol201314988289223810788
- EmensLBraitehFCassierPInhibition of PD-L1 by MPDL3280A leads to clinical activity in patients with metastatic triple-negative breast cancerSan Antonio Breast Cancer Symposium2014PD1PD16
- LoiblSUntchMBurchardiNRandomized phase II neoadjuvant study (GeparNuevo) to investigate the addition of durvalumab to a taxane-anthracycline containing chemotherapy in triple negative breast cancer (TNBC)J Clin Oncol20183615_suppl104
- LiCWLimSOChungEMEradication of triple-negative breast cancer cells by targeting glycosylated PD-L1Cancer Cell2018332e10:187201
- WingKOnishiYPrieto-MartinPCTLA-4 control over Foxp3+ regulatory T cell functionScience2008322589927127518845758
- SelbyMJEngelhardtJJQuigleyMAnti-CTLA-4 antibodies of IgG2a isotype enhance antitumor activity through reduction of intra-tumoral regulatory T cellsCancer Immunol Res201311324224777248
- Arce VargasFFurnessAJSLitchfieldKFc effector function contributes to the activity of human anti-CTLA-4 antibodiesCancer Cell201833464966329576375
- LarkinJChiarion-SileniVGonzalezRCombined nivolumab and ipilimumab or monotherapy in untreated melanomaN Engl J Med20153731233426027431
- HellmannMDCiuleanuTEPluzanskiANivolumab plus ipilimumab in lung cancer with a high tumor mutational burdenN Engl J Med2018378222093210429658845
- BrignoneCGutierrezMMeftiFFirst-line chemoimmunotherapy in metastatic breast carcinoma: combination of paclitaxel and IMP321 (LAG-3Ig) enhances immune responses and antitumor activityJ Transl Med201087120653948
- HongDSSchoffskiPCalvoAPhase I/II study of LAG525 ± spartalizumab (PDR001) in patients (pts) with advanced malignanciesJ Clin Oncol20183615_suppl3012
- PiconeseSValzasinaBColomboMPOX40 triggering blocks suppression by regulatory T cells and facilitates tumor rejectionJ Exp Med2008205482583918362171
- LinchSNMcNamaraMJRedmondWLOX40 agonists and combination immunotherapy: putting the pedal to the metalFront Oncol201553425763356
- DiabAHurwitzMEChoDCNKTR-214 (CD122-biased agonist) plus nivolumab in patients with advanced solid tumors: preliminary phase 1/2 results of PIVOTJ Clin Oncol201836300615_suppl3006
- CalvoAJoensuuHSebastianMPhase Ib/II study of lacnotu-zumab (MCS110) combined with spartalizumab (PDR001) in patients (pts) with advanced tumorsJ Clin Oncol201836301415_suppl3014
- KwonEDDrakeCGScherHICA184-043 InvestigatorsIpilimumab versus placebo after radiotherapy in patients with metastatic castration-resistant prostate cancer that had progressed after docetaxel chemotherapy (CA184-043): a multicentre, randomised, double-blind, phase 3 trialLancet Oncol201415770071224831977
- GoldenEBDemariaSSchiffPBChachouaAFormentiSCAn abscopal response to radiation and ipilimumab in a patient with metastatic non-small cell lung cancerCancer Immunol Res20131636537224563870
- KokMVoorwerkLHorlingsHAdaptive phase II randomized trial of nivolumab after induction treatment in triple negative breast cancer (TONIC trial): final response data stage I and first translational dataJ Clin Oncol20183615_suppl1012
- MilesDRochéHMartinMTheratope® Study GroupPhase III multicenter clinical trial of the sialyl-TN (STn)-keyhole limpet hemocyanin (KLH) vaccine for metastatic breast cancerOncologist20111681092110021572124
- IbrahimNKMurrayJLZhouDSurvival advantage in patients with metastatic breast cancer receiving endocrine therapy plus Sialyl Tn-KLH vaccine: post hoc analysis of a large randomized trialJ Cancer20134757758423983823
- MeleroIGaudernackGGerritsenWTherapeutic vaccines for cancer: an overview of clinical trialsNat Rev Clin Oncol201411950952425001465
- ŁukszaMRiazNMakarovVA neoantigen fitness model predicts tumour response to checkpoint blockade immunotherapyNature2017551768151752029132144
- OttPAHuZKeskinDBAn immunogenic personal neoantigen vaccine for patients with melanomaNature2017547766221722128678778
- LinnemannCvan BuurenMMBiesLHigh-throughput epitope discovery reveals frequent recognition of neo-antigens by CD4+ T cells in human melanomaNat Med2015211818525531942
- SahinUDerhovanessianEMillerMPersonalized RNA mutanome vaccines mobilize poly-specific therapeutic immunity against cancerNature2017547766222222628678784
- StrønenEToebesMKeldermanSTargeting of cancer neo-antigens with donor-derived T cell receptor repertoiresScience201635262911337134127198675
- VermorkenJBClaessenAMvan TinterenHActive specific immunotherapy for stage II and stage III human colon cancer: a randomised trialLancet199935391503453509950438
- SmallEDemkowTGerritsenWRA phase III trial of GVAX immunotherapy for prostate cancer in combination with docetaxel versus docetaxel plus prednisone in symptomatic, castration-resistant prostate cancer (CRPC)2009 Genitourinary Cancers Symposium200907
- SchusterSJNeelapuSSGauseBLVaccination with patient-specific tumor-derived antigen in first remission improves disease-free survival in follicular lymphomaJ Clin Oncol201129202787279421632504
- GiacconeGBazhenovaLANemunaitisJA phase III study of belagenpumatucel-L therapeutic tumor cell vaccine for non-small cell lung cancer (NSCLC)Eur J Cancer201349S2S3
- SchollSSquibanPBizouarneNMetastatic breast tumour regression following treatment by a gene-modified vaccinia virus expressing MUC1 and IL-2J Biomed Biotechnol20032003319420112975534
- ChungVMKosFHardwickNA phase 1 study of p53MVA vaccine in combination with pembrolizumabJ Clin Oncol2018365_suppl206
- KimataHImaiTKikumoriTPilot study of oncolytic viral therapy using mutant herpes simplex virus (HF10) against recurrent metastatic breast cancerAnn Surg Oncol20061381078108416865590
- SahinTTKasuyaHNomuraNImpact of novel oncolytic virus HF10 on cellular components of the tumor microenvironment in patients with recurrent breast cancerCancer Gene Ther201219422923722193629
