Abstract
Objectives
This meta-analysis aimed to demonstrate the impact of preoperative exercise therapy on surgical outcomes in patients with lung cancer and COPD. Pulmonary function and muscle capacity were investigated to explore their potential links with outcome improvements after exercise.
Methods
Articles were searched from PubMed, Embase, and the Cochrane Library with criteria of lung cancer patients with or without COPD, undergoing resection, and receiving preoperative exercise training. Key outcomes were analyzed using meta-analysis.
Results
Seven studies containing 404 participants were included. Patients receiving preoperative exercise training had a lower incidence of postoperative pulmonary complications (PPCs; OR 0.44, 95% CI 0.27–0.71) and shorter length of hospital stay (standardized mean difference −4.23 days, 95% CI −6.14 to −2.32 days). Exceptionally, pneumonia incidence remained unchanged. Patients with COPD could not obviously benefit from exercise training to reduce PPCs (OR 0.44, 95% CI 0.18–1.08), but still might achieve faster recovery. No significant difference in pulmonary function was observed between the two groups. However, 6MWD and VO2 peak were significantly improved after exercise training.
Conclusion
Preoperative exercise training may reduce PPCs for lung cancer patients. However, for patients with COPD undergoing lung cancer resection, the role of exercise is uncertain, due to limited data, which calls for more prospective trials on this topic. Rehabilitation exercise strengthens muscle capacity, but does not improve impaired pulmonary function, which emphasizes the possible mechanism of the protocol design.
Introduction
Lung cancer is the most fatal cancer worldwide, with an estimated 1.2 million new cases and 1.1 million deaths in 2012.Citation1 Lung cancer is also the leading cause of cancer death in low-urbanization areas for both males and females. The number of deaths from lung cancer in low-urbanization areas was 35,100, with mortality of 40.71 in 100,000.Citation2 Surgical resection remains the key treatment for patients with lung cancer. However, many patients referred for surgery may also have comorbidities, such as COPD or other systematic diseases,Citation3 which increase the risks of postoperative morbidity and mortality. Modern programs for enhanced recovery after surgery often include preoperative exercise training to reduce postoperative pulmonary complications (PPCs). Although isolated studies have looked at the impact of such preoperative exercise on patients with lung cancer and COPD, a comprehensive meta-analysis of the available data has hitherto been lacking. Some studies have revealed that intense-exercise therapy delivered in the perioperative period might be effective in helping patients recover well after lung surgery,Citation4,Citation5 though the extent of improvement varied among these reports. At the same time, there have been other studies not showing positive effects after rehabilitation training.Citation6–Citation8
PPCs are common after abdominal, cardiac, or thoracic surgery, and are associated with a higher rate of mortality, higher hospital costs, and prolonged hospital length of stay (LOS).Citation5 Two systemic reviews have reported that intense exercise before lung surgery might be applied as an effective preoperative therapy to decrease the risk of PCs.Citation4,Citation5,Citation9,Citation10 Nevertheless, neither of the reviews conducted a meta-analysis, because of the substantial heterogeneity among the intervention methods. Although statistical analysis was lacking, the outcomes described after exercise were clearly supportive of further meta-analysis. A recently published meta-analysisCitation11 presented optimistic evidence of the impact of preoperative exercise training on surgical outcomes. However, the unselected targeting population and limited sample size indicated that more trials were needed to distinguish the potential benefit.
For the large group of patients with lung cancer and COPD at diagnosis, the role of preoperative exercise in this specific group requires further investigation. Several randomized studies that included patients with COPD for preoperative rehabilitation were published recently, which may add more evidence in this regard. More importantly, detailed exploration of outcome improvement could facilitate protocol design for exercise therapy, such as pulmonary function rehabilitation or muscle-strengthening training. Therefore, we designed this meta-analysis with the aim of determining whether preoperative exercise helps to improve surgical outcomes in patients with lung cancer and COPD. Parameters of pulmonary function and muscle capacity were investigated to explore their potential links with outcome improvements after exercise training.
Methods
This meta-analysis was conducted according to the Cochrane Handbook for Systematic Reviews of Interventions and presented based on PRISMA guidance.Citation12 The meta-analyses of randomized trials adhered to the guidelines outlined in the PRISMA statement. The protocol for this meta-analysis is available from PROSPERO (CRD42018088413).
Eligibility criteria
We only included randomized controlled trials (RCTs) and prospective trials of preoperative exercise training compared with no exercise training for lung cancer patients with or without COPD. We considered studies published in any language. Patients with usual care were set as the control group. After these preoperative interventions and basic therapy, patients received video-assisted thoracoscopic surgery or open thoracotomy, as scheduled. Types of surgery included wedge resection, segmentectomy, lobectomy, and pneumonectomy. Patients received similar clinical monitoring after surgery, and PCs were clearly recorded. A subset of patients in the included trials was diagnosed with mild or moderate COPD, whose data were extracted for further analysis.
Interventions
Protocols of the included studies varied in terms of exercise type, frequency, and intensity, ranging from three times per day for 1 weekCitation13 to five times per week for 4 weeks.Citation14 Furthermore, two types of investigation after exercise were involved in the included studies: muscle capacity and pulmonary function analysis. Exercise programs contained aerobic exercise, resistance training, inspiratory muscle training, and education. In some studies, patients were advised to undertake a warm-up before exercise (after a 5-minute warm-up period, 50% of peak work rate was achieved).Citation15
Outcome measurements
Primary outcomes were PPCs (summarized by type based on included studies: pneumonia, atelectasis, pulmonary embolism, respiratory failure, dyspnea, hemorrhagic drainage, empyema, interstitial pneumonia, bronchial stump dehiscence, bronchospasm, and bronchopleural fistula), pneumonia after surgery (new infiltrate plus either fever [>38°C] and white-blood-cell count >11,000 or fever and purulent secretions),Citation11 duration of chest tube, and postoperative LOS. Secondary outcomes focused on the patients with lung cancer and COPD, including PPCs and postoperative LOS. Postintervention pulmonary function enhancement was also compared to analyze possible reasons linked with outcome change after preoperative exercise. Three parameters of exercise capacity were also compared after intervention: 6MWD (representing lower-limb muscle strength), VO2 peak (representing physical performance), and Borg scores (representing severity of dyspnea).
Search methods
PubMed, Medline, and the Cochrane Library (central) were searched from the earliest date of each to June 2017. The search string used the following keywords and was modified for each database: (“lung cancer” [MeSH] OR non-small-cell lung cancer OR small cell lung cancer) AND (lung surgery OR lobectomy) AND (physical therapy OR physiotherapy OR physical exercise OR physical therapy modalities).
Study selection
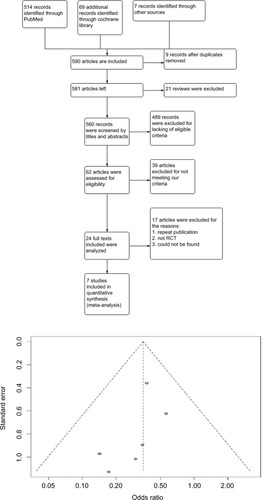
Through reading titles and abstracts, relevant articles were selected for full-text reading. Before this, two authors checked the search results and discussed the final list of the included articles. There was low bias in the included articles ().
Data extraction
Two authors read the articles and abstracted the data independently, and data were recorded using a predefined evidence table. Outcomes that we concentrated on were PPCs, LOS, and the duration of chest-tube drainage. We summarized information for each study in the list, eg, authors, publication year, type of study, number of participants, specific method of exercise, and index of pulmonary functions before surgery. The use of antibiotics was also clearly recorded.
Risk-of-bias appraisal
Risk of bias was assessed using the Cochrane Risk and Bias Tool, which was developed to evaluate the internal validity of the included RCTs.Citation16 In RevMan 5.0, the tool contains seven criteria: random-sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (report bias), and other risks of bias. The seventh criterion includes fraudulent results, other methodological flaws in RCTs, and the potential for industry bias.Citation17
Statistical analyses
Across all outcomes, a meta-analysis was conducted. Effect estimates are reported as ORs for the dichotomous outcomes. For continuous data, mean difference (MD) was used if outcomes were measured in the same way between trials, and standardized mean difference (SMD) was applied for combining trials measuring the same outcome but using different methods.
For primary outcomes, PPCs were evaluated using pooled RRs with corresponding 95% CIs, and a random-effect model was used to account for potential clinical heterogeneity.Citation18 Forest plots were constructed with RevMan 5.0, and P<0.05 was regarded as statistically significant. Heterogeneity was evaluated by I2: if I2>50%, an article was considered to display substantial heterogeneity, requiring subgroup analysis. To merge the outcomes, the statistic used for analysis was selected for paired analysis. Not all studies supplied complete data. Meanwhile, data that were able to be extracted from existing articles were merged in a forest plot.
Results
Search outcome
Two authors (XL and SLL) performed the literature search, and NW resolved conflicts and discrepancies. The primary literature search produced 590 results, including 20 reviews. After screening of titles and abstracts, 24 studies were found to be possibly relevant and underwent full-text critical appraisal, resulting in 16 exclusions (). Reasons for exclusion were outcomes recorded not being PPCs and LOS (n=12), no single regular intervention given (n=1), therapy was palliative (n=1), case reports (n=2), and duplicate publication (n=1). We included seven studies (Karenovics et al’s study was a substudy of Licker et al) in the final analysis, as shown in . All included studies were assessed by the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) evidence profile (). Guidance from GRADE offered a methodology to evaluate the quality of the evidence.
Table 1 Overview of included studies
Primary outcomes: PPCs, hospital LOS, chest-drain duration, pneumonia after preoperative exercise
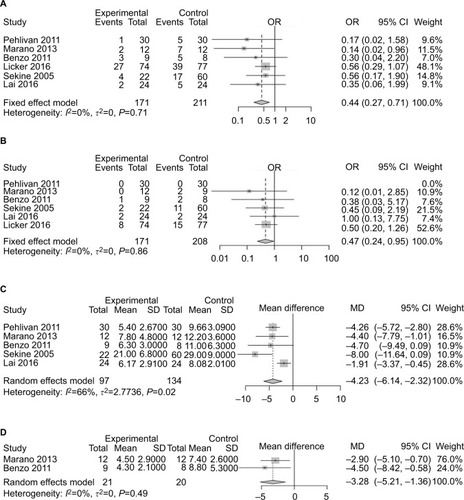
Six studiesCitation13,Citation14,Citation19–Citation22 had reported PPCs. Preoperative exercise reduced the risk of complications after surgery (OR 0.44, 95% CI 0.27–0.71; ). The heterogeneity of this result was acceptable (I2=0, P<0.0001). Five studiesCitation8,Citation13,Citation14,Citation21,Citation22 reported postoperative pneumonia. Patients who received preoperative exercise before lung cancer resection had no statistically significant differences in the rate of pneumonia after surgery compared with those receiving usual care only (OR 0.47, 95% CI 0.24–0.95; ). For LOS, five studiesCitation13,Citation14,Citation19,Citation21,Citation22 reported that patients receiving preoperative exercise training had shorter postoperative LOS (SMD −4.23 days, 95% CI −6.14 to −2.32 days; ). Two studiesCitation14,Citation19 recorded the duration of chest-tube drainage after surgery. Compared with patients receiving preoperative rehabilitation training, patients receiving usual care had a longer duration of chest-tube drainage (MD −3.28 days, 95% CI −5.21 to −1.36 days; ).
Figure 2 Forest plots of comparison: intervention group vs control group in lung cancer patients undergoing resection.
Note: (A) Risk of developing postoperative pulmonary complications; (B) incidence of postoperative pneumonia; (C) postoperative length of hospital stay; (D) duration of chest drainage.
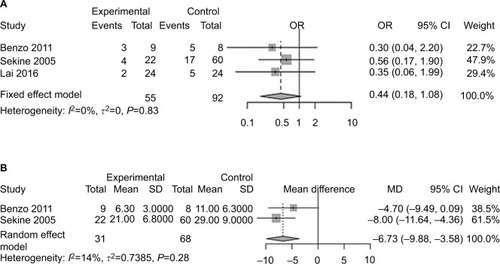
Primary outcomes: PPCs and LOS of patients with lung cancer and COPD
Three studiesCitation19,Citation21,Citation22 included patients diagnosed with COPD and lung cancer simultaneously. Statistically, no significant difference was found for PPC incidence between the exercise-intervention group and usual-care group (OR 0.44, 95% CI 0.18–1.08; ). Two studiesCitation19,Citation22 reported LOS of patients with COPD and lung cancer. Patients receiving preoperative exercise had shorter LOS (MD −6.73 days, 95% CI −9.88 to −3.58; ).
Secondary outcomes: impact of training exercise on pulmonary function capacity and exercise capacity before surgery
Pulmonary functions of patients in each study are listed in and analyzed in . There was little difference between the two groups. Three studies analyzed 6MWD,Citation13,Citation14,Citation21 which was considered an index of lower-limb muscle function.Citation23 Patients receiving exercise before surgery reported an improved 6MWD compared with those receiving usual care (SMD 71.25, 95% CI 39.68–102.82; ). VO2 peak, reflecting ability of oxygen uptake, was investigated to explore the role of exercise. After training, patients recorded a higher VO2 peak compared to those without trainingCitation20,Citation24 (SMD 3.26, 95% CI 2.17–4.35; ). Patients were less likely to improve in their dyspnea after preoperative exercise therapyCitation13,Citation21,Citation24 (MD −0.15, 95% CI −0.66 to 0.36; ).
Figure 4 Forest plots of comparison of post-intervention pulmonary function: intervention group vs control group in lung cancer patients undergoing resection.
Note: (A) FEV1; (B) FEV1%; (C) FVC%.
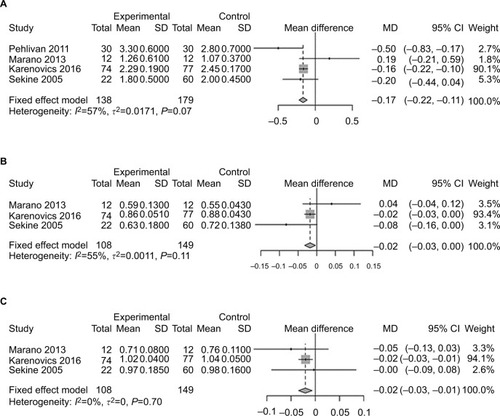
Figure 5 Forest plots of comparison: intervention group vs control group in lung cancer patients undergoing resection.
Note: (A) Postintervention 6MWD (index of lower-limb muscle strength); (B) VO2 peak (reflecting physical performance); (C) Borg scores (representing dyspnea).
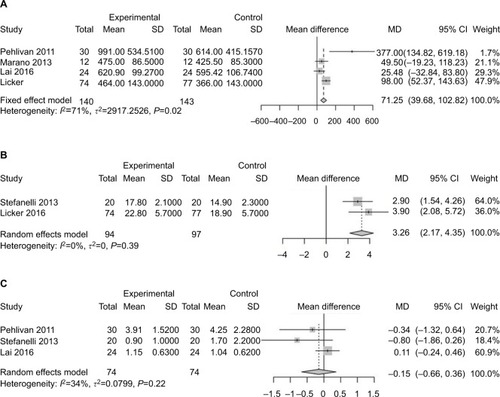
Table 2 Summary and comparison of pulmonary function in included studies
Discussion
Numerous studies with large samples have clearly demonstrated that the presence of COPD is linked with an increase in lung cancer incidence.Citation25 Many patients with lung cancer and COPD will face a significant challenge during the perioperative period. How to guide these patients with COPD before and after cancer surgery with a proper training protocol to improve surgical outcomes remains to be answered. In this meta-analysis, the results imply that preoperative exercise for patients with lung cancer and COPD may be associated with shorter LOS compared with usual care only, but incidence of PPCs remained unchanged even after exercise training. Accompanied by outcome improvement, several parameters of exercise capacity were found to be strengthening after exercise training, such as 6MWD and VO2 peak, because lower-limb muscle capacity was improved with higher ability of oxygen uptake. However, pulmonary function was not enhanced after training.
To date, a consistent protocol for preoperative exercise training has been lacking. Although pulmonary function and muscle-strength enhancement were commonly recorded in all the included studies, detailed methods for exercise training differed in terms of exercise duration and content.
Lai et alCitation21 designed an exercise protocol containing pharmacotherapy and intense-exercise training (respiratory training and endurance training). Notably, the pharmacotherapy in that study was used to relieve symptoms of dyspnea for patients with lung cancer and COPD, which helped patients to complete the exercise training smoothly. In that study, the small sample and patients in the usual-care group having a certain extent of exercise both contributed to a degree of bias.
Meanwhile, Morano et alCitation14 concluded that patients receiving preoperative exercise improved more when compared with those who received chest physical therapy only. The protocol was carefully designed, and contained less extreme endurance training and inspiratory muscle training. The protocol also included flexibility, stretching, and balance exercises in the warm-up and cooldown sections. At the same time, medicine was used to optimize the different preintervention conditions for better comparison. However, patients in the control group received chest physical therapy, which was different from usual care. Another study conducted by Sekine et al reported that COPD patients received breathing-exercise training and walking-exercise training. The reported protocol contained breathing exercises, such as incentive spirometry, abdominal breathing, detailed breathing exercises, and walking exercise, such as walking for 5,000 steps every day.Citation22 Although it was prospectively designed, allocation of the cases in the different groups was not randomized (60 vs 22).
Furthermore, Karenovics et alCitation15 reported an exercise protocol that included 5 minutes of warm-up and cooldown exercises. Patients were guided by a professional exercise physiotherapist. The workload of exercise was adjusted in each session to target near-maximal heart rate toward the end of each set of sprints. Notably, all patients were given advice regarding preoperative education and risk management.
Pulmonary rehabilitation has been proven to benefit patients with chronic lung disease, such as COPD.Citation26 Patients with COPD might experience deconditioning and exercise intolerance; therefore, preoperative rehabilitation should target these specific issues to obtain maximum effect. However, the mechanism of effect of exercise on outcome improvement remains unknown. Theoretically, preoperative exercise training is supposed to improve both lung function and muscle strength simultaneously. However, pulmonary function testing in this meta-analysis showed that most of the investigated parameters of pulmonary function were comparable or even slightly lower after exercise, though not significantly. A similar result was reported in other surgical procedures, such as lung transplantation.Citation27 Irreversible lung function after exercise training might represent the severity of the baseline condition of the lung disease and may not be the priority of treatment planning.
Interestingly, skeletal muscle weakness was reported commonly in patients with COPD,Citation28 which raised the question whether targeting muscle capacity may benefit surgical outcome. In this meta-analysis, we found a favorable trend of exercise capacity after training in the Forest plots, which might be related to outcome improvement, represented by improved 6MWD and VO2 peak. A newly published article reported a strong relationship between peak aerobic capacity, lower-limb muscle function, and lung-diffusion capacity. 6MWD is significantly related to lower-limb muscle function, but not to pulmonary function.Citation23 Licker et alCitation15 also reported the importance of VO2 peak in predicting cardiopulmonary complications. There is a lack of uniform recommendations for a training protocol before surgery for patients with lung cancer and COPD; therefore, these results provide positive evidence that a protocol designed to focus on exercise capacity in the future might have an impact on postoperative complications in this group.
Limitations
This study was subject to several limitations. First, PPCs were set as the main outcome in the analysis. However, different studies had individual definitions of complications, which might have caused bias in counting the PPCs. To reduce this selection bias, we chose those studies defining pneumonia clearly as a standard complication in the analysis, which showed a consistent trend with the overall outcome. Second, the protocol of every study was individually designed and the duration and intensity of exercise varied among the studies. During the process of meta-analysis, the heterogeneity of muscle strength and lung function among studies was still acceptable. Third, the end-point event for preoperative exercise is still obscure among studies, eg, how to decide the outcome of exercise, whether improved or declined, and what the parameters for performance evaluation are, such as lung function and exercise capacity. Exercise-protocol design should be based on information that allows evaluation of the efficacy of the procedure. Fourth, the type of exercise training (aerobic, strength, inspiratory muscle training) and the optimal duration were not consistent in the included studies, which should be balanced against the risk of delaying cancer resection and consequent extension of the disease. Finally, randomized trials on this topic are still scarce, especially for those patients with lung cancer and COPD, which may limit the power of the meta-analysis. In future, more prospective randomized studies are needed to accumulate further evidence.
Conclusion
The goal of the preoperative exercise is to decrease the risk of complications after surgery and enhance recovery, which can ultimately shorten LOS. This meta-analysis provides some evidence of the effect of preoperative exercise on enhanced recovery after surgery for patients with lung cancer and COPD. Future research should pay attention to details of the exercise protocol, such as intensity, duration, and methods, for those patients preparing for surgery.
Acknowledgments
The authors thank Elixigen Company (Huntington Beach, CA, USA) for proofreading. Beijing Municipal Administration of Hospitals Clinical Medicine Development Fund (grant number ZYLX201509), National Key R&D Program of China (No. 2018YFC0910700), Beijing Municipal Science & Technology Commission (No. Z161100000516063), Beijing Human Resources and Social Security Bureau (Beijing Millions of Talents Project, 2018A05), Special Fund of Beijing Municipal Administration of Hospitals Clinical Medicine Development (No. XMLX201841), Beijing Municipal Administration of Hospitals’Youth Programme (No. QML20171103), National Natural Science Foundation of China (grant number: 81502578), and Peking University Medicine Seed Fund for Interdisciplinary Research (BMU2018MX008).
Supplementary materials
Table S1 Studies excluded in this review
Table S2 Grading of recommendations, assessment, development, and evaluations
References
- CavalheriVJenkinsSCecinsNPatterns of sedentary behaviour and physical activity in people following curative intent treatment for non-small cell lung cancerChron Respir Dis201613828526721792
- EdvardsenESkjonsbergOHHolmeIHigh-intensity training following lung cancer surgery: a randomised controlled trialThorax20157024425025323620
- MaedaKHigashimotoYHondaNEffect of a postoperative outpatient pulmonary rehabilitation program on physical activity in patients who underwent pulmonary resection for lung cancerGeriatr Gerontol Int20161655055525953128
- SommerMSTrierKVibe-PetersenJPerioperative Rehabilitation in Operable Lung Cancer Patients (PROLUCA): A Feasibility StudyIntegr Cancer Ther20161545546627151595
- EstebanPAHernandezNNovoaNMEvaluating patients’ walking capacity during hospitalization for lung cancer resectionInteractive cardiovascular and thoracic surgery20172526827128475760
- CavalheriVGrangerCLIrvingLBShort-term preoperative exercise training: should we expect long-term benefits without postoperative exercise stimulus?European journal of cardiothoracic surgery : official journal of the European Association for Cardiothoracic Surgery2017521009
- ChangNWLinKCLeeSCEffects of an early postoperative walking exercise programme on health status in lung cancer patients recovering from lung lobectomyJ Clin Nurs2014233391340224646333
- MisselMPedersenJHHendriksenCRegaining familiarity with own body after treatment for operable lung cancer - a qualitative longitudinal explorationEur J Cancer Care (Engl)2016251076109026361265
- JonesLWPeddleCJEvesNDEffects of presurgical exercise training on cardiorespiratory fitness among patients undergoing thoracic surgery for malignant lung lesionsCancer200711059059817582629
- CoatsVMaltaisFSimardSHome-based rehabilitation program for lung cancer patientsEuropean Respiratory Journal2011
- CrandallKMaguireRCampbellAExercise intervention for patients surgically treated for Non-Small Cell Lung Cancer (NSCLC): a systematic reviewSurgical oncology201423173024529937
- WiskemannJHummlerSDiepoldCPOSITIVE study: physical exercise program in non-operable lung cancer patients undergoing palliative treatmentBMC cancer20161649927430336
- FangYMaGLouNPreoperative Maximal Oxygen Uptake and Exercise-induced Changes in Pulse Oximetry Predict Early Postoperative Respiratory Complications in Lung Cancer PatientsScandinavian Journal of Surgery201410320120824520103
- LoewenGMWatsonDKohmanLPreoperative exercise Vo2 measurement for lung resection candidates: results of Cancer and Leukemia Group B Protocol 9238Journal of thoracic oncology : official publication of the International Association for the Study of Lung Cancer20072619625
- WeinerPManAWeinerMThe effect of incentive spirometry and inspiratory muscle training on pulmonary function after lung resectionThe Journal of thoracic and cardiovascular surgery19971135525579081102
- SekineYChiyoMIwataTPerioperative rehabilitation and physiotherapy for lung cancer patients with chronic obstructive pulmonary diseaseThe Japanese journal of thoracic and cardiovascular surgery : official publication of the Japanese Association for Thoracic Surgery = Nihon Kyobu Geka Gakkai zasshi53237243
Disclosure
The authors report no conflicts of interest in this work.
References
- FerlayJSoerjomataramIDikshitRCancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012Int J Cancer20151365E359E38625220842
- ChenWZhengRZhangSCancer incidence and mortality in China in 2013: an analysis based on urbanization levelChin J Cancer Res201729111028373748
- LickerMJWidikkerIRobertJOperative mortality and respiratory complications after lung resection for cancer: impact of chronic obstructive pulmonary disease and time trendsAnn Thorac Surg20068151830183716631680
- Rodriguez-LarradALascurain-AguirrebenaIAbecia-InchaurreguiLCSecoJPerioperative physiotherapy in patients undergoing lung cancer resectionInteract Cardiovasc Thorac Surg201419226928124821016
- SommerMSTrierKVibe-PetersenJPerioperative rehabilitation in operation for lung cancer (PROLUCA) – rationale and designBMC Cancer20141440424898680
- CoatsVMaltaisFSimardSFeasibility and effectiveness of a home-based exercise training program before lung resection surgeryCan Respir J2013202e10e1623616972
- BobbioAChettaAAmpolliniLPreoperative pulmonary rehabilitation in patients undergoing lung resection for non-small cell lung cancerEur J Cardiothorac Surg2008331959818006327
- BenzoRWigleDNovotnyPPreoperative pulmonary rehabilitation before lung cancer resection: results from two randomized studiesLung Cancer201174344144521663994
- PouwelsSFiddelaersJTeijinkJAWoorstJFSiebengaJSmeenkFWPreoperative exercise therapy in lung surgery patients: a systematic reviewRespir Med2015109121495150426303337
- SmetanaGWPostoperative pulmonary complications: an update on risk assessment and reductionCleve Clin J Med200976Suppl 4S60S65
- CavalheriVGrangerCPreoperative exercise training for patients with non-small cell lung cancerCochrane Database Syst Rev20176CD01202028589547
- LiberatiAAltmanDGTetzlaffJThe PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health-care interventions: explanation and elaborationBMJ2009339b270019622552
- PehlivanETurnaAGursesAGursesHNThe effects of preoperative short-term intense physical therapy in lung cancer patients: a randomized controlled trialAnn Thorac Cardiovasc Surg201117546146821881371
- MoranoMTAraújoASNascimentoFBPreoperative pulmonary rehabilitation versus chest physical therapy in patients undergoing lung cancer resection: a pilot randomized controlled trialArch Phys Med Rehabil2013941535822926460
- KarenovicsWLickerMEllenbergerCShort-term preoperative exercise therapy does not improve long-term outcome after lung cancer surgery: a randomized controlled studyEur J Cardiothorac Surg2017521475428419206
- TriccoACCogoEHolroyd-LeducJEfficacy of falls prevention interventions: protocol for a systematic review and network meta-analysisSyst Rev2013213823738619
- TriccoACThomasSMVeronikiAAComparisons of interventions for preventing falls in older adults: a systematic review and meta-analysisJAMA2017318171687169929114830
- DerSimonianRLairdNMeta-analysis in clinical trials revisitedContemp Clin Trials201545Pt A13914526343745
- BenzoRWigleDNovotnyPPreoperative pulmonary rehabilitation before lung cancer resection: results from two randomized studiesLung Cancer201174344144521663994
- KarenovicsWLickerMEllenbergerCShort-term preoperative exercise therapy does not improve long-term outcome after lung cancer surgery: a randomized controlled studyEur J Cardiothorac Surg2017521475428419206
- LaiYSuJYangMZhouKCheGImpact and effect of preoperative short-term pulmonary rehabilitation training on lung cancer patients with mild to moderate chronic obstructive pulmonary disease: a randomized trialZhongguo Fei Ai Za Zhi20161911746753 Chinese27866517
- SekineYChiyoMIwataTPerioperative rehabilitation and physiotherapy for lung cancer patients with chronic obstructive pulmonary diseaseJpn J Thorac Cardiovasc Surg200553523724315952314
- BurtinCFranssenFMEVanfleterenLEGWGroenenMTJWoutersEFMSpruitMALower-limb muscle function is a determinant of exercise tolerance after lung resection surgery in patients with lung cancerRespirology20172261185118928370836
- StefanelliFMeoliICobuccioRHigh-intensity training and cardiopulmonary exercise testing in patients with chronic obstructive pulmonary disease and non-small-cell lung cancer undergoing lobectomyEur J Cardiothorac Surg2013444e260e26523892298
- HoughtonAMMechanistic links between COPD and lung cancerNat Rev Cancer201313423324523467302
- RiesALBauldoffGSCarlinBWPulmonary rehabilitation: joint ACCP/AACVPR evidence-based clinical practice guidelinesChest20071315 Suppl4S42S17494825
- PehlivanEBalcıAKılıçLKadakalFPreoperative pulmonary rehabilitation for lung transplant: effects on pulmonary function, exercise capacity, and quality of life; first results in turkeyExp Clin Transplant201816445546028969527
- AbdulaiRMJensenTJPatelNRDeterioration of limb muscle function during acute exacerbation of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2018197443344929064260