Abstract
Purpose
To improve public and medical awareness of the possibility of retinoblastoma (RB) in children who experienced inadvertent trauma with or without trauma-related symptoms and signs.
Patients and methods
Retrospective study of the clinical characteristics of children with a trauma history preceding a diagnosis of RB at the Zhongshan Ophthalmic Center, Sun Yat-sen University, between January 2013 and August 2018, and the number of children hospitalized with eye trauma during the same period.
Results
Among 793 consecutive patients with RB, 10 (1.3%) had a history of trauma. Two of these 10 patients (20%, accounting for nearly 0.2% of the 1103 eye trauma patients who were treated at our center) had undergone vitrectomy in an eye with unsuspected tumors. Of the 10 cases (12 eyes), only 5 (7 eyes) were initially diagnosed with RB or an intraocular space-occupying mass before referral to the oncology clinic, and 8 patients (80%) with 8 eyes that were ultimately staged as cT2b or higher underwent enucleation on referral to the oncology clinic. Although additional treatment was performed, two of these patients experienced intracranial metastasis and death during a mean follow-up time of 25.9 months from treatment.
Conclusion
More attention should be paid to the possibility of underlying RB in children of preschool age who have experienced trauma with or without eye signs.
Introduction
Retinoblastoma (RB) is a rare tumor of the eye that is usually initiated by biallelic mutation of the RB1 gene in a single susceptible developing retinal cell and is diagnosed in approximately 8000 children each year worldwide.Citation1 The survival rate of children with RB has drastically improved over the years as a result of early diagnosis and improved methods of treatment.Citation2 A recent analysis of RB patients in southwestern China showed that the overall mortality rate in this region was also low, at 9.1%.Citation3 Due to low public and medical awareness of the dangers of diagnostic delay, health care access barriers and socioeconomic issues,Citation1 the mortality rate of RB can reach 30% to 70% in developing countries in Africa and Asia.Citation2 The recognition of RB by medical professionals and family members of patients should be improved.
In recent years, researchers have reported a decrease in highly advanced tumors and tumors with a poor prognosis that has been attributed to early recognition and less mistreatment of these conditions.Citation4 However, a clear-cut history of trauma may also mask the diagnosis of RB in patients with various ocular complications, such as anterior chamber hemorrhage,Citation5 secondary glaucoma,Citation6 panophthalmitis,Citation7 and traumatic cataract,Citation8 and mislead the clinician, causing them to take inappropriate management measures, including cataract surgery,Citation8 vitrectomy,Citation9,Citation10 and trabeculectomy.Citation9 Unfortunately, a traumatic history not only obscures the diagnosis of RB but may also lead to cases not diagnosed based on the tumor presentation being a diagnosis in the advanced stages of the diseases.
Here, we review our experience with 10 children with RB with a diagnostic delay. We highlight the challenges experienced by doctors and their families in identifying this rare but important life-threatening disease.
Materials and Methods
After obtaining the approval from the ethics committee of Zhongshan Ophthalmic Center, we reviewed the computerized diagnostic records of consecutive patients with RB managed at Zhongshan Ophthalmic Center, Sun Yat-sen University, between January 2013 and August 2018. The charts of those patients who had a history of trauma before a diagnosis of RB were selected and studied in further detail. In addition, we determined the number of hospitalized children with eye trauma who were preschool-age (age 0–6 years) at our hospital during the corresponding period and calculated their mean age at the time of trauma. This study adhered to the tenets of the Declaration of Helsinki, and informed consent was obtained from the parents of all children.
The data collected in all RB patients with a history of trauma included the age at diagnosis, sex, trauma type, imaging features, previous interventions in the eyes, and the time interval between the trauma and initial RB treatment. Ultrasonography of the eye, CT scan or MRI of the orbit and brain and photographic documentation of the fundus were performed in all cases. Specifically, the initial diagnosis based on imaging features and management provided elsewhere before referral to our RB specialists were analyzed.
On referral to us, the RB laterality, pattern of heredity (sporadic or familial), and histopathologic features and the local and systemic management of the patients were reviewed. Furthermore, the T classification according to the American Joint Committee on Cancer (AJCC) tumor-node-metastasis (TNM) system (2017)Citation11 was assessed based on histopathological features or the results of ancillary examinations. During follow-up, patient status, including alive without metastasis, alive with orbital recurrence or dead as a result of intracranial metastasis, was recorded.
Results
Of 793 consecutive patients with RB managed at Zhongshan Ophthalmic Center, Sun Yat-sen University, 12 eyes of 10 children (6 males and 4 females) had an isolated history of trauma preceding their diagnosis, and there was a mean interval of 4.7 weeks between the trauma and RB treatment. In comparison to the mean age of 49.4 ± 19.8 months found in children with only eye trauma, the mean age at diagnosis of RB was 30.3 ± 19.4 months (). The disease was sporadic in all cases and unilateral in eight children ().
Table 1 Clinical Detail of 10 Patients Who Had a Background of Trauma Before the Diagnosis of Retinoblastoma
Table 2 Clinical Characteristics of 10 Patients Following Referral for the Diagnosis of Retinoblastoma
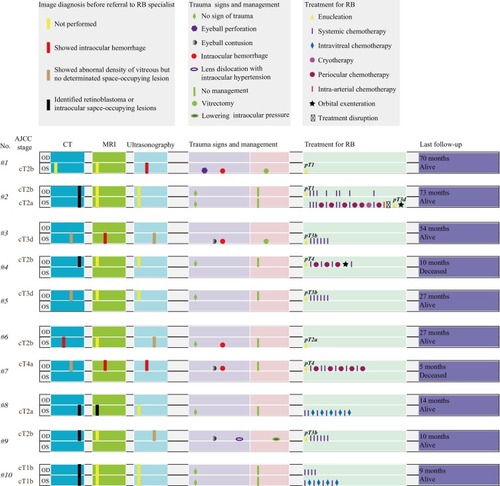
There are RB imaging signs of all patients depicted in , but only five patients had prior RB imaging diagnosis from . Five cases (7 eyes) were identified as having RB or intraocular space-occupying mass; however, there was an initial misdiagnosis at another clinic in five cases (5 eyes) before referral to our clinic. The misdiagnoses included abnormal density of the vitreous (n=1) and intraocular hemorrhage (n=4).
As shown in , of the patients who had a history of trauma, two suffered eye trauma with head trauma, three had only eye trauma, and one had only head trauma. In addition (and perhaps more notably), as a result of intraocular hemorrhage, 23 G vitrectomy was performed in two patients (0.2% of the 1103 children with eye trauma who underwent surgical intervention at our center during the corresponding period). However, RB was initially suspected in these two patients at the time of surgery, and the surgery was therefore stopped. Furthermore, periocular chemotherapy (20 mg of carboplatin) was performed to prevent orbital seeding. The two patients were then referred to RB specialists after cytologic analysis of the vitrectomy specimens. In one patient, no additional systemic chemotherapy was provided due to the parents’ refusal to accept it.
On referral to our oncology clinic, RB was confirmed by diagnostic examination (). According to the T classification, eight eyes of eight patients (80%) were staged as cT2b or higher and underwent enucleation. Ultimately, orbital exenteration was performed in two eyes of two patients with orbital recurrence, including one due to disease progression resulting from treatment interruption. To prevent RB metastasis, six patients with pT3a or higher, which is considered a high-risk feature, received adjuvant therapies (). However, only two patients classified as cT2a or cT1b received chemotherapy to preserve the eyeball (). Over a mean follow-up period of 31.7 months from the time of referral to our RB specialists, two children (20%) who were classified as pT4 died despite aggressive therapy.
Discussion
Early diagnosis is critical for the optimal prognosis of RB. The treatment regimen depends on the clinical severity of the disease at presentation. RB is curable when diagnosed early and treated appropriately.Citation12 However, we performed enucleation in eight eyes (8 patients) classified cT2b or higher (80% cases), indicating they carried a risk of extraocular spreadingCitation13 or failure to save the eye with poor vision.Citation14 Therefore, a diagnostic delay of RB could be associated with poor vision.
In a previous report, a delay in the diagnosis of RB accounted for an increased risk of highly advanced disease and mortality,Citation3,Citation4,Citation15 including enucleation in eight eyes (8 patients), a high risk of poor histology in six eyes (6 patients), and death in 20% of the patients in this study. Duration of symptoms longer than 9 months was previously shown to be a prognostic factor for a poor outcome.Citation3,Citation4 However, in our study, the mean time interval between trauma and RB treatment was 4.7 weeks. Therefore, there can be a long lag period between the first symptoms and trauma.
Early recognition of RB remains a challenge for patients’ family members because most of the presenting signs develop gradually over time in a tumor stage-dependent fashion, with near all patients exhibiting one or more of these signs by the time that the RB had reached an advanced stage. Zhao et alCitation16 investigated the clinical presentations observed in 595 eyes (470 patients) with untreated RB and reported that 73% of the patients exhibited the typical leukocoria feature at a mean age of 23 months, and 84% of the patients were younger than 3 years old at the time of diagnosis. Obtaining an early diagnosis shortly after the detection of symptoms can improve the survival rate.Citation17 Multiple campaigns should be initiated to increase public awareness and inform family members of RB signs.
Although the diagnosis of RB based on clinical features and ancillary tests is accurate in most cases, media opacity with a history of trauma can be misled the clinician away from an RB diagnosis. As reported by Balasubramanya et al,Citation18 atypical signs, such as secondary glaucoma (1%) and hyphema (<0.5%), may lead to misdiagnosis. Accordingly, intraocular hemorrhage is common in patients with ocular trauma and can occasionally completely mask an intraocular mass, as occurred in the initial misdiagnosis of RB observed in this study. Imaging examinations are especially useful in diagnosing RB with atypical presentation. However, the patient who underwent CT still had an undefined diagnosis of RB before referral to the oncology clinic. Given this consideration, clinicians should pay more attention to identifying imaging features that could potentially indicate an underlying retinal mass in preschool children with a history of trauma.
To avoid a life-threatening prognosis due to a diagnostic delay or vitrectomy in unsuspected RB,Citation19,Citation20 after exhaustive history-taking, physicians must be able to recognize the rare and puzzling effects of a background of trauma to have an adequate degree of suspicion to identify RB in children based on imaging features and provide them with a suitable treatment regimen.
Conclusions
RB may present in a child with a history of trauma in the involved eye or not involved eye. More importantly, the primary intraocular disease should not be interpreted clinically as a complication of trauma until the possibility of underlying RB is excluded.
Eye and head trauma in children should always warn pediatricians on the possibility of having visual impairment etiology. Ophthalmologists must rule out RB in all pediatric patients under 5 years old with unusual intraocular findings at the Emergency Department.
Ethics Approval and Informed Consent
Ethics Committee of Zhongshan Ophthalmic Center, Sun Yat-sen University approved this study and informed consent was obtained from the parents of all children.
Author Contributions
All authors contributed to conception and design, analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest related to this work.
Acknowledgments
We thank all the patients for cooperating in RB treatment and accepting our follow-up interview. This work was partly supported by the Ph.D. Start-up Fund of the Natural Science Foundation of Guangdong Province of China (grant number 2017A030310549), the Medical Scientific Research Foundation of Guangdong Province of China (grant number A2017488), and the National Natural Science Foundation of China (grant number 81800866; 81470664). The sponsors had no role in any stages from study design to manuscript preparation. Rongxin Chen, Huijing Ye, and Shu Liu are co-first authors for this study.
References
- Dimaras H, Corson TW, Cobrinik D, et al. Retinoblastoma. Nat Rev Dis Primers. 2015;1:15021. doi:10.1038/nrdp.2015.2127189421
- Kivela T. The epidemiological challenge of the most frequent eye cancer: retinoblastoma, an issue of birth and death. Br J Ophthalmol. 2009;93(9):1129–1131. doi:10.1136/bjo.2008.15029219704035
- Gao J, Zeng J, Guo B, et al. Clinical presentation and treatment outcome of retinoblastoma in children of South Western China. Medicine (Baltimore). 2016;95(42):e5204. doi:10.1097/MD.000000000000520427759657
- Faranoush M, Hedayati Asl AA, Mehrvar A, et al. Consequences of delayed diagnosis in treatment of retinoblastoma. Iran J Pediatr. 2014;24(4):381–386. doi:10.1111/ped.1240225755858
- Egleston D, Mc PS Jr., Perry R. Retinoblastoma with intracranial extension masked by trauma and anterior chamber hemorrhage: report of a case. Am J Ophthalmol. 1958;46(2):201–205. doi:10.1016/0002-9394(59)90009-113559355
- Gass JD. Retinoblastoma obscured by recent trauma. Arch Ophthalmol. 1963;69:583–584. doi:10.1001/archopht.1963.0096004058901013946747
- Spaulding AG, Naumann G. Unsuspected retinoblastoma. Enucleation in an 11-year-old girl following injury and panophthalmitis. Arch Ophthalmol. 1966;76(4):575–577. doi:10.2307/30067155928145
- Roth AM. Retinoblastoma seen after surgery for traumatic cataract. Ann Ophthalmol. 1978;10(11):1561–1564.727632
- Shen T, Liu R, Lin J, Huang H, Li X, Yan J. Pars plana vitrectomy and evisceration resulting in death due to misdiagnosis of retinoblastoma in children: a review of 3 cases. Medicine (Baltimore). 2015;94(32):e1338. doi:10.1097/MD.000000000000133826266382
- Chawla B, Hada M, Seth R, et al. Trabeculectomy in eyes with unsuspected retinoblastoma. Ophthalmic Genet. 2016;37(4):437–440. doi:10.3109/13816810.2015.112661026966836
- Mallipatna A, Gallie BL, Chévez-Barrios P, et al. Retinoblastoma In: Amin MB, Edge SB, Greene FLE, editors. AJCC Cancer Staging Manual, 8th New York, NY: Springer Science and Business Media; 2017:819–831.
- Rodriguez-Galindo C, Wilson MW, Chantada G, et al. Retinoblastoma: one world, one vision. Pediatrics. 2008;122(3):e763–e770. doi:10.1542/peds.2008-051818762512
- Murphree AL. Intraocular retinoblastoma: the case for a new group classification. Ophthalmol Clin North Am. 2005;18(1):41–53, viii. doi:10.1016/j.earlhumdev.2008.05.00815763190
- Gunduz K, Gunalp I, Yalcindag N, et al. Causes of chemoreduction failure in retinoblastoma and analysis of associated factors leading to eventual treatment with external beam radiotherapy and enucleation. Ophthalmology. 2004;111(10):1917–1924. doi:10.1016/j.ophtha.2004.04.01615465557
- Ghassemi F, Khodabande A. Risk definition and management strategies in retinoblastoma: current perspectives. Clin Ophthalmol. 2015;9:985–994. doi:10.2147/OPTH.S5982826089630
- Zhao J, Li S, Shi J, Wang N. Clinical presentation and group classification of newly diagnosed intraocular retinoblastoma in China. Br J Ophthalmol. 2011;95(10):1372–1375. doi:10.1136/bjo.2010.19113021252083
- Rodrigues KE, Latorre Mdo R, de Camargo B. Delayed diagnosis in retinoblastoma. J Pediatria. 2004;80(6):511–516. doi:10.2223/JPED.1266
- Balasubramanya R, Pushker N, Bajaj MS, Ghose S, Kashyap S, Rani A. Atypical presentations of retinoblastoma. J Pediatr Ophthalmol Strabismus. 2004;41(1):18–24. doi:10.1016/j.jcrs.2003.12.00314974830
- Kaliki S, Taneja S, Palkonda VAR. Inadvertent intraocular surgery in children with unsuspected retinoblastoma: a study of 14 cases. Retina. 2019;39(9):1794–1801. doi:10.1097/IAE.000000000000221429863537
- Stevenson KE, Hungerford J, Garner A. Local extraocular extension of retinoblastoma following intraocular surgery. Br J Ophthalmol. 1989;73(9):739–742. doi:10.1136/bjo.73.9.7392804029