Abstract
Background
In this study, we retrospectively evaluated a series of metastatic nasopharyngeal carcinoma (mNPC) patients who received oral maintenance chemotherapy using S-1/capecitabine after systemic chemotherapy and local radiation therapy, and aimed to explore potential efficient treatment strategies for this subset of patients.
Patients and Methods
Thirty-seven patients with mNPC (19 newly diagnosed metastatic patients and 18 metastatic cases after definitive chemoradiotherapy) who received the treatment strategies mentioned above were analyzed.
Results
After a median follow-up time of 37 months, the 3-year progression-free survival and overall survival (OS) rates were 47.6% and 87.7%, respectively. The median time to progression was 27.6 months, while the median OS was not reached at time of last follow-up. The most common acute adverse events were hematological and gastrointestinal toxicity, and all were tolerable and curable.
Conclusion
Oral maintenance chemotherapy using S-1/capecitabine in mNPC patients after systemic chemotherapy could yield a superb outcome. Further multicenter prospective clinical trials are warranted.
Introduction
As demonstrated in National Comprehensive Cancer Network (NCCN) and European Society for Medical Oncology (ESMO) guidelines, the management of nasopharyngeal carcinoma (NPC) patients with distant metastases at initial presentation or at the time of disease recurrence is generally palliative, with no standard treatment modality having been clearly established.Citation1,Citation2 Palliative chemotherapy, usually with platinum-based combination regimens, is commonly used as first-line therapy since platinum represents the most effective drug. Other active agents, such as paclitaxel, docetaxel, gemcitabine and capecitabine, can be used as single agents or in combination.Citation1 However, the standard first-line chemotherapeutic regimen is yet to be established, although the use of gemcitabine and cisplatin (known as the GP regimen) was shown to be superior to the traditional regimen with 5-fluorouracil (5-FU) and cisplatin (known as the PF regimen) in a phase III randomized controlled trial.Citation3
Another issue for metastatic NPC (mNPC) is the rationality of radiotherapy for primary and regional tumors, and even for metastatic foci. As reported in many published studies, including ours, besides systemic chemotherapy, the addition of radiotherapy to the primary tumor for newly diagnosed metastatic NPC (synchronous metastatic NPC [smNPC]) and palliative local treatment of the metastatic sites in selected patients would improve survival outcomes, with the 3-year overall survival (OS) indicated to be 33.7–60.7%.Citation4–Citation19 However, since survival outcomes in these situations were still far from satisfactory, how to optimize the treatment strategies and further increase the response rates and survival outcomes are important issues.
Maintenance chemotherapy, which refers to the utilization of regimens with less toxicity after upfront chemotherapy, has been incorporated into treatment paradigms for various cancers, including NPC, aiming to maximize the control of the tumor.Citation20 Among the several anticancer agents that have been tried for mNPC in a maintenance setting, only 5-FU presented promising results.Citation21–Citation24 However, the benefits were to some extent offset by side effects and the inconvenience of continuous intravenous infusion. S-1 and capecitabine are two oral anticancer agents that may act as substitutes for 5-FU, with sufficient efficacy and relatively low toxicity profiles, offering an attractive choice for patients who have been significantly jeopardized by the complications caused by prior courses of palliative chemoradiotherapy.Citation25,Citation26 Published data have proved their efficacy in various solid tumors, including NPC;Citation27–Citation38 however, their utilization as maintenance therapy for mNPC has not been reported. Whether the use of these two oral agents in the maintenance phase could benefit mNPC patients who responded to previous systemic chemotherapy and radiotherapy remains unknown.
Based on the above considerations, we retrospectively analyzed a series of mNPC patients who had received oral maintenance chemotherapy using S-1/capecitabine after systemic chemotherapy with or without local radiation therapy, to explore potential efficient treatment strategies for this subset of patients.
Materials and Methods
Patients
Patients with mNPC, including smNPC patients and cases of metastasis after definitive chemoradiotherapy (metachronous metastatic NPC [mmNPC]), who received maintenance therapy with S-1/capecitabine after systemic chemotherapy at Fujian Cancer Hospital & Fujian Medical University Cancer Hospital, Fuzhou, China, were candidates for this retrospective study. Notably, the use of maintenance chemotherapy was not protocolized at our institution, and only after June 2013 was S-1/capecitabine applied as maintenance therapy in a small number of mNPC patients, at the discretion of the attending physicians. Thus, patients were included in the analysis between June 2013 and December 2017 if they met the following criteria: (1) metastasic foci should be histopathologically proven; otherwise, a diagnosis of distant metastases must be fully discussed and agreed by radiologists and clinicians based on evidence from at least two types of imaging modality, and no prior treatment should have been given after the metastasis diagnosis; (2) for non-bone-only metastatic disease, this should be at least one measurable disease, as assessed by Response Evaluation Criteria In Solid Tumors (RECIST); (3) for patients with smNPC, only those who received the GP regimen as systemic chemotherapy were included in the analysis, while patients with mmNPC who underwent chemotherapy with a non-GP regimen could be collected in our analysis if they had disease progression within 1 year after the GP regimen or in cases of patient refusal; (4) systemic chemotherapy should have completed six cycles; however, patients who had received four or five cycles were permitted to be included in cases of patient refusal, intolerable side effects or physician decision; and (5) there was no previous history of cancers at other sites and no history of second primary cancers. This retrospective study was conducted in compliance with the policy of our institution to protect the private information of enrolled patients, and was approved by the Institutional Review Board of our hospital.
Systemic Chemotherapy and Local Consolidative Treatment
All patients underwent systemic chemotherapy as the basic treatment. For de novo mNPC patients who underwent local radiotherapy to the primary tumor and neck lymph-node region, intensity-modulated radiation therapy (IMRT) was applied according to our institutional protocol. A detailed description of the IMRT planning and dose prescription has been published previously.Citation39 Local consolidative treatment to the metastatic foci was administered according to our institutional protocol: patients with oligometastasis in the lung and lymph nodes in distant parts received radiation therapy, while those with solitary metastasis in the liver were given radiofrequency ablation (RFA). Notably, in our institution, palliative radiotherapy to bone was only used for cases with painful symptoms or weight-bearing bone involvement.
Oral Maintenance Chemotherapy
Oral maintenance chemotherapy was not protocolized in our institution. For patients who received maintenance chemotherapy, S-1 was the first preference in our institution, while capecitabine was used in case of drug shortages in the pharmacy, unacceptable toxicity or patient refusal of S-1. S-1, consisting of tegafur (FT), 5-chloro-2,4-dihydroxypyridine (CDHP) and potassium oxonate (Oxo), was orally administered twice daily after a meal for 2 weeks followed by a 2-week rest, at the following doses based on body surface area: <1.25 m2, 40 mg; <1.50 m2, 50 mg; and >1.50 m2, 60 mg. Capecitabine was administered orally at a dose of 1–1.25 g/m2 twice daily in 4-week cycles, consisting of 2 weeks of treatment followed by a rest period of 2 weeks. Patients commenced oral maintenance chemotherapy 1 month after they finished radiotherapy and systemic chemotherapy. Oral maintenance chemotherapy was scheduled for up to 24 cycles or until confirmed progressive disease, unacceptable adverse events or patient refusal.
Assessments and Follow-Up
Response to treatment was assessed by imaging after every two courses of systemic chemotherapy and at completion of radiotherapy to the primary tumor and neck lymph-node region for all patients, as evaluated by computed tomography (CT) or magnetic resonance imaging (MRI) according to RECIST version 1.1. The evaluation of bone metastasis was based on the response criteria for the practical management of osseous metastases proposed by Hamaoka et al.Citation40 For those who underwent RFA, mRECIST was applied.Citation41,Citation42 All patients achieved a response of at least stable disease (SD) before maintenance chemotherapy. During the maintenance phase, all patients were assessed every 3 months in the first 2 years, every 6 months from year 2 to year 5, and annually thereafter. Toxicities were assessed weekly during radiotherapy and every cycle of chemotherapy, and were graded according to National Cancer Institute Common Terminology Criteria for Adverse Events version 4.0 (CTCAE 4.0).
Statistical Analysis
The primary endpoints were progression-free survival (PFS) (time from the date of diagnosis as mNPC to progression) and OS (time from the date of diagnosis as mNPC to death due to any cause). Descriptive statistics were provided with median and ranges for continuous variables, and frequency and percentages for categorical variables. Survival curves were created with the Kaplan–Meier method and compared between smNPC and mmNPC cohorts with the log-rank test. All statistical analyses were conducted with SPSS version 22.0, and two-tailed P values <0.05 were considered statistically significant.
Results
Patient Characteristics
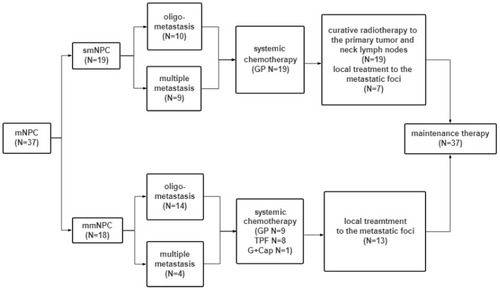
With the criteria mentioned in the “Patients” subsection above, 37 patients were included in this analysis, of whom 19 were diagnosed with smNPC, while 18 were considered as metastasis cases after definitive treatment. All were non-keratinizing carcinoma according to the World Health Organization (WHO) classification, with 34 (91.9%) and three (8.1%) indicated to be undifferentiated and differentiated, respectively. Other details of patients’ characteristics are shown in and .
Table 1 Patient Characteristics
Figure 1 Treatment flowchart.
Abbreviations: mNPC = metastatic nasopharyngeal carcinoma; smNPC = synchronous mNPC; mmNPC = metachronous metastasis NPC GP = gemcitabine and cisplatin; TPF = docetaxel, cisplatin and fluorouracil; G+Cap = gemcitabine plus capecitabine.
The median follow-up time for the whole cohort was 37 months (range 10–71 months). At the time of censoring, 10 patients had completed 2 years of maintenance chemotherapy (24 cycles) and five were still in the maintenance phase, while 14 had discontinued, primarily owing to disease progression (37.8%). Other reasons for discontinuation were intolerable toxicity (four patients, 10.8%), physician decision (one patient, 2.7%) and patient withdrawal (three patients, 8.1%), with the median duration of maintenance chemotherapy found to be 12 cycles (range 2–24 cycles). A total of 19 patients were treated with S-1 alone, eight received capecitabine alone and 10 had switched from S-1 to capecitabine during the phase of maintenance chemotherapy.
Survival
All patients were included in the efficacy and adverse events analyses. No statistically significant differences in OS and PFS were identified between the smNPC and mmNPC patients. At the time of this analysis, a total of 18 patients failed the above-mentioned treatment and were classified as progressive disease; median time to progression (mPFS) was 27.6 months, with the 3-year PFS reported to be 47.6%. It is worth mentioning that of the 18 patients who had disease progression, 16 received non-protocolized salvage treatment, six of whom underwent maintenance chemotherapy again after they responded (at least SD) to salvage treatment; details are presented in . For these six patients, four remained stable at the time of this analysis. The duration of RECIST-defined initial progression to the date of secondary progression for the other two patients was 15 and 24 months, respectively.
Figure 2 Kaplan–Meier curves for (A) OS and (B) PFS in mNPC patients. (C, D) Kaplan–Meier estimates of smNPC and mmNPC patients . (E) Treatment exposure and response.
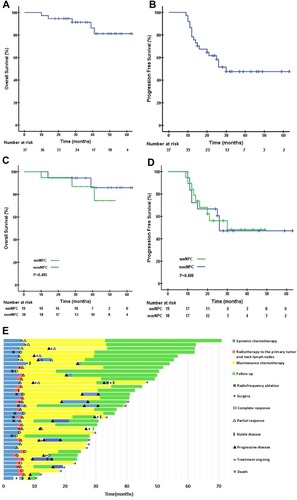
Five patients had died at the time of last follow-up, and all deaths were attributed to disease progression. The 3-year OS was 87.7%, and the median overall survival (mOS) had not been reached at the time of censoring. A noteworthy phenomenon on OS curves was the relatively apparent “tail”, implying that a considerable proportion of patients could potentially experience long-term survival.
Toxicity
As summarized in , systemic treatment was generally well tolerated. The most commonly observed adverse events were grade 1–2 gastrointestinal side effects (33/37, 89.9%), hematological toxicity (19/37, 51.4%) and liver dysfunction (29/37, 78.4%). Grade 3 hematological toxicity and liver dysfunction occurred in 14 and three patients, respectively. Four patients presented with a grade 4 side effect (neutropenia). All events resolved.
Table 2 Summary of Toxicities (N=37)
Toxicities during the maintenance setting, as documented in , were very mild. The most common toxicities were hematological-related events of grade 1–2, with only seven patients (18.8%) developing grade 3 toxicities); one of these patients had both grade 3 neutropenia and gastrointestinal side effects lasting for more than 1 week concurrently. Treatment interruption secondary to adverse events was observed in four patients (13.8%), including three with grade 3 gastrointestinal side effects and one with grade 3 mucositis. No grade 4 adverse effects were recorded and there were no treatment-related deaths. Long-term side effects were not analyzed in this study because of the relatively short survival time.
Discussion
Despite many efforts and attempts made so far, the survival outcomes of mNPC are still disappointing. For such a subgroup of patients with an aggressive prognosis, the optimal treatment strategy remains a subject of debate.Citation43 Here, we report on the efficacy of a novel treatment modality for mNPC and present encouraging results, with substantially longer survival times than in the historical cohorts reported in previous studies.Citation4–Citation19,Citation21–Citation24 With a median follow-up time of 37 months, the 3-year PFS and OS rates were 47.6% and 87.7%, respectively. The mPFS was 27.6 months and the mOS was not reached at the time of last follow-up. Our treatment strategies were generally tolerable, except for four patients who withdrew in the maintenance setting owing to grade 3 gastrointestinal side effects (three cases) and grade 3 mucositis after capecitabine (one case). Our results are of particular importance in that we report a potential promising approach to improve survival in mNPC patients.
Most noteworthy of all is that we exemplified the treatment strategy by introducing oral maintenance chemotherapy immediately after achieving disease control (at least SD) with up-front chemoradiotherapy, with the goal of prolonging a favorable clinical state. Potential rationales for maintenance therapy include increased exposure to effective therapies, decreasing chemotherapy resistance, optimizing the efficacy of chemotherapeutic agents, antiangiogenic effects and altering antitumor immunity.Citation20 In recent years, oral 5-FU substitutes (tegafur-uracil, S-1 and capecitabine) administered on an outpatient basis in the maintenance setting have been proven to have very satisfactory results in NPC.Citation29,Citation32,Citation44 Liu et alCitation32 and Twu et al,Citation44 from Taiwan, indicated that oral tegafur-uracil as adjuvant chemotherapy for 1 year can reduce distant failure and improve overall survival in high-risk NPC patients after curative chemoradiotherapy. A retrospective study of 44 patients with N3 disease also indicated that oral S-1 in the adjuvant setting for about 6 months after cisplatin-based concurrent chemotherapy could yield excellent survival outcomes compared to historical data, with the 3-year OS and distant metastasis-free survival (DMFS) reported to be 86.4% and 84.1%, respectively.Citation29 Although there is no experience of capecitabine being used as maintenance therapy in NPC, published research concluded that oral capecitabine was effective and safe, and was particularly suitable for the management of mNPC.Citation37
The present study is the first to report the use of oral 5-FU substitutes as maintenance therapy in mNPC. Despite the exciting therapeutic effect of this treatment strategy, many issues still puzzle us. Of these, the optimal duration of S-1/capecitabine administration was the most imperative problem to be clarified. As indicated in the studies mentioned above, the reported duration of oral maintenance therapy in NPC varied in different institutions, being either 6 months or 1 year,Citation29,Citation32 while our study demonstrated an even longer duration, with a maximum continuation of 2 years. Although there have been no prospective trials on this issue, a retrospective study on squamous cell carcinoma of the head and neck (SCCHN),Citation31 which included about 10% NPC patients, lends support to our results, as it advocated that a longer period of S-1 administration as an adjuvant setting for SCCHN may be better. It seems that patients with SCCHN should take S-1 as adjuvant chemotherapy for more than 1 year and, if possible, for more than 2 years.Citation31 Prospective clinical trials incorporating molecular biomarkers, such as Epstein–Barr virus (EBV)-DNA, are warranted to illustrate this issue more clearly.
Besides maintenance chemotherapy, sufficient up-front chemotherapy contributes to such excellent survival outcomes. Although the optimal chemotherapy intensity has not been clearly defined in the current NCCN guidelines, available studies have indicated the importance of sufficient chemotherapy for such a subgroup of patients with aggressive disease behavior.Citation6–Citation8,Citation45 In a retrospective study from Tunisia, involving 20 long-term disease-free survivors with mNPC,Citation46 a median of six cycles of chemotherapy was indicated. In China, Wang et alCitation47 and Tian et alCitation48 then proved that receiving six cycles of chemotherapy was associated with significantly better prognosis; however, in Tian’s study, survival between patients with four to five cycles and those with six or more cycles showed no difference, which raises concerns over acquired chemoresistance in NPC patients after six cycles of chemotherapy. Based on these results, the Nasopharyngeal Cancer Committee of China Anti-Cancer Association recommended that, for patients with mNPC, four to six cycles of chemotherapy should be delivered, unless contraindicated.Citation49 As indicated in , most patients in our cohort underwent six cycles of chemotherapy, which was well tolerated except in four patients, for whom systemic chemotherapy had to be discontinued because of patient withdrawal in one patient and physiological reasons in three patients. Of note, all four of these patients had achieved disease control at the time of discontinuation.
The last point that should be noted is that active local treatments were performed in the present series, both on the primary/neck site and at the metastatic foci. For smNPC, the importance of definitive locoregional radiotherapy (LRRT) has been advocated in the current NCCN guidelines and frequently emphasized in published data.Citation4,Citation5,Citation8,Citation12,Citation16–Citation18 However, some investigators have argued that not all de novo metastatic NPC would benefit from LRRT, and that therapeutic advantages could be found only in patients with oligometastases (limited metastatic sites), undetectable EBV-DNA and satisfactory tumor response after palliative chemotherapy,Citation50,Citation51 suggesting that for high-risk patients, the distant lesions were not under control and the post-PCT LRRT might have been insufficient for controlling the distant lesions. Because of technical restrictions at the time, EBV-DNA data were unavailable for reference in this cohort. However, all patients in our series, including seven cases with multiple metastases (all alive at the time of censoring), achieved a response of at least SD after systemic chemotherapy.
Although local treatment to the metastatic foci is not routinely recommended in current clinical guidelines, the concept of using aggressive local therapy for disease control after chemotherapy to eradicate micrometastases is a common theme in oncology. Published data have provided convincing evidence to justify the intervention of metastatic foci in mNPC patients with limited tumor burden, namely oligometastases.Citation7,Citation9,Citation11,Citation13 Local treatment strategies adopted in the current body of NPC literature include surgery, radiotherapy and RFA,Citation6,Citation14,Citation52–Citation55 and the application of stereotactic body radiotherapy (SBRT), which offers non-invasive, yet aggressive local therapy, is especially appealing in oligometastatic disease.Citation15 According to our institutional protocol, only patients with oligo-etastatic disease in lung and liver underwent local treatment to metastatic foci in our study, since for those with widespread dissemination, there is no evidence to support the additional benefit of local therapy to metastatic foci. For such an aggressive subtype of cancer, palliative local intervention was limited to local symptomatic control. It should be noted that palliative radiotherapy to bone was only delivered to those with disease occurring in weight-bearing bone or those with bone pain in our study. This may somewhat negatively impact survival outcomes, as several retrospective studies have indicated significant survival advantages of local radiotherapy in patients with bone-only metastases, regardless of metastatic site and local symptoms.Citation9,Citation10,Citation56
Despite the excellent treatment outcomes of this innovative therapeutic approach, several limitations should be addressed. Firstly, given the retrospective design, all analyses are subject to the clinical influences of selection bias. Secondly, our results were derived from a small sample of patients in a single institution, which may be not representative of the general population of patients from other institutions. Thirdly, the toxicity profile could have been underestimated in a retrospective analysis, although we thoroughly reviewed the medical records. Lastly, the circulating EBV-DNA load and its clearance rate have been shown to predict treatment response and survival in disseminated NPC,Citation50,Citation57,Citation58 which may help in refining case selection and decision making for this treatment modality. However, most patients enrolled in this study had no available EBV-DNA data at the diagnosis of metastases owing to technical restrictions.
Conclusion
Oral maintenance chemotherapy using S-1/capecitabine after systemic chemotherapy and local treatment yielded favorable treatment outcomes and acceptable toxicity profiles in a particular subset of patients with mNPC. Although our results are derived from a single center with a relatively small sample, they may shed new light on the treatment of such a subgroup of patients with aggressive prognosis and provide a reference for the design of future clinical trials, and well-designed multicenter prospective trials are warranted for validation. Future emphasis should be placed on the incorporation of clinical features (e.g. number of metastatic foci/sites and treatment response) and specific biological markers (e.g. EBV-DNA) that reflect individual tumor characteristics into the decision-making algorithm to refine the treatment strategy and maximize the therapeutic gain.
Abbreviations
mNPC, metastatic nasopharyngeal carcinoma; smNPC, synchronous metastatic nasopharyngeal carcinoma; mmNPC, metachronous metastatic nasopharyngeal carcinoma; NCCN, National Comprehensive Cancer Network; ESMO, European Society for Medical Oncology; IMRT, intensity-modulated radiation therapy; OS, overall survival; PFS, progression-free survival; EBV, Epstein–Barr virus.
Ethics Approval and Consent to Participate
The study was approved by the Fujian Cancer Hospital Institutional Review Board.
Availability of Data and Material
The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
- Pfster DG, Spencer S, Adelstein D, et al. NCCN Clinical Practice Guidelines in Oncology. 2019.
- Chan AT, Gregoire V, Lefebvre JL, et al. Nasopharyngeal cancer: EHNS-ESMO-ESTRO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23(Suppl 7):vii83–85. doi:10.1093/annonc/mds26622997460
- Zhang L, Huang Y, Hong S, et al. Gemcitabine plus cisplatin versus fluorouracil plus cisplatin in recurrent or metastatic nasopharyngeal carcinoma: a multicentre, randomised, open-label, Phase 3 trial. Lancet (London, England). 2016;388(10054):1883–1892. doi:10.1016/S0140-6736(16)31388-5
- Yin Z, Zhang X, Wang Y, Wang P, Yuan Z. The combination of systemic therapy and locoregional radiotherapy prolongs survival in newly diagnosed metastatic nasopharyngeal carcinoma patients. Onco Targets Ther. 2017;10:5677–5683. doi:10.2147/OTT.S15003529225474
- Rusthoven CG, Lanning RM, Jones BL, et al. Metastatic nasopharyngeal carcinoma: patterns of care and survival for patients receiving chemotherapy with and without local radiotherapy. Radiother Oncol. 2017;124(1):139–146. doi:10.1016/j.radonc.2017.03.01928433411
- Li W, Bai Y, Wu M, et al. Combined CT-guided radiofrequency ablation with systemic chemotherapy improves the survival for nasopharyngeal carcinoma with oligometastasis in liver: propensity score matching analysis. Oncotarget. 2017;8(32):52132–52141. doi:10.18632/oncotarget.1038328881719
- Zheng W, Zong J, Huang C, et al. Multimodality treatment may improve the survival rate of patients with metastatic nasopharyngeal carcinoma with good performance status. PLoS One. 2016;11(1):e0146771. doi:10.1371/journal.pone.014677126757277
- Tian YH, Zou WH, Xiao WW, et al. Oligometastases in AJCC stage IVc nasopharyngeal carcinoma: a subset with better overall survival. Head Neck. 2016;38(8):1152–1157. doi:10.1002/hed.2434527220062
- Lu T, Guo Q, Cui X, et al. Prognostic evaluation of nasopharyngeal carcinoma with bone-only metastasis after therapy. Yonsei Med J. 2016;57(4):840–845. doi:10.3349/ymj.2016.57.4.84027189275
- Shen L, Dong J, Li S, et al. M1 stage subdivision and treatment outcome of patients with bone-only metastasis of nasopharyngeal carcinoma. Oncologist. 2015;20(3):291–298. doi:10.1634/theoncologist.2014-020625660157
- Chan OS, Ngan RK. Individualized treatment in stage IVC nasopharyngeal carcinoma. Oral Oncol. 2014;50(9):791–797. doi:10.1016/j.oraloncology.2014.01.00424518920
- Chen MY, Jiang R, Guo L, et al. Locoregional radiotherapy in patients with distant metastases of nasopharyngeal carcinoma at diagnosis. Chin J Cancer. 2013;32(11):604–613. doi:10.5732/cjc.013.1014824206918
- Cao X, Han Y, He L, Xiang J, Wen Z. Risk subset of the survival for nasopharyngeal carcinoma patients with bone metastases: who will benefit from combined treatment? Oral Oncol. 2011;47(8):747–752. doi:10.1016/j.oraloncology.2011.05.01021665523
- Ma J, Wen ZS, Lin P, Wang X, Xie FY. The results and prognosis of different treatment modalities for solitary metastatic lung tumor from nasopharyngeal carcinoma: a retrospective study of 105 cases. Chin J Cancer. 2010;29(9):787–795. doi:10.5732/cjc.010.1009820800020
- Niibe Y, Yamashita H, Sekiguchi K, et al. Stereotactic body radiotherapy results for pulmonary oligometastases: a two-institution collaborative investigation. Anticancer Res. 2015;35(9):4903–4908.26254386
- Hu J, Kong L, Gao J, Hu W, Guan X, Lu JJ. Use of radiation therapy in metastatic nasopharyngeal cancer improves survival: a SEER analysis. Sci Rep. 2017;7(1):721. doi:10.1038/s41598-017-00655-128389658
- Verma V, Allen PK, Simone CB 2nd, Gay HA, Lin SH. Addition of definitive radiotherapy to chemotherapy in patients with newly diagnosed metastatic nasopharyngeal cancer. J Natl Compr Cancer Net. 2017;15(11):1383–1391. doi:10.6004/jnccn.2017.7001
- Lin S, Tham IW, Pan J, Han L, Chen Q, Lu JJ. Combined high-dose radiation therapy and systemic chemotherapy improves survival in patients with newly diagnosed metastatic nasopharyngeal cancer. Am J Clin Oncol. 2012;35(5):474–479. doi:10.1097/COC.0b013e31821a945221577086
- Hu SX, He XH, Dong M, et al. Systemic chemotherapy followed by locoregional definitive intensity-modulated radiation therapy yields prolonged survival in nasopharyngeal carcinoma patients with distant metastasis at initial diagnosis. Med Oncol. 2015;32(9):224. doi:10.1007/s12032-015-0663-226219572
- Kasi PM, Grothey A. Chemotherapy maintenance. Cancer J (Sudbury, Mass). 2016;22(3):199–204. doi:10.1097/PPO.0000000000000195
- Hong RL, Sheen TS, Ko JY, Hsu MM, Wang CC, Ting LL. Induction with mitomycin C, doxorubicin, cisplatin and maintenance with weekly 5-fluorouracil, leucovorin for treatment of metastatic nasopharyngeal carcinoma: a Phase II study. Br J Cancer. 1999;80(12):1962–1967. doi:10.1038/sj.bjc.669062710471046
- Leong SS, Wee J, Rajan S, et al. Triplet combination of gemcitabine, paclitaxel, and carboplatin followed by maintenance 5-fluorouracil and folinic acid in patients with metastatic nasopharyngeal carcinoma. Cancer. 2008;113(6):1332–1337. doi:10.1002/cncr.v113:618615622
- You B, Le Tourneau C, Chen EX, et al. A Phase II trial of erlotinib as maintenance treatment after gemcitabine plus platinum-based chemotherapy in patients with recurrent and/or metastatic nasopharyngeal carcinoma. Am J Clin Oncol. 2012;35(3):255–260. doi:10.1097/COC.0b013e31820dbdcc21358293
- Xue C, Huang Y, Huang PY, et al. Phase II study of sorafenib in combination with cisplatin and 5-fluorouracil to treat recurrent or metastatic nasopharyngeal carcinoma. Ann Oncol. 2013;24(4):1055–1061. doi:10.1093/annonc/mds58123172635
- Walko CM, Lindley C. Capecitabine: a review. Clin Ther. 2005;27(1):23–44. doi:10.1016/j.clinthera.2005.01.00515763604
- Miura K, Shirasaka T, Yamaue H, Sasaki I. S-1 as a core anticancer fluoropyrimidine agent. Expert Opin Drug Deliv. 2012;9(3):273–286. doi:10.1517/17425247.2012.65294522235991
- Peng PJ, Lv BJ, Wang ZH, et al. Multi-institutional prospective study of nedaplatin plus S-1 chemotherapy in recurrent and metastatic nasopharyngeal carcinoma patients after failure of platinum-containing regimens. Ther Adv Med Oncol. 2017;9(2):68–74. doi:10.1177/175883401667509928203299
- Wen L, You C, Lu X, Zhang L. Phase II trial of concurrent chemoradiotherapy with S-1 versus weekly cisplatin for locoregionally advanced nasopharyngeal carcinoma. Mol Clin Oncol. 2015;3(3):687–691. doi:10.3892/mco.2015.52926137288
- Zhang S, Zhou L, Huang X, Lin S. A retrospective study of concurrent chemoradiotherapy plus S-1 adjuvant chemotherapy on curative effect for treatment of patients with N3 stage nasopharyngeal carcinoma. Cancer Manag Res. 2018;10:1705–1711. doi:10.2147/CMAR.S16580429983590
- Tsukahara K, Kubota A, Hasegawa Y, et al. Randomized phase III trial of adjuvant chemotherapy with S-1 after curative treatment in patients with squamous-cell carcinoma of the head and neck (ACTS-HNC). PLoS One. 2015;10(2):e0116965. doi:10.1371/journal.pone.011696525671770
- Hirai M, Orita Y, Takao S, et al. How long should we continue S-1 as adjuvant chemotherapy for squamous cell carcinoma of the head and neck? Acta Otolaryngol. 2015;135(10):1079–1085. doi:10.3109/00016489.2015.104966426004393
- Liu YC, Wang WY, Twu CW, et al. Prognostic impact of adjuvant chemotherapy in high-risk nasopharyngeal carcinoma patients. Oral Oncol. 2017;64:15–21. doi:10.1016/j.oraloncology.2016.11.00828024719
- Kim HS, Kim HR, Kim GM, et al. The efficacy and toxicity of S-1 and cisplatin as first-line chemotherapy in recurrent or metastatic head and neck squamous cell carcinoma. Cancer Chemother Pharmacol. 2012;70(4):539–546. doi:10.1007/s00280-012-1933-822868340
- Luo HY, Li YH, Wang W, et al. Single-agent capecitabine as maintenance therapy after induction of XELOX (or FOLFOX) in first-line treatment of metastatic colorectal cancer: randomized clinical trial of efficacy and safety. Ann Oncol. 2016;27(6):1074–1081. doi:10.1093/annonc/mdw10126940686
- Suzuki S, Karayama M, Inui N, et al. Continuation maintenance therapy with S-1 in chemotherapy-naive patients with advanced squamous cell lung cancer. Invest New Drugs. 2016;34(4):490–496. doi:10.1007/s10637-016-0365-427279143
- Peng PJ, Cheng H, Ou XQ, et al. Safety and efficacy of S-1 chemotherapy in recurrent and metastatic nasopharyngeal carcinoma patients after failure of platinum-based chemotherapy: multi-institutional retrospective analysis. Drug Des Devel Ther. 2014;8:1083–1087. doi:10.2147/DDDT.S67592
- Chua DT, Sham JS, Au GK. A phase II study of capecitabine in patients with recurrent and metastatic nasopharyngeal carcinoma pretreated with platinum-based chemotherapy. Oral Oncol. 2003;39(4):361–366. doi:10.1016/S1368-8375(02)00120-312676255
- Surmeli ZG, Varol U, Cakar B, et al. Capecitabine maintenance therapy following docetaxel/capecitabine combination treatment in patients with metastatic breast cancer. Oncol Lett. 2015;10(4):2598–2602. doi:10.3892/ol.2015.354626622896
- Lin S, Pan J, Han L, Zhang X, Liao X, Lu JJ. Nasopharyngeal carcinoma treated with reduced-volume intensity-modulated radiation therapy: report on the 3-year outcome of a prospective series. Int J Radiat Oncol Biol Phys. 2009;75(4):1071–1078. doi:10.1016/j.ijrobp.2008.12.01519362784
- Hamaoka T, Madewell JE, Podoloff DA, Hortobagyi GN, Ueno NT. Bone imaging in metastatic breast cancer. J Clin Oncol. 2004;22(14):2942–2953. doi:10.1200/JCO.2004.08.18115254062
- Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010;30(1):52–60. doi:10.1055/s-0030-124713220175033
- Arora A, Kumar A. Treatment response evaluation and follow-up in hepatocellular carcinoma. J Clin Exp Hepatol. 2014;4(Suppl 3):S126–129. doi:10.1016/j.jceh.2014.05.00525755604
- Chen YP, Chan ATC, Le QT, Blanchard P, Sun Y, Ma J. Nasopharyngeal carcinoma. Lancet (London, England). 2019.
- Twu CW, Wang WY, Chen CC, et al. Metronomic adjuvant chemotherapy improves treatment outcome in nasopharyngeal carcinoma patients with postradiation persistently detectable plasma Epstein-Barr virus deoxyribonucleic acid. Int J Radiat Oncol Biol Phys. 2014;89(1):21–29. doi:10.1016/j.ijrobp.2014.01.05224725686
- Jin Y, Shi YX, Cai XY, et al. Erratum to: comparison of five cisplatin-based regimens frequently used as the first-line protocols in metastatic nasopharyngeal carcinoma. J Cancer Res Clin Oncol. 2015;141(4):767. doi:10.1007/s00432-015-1926-125672952
- Fandi A, Bachouchi M, Azli N, et al. Long-term disease-free survivors in metastatic undifferentiated carcinoma of nasopharyngeal type. J Clin Oncol. 2000;18(6):1324–1330. doi:10.1200/JCO.2000.18.6.132410715304
- Wang CT, Cao KJ, Li Y, Xie GF, Huang PY. Prognosis analysis of nasopharyngeal carcinoma patients with distant metastasis. Ai Zheng. 2007;26(2):212–215.17298756
- Tian Y-M, Zeng L, Wang F-H, et al. Prognostic factors in nasopharyngeal carcinoma with synchronous liver metastasis: a retrospective study for the management of treatment. Rad Oncol. 2013;8(1):272. doi:10.1186/1748-717X-8-272
- Committee of Nasopharyngeal Cancer of Chinese Anti-Cancer Association CX, Jingao L, et al. Expert consensus on the treatment of metastasis nasopharyngeal carcinoma. Chin J Rad Oncol. 2018;27(1):23–28.
- Sun XS, Liu LT, Liu SL, et al. Identifying optimal candidates for local treatment of the primary tumor among patients with de novo metastatic nasopharyngeal carcinoma: a retrospective cohort study based on Epstein-Barr virus DNA level and tumor response to palliative chemotherapy. BMC Cancer. 2019;19(1):92. doi:10.1186/s12885-019-5281-530665378
- Zou X, You R, Liu H, et al. Establishment and validation of M1 stage subdivisions for de novo metastatic nasopharyngeal carcinoma to better predict prognosis and guide treatment. Eur J Cancer (Oxford, England: 1990). 2017;77:117–126. doi:10.1016/j.ejca.2017.02.029
- Pan C, Wu P, Yu J, et al. CT-guided radiofrequency ablation prolonged metastatic survival in patients with liver metastases from nasopharyngeal carcinoma. Int J Hyperther. 2011;27(6):549–554. doi:10.3109/02656736.2011.593019
- Jin Y, Cai YC, Cao Y, et al. Radiofrequency ablation combined with systemic chemotherapy in nasopharyngeal carcinoma liver metastases improves response to treatment and survival outcomes. J Surg Oncol. 2012;106(3):322–326. doi:10.1002/jso.2303422271524
- Cheng LC, Sham JS, Chiu CS, Fu KH, Lee JW, Mok CK. Surgical resection of pulmonary metastases from nasopharyngeal carcinoma. Aust N Z J Surg. 1996;66(2):71–73. doi:10.1111/j.1445-2197.1996.tb01114.x8602817
- Pan CC, Wu PH, Yu JR, et al. Comparative survival analysis in patients with pulmonary metastases from nasopharyngeal carcinoma treated with radiofrequency ablation. Eur J Radiol. 2012;81(4):e473–477. doi:10.1016/j.ejrad.2011.05.03721700408
- Sun XS, Liang YJ, Liu SL, et al. Subdivision of nasopharyngeal carcinoma patients with bone-only metastasis at diagnosis for prediction of survival and treatment guidance. Cancer Res Treat. 2019;51:1259–1268. doi:10.4143/crt.2018.65230653745
- Wang WY, Twu CW, Chen HH, et al. Plasma EBV DNA clearance rate as a novel prognostic marker for metastatic/recurrent nasopharyngeal carcinoma. Clin Cancer Res. 2010;16(3):1016–1024. doi:10.1158/1078-0432.CCR-09-279620103659
- An X, Wang FH, Ding PR, et al. Plasma Epstein-Barr virus DNA level strongly predicts survival in metastatic/recurrent nasopharyngeal carcinoma treated with palliative chemotherapy. Cancer. 2011;117(16):3750–3757. doi:10.1002/cncr.2593221319149
