Abstract
Background
To investigate the effectiveness and cost minimization of comprehensive pulmonary rehabilitation (CPR) in lung cancer patients who underwent surgery.
Patients and Methods
A retrospective observational study based on medical records was conducted, with 2410 lung cancer patients who underwent an operation with/without CPR during the peri-operative period. Variables including clinical characteristics, length of stay (LOS), postoperative pulmonary complications (PPCs), and hospitalization expenses were compared between the intervention group (IG) and control group (CG). The CPR regimen consists of inspiratory muscle training (IMT), aerobic endurance training, and pharmacotherapy.
Results
Propensity score matching analysis was performed between two groups, and the ratio of matched patients was 1:4. Finally, 205 cases of IG and 820 cases of CG in the matched cohort of our study were identified. The length of postoperative hospital stay [median: 5 interquartile (4–7) vs 7 (4–8) days, P < 0.001] and drug expenses [7146 (5411–8987) vs 8253 (6048–11,483) ¥, P < 0.001] in the IG were lower compared with the CG. Additionally, the overall incidence of PPCs in the IG was reduced compared with the CG (26.8% vs 36.7%, P = 0.008), including pneumonia (10.7% vs 16.8%, P = 0.035) and atelectasis (8.8% vs 14.0%, P = 0.046). Multivariable analysis showed that CPR intervention (OR = 0.655, 95% CI: 0.430–0.865, P = 0.006), age ≥70 yr (OR = 1.919, 95% CI: 1.342–2.744, P < 0.001), smoking (OR = 2.048, 95% CI: 1.552–2.704, P < 0.001) and COPD (OR = 1.158, 95% CI: 1.160–2.152, P = 0.004) were related to PPCs.
Conclusion
The retrospective cohort study revealed a lower PPC rate and the shorter postoperative length of stay in the patients receiving CPR, demonstrating the clinical value of CRP as an effective strategy for surgical lung cancer patients with risk factors.
Introduction
Lung cancer has always been one of the most health-threatening and fatal diseases in China, ranking the highest in morbidity and mortality among malignant diseases and causing unbearable social and economic burden globally. Among various treatments for lung cancer, surgery remains the primary or optimal approach, especially for limited stage patients.Citation1 Due to reduced lung function and sequential postoperative pulmonary complications (PPCs), extended in-hospital stay and significant cost after surgeries are frequently required.Citation2–Citation4 Effective comprehensive preoperative prevention, including pulmonary rehabilitation or drug intervention for non-small cell lung cancer (NSCLC) patients, may reduce the risk of PPCs and effectively achieve optimistic clinical outcomes.Citation5,Citation6 Given the high incidence of cardiopulmonary comorbidities in lung cancer patients, these individuals are particularly at high risk of PPCs. In the Chinese expert consensus statement on multi-disciplinary peri-operative airway management (2016 version),Citation7 comprehensive pulmonary rehabilitation (CPR), including physical exercise and pharmacotherapy (inhaled corticosteroid (ICS) and bronchodilator), was recommended for patients during peri-operation because it plays a vital role in enhancing cardiopulmonary capacity and subsequently decreasing PPC rates.Citation8–Citation10
Clinical experiments have demonstrated the effectiveness and feasibility of pulmonary rehabilitation (PR) as a cost-effective intervention for preoperative conditioning, especially for patients with high risks of PPCs due to limited lung function.Citation11,Citation12 However, the appropriate rehabilitation regimen, duration, and intensity remain unclear. Only a few small randomized controlled trials (RCT) confirmed that CPR helps to shorten the hospitalization time and reduce the PPC rates in lung cancer patients; thus, evidence on the feasibility and effectiveness of CPR is limited.Citation13–Citation15 Furthermore, CPR outcomes in Chinese surgical lung cancer patients remain unknown and need to be explored in the real world. Our study team focused on studies concerning the effectiveness of CPR combined with physical exercise and pharmacotherapy (ICS and bronchodilators) for lung cancer patients in the peri-operation period, seeking to provide substantial evidence of the positive effect of CPR in this population.
Patients and Methods
Study Design
This is a retrospective cohort study based on medical records to describe recovery outcomes in surgical lung cancer patients with/without comprehensive pulmonary rehabilitation during the peri-operative period. Data were extracted from the hospital information system or paper medical record.
Patient Selection
Lung cancer patients who underwent surgery at the Department of Thoracic Surgery, West China Hospital from January 1, 2012 to December 31, 2017 were collected. Each subject should meet all of the inclusion criteria and none of the exclusion criteria for this study. The inclusion criteria included the following: (1) aged between 40 and 85 years old; (2) patients with physician-diagnosed primary NSCLC who underwent single lobectomy as noted in the medical record; (3) patients underwent comprehensive pulmonary rehabilitation (CPR group) or no physical or drug rehabilitation (non-CPR group); (4) patients underwent video-assisted thoracoscopic surgery (VATS) or thoracotomy. The exclusion criteria were as follows: (1) patients with intraoperative haemorrhage greater than 1000 mL; (2) patients with conversion to thoracotomy; (3) patients who underwent neoadjuvant therapy.
Patients enrolled in the rehabilitation program need to meet at least one of the following criterion: age > 70 yr, a ≥ 20 pack-year smoking history, chronic obstructive pulmonary disease (COPD) or airway hyperresponsiveness, and postoperative predicted percentage forced expiratory volume in 1 s (ppoFEV1%) < 60%. The exclusion criteria included refusal to participate or any contraindication to adverse events, such as cardio-cerebral vascular accident within the past year, haemoptysis, unstable chest pain, arrhythmia or musculoskeletal disorders. All patients in the intervention group had to admit at least 7 days before surgery. Lung cancer was pathologically staged according to the International Union Against Cancer staging system (8th edition).Citation16
Intervention
Inspiratory Muscles Training
Inspiratory muscle training (IMT) was conducted in the hospital ward before operation and included the following: (1) Inspiration training: the Voldyne 2500 device (Sherwood Medical Supplies, St Louis, MO, USA) was used for inspiratory muscle exercising. The physiotherapist instructed patients to breathe out naturally, exhaling as much air from lungs as possible, and then take a deep, slow breath through the mouthpiece until the marked goal is reached or the patient cannot inhale further. Then, the patient was instructed to hold his/her breath for a short time and exhale slowly (3 times a day, 20 minutes each time for 7 days). (2) Abdominal breathing training: the patients slowly inhaled the maximum lung volume through the nose and held the breath for several seconds. The patients then tighten the abdominal muscles and slowly exhales through the mouth to strengthen the diaphragm muscles (3 times a day, 10–15 minutes each time for 7 days).
Aerobic Endurance Training
In the intervention group, patients underwent preoperative training using the Nu-Step device (NuStep, Inc., Ann Arbor, Michigan) in the rehabilitation department of the hospital. They could adjust the device resistance range based on their physical strength, and then the resistance of the device was gradually increased while the heart rate was maintained at 120–160 beats/min. The training must be stopped if patients experienced any discomforts, such as dizziness, dyspnoea, or cardiopalmus. Patients could take a break until their physical condition allowed completion of the remainder of the training. This training lasted 30 minutes daily for 7 days.
Pharmacotherapy
Pharmacotherapy was achieved using corticosteroid and bronchodilator aerosol inhalation during peri-operation in the hospital ward. The usage and dosage were as follows: 2 mg nebulized budesonide (Pulmicort Respules) and 5 mg terbutaline (Bricanyl Respules) twice daily. Duration: 5 to 7 days before the operation and at least 3 days after the operation.
Outcome Assessment
The primary endpoint was the PPC rates of the two groups. The secondary endpoints included the length of hospitalization after operation (=discharge date – operation date + 1) and hospitalization expense.
Criteria of PPCs
The following PPC criteria were established according to the STS/ESTS (2015) complication definitions and were experienced by the patients:Citation17 (1) air leak >5 days; (2) bronchoscopy for atelectasis; (3) pneumonia; (4) adult respiratory distress syndrome (ARDS); (5) bronchopleural fistula; (6) pulmonary embolism (7) ventilator support > 48 hours; (8) reintubation; (9) empyema; and (10) unexpected admission to the intensive care unit (ICU).
Statistical Analysis
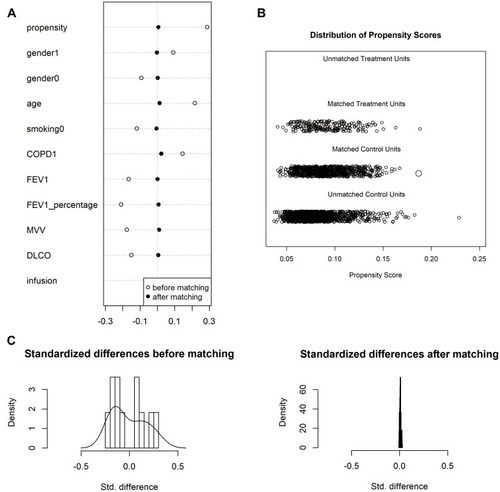
Descriptive statistics of primary and secondary outcomes, demographics, and clinical characteristics are presented for the intervention group and control group. Because the patient characteristics and the disease status between groups at baseline are imbalanced, propensity score matching (PSM) with a 1:4 ratio was performed to match the cases in two groups using the nearest matching method with a caliper width equal to 0.2. We used the standardized difference of each covariate to assess the balance of covariate before and after PSM. Standardized difference < 0.1 of the absolute value was considered to be a relatively small imbalance.Citation18 Multivariable logistic regression was used to determine propensity scores for each patient based on age, gender, FEV1, FEV1%, DLco%, MVV%, intraoperative infusion, smoking status, and COPD. Continuous variables were presented as the mean with standard deviation (mean ± SD). Data not obeying normal distribution were presented as the median and interquartile range (IQR), and categorical variables were presented as numbers with percentages. In univariate analyses, continuous variables were compared by t-test or Mann–Whitney U-test wherever applicable, and categorical variables were analysed by Pearson’s chi-squared or Fisher’s exact test. Logistic regression was performed to identify independent risk factors of PPCs. All results were considered significant at a P-value <0.05. Statistical analyses were performed using SPSS software v.22.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
Baseline and Clinical Characteristics
A total of 2410 patients met eligibility criteria. In total, 205 patients were included in the intervention group (IG), and 2205 patients were included in as the control group (CG). Groups were established based on whether patients underwent comprehensive pulmonary rehabilitation. Patients in the IG were older compared with the CG (60.13 ± 9.23 vs 57.98 ± 10.06 yr, P = 0.003). Lower FEV1 value (2.43 ± 0.61 vs 2.55 ± 0.64 L, P = 0.019), FEV1% (96.97 ± 18.26 vs 101.03 ± 18.82, P = 0.003), DLco% (93.84 ± 16.96 vs 96.78 ± 17.21, P = 0.019) and MVV% (97.83 ± 20.42 vs 101.71 ± 20.78) were found in the IG. There were more patients with COPD in the IG (25.4% vs 18.7%, P = 0.021) compared with the CG.
We identified 205 cases of IG and 820 cases of CG for our study based on PSM analysis. The baseline characteristics of the two groups were balanced, as shown in and .
Table 1 Baseline and Clinical Characteristics Between Two Groups Before and After Propensity Score Matching
Peri-Operative Outcomes
Before PSM, the IG presented a shorter postoperative hospital stay [5 (4–7) vs 6 (4–8) days, P < 0.001] and lower drug expenses [7146 (5411–8987) vs.7577 (5567–9880) ¥, P = 0.045] compared with the CG. Concerning PPCs, no significant difference was observed between the two groups.
In the matched cohort, the length of postoperative hospital stay [5 (4–7) vs 7 (4–8) days, P < 0.001] and drug expenses [7146 (5411–8987) vs.8253 (6048–11,483) ¥, P < 0.001] in the IG were also reduced compared with the CG. IG patients spent an extra ¥ 983.25 on the rehabilitation regimen. Fortunately, the cost of rehabilitation did not increase the total hospitalization expenditure. Additionally, the overall incidence of PPCs in the IG was lower compared with the CG (26.8% vs.36.7%, P = 0.008). Furthermore, the incidences of pneumonia (10.7% vs 16.8%, P = 0.035) and atelectasis (8.8% vs 14.0%, P = 0.025) in the IG were significantly reduced compared with the CG. Details are provided in .
Table 2 The Outcomes and Postoperative Pulmonary Complications Rate Between Two Groups Before and After Propensity Score Matching
Risks of PPCs After PSM
Matched patients were divided into the PPCs group (n = 356) and non-PPCs group (n = 669) based on whether patients experienced pulmonary complications. In univariate analysis, the percentages of age > 70 yr, FEV1% < 70%, DLco% < 70%, MVV% < 70%, male patients, smokers, and COPD were significantly increased in the PPCs group. Additionally, the proportion of patients performing CPR in the PPCs group was lower than that in the non-PPCs group (). The above variables were related to the risk of PPCs.
Table 3 Clinical Characteristics Between PPCs Group and Non-PPCs Group After Propensity Score Matching
Logistic regression analysis was subsequently used to identify variables that independently correlate with PPCs. Multivariable analysis showed that CPR intervention (OR = 0.655, 95% CI: 0.430–0.865, P = 0.006) was a protective factor, and age ≥ 70 yr (OR = 1.919, 95% CI: 1.342–2.744, P < 0.001), smoking (OR = 2.048, 95% CI: 1.552–2.704, P < 0.001) and COPD (OR = 1.158, 95% CI: 1.160–2.152, P = 0.004) were independent risk factors of PPCs ().
Table 4 Multivariable Analysis of Risk to PPCs After Propensity Score Matching
Discussion
This large sample size retrospective study investigated the effectiveness and cost-efficiency of CPR in lung cancer patients who underwent surgery. We found that CPR reduces the incidence of PPCs, including pneumonia and atelectasis. Meanwhile, patients who performed the CPR regimen experienced a shorter length of postoperative hospital stay without an increase in hospitalization costs.
Over recent decades, numerous studies have demonstrated that pulmonary rehabilitation is beneficial for enhancing the functional and physiological capacity of patients even if the regimens differ in intensity, duration, and exercise plans.Citation19–Citation23 Emerging evidence suggest that prehabilitation plays a crucial role in decreasing the risk of postoperative complications and the length of stay.Citation22,Citation24–Citation26 Our preoperative rehabilitation was performed in the hospital and the duration was seven days, which was shorter than most other rehabilitation regimens.Citation27 In China, underdeveloped community health systems and regional imbalances make family training inappropriate for community institutions. In addition, an in-patient or physiotherapist-guided session will optimize technology and safety. Recent trials revealed smaller improvements in physical capacity with home-based exercise compared with supervised hospital rehabilitation. Nolan et al found that greater mean improvements in shutter walk test with hospital pulmonary rehabilitation compared with home-based exercise (59 m vs 29 m, P = 0.003).Citation28 Moreover, Edbrooke et al reported that home-based rehabilitation demonstrated no statistically significant change in physical function of inoperable lung cancer patients.Citation29 Home-based participants were likely exercising at lower adherence and intensity. As a result, the hospital is an ideal location for CPR. Generally, an exercise program initiative should last for two weeks or more significantly improve functional capacity.Citation25,Citation30 However, for patients with suspected lung cancer facing a potentially curative resection, the long-term regimen seems unacceptable for some patients. Lung cancer patients usually spend approximately one week in the hospital in China for surgery preparations, including CT scans, bone imaging, bronchoscopy, and other surgery-related examinations. Hence, we employed a pragmatic approach in which the duration and intensity of the training fit with preoperative waiting time. The one-week high-intensity preoperative program was feasible and effective. The program not only enhanced patient compliance but also did not increase the in-hospital stay. It is noteworthy that outpatient preoperative rehabilitation seems to be more recommended than inpatient rehabilitation in areas with the developed health system. Outpatient pulmonary rehabilitation not only ensures program fidelity but also shortens the length of stay and reduces the cost of hospitalization. The rehabilitation regimen should be designed flexibly to adapt to the medical policies of different regions, and follow the principle of maximizing the benefits of patients.
Another thing that should be noticed is the use of aerosol therapy with glucocorticoids and bronchodilators during the peri-operative period of CPR. COPD presented concomitantly in 73% of men and 53% of women with newly diagnosed primary lung cancer.Citation31 In addition, one-lung ventilation during thoracic surgery, inflammation can be induced by oxidative stress-related damage, alveolar collapse and reopening, surgical procedure and over-expansion of alveolar vessel in ventilated lung.Citation32–Citation34 Budesonide and terbutaline can alleviate airway spasm, eliminate odema, improve tolerance to tracheal intubation, inhibit the release of inflammatory factors, and reduce respiratory secretions, these drugs are widely used to treat COPD, asthma, and many other respiratory diseases.Citation35–Citation37 Aerosolized drugs play a role in moistening the bronchial mucosa, relieving bronchospasm, reducing the viscosity of the sputum, and easily expelling the sputum.Citation38 We hypothesized that inhaled budesonide and terbutaline might mitigate the inflammatory response and improve pulmonary protective effects in patients undergoing thoracic surgery.
PPCs are vital elements that negatively affects the peri-operative morbidity and mortality rates. Over recent decades, numerous studies have investigated the relationship between pulmonary rehabilitation and PPCs, and most of them report the positive consequence of pulmonary rehabilitation on surgical patients with lung cancer, including a decrease in PPC rates.Citation39 However, controversy remains as some studies hold the view that pulmonary rehabilitation fails to reduce the incidence of PPCs.Citation12 Of note, patient heterogeneity, a variety of PR approaches, and a lack of consistent criteria for PPCs make it difficult to draw firm conclusions. Our results revealed a significantly reduced incidence of PPCs in the IG compared with the matched CG. Moreover, the outcome of the sub-items of PPCs showed that the diminishing rate of pneumonia and atelectasis that occurred in the patients experiencing CPR. Multivariable analysis of risk factors of PPCs also indicated that CPR intervention is an independent protective factor of PPCs. Two potential reasons explain these results. First, the high-intensity IMT combined aerobic endurance training enhanced the physical fitness and cardiorespiratory capacity, sequentially enabling patients to withstand surgical stress and aiding in recovery. Second, peri-operative use of glucocorticoids and bronchodilators provided pulmonary protective effects, which ameliorated lung injury, expanded the bronchus, and reduced inflammatory factors and secretions. The other two independent risks of PPCs included smoking status and COPD, which were consistent with other study findings.Citation40
This research also has some limitations. First, it is a retrospective cohort study. The nature of this study may lead to the unmeasured or residual confounding between the two groups, even though we performed PSM analysis that could help to reduce the bias. Another issue that should be noticed is the potential residual confounders, including smoking status and COPD, which may confound the results. It is better to stratify them according to smoking index and COPD severity in baseline data and regression analysis, but unfortunately, due to the limited data we obtained, further stratified analysis concerning smoking status or COPD is unable to be completed. Given potentially poor records of some clinical data and the subjective bias of recorders, our statistical complications rate may be lower than the real situation. Hence, our study cannot reflect real-world information. Second, the study subjects were recruited from a single regional medical center, and further research needs to confirm whether our findings are universally applicable. Third, more variables, including quality of life, should be included in the analysis to better assess the effectiveness of the CPR regimen.
Conclusions
In this study, we found that postoperative length of stay (LOS) and drug expenses were reduced in the IG compared with the CG both before and after patient matching. PPCs were regarded as the leading cause of increased hospitalization expenses and LOS. These economic findings indicated that this rehabilitation regimen was a cost-effective intervention for lung cancer patients with risk factors. Possible explanations for our results may attribute to a lower rate of complications and better recovery after surgery in the CPR group, thus reducing medical interference.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethics Approval and Informed Consent
This study was approved by the Ethics Committee of West China Hospital, and registered in the Chinese Clinical Trial Registry (ChiCTR1800020097). We declared that the study adhered to the tenets of the Declaration of Helsinki. All patient data accessed complied with national, regional, and local regulations with respect to privacy and data protection. The investigators could collect data after Informed Consent Waiver was written approved by Ethics Committee of West China Hospital, because of the retrospective nature of the study.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed on the journal to which the article will be submitted; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- Boffa DJ, Allen MS, Grab JD, et al. Data from The Society of Thoracic Surgeons General Thoracic Surgery database: the surgical management of primary lung tumors. J Thorac Cardiovasc Surg. 2008;135(2):247–254. doi:10.1016/j.jtcvs.2007.07.06018242243
- Stéphan F, Boucheseiche S, Hollande J, et al. Pulmonary complications following lung resection: a comprehensive analysis of incidence and possible risk factors. Chest. 2000;118(5):1263–1270. doi:10.1378/chest.118.5.126311083673
- Ha D, Choi H, Zell K, et al. Association of impaired heart rate recovery with cardiopulmonary complications after lung cancer resection surgery. J Thorac Cardiovasc Surg. 2015;149(4):1168–73.e3. doi:10.1016/j.jtcvs.2014.11.03725583106
- Zhang J, Zhao T, Long S, Liu X, Yu H. Risk factors for postoperative infection in Chinese lung cancer patients: a meta-analysis. J Evid Based Med. 2017;10(4):255–262. doi:10.1111/jebm.1227628884946
- Li S, Zhou K, Che G, et al. Enhanced recovery programs in lung cancer surgery: systematic review and meta-analysis of randomized controlled trials. Cancer Manag Res. 2017;9:657–670. doi:10.2147/CMAR.S15050029180901
- Fiore JF, Bejjani J, Conrad K, et al. Systematic review of the influence of enhanced recovery pathways in elective lung resection. J Thorac Cardiovasc Surg. 2016;151(3):708–715.e6. doi:10.1016/j.jtcvs.2015.09.11226553460
- Zhi XY, He JX, Liu LX, Jiang GN, Che GW. Chinese consensus statement on multi-disciplinary perioperative airway management (2016 version). Chin J Clin Thorac Cardiovasc Surg. 2016;23:641–645.
- Gao W, Li N, Jin ZH, et al. Effect of preoperative inhaled budesonide on pulmonary injury after cardiopulmonary bypass: a randomized pilot study. J Thorac Cardiovasc Surg. 2019;157(1):272–284. doi:10.1016/j.jtcvs.2018.09.01730396739
- Jin Z, Chun Suen K, Ma D. Perioperative “remote” acute lung injury: recent update. J Biomed Res. 2017;31(3):197–212. doi:10.7555/JBR.31.2016005328808222
- Takegahara K, Usuda J, Inoue T, et al. Preoperative management using inhalation therapy for pulmonary complications in lung cancer patients with chronic obstructive pulmonary disease. Gen Thorac Cardiovasc Surg. 2017;65(7):388–391. doi:10.1007/s11748-017-0761-528281043
- Zhou K, Su J, Lai Y, Li P, Li S, Che G. Short-term inpatient-based high-intensive pulmonary rehabilitation for lung cancer patients: is it feasible and effective? J Thorac Dis. 2017;9(11):4486–4493. doi:10.21037/jtd.2017.10.10529268518
- Bradley A, Marshall A, Stonehewer L, et al. Pulmonary rehabilitation programme for patients undergoing curative lung cancer surgery. Eur J Cardiothorac Surg. 2013;44(4):e266–e271. doi:10.1093/ejcts/ezt38123959742
- Stigt JA, Uil SM, van Riesen SJ, et al. A randomized controlled trial of postthoracotomy pulmonary rehabilitation in patients with resectable lung cancer. J Thorac Oncol. 2013;8(2):214–221. doi:10.1097/JTO.0b013e318279d52a23238118
- Divisi D, Di Francesco C, Di Leonardo G, et al. Preoperative pulmonary rehabilitation in patients with lung cancer and chronic obstructive pulmonary disease. Eur J Cardiothorac Surg. 2013;43(2):293–296. doi:10.1093/ejcts/ezs25722588033
- Lai Y, Huang J, Yang M, et al. Seven-day intensive preoperative rehabilitation for elderly patients with lung cancer: a randomized controlled trial. J Surg Res. 2017;209:30–36. doi:10.1016/j.jss.2016.09.03328032568
- Goldstraw P, Chansky K, Crowley J, et al. The IASLC lung cancer staging project: proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J Thorac Oncol. 2016;11(1):39–51. doi:10.1016/j.jtho.2015.09.00926762738
- Seder CW, Salati M, Kozower BD, et al. Variation in pulmonary resection practices between The Society of Thoracic Surgeons and the European Society of Thoracic Surgeons General Thoracic Surgery databases. Ann Thorac Surg. 2016;101(6):2077‐2084. doi:10.1016/j.athoracsur.2015.12.073
- Austin PC. Assessing the performance of the generalized propensity score for estimating the effect of quantitative or continuous exposures on binary outcomes. Stat Med. 2018;37(11):1874–1894. doi:10.1002/sim.761529508424
- Edvardsen E, Skjønsberg OH, Holme I, et al. High-intensity training following lung cancer surgery: a randomised controlled trial. Thorax. 2015;70(3):244‐250. doi:10.1136/thoraxjnl-2014-205944
- Rivas-Perez H, Nana-Sinkam P. Integrating pulmonary rehabilitation into the multidisciplinary management of lung cancer: a review. Respir Med. 2015;109(4):437–442. doi:10.1016/j.rmed.2015.01.00125641113
- Bobbio A, Chetta A, Ampollini L, et al. Preoperative pulmonary rehabilitation in patients undergoing lung resection for non-small cell lung cancer. Eur J Cardiothorac Surg. 2008;33(1):95–98. doi:10.1016/j.ejcts.2007.10.00318006327
- Pehlivan E, Turna A, Gurses A, et al. The effects of preoperative short-term intense physical therapy in lung cancer patients: a randomized controlled trial. Ann Thorac Cardiovasc Surg. 2011;17(5):461–468. doi:10.5761/atcs.oa.11.0166321881371
- Stefanelli F, Meoli I, Cobuccio R, et al. High-intensity training and cardiopulmonary exercise testing in patients with chronic obstructive pulmonary disease and non-small-cell lung cancer undergoing lobectomy. Eur J Cardiothorac Surg. 2013;44(4):e260–e265. doi:10.1093/ejcts/ezt37523892298
- Agostini P, Naidu B, Cieslik H, et al. Effectiveness of incentive spirometry in patients following thoracotomy and lung resection including those at high risk for developing pulmonary complications. Thorax. 2013;68(6):580–585. doi:10.1136/thoraxjnl-2012-20278523429831
- Benzo R, Wigle D, Novotny P, et al. Preoperative pulmonary rehabilitation before lung cancer resection: results from two randomized studies. Lung Cancer. 2011;74(3):441–445. doi:10.1016/j.lungcan.2011.05.01121663994
- Huang J, Lai Y, Zhou X, et al. Short-term high-intensity rehabilitation in radically treated lung cancer: a three-armed randomized controlled trial. J Thorac Dis. 2017;9(7):1919–1929. doi:10.21037/jtd.2017.06.1528839990
- Lai Y, Wang X, Zhou K, et al. Impact of one-week preoperative physical training on clinical outcomes of surgical lung cancer patients with limited lung function: a randomized trial. Ann Transl Med. 2019;7(20):544. doi:10.21037/atm.2019.09.15131807526
- Nolan CM, Kaliaraju D, Jones SE, et al. Home versus outpatient pulmonary rehabilitation in COPD: a propensity-matched cohort study. Thorax. 2019;74(10):996–998. doi:10.1136/thoraxjnl-2018-21276531278173
- Edbrooke L, Aranda S, Granger CL, et al. Multidisciplinary home-based rehabilitation in inoperable lung cancer: a randomised controlled trial. Thorax. 2019;74(8):787–796. doi:10.1136/thoraxjnl-2018-21299631048509
- Morano MT, Araújo AS, Nascimento FB, et al. Preoperative pulmonary rehabilitation versus chest physical therapy in patients undergoing lung cancer resection: a pilot randomized controlled trial. Arch Phys Med Rehabil. 2013;94(1):53–58. doi:10.1016/j.apmr.2012.08.20622926460
- Loganathan RS, Stover DE, Shi W, et al. Prevalence of COPD in women compared to men around the time of diagnosis of primary lung cancer. Chest. 2006;129(5):1305–1312. doi:10.1378/chest.129.5.130516685023
- Misthos P, Katsaragakis S, Milingos N, et al. Postresectional pulmonary oxidative stress in lung cancer patients. The role of one-lung ventilation. Eur J Cardiothorac Surg. 2005;27(3):379–383. doi:10.1016/j.ejcts.2004.12.02315740942
- Lases EC, Duurkens VA, Gerritsen WB, et al. Oxidative stress after lung resection therapy: a pilot study. Chest. 2000;117(4):999–1003. doi:10.1378/chest.117.4.99910767230
- Tremblay LN, Slutsky AS. Pathogenesis of ventilator-induced lung injury: trials and tribulations. Am J Physiol Lung Cell Mol Physiol. 2005;288(4):L596–L598. doi:10.1152/ajplung.00438.200415757952
- Chen C, Jian W, Gao Y, et al. Early COPD patients with lung hyperinflation associated with poorer lung function but better bronchodilator responsiveness. Int J Chron Obstruct Pulmon Dis. 2016;11:2519–2526. doi:10.2147/COPD.S11002127785008
- Ramadan AA, Gaffin JM, Israel E, et al. Asthma and corticosteroid responses in childhood and adult asthma. Clin Chest Med. 2019;40(1):163–177. doi:10.1016/j.ccm.2018.10.01030691710
- Bölükbas S, Eberlein M, Eckhoff J, et al. Short-term effects of inhalative tiotropium/formoterol/budenoside versus tiotropium/formoterol in patients with newly diagnosed chronic obstructive pulmonary disease requiring surgery for lung cancer: a prospective randomized trial. Eur J Cardiothorac Surg. 2011;39(6):995–1000. doi:10.1016/j.ejcts.2010.09.02520970351
- Li W, Zhao Y, Sun Z, et al. Lung protective effects of budesonide nebulization during perioperative period of thoracolumbar fusion. J Thorac Dis. 2014;6(12):1800‐1807. doi:10.3978/j.issn.2072-1439.2014.12.36
- Sebio Garcia R, Yáñez Brage MI, Giménez Moolhuyzen E, et al. Functional and postoperative outcomes after preoperative exercise training in patients with lung cancer: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg. 2016;23(3):486‐497. doi:10.1093/icvts/ivw152
- Agostini P, Cieslik H, Rathinam S, et al. Postoperative pulmonary complications following thoracic surgery: are there any modifiable risk factors? Thorax. 2010;65(9):815‐818. doi:10.1136/thx.2009.123083