Abstract
Introduction
Chronic obstructive pulmonary disease (COPD) is an increasingly common cause of death worldwide. Its cardinal symptoms include breathlessness and severely reduced exercise capacity. Several patient-reported outcome (PRO) measures are used to assess health-related quality of life (HRQoL), functional performance, and breathlessness in patients with COPD. Exercise testing is employed to measure functional performance objectively, which is generally believed to impact on overall HRQoL. However, the extent to which commonly used laboratory- and field-based exercise test results correlate with PROs has not been systematically assessed.
Materials and methods
A search of Embase, MedLine, and the Cochrane Library identified primary publications in English that reported data on the correlations (Pearson’s r or Spearman’s ρ) between the outcomes of exercise tests and HRQoL and breathlessness PROs. Studies reporting on the following tests were included: 6-minute walk test (6MWT), 12MWT, incremental and endurance shuttle walk tests, incremental and endurance cycle ergometer tests, and treadmill tests.
Results
Of 3,205 articles screened, 28 were deemed eligible for inclusion. The most commonly reported HRQoL PRO measure was the St George’s Respiratory Questionnaire (13 studies), and the most commonly reported breathlessness PRO measure was the Baseline Dyspnea Index (six studies). The St George’s Respiratory Questionnaire appears to correlate very weakly to moderately with the 6MWT, and breathlessness PROs appear to be moderately to strongly associated with 6MWT outcomes. Across all studies, the 6MWT was the most commonly reported exercise test. Very few publications reporting associations between other exercise tests and PRO measures were found.
Conclusion
This review found evidence to support the association of 6MWT outcomes with HRQoL and breathlessness PROs. There were limited data showing correlations with the outcomes of other exercise tests. Further work is required to examine the associations between these PROs and exercise test outcomes.
Introduction
Chronic obstructive pulmonary disease (COPD) is a leading cause of death worldwide. The prevalence of the disease is projected to increase as the population ages and as exposure to risk factors, such as smoking, continues.Citation1–Citation3 COPD is characterized by breathlessness, episodes of exacerbations, and reduced exercise capacity.Citation4 Decreased exercise capacity can result in reduced ability to perform the activities of daily living, and the resultant inactivity and sedentary lifestyle can further exacerbate exercise-capacity impairment.Citation5,Citation6
In clinical practice, spirometry is recommended by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) for the diagnosis of COPD.Citation4 However, spirometry is a poor predictor of disability and health-related quality of life (HRQoL) in patients with COPD,Citation7 and correlates weakly with dyspnea, exercise capacity, and health status.Citation8–Citation10 Functional evaluations, such as exercise tests, are thus recommended in addition to spirometry. However, there is currently no single standard test for the assessment of exercise capacity. Field-based tests routinely used to measure exercise capacity include the 6-minute walk test (6MWT),Citation11 12MWT,Citation12 incremental shuttle walk test (ISWT),Citation13 and endurance SWT (ESWT).Citation14 Laboratory-based assessments allow the researcher to monitor several concomitant physiological variables, such as heart rate, workload performed, and oxygen consumption. Such tests include the incremental cycle ergometer test (ICET), endurance CET (ECET), and treadmill test (TT). It has been demonstrated that COPD and its consequent limitation of daily activity affect the HRQoL of patients.Citation15 Exercise tests are designed to reflect a patient’s exercise capacity, but how accurately they reflect patients’ HRQoL as assessed by patient-reported outcomes (PROs) of HRQoL and breathlessness in individuals with COPD is unclear. While there have been studies in which exercise tests have been included in the validation of new PRO instruments,Citation16,Citation17 it has elsewhere been reported that improvements in exercise capacity elicited by rehabilitation do not necessarily correlate with HRQoL PROs in patients with COPD.Citation18
Several questions remain regarding the associations between exercise tests and PROs. Which PROs are independent of exercise and which are not? Which, if any, PROs accurately and consistently reflect the ability of a patient with COPD to perform exercise? The purpose of this systematic review was to assess the strength of the available evidence supporting correlations between the outcomes of different exercise tests and the PROs most commonly used to assess HRQoL and breathlessness.
Materials and methods
Search strategy
Literature searches were conducted using Ovid, incorporating MedLine (1948 to January 22, 2013, then updated to include articles from July 23, 2012 to September 13, 2016), Embase (1974 to January 22, 2013 and July 23, 2012 to September 13, 2016), and the Cochrane Library (to January 22, 2013 and July 23, 2012 to September 12, 2016). Search strings were constructed to identify study publications (including those specific to emphysema and bronchitis) reporting primary data on the outcomes of the following exercise tests in patients with COPD: 6MWT, 12MWT, ISWT, ESWT, ICET, ECET, and TT. The full search strings used have been published previously.Citation19
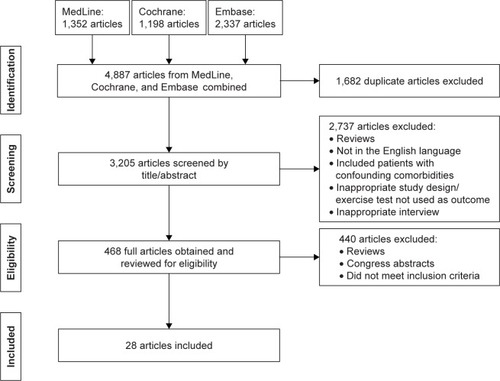
Study selection
Study selection followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for performing a systematic literature review.Citation20 Publications were initially screened based on titles and abstracts, and full articles were reviewed when their relevance was unclear from the abstract. Publications were excluded if they were review articles, not in English, studied patients with confounding comorbidities (eg, cancers or diabetes), unclear on the precise variables used for regression analysis, or examined an inappropriate intervention (eg, nonbronchodilatory pharmacotherapy or homeopathy). Articles were subsequently included for assessment only if they reported data on the correlations (Pearson’s r and/or Spearman’s ρ) between any of the prespecified exercise tests and PRO measures, such as the St George’s Respiratory Questionnaire (SGRQ)Citation17 total and individual domain scores (while the former is the usual means of reporting SGRQ data, significant correlations may exist within individual domains alone), the 36-item Short-Form Health Survey (SF-36),Citation21 the five-domain European QoL questionnaire (EQ-5D),Citation22,Citation23 the Chronic Respiratory Disease Questionnaire (CRQ),Citation24 the baseline dyspnea index (BDI),Citation25 the oxygen-cost diagram (OCD),Citation26 the Medical Research Council dyspnea scale (MRC),Citation27 and the modified MRC dyspnea scale (mMRC).Citation28 MRC and mMRC correlations were reported in combination, given that they report the same scale on different intervals.
Exercise tests and PRO measures
Exercise tests and respiratory-related PRO measures
The SGRQ is a disease-specific, self-administered questionnaire assessing symptoms, activity, and impacts on health status in COPD and asthma. Lower scores are associated with improved health status.Citation29 The CRQ is a comprehensive HRQoL questionnaire specific for individuals with COPD that assesses dyspnea, fatigue, emotional function, and mastery (the feeling of control over the disease and its effects). Each component is scored using a 7-point Likert scale, which can be combined to produce a total score of 20–140, with higher scores indicating improvement.Citation24 The BDI questionnaire assesses the severity of dyspnea based on the three components of functional impairment, magnitude of task, and magnitude of effort, which are rated from 0 (very severe) to 4 (no impairment). These scores can be combined to produce a focal score of 0–12, with higher scores indicating improved health status.Citation25 The OCD assesses dyspnea and measures the oxygen requirement of different activity levels. It is scored from 0 to 100 mm, with higher scores indicating greater improvement.Citation26 The MRC is a simple questionnaire that evaluates the effect of breathlessness on daily activities by grading patients’ perceptions of breathlessness from 1 to 5, with lower grades indicating less breathlessness and improved health status.Citation30 The mMRC is a 5-point version of this questionnaire.Citation31
Exercise tests and non-disease-specific PRO measures
The SF-36 is a generic questionnaire of 36 items, which assesses physical functioning, social functioning, role limitations (physical), role limitations (emotional), emotional well-being, mental health, energy and vitality, pain, general health perceptions, and current general health perceptions compared with the previous year to determine the general health status of a patient. Higher scores indicate better health status.Citation32 The EQ-5D is another measure that assesses HRQoL across the five dimensions of mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each dimension is scored from 1 (no problem) to 3 (severe problem). The test also includes a visual analog scale to measure general HRQoL from 0 to 100, with 100 representing the best health condition.Citation22
Inclusion/exclusion criteria and data abstraction
Owing to a lack of high-quality evidence for associations between these tests and the prespecified PRO measures, we included observational studies in our final analysis in addition to randomized controlled trials. In our literature search, we reviewed articles to identify those presenting Pearson’s and/or Spearman’s correlations between our stated PRO measures and the most commonly reported exercise test outcomes. Studies reporting lung-function variables only as a percentage of age-, sex-, and body-mass index-predicted values were excluded. Publications involving studies assessing multivariate regressions were also excluded, owing to the multifactorial nature of the statistical approach and the unsuitability of the output for aggregation.
Data were primarily abstracted by a single reviewer. A randomly generated selection of 30% of all articles was reviewed by a second reviewer in both phases for quality-control purposes. The following outcomes of exercise tests were recorded: distance or stages achieved for the 6MWT, 12MWT, and ISWT, duration of exercise for the ESWT and ECET, and the highest recorded volume of oxygen consumption (peak VO2) and maximum workload (Wmax) for the TT and ICET.
Statistical analysis
Pearson’s and Spearman’s correlations between PRO scores and the most commonly reported exercise test outcomes are presented. Pearson’s correlations are often used to describe the linear association between two variables when comparing continuous variable data. Spearman’s correlations are commonly used to describe the linear association between two sets of ranked (ordinal) data. Correlations are presented as the range of significant values reported in the study publications reviewed. The strength of correlations has been classified according to British Medical Journal guidelines, which regard significant correlation coefficients of 0–0.19 as very weak, 0.2–0.39 as weak, 0.4–0.59 as moderate, 0.6–0.79 as strong, and 0.8–1 as very strong.Citation33
Results
Overview of identified studies
The PRISMA-compliant search methodology used to identify relevant articles is summarized in . Of 3,205 articles screened, 28 were ultimately deemed eligible for inclusion in this review.Citation34–Citation61 provides a summary of the studies included.
Table 1 Summary of studies included
Correlations between exercise test outcomes and patient-reported quality of life-measure outcomes
St George’s Respiratory Questionnaire total score
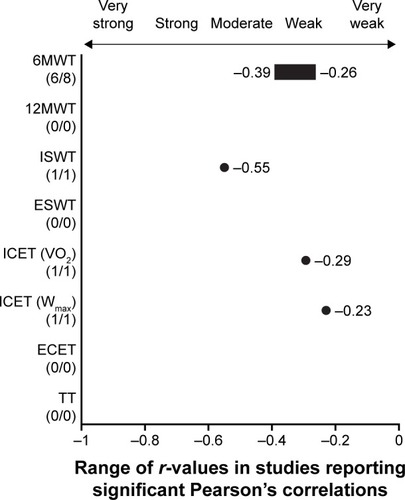
In total, 13 study publications reported correlations between the SGRQ total score (SGRQtotal) and one or more exercise test outcomes (, ).Citation37,Citation41–Citation43,Citation45,Citation46,Citation49,Citation50,Citation52,Citation53,Citation55,Citation59,Citation60 Of these, correlations between outcomes from the SGRQtotal and distance covered in the 6MWT were most commonly reported. These correlations were typically significant, with six articles reporting weak negative Pearson’s correlations of −0.26,Citation37 −0.26 (P<0.01),Citation59 −0.37 (P<0.05),Citation41 −0.37 (P=0.0228),Citation49 −0.39 (P<0.01),Citation53 and −0.39 (P=0.01),Citation60 demonstrating that as distance covered in the 6MWT increases, SGRQtotal scores decrease, indicating better health status. There were also two studies reporting Spearman’s correlations of −0.27Citation42 (JP de Torres confirmed this was incorrectly reported as 0.27 in the article) and −0.56.Citation50 Three papers noted nonsignificant associations between the 6MWT and SGRQtotal.Citation46,Citation52,Citation55 Limited data were available for other exercise tests, with moderate correlations given for the ISWT (r=−0.55Citation45, ρ=−0.55Citation43), weak–moderate correlations for the ICET (r=−0.29 to −0.23,Citation37,Citation41 ρ=−0.49 to −0.36,Citation50 depending on the outcome measure obtained [VO2 or Wmax]), and moderate Spearman’s correlations (ρ=−0.54Citation50 and −0.58Citation43) for the ECET and TT, respectively.
Table 2 Correlations between exercise test outcomes and selected quality-of-life PRO measures
Figure 2 Pearson’s correlations in studies reporting significant associations between exercise test outcomes and SGRQtotal.
Abbreviations: 6MWT, 6-minute walk test; 12MWT, 12-minute walk test; ECET, endurance cycle ergometer test; ESWT, endurance shuttle walk test; ICET, incremental cycle ergometer test; ISWT, incremental shuttle walk test; peak VO2, peak rate of oxygen consumption; SGRQtotal, St George’s Respiratory Questionnaire total score; TT, treadmill test; Wmax, highest workload achieved.
St George’s Respiratory Questionnaire activity domain
Correlations between exercise test outcomes and the SGRQ activity domain score (SGRQactivity) were reported in nine study publications ().Citation37,Citation43,Citation45,Citation46,Citation50,Citation53,Citation55,Citation59,Citation60 Of these, four articles noted significant weak–strong negative correlations between 6MWT distance and SGRQactivity (r=−0.35,Citation37 −0.36Citation53 [weak], and −0.44Citation60 [moderate]; ρ=−0.68Citation50 and an unspecified correlation of −0.37Citation46). Two further studies found strong correlations between SGRQactivity and ISWT outcome (r=−0.67Citation45 and ρ=−0.62Citation43), with two more finding no significant association for this relationship.Citation55,Citation59 One studyCitation50 reported moderate correlations between SGRQactivity and ICET peak VO2 (ρ=−0.51) and strong correlations between SGRQactivity and ICET Wmax (ρ=−0.62) and ECET (ρ=−0.62), with a weak correlation for the ICET Wmax found in one other study (r=−0.31).Citation37 Finally, one publication reported moderate correlations between TT peak VO2 and SGRQactivity (ρ=−0.58).Citation43 Again, these negative correlations suggest that as exercise performance increases, SGRQactivity scores decrease, indicating improved health status.
St George’s Respiratory Questionnaire impact domain
Correlations between exercise test outcomes and the SGRQ impact domain score (SGRQimpact) were reported in nine articles ().Citation37,Citation43,Citation45,Citation46,Citation50,Citation53,Citation55,Citation59,Citation60 Five studies found weak–moderate correlations between the SGRQimpact and the 6MWT (r=−0.22, −0.28, −0.37,Citation37,Citation53,Citation59 and 0.4;Citation60 ρ=−0.5Citation55), two found moderate evidence for an association between the SGRQimpact and the ISWT (r=−0.53Citation45 and ρ=−0.48Citation43), and there was moderate evidence for an association between the SGRQimpact and the ECET (ρ=−0.50)Citation50 or TT (ρ=−0.54).Citation43 A further study found a weak correlation between the SGRQimpact and the ICET Wmax (r=−0.20).Citation37
St George’s Respiratory Questionnaire symptom domain
Very limited data were found concerning associations between the SGRQ symptom domain score (SGRQsymptom) and exercise test outcomes (). Five studiesCitation46,Citation50,Citation53,Citation55,Citation60 of sevenCitation37,Citation46,Citation50,Citation53,Citation55,Citation59,Citation60 assessing the association between SGRQsymptom and 6MWT distance reported nonsignificant relationships. In the two studies that reported significant correlations between SGRQsymptom and 6MWT, very weak negative (−0.03)Citation37 and weak negative (−0.35)Citation59 correlations were found. Two studiesCitation45,Citation55 of threeCitation43,Citation45,Citation55 examining ISWT found no correlation with SGRQsymptom. One article reported weak (ρ=−0.34) and moderate (ρ=−0.44) correlations between the SGRQsymptom and the ISWT and TT, respectively.Citation43
St George’s Respiratory Questionnaire for COPD
One study publication reported on the relationship between the 6MWT and the disease-specific SGRQ for COPD (SGRQ-c); however, this study examined risk factors, and reported only that worse (higher) SGRQ-c scores were an independent predictor of lower 6MWT distances.Citation62
Other quality-of-life instruments
Too few publications reporting associations between exercise test outcomes and the SF-36, CRQ, or EQ-5D PROs were found to enable any meaningful assessment of their relationships.
Correlations between exercise test outcomes and self-reported breathlessness
Associations between the BDI and exercise test outcomes were reported for six studies (; ).Citation36,Citation44,Citation48,Citation52,Citation55,Citation56 Four articles noted an association between the 6MWT and BDI score: three publications reported moderate–very strong Pearson’s correlations (r=0.47–0.86),Citation44,Citation48,Citation56 with another reporting a moderate Spearman’s correlation (ρ=0.49).Citation55 Only one study assessing this relationship found no significant correlation.Citation52 Two additional publications reported moderate–strong Pearson’s correlations between the BDI and ISWT (−0.46Citation36 and 0.76Citation48), with another reporting no significant correlation.Citation55 The positive correlations demonstrated in these studies show that PRO scores increase as exercise performance improves, indicating improved health status.
Table 3 Correlations between exercise test outcomes and selected patient-reported breathlessness measures
Figure 3 Pearson’s correlations in studies reporting significant associations between the 6-minute walk-test outcomes and breathlessness PROs.
Abbreviations: BDI, Baseline Dyspnea Index; mMRC, modified Medical Research Council (dyspnea scale); PRO, patient-reported outcome; OCD, oxygen-cost diagram.
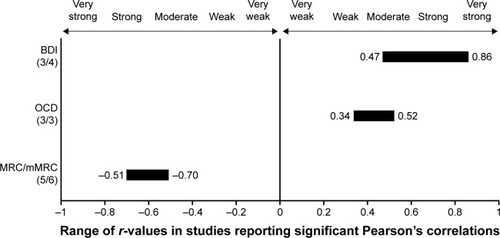
Associations between OCD and exercise test outcomes were reported in seven articles (; ).Citation36,Citation39,Citation40,Citation44,Citation50,Citation51,Citation56 Of these, three publications reported weak–moderate Pearson’s correlations between the 6MWT and the OCD, ranging from 0.34 to 0.52,Citation40,Citation44,Citation56 with a further study finding a strong Spearman’s correlation (ρ=0.66).Citation50 Only one study found no significant correlation between the 6MWT and the OCD.Citation39 Single articles noted weak–moderate correlations for the 12MWT (r=0.50)Citation51 and the ISWT (r=0.33),Citation36 and a further paper reported strong Spearman’s correlations of 0.61 and 0.74 for the ICET, when peak VO2 and Wmax were used for the main outcome measure, respectively.Citation50 The same study also found moderate (ρ=0.59) correlations between the OCD and the ECET. Of six studiesCitation41,Citation47,Citation52,Citation53,Citation56,Citation61 reporting Pearson’s correlations between the 6MWT and the MRC/mMRC scale, fiveCitation41,Citation47,Citation53,Citation56,Citation61 reported r-values ranging from −0.51 to −0.7. However, one of these studies reporting Pearson’s correlations between the 6MWT and the MRC/mMRC scale described r2 rather than r. For the basis of this analysis, this study was included under the assumption that a Pearson’s correlation was used and rCitation2 was a typographical error.Citation61 One studyCitation52 reported no significant correlation (; ), and another two studies reported a significant Spearman’s correlation between MRC/mMRC and the 6MWT (−0.51Citation39 and −0.39Citation38). The negative correlations demonstrated in these studies show that PRO scores decrease as exercise performance improves, indicating improved health status.
Discussion
This systematic review has shown that there are limited studies available reporting on the correlations between exercise test outcomes and PROs. Of these, the body of evidence describing a relationship between these outcome measures is even smaller. The most commonly reported association was between SGRQtotal outcomes and distance covered in the 6MWT. Though typically significant, these correlations were generally weak–moderate. The available evidence also showed correlations between the SGRQtotal and SGRQactivity and the ISWT, ICET (Wmax), ECET, and TT, which tended to be moderate–strong. No studies were found that assessed associations between exercise test and SGRQ outcomes (including all subscales) for 12MWT and ESWT. However, all of these correlations must be considered in the context of substantial heterogeneity in study design, disease severity, and sample size.
The majority of studies investigating associations between exercise test outcomes and self-reported breathlessness scores, such as the BDI, OCD, and mMRC, have used the 6MWT. The PROs of these tended to exhibit at least moderate correlations with exercise test outcomes. In particular, the BDI was generally reported to have a moderate–very strong Pearson’s correlation with the 6MWT in three of four studies, with a further study reporting a moderate Spearman’s correlation for this relationship.
Among included studies, there was a wide range of study designs and patient cohorts. As high-quality evidence is limited in this field, observational studies were combined with the results of randomized controlled trials, with the risk of affording similar weight to their interpretation. It is thus possible that significant associations could be underrecognized, owing to a type II statistical reporting error, a factor that must be considered when designing or interpreting studies to assess these exercise tests. Many of these studies reported nonsignificant correlations. Given the number of studies with small patient numbers that did report significant correlations, sample size is unlikely to be a factor in the nonsignificant correlations demonstrated by some studies. However, substantial heterogeneity was observed among some of the patient populations in terms of baseline demographics.
There are also inconsistencies in the way in which results were reported, with some study publications reporting incongruous negative/positive correlations compared with others describing the same relationship. It is unclear whether this reflects differences in the way in which the instruments were used or the way in which the statistical tests were applied between instruments and exercise test outcomes. We have presented such values as reported in the source articles. Additionally, the inclusion criteria and COPD severity are often not clearly stated in the articles included in this review. There is thus a risk that the patients in the studies included were not a broadly homogeneous group. Therefore, we would recommend that future studies clearly state inclusion criteria and the clinical rationale for diagnosis whenever possible.
Although not included in the review, consideration should also be given to the correlations demonstrated in studies that fell outside the selected search criteria. Several studies that were not included here showed significant relationships between exercise and breathlessness or PROs, either demonstrating correlations with new tools or using correlation coefficients other than Pearson’s or Spearman’s. For example, associations between exercise capacity and the i-BODE index (body-mass index, airflow obstruction, dyspnea, exercise-capacity index [exercise-capacity measured using ISWT]),Citation63 the Functional Assessment of Chronic Illness Therapy – fatigue (FACIT-F) instrument,Citation64 the London Chest Activity of Daily Living (LCADL) scale,Citation65 and the McGill Pain Questionnaire (MPQ)Citation66 were identified in patients with COPD. Moreover, correlations between the 6MWT and the COPD assessment test (CAT)Citation67 and between the desaturation:distance ratio (DDR) and Borg scaleCitation68 have been identified. The criteria chosen for this review were based on well-established PROs, rather than those that have been more recently developed. However, many of these more novel tests are increasing in popularity, and as such, further investigation into their correlation with breathlessness or HRQoL PROs will be useful to determine their relevance in predicting prognosis in patients with COPD.
Despite the noted limitations, three further recommendations can be drawn directly from these findings. First, one of our included studies reported correlations between two PRO measures (SGRQtotal and OCD) and two common outcome measures for the ICET: peak VO2 and Wmax. In both, the PRO was more closely correlated with the ICET Wmax than the ICET peak VO2. This finding complements that of another systematic review conducted by these authors,Citation69 which showed that exercise test outcomes tended to be more closely correlated with Wmax as a measure of lung function than with peak VO2. It thus seems prudent to suggest that when investigating ICET, researchers report Wmax values as a priority.
Second, as a combination of the SF-36 and EQ-5D is the instrument of choice for assessing HRQoL of several health technology-assessment bodies, the lack of studies reporting associations between this outcome measure and exercise tests is of note. Clinical trial designers might usefully consider this in assessing the most appropriate clinical trial end point. Third, the results of this review suggest that exercise tests are not interchangeable, and as such, comparisons of different exercise tests in response to interventions are inappropriate.
In conclusion, these findings indicate that only limited evidence is available to support an association between exercise test outcomes and HRQoL and breathlessness PROs in patients with COPD. The evidence that does exist suggests a very weak–moderate negative correlation between the 6MWT and the SGRQ. Both moderate–strong positive and negative correlations between 6MWT outcomes and breath-lessness were observed. It has not been possible to assess other tests adequately, though the limited data available suggest that the ISWT, ICET, ECET, and TT may be more closely associated with the SGRQ (and HRQoL outcomes) than the 6MWT. Recent guidelines on the diagnosis and treatment of COPD indicate that the assessment of disease severity is improved by using functional criteria, such as exercise capacity.Citation4,Citation70,Citation71 However, the current evidence suggests that no single exercise test accurately reflects HRQoL or breathlessness in patients with COPD. Therefore, despite the paucity of data for some tests, it may be justified to conclude that these tests assess features not measured by these HRQoL outcomes. Consequently, a composite measurement assessing several factors reflective of COPD, such as the BODE index, which evaluates a surrogate of nutritional state (body-mass index), airflow obstruction (FEV1), dyspnea (mMRC), and exercise capacity (6MWT), may be a more accurate measure of COPD severity and prognosis.Citation72 The BODE index predicts the requirement for hospitalizations among patients with COPD better than either FEV1 or classic GOLD staging.Citation73 It thus seems reasonable to surmise that individual PROs may have limited prognostic ability in patients with COPD, and should be supported by additional measurements wherever possible.
Author contributions
All authors contributed to the conception and design of the study, analysis and interpretation of data, and revision of the manuscript, and approved the final version of the manuscript.
Acknowledgments
The authors would like to thank Martin Bell, Iain Fotheringham, and Sarah Cockle for their contribution to the original study, and Jelle Spoorendonk, Weiwei Xu, and Janita Balradi (Pharmerit International) for conducting the updated systematic literature review. Editorial support (in the form of writing assistance, assembling tables and figures, collating author comments, grammatical editing, and referencing) was provided by Rachael Baylie, PhD at Fishawack Indicia Ltd, UK, and was funded by GSK. This study was funded by GSK.
Disclosure
YSP, JHR, EL, and MD are current employees of Glaxo-SmithKline and hold stocks in GlaxoSmithKline. SJS was involved with the development of the incremental shuttle walk test, and has served on advisory boards for GlaxoSmithKline. SJS was part funded by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care East Midlands (CLAHRC EM). Support was also provided by the NIHR Leicester Respiratory Biomedical Research Unit. The views expressed are those of the authors, and not necessarily those of the National Health Service (NHS), the NIHR, or the Department of Health. The work presented here, including the conduct of the study, data analysis, and interpretation, was funded by GSK (HO-12-12583).
References
- LopezADShibuyaKRaoCChronic obstructive pulmonary disease: current burden and future projectionsEur Respir J200627239741216452599
- HalbertRJNatoliJLGanoABadamgaravEBuistASManninoDMGlobal burden of COPD: systematic review and meta-analysisEur Respir J200628352353216611654
- MathersCDLoncarDProjections of global mortality and burden of disease from 2002 to 2030PLoS Med2006311e44217132052
- Global Initiative for Chronic Obstructive Lung Disease (GOLD)Global Strategy for the Diagnosis, Management, and Prevention of COPDBethesda (MD)GOLD2014
- GoskerHRLencerNHFranssenFMVan Der VusseGJWoutersEFScholsAMStriking similarities in systemic factors contributing to decreased exercise capacity in patients with severe chronic heart failure or COPDChest200312351416142412740256
- O’DonnellDEGebkeKBActivity restriction in mild COPD: a challenging clinical problemInt J Chron Obstruct Pulmon Dis2014957758824940054
- JonesPMiravitllesMvan der MolenTKulichKBeyond FEV1 in COPD: a review of patient-reported outcomes and their measurementInt J Chron Obstruct Pulmon Dis2012769770923093901
- CooperCBThe connection between chronic obstructive pulmonary disease symptoms and hyperinflation and its impact on exercise and functionAm J Med200611910 Suppl 1213116996896
- JonesPWIssues concerning health-related quality of life in COPDChest19951075 Suppl187S193S7743825
- MahlerDAHarverAA factor analysis of dyspnea ratings, respiratory muscle strength, and lung function in patients with chronic obstructive pulmonary diseaseAm Rev Respir Dis19921452 Pt 14674701736759
- ButlandRJPangJGrossERWoodcockAAGeddesDMTwo-, six-, and 12-minute walking tests in respiratory diseaseBr Med J (Clin Res Ed)1982284632916071608
- McGavinCRGuptaSPMcHardyGJTwelve minute walking test for assessing disability in chronic bronchitisBr Med J1976160138228231260350
- SinghSJMorganMDScottSWaltersDHardmanAEDevelopment of a shuttle walking test of disability in patients with chronic airways obstructionThorax19924712101910241494764
- RevillSMMorganMDSinghSJWilliamsJHardmanAEThe endurance shuttle walk: a new field test for the assessment of endurance capacity in chronic obstructive pulmonary diseaseThorax199954321322210325896
- LuYNyuntMSGweeXLife event stress and chronic obstructive pulmonary disease (COPD): associations with mental well-being and quality of life in a population-based studyBMJ Open201226e001674
- GarrodRMarshallJBarleyEJonesPWPredictors of success and failure in pulmonary rehabilitationEur Respir J200627478879416481381
- JonesPWQuirkFHBaveystockCMLittlejohnsPA self-complete measure of health status for chronic airflow limitation: the St George’s Respiratory QuestionnaireAm Rev Respir Dis19921456132113271595997
- WijkstraPJVan AltenaRKraanJOttenVPostmaDSKoeterGHQuality of life in patients with chronic obstructive pulmonary disease improves after rehabilitation at homeEur Respir J1994722692738162979
- FotheringhamIMeakinGPunekarYSRileyJHCockleSMSinghSJComparison of laboratory-and field-based exercise tests for COPD: a systematic reviewInt J Chron Obstruct Pulmon Dis20151062564325834421
- MoherDLiberatiATetzlaffJAltmanDGGroupPPreferred reporting items for systematic reviews and meta-analyses: the PRISMA statementBMJ2009339b253519622551
- JenkinsonCCoulterAWrightLShort form 36 (SF36) health survey questionnaire: normative data for adults of working ageBMJ19933066890143714408518639
- EuroQol GroupEuroQol: a new facility for the measurement of health-related quality of lifeHealth Policy199016319920810109801
- BrooksREuroQol: the current state of playHealth Policy1996371537210158943
- GuyattGHBermanLBTownsendMPugsleySOChambersLWA measure of quality of life for clinical trials in chronic lung diseaseThorax198742107737783321537
- MahlerDAWeinbergDHWellsCKFeinsteinARThe measurement of dyspnea: contents, interobserver agreement, and physiologic correlates of two new clinical indexesChest19848567517586723384
- McGavinCRArtvinliMNaoeHMcHardyGJDyspnoea, disability, and distance walked: comparison of estimates of exercise performance in respiratory diseaseBr Med J197826132241243678885
- FletcherCMElmesPCFairbairnASWoodCHThe significance of respiratory symptoms and the diagnosis of chronic bronchitis in a working populationBr Med J19592514725726613823475
- MahlerDARosielloRAHarverALentineTMcGovernJFDaubenspeckJAComparison of clinical dyspnea ratings and psychophysical measurements of respiratory sensation in obstructive airway diseaseAm Rev Respir Dis19871356122912333592398
- JonesPWQuirkFHBaveystockCMLittlejohnsPA self-complete measure of health status for chronic airflow limitation: the St. George’s Respiratory QuestionnaireAm Rev Respir Dis19921456132113271595997
- BestallJPaulEGarrodRGarnhamRJonesPWedzichaJUsefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary diseaseThorax199954758158610377201
- Global Initiative for Chronic Obstructive Lung Disease (GOLD)Global Strategy for the Diagnosis, Management, and Prevention of COPDBethesda (MD)GOLD2016
- JenkinsonCCoulterAWrightLShort form 36 (SF36) health survey questionnaire: normative data for adults of working ageBMJ19933066890143714408518639
- BMJ Publishing GroupCorrelation and regression Available from: http://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one/11-correlation-and-regressionAccessed May 16, 2017
- BelzaBSteeleBGHunzikerJLakshminaryanSHoltLBuchnerDMCorrelates of physical activity in chronic obstructive pulmonary diseaseNurse Res2001504195202
- BenzoRPSciurbaFCOxygen consumption, shuttle walking test and the evaluation of lung resectionRespiration2010801192319672050
- BoerLMAsijeeGMvan SchayckOCSchermerTRHow do dyspnoea scales compare with measurement of functional capacity in patients with COPD and at risk of COPD?Prim Care Respir J201221220220722453664
- BrownCDBendittJOSciurbaFCExercise testing in severe emphysema: association with quality of life and lung functionCOPD20085211712418415810
- CallensEGrabaSGillet-JuvinKMeasurement of dynamic hyperinflation after a 6-minute walk test in patients with COPDChest200913661466147219581350
- CamargoLAPereiraCADyspnea in COPD: beyond the modified Medical Research Council scaleJ Bras Pneumol201036557157821085822
- ChuangMLLinIFWassermanKThe body weight-walking distance product as related to lung function, anaerobic threshold and peak VO2 in COPD patientsRespir Med200195761862611453321
- CoteCGPinto-PlataVKasprzykKDordellyLJCelliBRThe 6-min walk distance, peak oxygen uptake, and mortality in COPDChest200713261778178517925409
- de TorresJPCasanovaCHernandezCGender associated differences in determinants of quality of life in patients with COPD: a case series studyHealth Qual Life Outcomes200647217007639
- DowsonLJNewallCGuestPJHillSLStockleyRAExercise capacity predicts health status in alpha1-antitrypsin deficiencyAm J Respir Crit Care Med2001163493694111282769
- EakinEGKaplanRMRiesALSassi-DambronDEPatients’ self-reports of dyspnea: An important and independent outcome in chronic obstructive pulmonary diseaseAnn Behav Med1996182879024203690
- EmtnerMIArnardottirHRHallinRLindbergEJansonCWalking distance is a predictor of exacerbations in patients with chronic obstructive pulmonary diseaseRespir Med200710151037104017085030
- HeijdraYFPinto-PlataVMKenneyLARassuloJCelliBRCough and phlegm are important predictors of health status in smokers without COPDChest200212151427143312006424
- HillmanCMHeineckeELHiiJWCecinsNMJenkinsSCEastwoodPRRelationship between body composition, peripheral muscle strength and functional exercise capacity in patients with severe chronic obstructive pulmonary diseaseIntern Med J201242557858122616963
- HodgevVAAlimanOIMarinovBIKostianevSSMandulovaPVCardiovascular and dyspnea response to six-minute and shuttle walk tests in COPD patientsFolia Med (Plovdiv)2003453263315366663
- MangueiraNMViegaILMangueiraMAPinheiroANCostaMRCorrelation between clinical parameters and health-related quality of life in women with COPDJ Bras Pneumol200935324825519390723
- OgaTNishimuraKTsukinoMHajiroTIkedaAMishimaMRelationship between different indices of exercise capacity and clinical measures in patients with chronic obstructive pulmonary diseaseHeart Lung200231537438112487016
- O’ReillyJFShaylorJMFromingsKMHarrisonBDThe use of the 12 minute walking test in assessing the effect of oral steroid therapy in patients with chronic airways obstructionBr J Dis Chest19827643743826758833
- PelegrinoNRLuchetaPASanchezFFFaganelloMMFerrariRde GodoyIInfluence of lean body mass on cardiopulmonary repercussions during the six-minute walk test in patients with COPDJ Bras Pneumol2009351202619219327
- PeruzzaSSergiGVianelloAChronic obstructive pulmonary disease (COPD) in elderly subjects: impact on functional status and quality of lifeRespir Med200397661261712814144
- RejeskiWJFoleyKOWoodardCMZaccaroDJBerryMJEvaluating and understanding performance testing in COPD patientsJ Cardiopulm Rehabil2000202798810763155
- RosaFWCamelierAMayerAJardimJREvaluating physical capacity in patients with chronic obstructive pulmonary disease: comparing the shuttle walk test with the encouraged 6-minute walk testJ Bras Pneumol200632210611317273579
- WegnerREJorresRAKirstenDKMagnussenHFactor analysis of exercise capacity, dyspnoea ratings and lung function in patients with severe COPDEur Respir J1994747257298005256
- WijkstraPJTenVergertEMvan der MarkTWRelation of lung function, maximal inspiratory pressure, dyspnoea, and quality of life with exercise capacity in patients with chronic obstructive pulmonary diseaseThorax19944954684728016768
- KaplanRMRiesALReillyJMohsenifarZMeasurement of health-related quality of life in the national emphysema treatment trialChest2004126378178915364757
- AgrawalSRJoshiRJainACorrelation of severity of chronic obstructive pulmonary disease with health-related quality of life and six-minute walk test in a rural hospital of central IndiaLung India201532323324025983408
- BavarsadMBShariatiAEidaniELatifiMRelationship between exercise capacity and clinical measures in patients with chronic obstructive pulmonary diseaseBiomed Pharmacol J2015817
- SunKSLinMSChenYJChenYYChenSCChenWIs asymptomatic peripheral arterial disease associated with walking endurance in patients with COPD?Int J Chron Obstruct Pulmon Dis2015101487149226251588
- SpruitMAWatkinsMLEdwardsLDDeterminants of poor 6-min walking distance in patients with COPD: the ECLIPSE cohortRespir Med2010104684985720471236
- UtkuESErgunPSKaymazDYi-BODE for evaluating the efficiency of pulmonary rehabilitation in patients with COPDEur Respir J201342Suppl 57P2230
- AlahmariADKowlessarBSPatelARPhysical activity and exercise capacity in patients with moderate COPD exacerbationsEur Respir J201648234034927126688
- Garcia-PoloCAlcazar-NavarreteBRuiz-IturriagaLAFactors associated with high healthcare resource utilisation among COPD patientsRespir Med2012106121734174223058483
- GhanbariBHGarlandSJRoadJDReidWDPain and physical performance in people with COPDRespir Med2013107111692169923845881
- AkorAAObasekiDAdeniylBCOPD assessment test in patients with COPD in Africa: a preliminary surveyAm J Respir Crit Care Med2014189A2951
- IjiriNKanazawaHYoshikawaTHirataKApplication of a new parameter in the 6-minute walk test for manifold analysis of exercise capacity in patients with COPDInt J Chron Obstruct Pulmon Dis201491235124025395845
- BellMFotheringhamIPunekarYSRileyJHCockleSSinghSJSystematic review of the association between laboratory- and field based exercise tests and lung function in patients with chronic obstructive pulmonary diseaseChronic Obstr Pulm Dis201523321342
- National Institute for Health and Care ExcellenceManagement of Chronic Obstructive Pulmonary Disease in Adults in Primary and Secondary Care Partial updateLondonNICE2010
- American Thoracic Society/European Respiratory Society Task ForceStandards for the Diagnosis and Management of Patients with COPD. Version 1.2New YorkAmerican Thoracic Society2005
- CelliBRCoteCGMarinJMThe body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary diseaseN Engl J Med2004350101005101214999112
- OngKCEarnestALuSJA multidimensional grading system (BODE index) as predictor of hospitalization for COPDChest200512863810381616354849
- No authors listedRationale and design of the national emphysema treatment trial: a prospective randomized trial of lung volume reduction surgeryChest199911661750176110593802
- FishmanAMartinezFNaunheimKA randomized trial comparing lung-volume-reduction surgery with medical therapy for severe emphysemaN Eng J Med20033482120592073
- Sassi-DambronDEEakinEGRiesALKaplanRMTreatment of dyspnea in COPD: a controlled clinical trial of dyspnea management strategiesChest199510737247297874944