Abstract
Introduction
Chemokine (C-C motif) ligand 18 (CCL-18) has been shown to be elevated in chronic obstructive pulmonary disease (COPD) patients. This study primarily aimed to evaluate whether the serum CCL-18 level differentiates the frequent exacerbator COPD phenotype from infrequent exacerbators. The secondary aim was to investigate whether serum CCL-18 level is a risk factor for exacerbations requiring hospitalization.
Materials and methods
Clinically stable COPD patients and participants with smoking history but normal spirometry (NSp) were recruited for the study. Modified Medical Research Council Dyspnea Scale, COPD Assessment Test, spirometry, and 6-min walking test were performed. Serum CCL-18 levels were measured with a commercial ELISA Kit.
Results
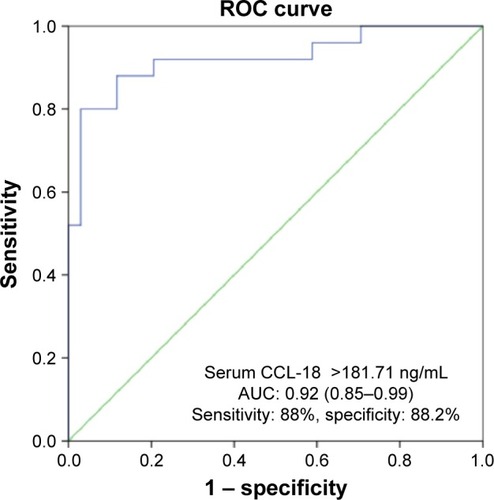
Sixty COPD patients and 20 NSp patients were recruited. Serum CCL-18 levels were higher in COPD patients than those in NSp patients (169 vs 94 ng/mL, P<0.0001). CCL-18 level was significantly correlated with the number of exacerbations (r=0.30, P=0.026), although a difference in CCL-18 values between infrequent and frequent exacerbator COPD (168 vs 196 ng/mL) subgroups did not achieve statistical significance (P=0.09). Serum CCL-18 levels were significantly higher in COPD patients who had experienced at least one exacerbation during the previous 12 months. Overall, ROC analysis revealed that a serum CCL-18 level of 181.71 ng/mL could differentiate COPD patients with hospitalized exacerbations from those who were not hospitalized with a 88% sensitivity and 88.2% specificity (area under curve: 0.92). Serum CCL-18 level had a strong correlation with the frequency of exacerbations requiring hospitalization (r=0.68, P<0.0001) and was found to be an independent risk factor for hospitalized exacerbations in the multivariable analysis.
Conclusion
CCL-18 is a promising biomarker in COPD, as it is associated with frequency of exacerbations, particularly with severe COPD exacerbations requiring hospitalization, as well as with functional parameters and symptom scores.
Introduction
Chronic obstructive pulmonary disease (COPD) is a major cause of mortality and morbidity worldwide. It is a chronic and progressive disease often associated with periods of exacerbation that are related with reduced health-related quality of life, accelerated forced expiratory volume in 1 s (FEV1) decline, increased health resource utilization and increased mortality.Citation1,Citation2 Acute exacerbations of COPD requiring hospitalization are particularly important because they lead to an increased economical burden, and each has the potential for a fatal outcome.Citation3 Current knowledge of factors associated with exacerbations requiring hospitalization is limited.Citation4,Citation5 It is suggested that COPD patients suffering from frequent exacerbations belong to a distinct phenotype, as demonstrated in the Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) study.Citation6,Citation7
Currently, COPD diagnosis is based on the presence of symptoms and risk factors with a spirometric evaluation demonstrating FEV1 over forced vital capacity (FVC) <0.70. Since this approach has several limitations, a molecular biomarker would be of great use for diagnosing, staging, and phenotyping COPD and also for singling out the exacerbator phenotype. The potential value of several biomarkers in diagnosis, assessing the severity assessment, etiology, and frequency of COPD exacerbations has been examined in recent studies, and plausible candidates have been identified.Citation8–Citation10
Pulmonary and activation-regulated chemokine (PARC)/chemokine (C-C motif) ligand 18 (CCL-18) is a 7-kD protein that is mainly expressed by monocytes/macrophages and dendritic cells. It is secreted predominantly by the lungs, avoiding the possible interference of any protein derived from nonpulmonary organs such as the liver.Citation11 In the ECLIPSE cohort, it was shown that serum CCL-18 levels were found to be elevated in patients with COPD and associated with COPD-related clinical and functional outcomes and mortality.Citation12,Citation13 The primary aim of this study was to evaluate whether levels of serum CCL-18 could differentiate the frequent exacerbator COPD phenotype from infrequent exacerbators, and the secondary aim was to investigate whether serum CCL-18 levels can predict exacerbations that would require hospitalization.
Materials and methods
Study subjects and study design
This case–control study was conducted in the outpatient clinic at the Department of Pulmonary Diseases, Uludağ University Faculty Hospital – a tertiary reference center in the Southern Marmara Region, the most populous area of Turkey. COPD patients aged 40–75 years with a smoking history of ≥10 pack-years, who met diagnostic criteria of the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines and were characterised by persistent airway limitation (post-bronchodilator FEV1/FVC <0.70) were recruited.Citation1 Clinically stable COPD patients with no episodes of exacerbation in the previous 2 months were consecutively enrolled from October 2012 to April 2013. COPD exacerbation was defined as an event in the natural course of the disease characterized by a change in the patient’s baseline dyspnea, cough, and/or sputum that was beyond normal day-to-day variations and that required treatment with systemic steroids or antibiotics, and/or a visit to the emergency room or admission to hospital.Citation14,Citation15 Acute COPD exacerbations in the previous 12 months were assessed using both patients’ recall of exacerbation events and medical records. Based on their frequency in the previous 12 months, COPD patients were classified as either frequent (≥2 events, FE-COPD) or infrequent (<2 events, IE-COPD) exacerbators.Citation16 In a separate analysis, baseline characteristics of COPD patients with and without hospitalized exacerbation in the previous 12 months were compared. The control group consisted of apparently healthy volunteer participants with a smoking history of ≥10 pack-years and normal spirometry (NSp). Exclusion criteria for both COPD and NSp were asthma, bronchiectasis, presence of tuberculosis, pneumonia or sign of any other active infection, inflammatory diseases such as connective tissue disorder, arthritis or inflammatory bowel disease, and malignancy. This study was approved by the ethics comittee of the Uludag University. All participants provided written informed consent prior to their inclusion in the study.
Methods
Participants were examined by one of the study researchers, and a detailed structured questionnaire including risk factors, smoking status, disease history including exacerbations, and comorbid conditions was completed for each patient. Severity of dyspnea was assessed by using the modified Medical Research Council (mMRC) Dyspnea Scale.Citation17 Symptom severity was assessed with the eight-item patient-reported outcome measure, the COPD Assessment Test (CAT).Citation18 The Turkish version of the CAT was shown to be a valid and reliable tool.Citation19 Spirometry was performed before and after administration of short-acting β2-agonist (albuterol) by using Vmax Encore System (Sensormedics, Viasys, Yorba Linda, CA, USA) in accordance with ATS/ERS recommendations.Citation20 Spirometric staging of COPD was based on GOLD guidelines.Citation1 Subjects underwent the 6-min walking test according to the ATS statement.Citation21 The body mass index, airflow obstruction, dyspnea, exercise capacity index (BODE index) is a multidimensional grading system comprising body mass index (BMI), airflow obstruction assessed by postbronchodilator FEV1 %predicted, functional dyspnea based on mMRC scale, and the 6-min walking distance (6MWD) as a measure of functional exercise capacity.Citation22 For computing the BODE index, the predescribed model was used: for each threshold value of FEV1, 6MWD, and mMRC scale, the patients received scores ranging from 0 (lowest) through 3 (maximum), while BMI was scored 0 or 1 (BMI ≤21 and >21, respectively). Points for each variable were added, and the BODE index was calculated ranging from 0 to 10 points for each patient.Citation22 Comorbidities were quantified by the Charlson Comorbidity Index (CCI).Citation23
Measurement of serum CCL-18 and C-reactive protein (CRP) measurement
Approximately 10 mL of peripheral venous blood was collected from study participants into vacutainer EDTA-containing tubes. Serum was obtained by centrifugation at 1,500× g for 10–15 min. Samples were stored at −80°C until analysed. Levels of PARC/CCL-18 were measured with a human PARC ELISA Kit (Ray Biotech, Inc) according to the manufacturer’s instructions. The detection limit of this assay was 2 pg/mL. Serum CRP levels were determined by an immunonephelometric method by using the BN II device (Siemens, Germany); the detection limit was 0.5 mg/dL.
Statistical analysis
Statistical analyses were performed using the IBM SPSS Statistics for Windows, Version 22.0 software program (IBM Corp., Armonk, NY, USA). Variables were investigated using visual (histograms and probability plots) and analytical methods (Kolmogorov–Smirnov/Shapiro–Wilk’s test) to determine whether or not they were normally distributed. Data were presented by mean ± standard deviation. Categorical variables were reported as proportions. A chi-square test was used to compare proportions between the two groups and a two-sample t-test for continuous outcome variables with normal distribution (–). For non-normal data, Mann–Whitney U-test was performed (– and and ). The ability of serum CCL-18 level to discriminate COPD versus NSp and to discriminate patients with COPD exacerbations in the previous 12 months who required hospitalization from those who were not hospitalized was analyzed using receiver operating characteristics (ROC) curve analysis. Optimal cutoff maximizing sensitivity and specificity was selected. Sensitivity and specificity were reported using the optimal ROC curve value according to the Youden Index. While evaluating the area under curve (AUC), a 5% type-1 error level was used to accept a statistically significant predictive value of the test variable ( and ). The possible factors identified with univariable analysis were further entered into a logistic regression analysis to determine independent predictors of hospitalized COPD exacerbations. Covariates were included in the model if the P<0.10. Hosmer–Lemeshow goodness-of-fit test was used to assess model fit. Two-tailed statistical significance level was considered as 5%, and unadjusted P-values were reported (). Correlations between CCL-18 and the other variables were explored using Spearman’s rank correlations ( and ).
Table 1 Characteristic features of the study groups
Table 2 Clinical and functional characteristics of the infrequent versus frequent exacerbator COPD patients
Table 3 Clinical and functional characteristics of the COPD patients with and without exacerbations requiring hospitalization
Table 4 Univariable and multivariable analysis of possible risk factors for exacerbation requiring hospitalization in the previous year
Table 5 Univariate correlations (r) between serum CCL-18 level and frequency of exacerbations, frequency of exacerbations requiring hospitalization, airflow limitation, dyspnea perception, total symptom scores, 6-min walking distance, BODE index, and comorbidities in the COPD group (n=60)
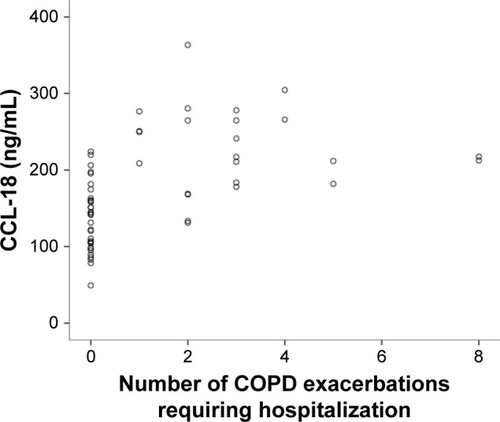
Figure 1 Comparison of serum CCL-18 concentration of infrequent exacerbator COPD patients with frequent exacerbator COPD patients. The central horizontal line on each box represents the median, the ends of the boxes are 25 and 75 percentiles and the error bars 5% and 95%. P-values derived from the Mann–Whitney U-test.
Abbreviations: COPD, chronic obstructive pulmonary disease; IE-COPD, infrequent exacerbator chronic obstructive pulmonary disease patients; FE-COPD, frequent exacerbator chronic obstructive pulmonary disease patients.
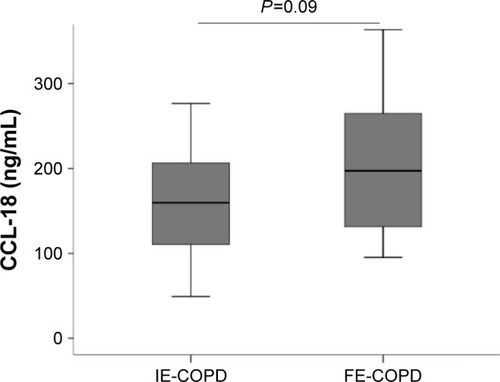
Figure 2 Comparison of serum CCL-18 concentration in COPD patients with ≥1 hospitalized exacerbations and those who were not hospitalized. The central horizontal line on each box represents the median, the ends of the boxes are 25 and 75 percentiles and the error bars 5% and 95%. P-values derived from the Mann–Whitney U-test.
Abbreviations: CCL-18, chemokine (C-C motif) ligand 18; COPD, chronic obstructive pulmonary disease.
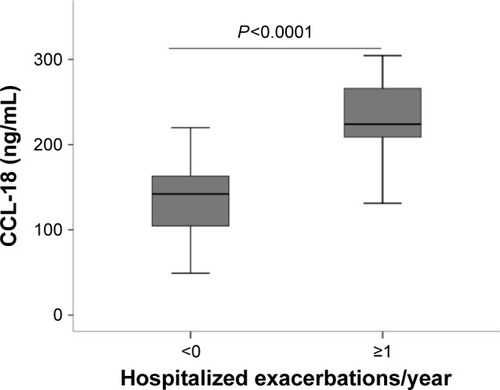
Figure 3 Receiver operator characteristic curve distinguishing COPD patients and smokers with normal spirometry AUC: 0.86 (95% CI: 0.77–0.94). The cutoff that maximizes the sum of sensitivity (83.1%) and specificity (73.7%) was >105.76 ng/mL.
Abbreviations: ROC, receiver operating characteristics curve anlaysis; CCL-18, chemokine (C-C motif) ligand 18; AUC, area under curve; CI, confidence intervals.
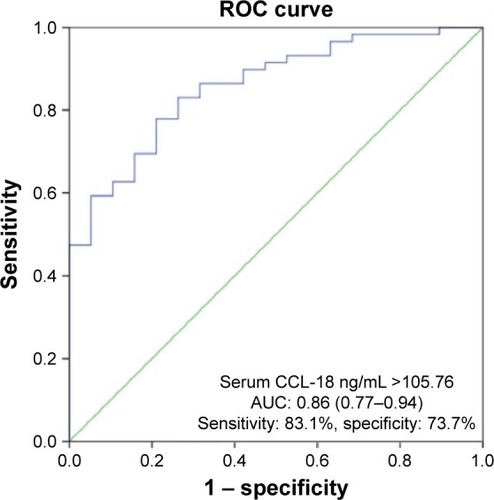
Figure 4 Receiver operator characteristic curve distinguishing COPD patients with hospitalized exacerbations from those who were not hospitalized, AUC: 0.92 (95% CI: 0.85–0.99). The cutoff that maximizes the sum of sensitivity (88%) and specificity (88.2%) was >108.71 ng/mL.
Abbreviations: ROC, receiver operating characteristics curve anlaysis; CCL-18, chemokine (C-C motif) ligand 18; AUC, area under curve; CI, confidence intervals.
Results
Subject characteristics
Sixty COPD patients and 20 NSp patients were consecutively enrolled in the study. The characteristic and clinical features of the study subjects are outlined in . Male sex was more dominant among COPD patients. When the risk factors for COPD were analyzed, although only 15% of the COPD patients were current smokers, 85% were ex-smokers while 80% of the NSp group were current smokers. According to the GOLD criteria, ~80% of the overall COPD patients had spirometrically moderate or severe disease ().
Of the 60 COPD patients, 27 (45%) had frequent exacerbations and 33 (55%) infrequent exacerbations in the previous 12 months. shows the clinical characteristics of the IE-COPD and FE-COPD patients. FE-COPD patients were more likely to have higher smoking exposure, poorer FEV1 %predicted and FEV1/FVC% compared with IE-COPD patients. The mMRC, CAT scores, and BODE index were significantly higher; while 6MWD, and the CCI indices were lower in FE-COPD group when compared with IE-COPD patients (). FE-COPD group had significantly more exacerbations requiring hospitalization compared to IE-COPD patients (P<0.0001).
Of the 60 COPD patients, 25 (41.7%) reported a total of 47 exacerbations requiring hospitalization in the previous 12 months prior to study admission. Of those 25, 15 (60%) reported multiple episodes. The clinical characteristics of patients who had at least one hospitalized exacerbation versus those who were not hospitalized are summarized in . Patients with at least one hospitalized exacerbation were older. Airflow limitation, dyspnea, CAT scores, functional exercise capacity, and the BODE index were significantly worse in COPD patients who had at least one hospitalized exacerbation ().
Serum CCL-18 levels
The serum CCL-18 levels were elevated in COPD patients when compared to the NSp group (180.3±75.5 vs 95.4±38.2 ng/mL, P<0.0001). Serum CCL-18 values did not differ significantly between the IE-COPD and FE-COPD groups, although there was a trend for FE-COPD to be higher (167.9±76.5 vs 195.9±72.6 ng/mL, P=0.09) (). Importantly, levels of serum CCL-18 were significantly higher in COPD patients who had at least one hospitalized exacerbation compared to those who had not been hospitalized (P<0.0001, ). There was no difference in serum CRP levels between study groups stratified by either exacerbation phenotype or patients with a history of exacerbations requiring hospitalization ( and ).
A ROC curve analysis was carried out to evaluate the sensitivity, specificity, and the diagnostic accuracy of the serum CCL-18 levels in distinguishing COPD from NSp. The serum CCL-18 level with a threshold of 105.76 ng/mL discriminated COPD from NSp with an 83.1% sensitivity, 73.7% specificity (AUC: 0.86; 95% confidence interval [CI]: 0.77–0.94; ). In order to identify the optimum serum CCL-18 concentration threshold which would discriminate COPD patients with hospitalized exacerbations from those who were not hospitalized, a separate ROC curve analysis was performed. The results showed that serum CCL-18 level with a threshold of 181.71 ng/mL could discriminate COPD patients with hospitalized exacerbations from those who were not hospitalized with an 88% sensitivity and 88.2% specificity (AUC: 0.92; 95% CI: 0.85–0.99; ).
The serum CCL-18 levels were not associated with the severity of COPD based on GOLD criteria or with the updated multidimensional COPD strategy categories (158.0±58.6; 168.8±52.8; 164.3±65.5; 188.2±73.4 ng/mL for A, B, C, and D categories respectively; P>0.05).Citation1 In order to better understand whether smoking status was a determinant of serum CCL-18 levels, serum CCL-18 concentrations in current versus ex-smokers in both the groups were compared. In the COPD group, there was no difference in median concentrations of serum CCL-18 between current and ex-smokers (208.0±122.2 vs 175.3±64.3 ng/mL, respectively, P=0.59). Although, CCL-18 levels were higher in ex-smokers compared to current smokers in NSp (117.3±47.6 vs 89.5±34.9 ng/mL), but the difference failed to reach statistical significance level (P=0.18; data not shown).
Correlation of serum CCL-18 with exacerbations, clinical and functional features of COPD
In the COPD group, there was a significant association between the number of COPD exacerbations and CCL-18 (Spearman correlation coefficient (r) of 0.30; P=0.026). Importantly, serum CCL-18 level had a stronger correlation with the number of exacerbations requiring hospitalization (r=0.68, P<0.0001, ). Serum CCL-18 levels were inversely correlated with the postbronchodilator FEV1 %predicted and postbronchodilator FEV1/FVC. Elevated serum CCL-18 levels were associated with higher dyspnea perception on mMRC scale and also higher symptom scores on CAT. Decreased exercise capacity as measured by 6MWD and resting oygen saturation were inversely related to serum CCL-18 levels. There was a significant association between CCI and serum CCL-18 levels and between the serum CCL-18 levels and BODE index. Serum CCL-18 levels were positively correlated with the smoking exposure, expressed as pack-years ().
Multivariable analysis performed to define risk factors for exacerbations requiring hospitalization identified only serum CCL-18 levels (odds ratio: 1.05; 95% CI: 1.01–1.09, P=0.014) as independent predictors for hospitalized exacerbations ().
Discussion
This study sought to evaluate the serum CCL-18 levels in COPD patients subgrouped by the frequency of exacerbation, and the presence of hospitalized exacerbations in the previous 12 months. The main findings of this study are as follows: first, it was found that serum CCL-18 levels are elevated in COPD patients relative to NSp participants. Serum CCL-18 level >105.76 had a sensitivity of 83% and specificity of 74% for identifying COPD patients (AUC: 0.86). Second, it was observed that serum CCL-18 levels clearly presented significant associations with important clinical correlates of COPD such as lung functions, smoking exposure, aging, symptom scales, functional exercise capacity, and exacerbation frequency. Most importantly, serum CCL-18 levels were found to be significantly higher in COPD patients who had experienced at least one exacerbation during the previous year. ROC analysis revealed that a serum CCL-18 level of 181.71 ng/mL could differentiate COPD patients with hospitalized exacerbations in the previous 12 months from those who were not hospitalized with an 88.0% sensitivity and 88.2% specificity (AUC: 0.92). CCL-18 levels have strong correlations to the frequency of exacerbations requiring hospitalization, and it is an independent risk factor for hospitalized exacerbations in the multivariable analysis. Last, a trend for CCL-18 level to be higher among FE-COPD than IE-COPD patients (P=0.09) was observed.
COPD is known as a disease of systemic inflammation. As the identification of biomarkers in COPD is a developing field, a topic of active research is the utility of biomarkers in improving subphenotyping of COPD patients.Citation24 CCL-18 is mainly expressed by monocytes/macrophages and immature dendritic cells. It is involved in primary immune responses and induces collagen production in lung fibroblasts.Citation25 CCL-18 was elevated in various fibrotic lung diseases such as idiopathic pulmonary fibrosis, idiopathic interstitial pneumonia, systemic sclerosis, sarcoidosis, and hypersensitivity pneumonitis.Citation11,Citation26,Citation27 Similar to findings reported in two large cohorts (the Lung Health Study and ECLIPSE),Citation12 it was observed that there was a marked increase in serum CCL-18 levels of COPD patients compared to NSp patients.
Macrophages play a key role in respiratory defense mechanisms. They have the possibility to morph into different phenotypes (M1, M2, M2-like macrophages) depending on the signals they receive from the micro-environment. M2 macrophages have poor antigen-presenting capabilities; they play a role in physiological/pathological tissue remodeling, maintenance, and progression of fibrosis; and they are considered to be wound-healing macrophages.Citation28 CCL-18 was shown to be a macrophage differentiation factor and to induce an M2 spectrum macrophage phenotype.Citation29 There is an accumulation of M2 macrophages and, therefore, abundant collagen deposition in idiopathic pulmonary fibrosis (IPF) patients’ lungs.Citation30 The maintenance and progression of pulmonary fibrosis are postulated to be associated with M2 macrophages.Citation31 There is also evidence supporting the role of M2 macrophage activation and dysregulation in COPD.Citation28 Shaykhiev et al showed that M2 genes in bronchoalveolar lavage macrophages were upregulated after smoking; and this finding is more pronounced in smokers with COPD.Citation32 Biomarker studies performed in COPD and IPF patients pointed out an overlap in elevation of several biomarkers (interleukin-6, interleukin-8, matrix metalloproteinase-1,7,9) including CCL-18 in both the diseases.Citation31 Accordingly, it is suggested that both the diseases may share a similarity in the pathogenesis. Cigarette smoke exposure is a common and dominant risk factor for the development of both those chronic progressive parenchymal lung diseases. M2 macrophages are defective in phagocytosis and inefficient supporters of host defense mechanisms. For this reason, it is suggested that M2 macrophage accumulation may be responsible for repeated pulmonary infections and frequent exacerbations in both COPD and IPF patients.Citation33
Despite a trend for CCL-18 to be higher in patients experiencing frequent exacerbations, the difference failed to achieve statistical significance in our study. In their study exploring factors associated with change in exacerbation frequency in the ECLIPSE cohort consisting of COPD patients, Donaldson et al observed higher serum CCL-18 levels in frequent exacerbators at baseline compared with the infrequent exacerbators.Citation16 But, CCL-18 was not an imminent factor associated with changes in the exacerbation frequency categories of COPD patients.Citation16 It seems possible that the sample size might not be large enough for a statistically significant difference in serum CCL-18 levels between IE-COPD and FE-COPD groups to be observed. On the other hand, the study was successful in showing the significant correlation between serum CCL-18 levels and the frequency of the overall COPD exacerbations and exacerbations requiring hospitalization. One possible explanation for this finding might be that CCL-18 − a differentiation factor inducing M2 macrophage phenotype − may be responsible for repeated exacerbations driven by an endogenous M2-type macrophage inflammation. Importantly, serum CCL-18 levels of COPD patients who had at least one hospitalized exacerbation in the previous year were significantly higher compared to those who did not require hospitalization. This study was also able to define a threshold of serum CCL-18 >181.71 ng/mL that differentiates COPD patients with hospitalized exacerbations from those who were not hospitalized with a high sensitivity and specificity. Whether M2-type macrophage activation is responsible for severe COPD exacerbations requiring hospitalization is unknown. It is believed that further research profiling cytokines and macrophages is required to understand the pathomechanisms for frequent exacerbations in COPD.
The GOLD guidelines acknowledge the importance of frequent exacerbations (defined as ≥2 events/year) in the disease course of COPD. FE and IE phenotypes are recognized as important COPD phenotypes that influence the clinical management of the patient.Citation1 In the present study, frequent exacerbators were more likely to have a more severe airflow limitation consistent with the previous studies reporting an increase in exacerbation frequency as disease severity rises.Citation8,Citation34 Furthermore, FE-COPD patients had significantly higher CAT and mMRC scores than the IE-COPD group, also consistent with previous reports.Citation35,Citation36 Al Ahmari et al observed a 54 m reduction in exercise capacity in 6MWD in FE-COPD compared to IE-COPD exacerbators.Citation37 Interestingly, an even greater difference was observed in 6MWD between IE-COPD and FE-COPD groups (380±68 vs 235±114 m, P<0.0001, respectively). One explanation for this finding might be that the frequent exacerbator COPD group in this study suffered from more severe airflow obstruction. It was also found that FE-COPD patients had higher BODE indices than the infrequent exacerbators. Recently, it was shown that the BODE index – a predictor of survival in COPD – was also a good predictor of the likely number of exacerbations in COPD patients.Citation38 Overall, the results confirm that the frequent exacerbator phenotype is a distinct subgroup in COPD with more severe clinical features and functional impairment. It is also shown that serum CCL-18 levels were correlated to postbronchodilator FEV1/FVC, postbronchodilator FEV1 %predicted, and the composite BODE index. Similarly, Pinto-Plata et al described a significant relationship between the serum CCL-18 levels and reduced FEV1 %predicted and BODE scores.Citation13 Despite its correlation with FEV1, in our study serum CCL-18 concentrations did not differ across the GOLD stages, in concurrence with the findings of both Sin et al and Pinto-Plata et al.Citation12,Citation13 Importantly, it was observed that CCL-18 had significant correlations with dyspnea, CAT symptom score, functional exercise capacity, the composite BODE index, oxygen saturation, and comorbidity impact. This study thus demonstrates a wide association between serum CCL-18 levels and hospitalized exacerbations as well as a wide range of prognostic and clinical COPD parameters.
Preliminary data support that CCL-18 expression can be modified by acute effects of smoking.Citation39 The present study design does not enable us to evaluate the effects of acute smoking on CCL-18 in the study population; however, in the COPD group, CCL-18 levels were higher in current smokers than in ex-smokers (P=0.59), whereas in the NSp group, they were higher in ex-smokers than in current smokers (P=0.18), albeit with no significant difference. Investigating both the Lung Health Study and ECLIPSE cohorts, Sin et al reported that COPD patients who were ex-smokers had higher serum CCL-18 expression than current smokers.Citation12 It is possible that the lack of association between smoking status and serum CCL-18 concentration in the present study may be a result of inadequate statistical power rather than a true lack of association. Sin et al also reported that total smoking exposure was not significantly associated with the serum CCL-18 level. Interestingly, the present study has found a positive correlation between the total smoking exposure (pack-years of smoking) and the serum CCL-18 expression (r=0.45, P<0.0001). Further investigations are needed to clarify the effect of smoking on CCL-18, and whether this biomarker plays a role in the COPD pathogenesis.
There are some limitations to this study. First, this study had a cross-sectional design. The number of COPD exacerbations during the previous year was recorded based on each patient’s self-report and available medical records. A prospective cohort study would enable us to evaluate the association of serum CCL-18 levels with the future exacerbations. However, it has been recently shown in the ECLIPSE cohort that hospitalized exacerbations of the past year were a strong predictor of future exacerbations requiring hospitalization.Citation4 Second, despite CCL-18 being a predominantly pulmonary chemokine, it may be secreted by the myeloid cells, and other organs such as liver, bone marrow, and so on. Hence, measuring CCL-18 production in bronchoalveolar lavage fluid might be more revealing. However, a close correlation between CCL-18 concentration in serum and bronchoalveolar lavage was observed by Prasse et al suggesting that CCL-18 production within the lungs was reflected by the CCL-18 levels in the serum of smokers.Citation11 Third, the prominent role of inflammatory pathways in exacerbations of COPD is well known. Although it is recognized that CRP independently contributes to COPD-related important clinical outcomes, similar to the analysis by Müllerova et al in the ECLIPSE cohort, the present study did not observe CRP as a significant determinant for hospitalized COPD exacerbations.Citation4 On the other hand, elevated fibrinogen levels were reported as independent risk factors for exacerbations and future hospitalized exacerbations in COPD.Citation4,Citation40 Since serum fibrinogen level was not analyzed, the relationship of CCL-18 with fibrinogen could not be evaluated. Last, previous research by Kollert et al showed evidence that chronic cigarette smoking alters alveolar macrophage phenotype and CCL-18 is down-regulated in smokers.Citation39 In this regard, to be able to make a reliable evaluation of serum CCL-18 levels between COPD and NSp groups, only smokers and ex-smokers with at least 10 pack-years of smoking history were enrolled with NSp, as apparently healthy controls for our study. Since never smoker NSp healthy controls were not enrolled, our results regarding effect of smoking on CCL-18 are limited and should be interpreted with caution.
CCL-18 levels were elevated and associated with increased mortality in COPD patients of the ECLIPSE cohort.Citation12 Findings in the Lung Health Study cohort indicated serum CCL-18 as an independent risk factor for higher cardiovascular hospitalization and deaths.Citation12 In another cross-sectional study profiling inflammatory phenotypes and clinical outcomes of a cohort of COPD patients, an association between elevated serum CCL-18 level and reduced FEV1, lower exercise capacity (6MWD), and frequent exacerbations were reported.Citation13 Consistent with previous studies, it was observed that serum CCL-18 presents significant associations with all of the important clinical correlates of COPD (lung functions, smoking exposure, symptom scales, functional exercise capacity, and exacerbation frequency). Müllerova et al recently reported a comprehensive systemic inflammatory profiling (white blood cells, neutrophils, CRP, fibrinogen, and CCL-18) of the COPD patients at baseline in the ECLIPSE cohort, classified by the incidence of hospital admissions during follow-up period. Despite markers of systemic inflammation, including CCL-18 being significantly higher in COPD patients with hospitalized exacerbations compared with those without hospital admission in univariable analysis, the only inflammation markers identified as independent risk factors for future hospitalized exacerbations were serum fibrinogen and white blood cells.Citation4 The present study reports for the first time that CCL-18 levels have a strong correlation with the frequency of hospitalized exacerbations and that serum CCL-18 level is an independent risk factor for hospitalized exacerbations.
In summary, the lung-predominant chemokine, CCL-18, could be a useful biomarker in COPD. This study demonstrates that it is significantly increased in COPD, that it has a trend to increase in COPD patients with frequent exacerbations, and that it presents a marked increase in COPD patients suffering from exacerbations requiring hospitalization. It is associated with frequency of exacerbations, exacerbations requiring hospitalization, as well as functional parameters, symptom scores, and the composite BODE index. As the validity and utility of biomarkers depend on characteristics such as association with the clinical outcomes and sensitivity in detecting clinically important differences, CCL-18 seems like a promising marker in COPD. Further studies are required to determine whether this biomarker has a causal role in the disease and has association with various COPD phenotypes.
Acknowledgments
We would like to express our sincere gratitude to Richard Casaburi, PhD, MD, and Abdullah Sayiner, MD, for their significant intellectual contribution and critically reviewing the manuscript. We also acknowledge Claire Ölmez for professional editing. Some of the results of this study have been reported in the form of an abstract (Dilektasli AG, Cetinoglu ED, Uzaslan E, Budak F, Coskun F, Ursavas A, Ege E. Feasibility of serum PARC/CCL-18 levels discriminating the frequent exacerbator COPD phenotype: a case-control study. Chest. 2014;146:61A).
Disclosure
The authors report no conflicts of interest in this work.
References
- VestboJHurdSSAgustíAGGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med2013187434736522878278
- UzaslanEMahboubBBejiMThe burden of chronic obstructive pulmonary disease in the Middle East and North Africa: results of the BREATHE studyRespir Med2012106S45S5923290704
- ManninoDMBuistASGlobal burden of COPD: risk factors, prevalence, and future trendsLancet2007370958976577317765526
- MullerovaHMaselliDJLocantoreNHospitalized exacerbations of COPD: risk factors and outcomes in the ECLIPSE cohortChest20151474999100725356881
- BahadoriKFitzGeraldJMRisk factors of hospitalization and readmission of patients with COPD exacerbation – systematic reviewInt J Chron Obstruct Pulmon Dis20072324125118229562
- HurstJRVestboJAnzuetoASusceptibility to exacerbation in chronic obstructive pulmonary diseaseN Engl J Med2010363121128113820843247
- HanMKAgustiACalverleyPMChronic obstructive pulmonary disease phenotypes: the future of COPDAm J Respir Crit Care Med2010182559860420522794
- HurstJRDonaldsonGCPereraWRUse of plasma biomarkers at exacerbation of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2006174886787416799074
- BozinovskiSHutchinsonAThompsonMSerum amyloid a is a biomarker of acute exacerbations of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2008177326927818006888
- DonaldsonGCSeemungalTAPatelISAirway and systemic inflammation and decline in lung function in patients with COPDChest200512841995200416236847
- PrasseAPechkovskyDVToewsGBCCL18 as an indicator of pulmonary fibrotic activity in idiopathic interstitial pneumonias and systemic sclerosisArthritis Rheum20075651685169317469163
- SinDDMillerBEDuvoixASerum PARC/CCL-18 concentrations and health outcomes in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med201118391187119221216880
- Pinto-PlataVCasanovaCMüllerovaHInflammatory and repair serum biomarker pattern. Association to clinical outcomes in COPDRespir Res20121317122906131
- BurgeSWedzichaJACOPD exacerbations: definitions and classificationsEur Respir J2003414653
- CelliBRMacNeeWStandards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paperEur Respir J200423693294615219010
- DonaldsonGCMüllerovaHLocantoreNFactors associated with change in exacerbation frequency in COPDRespir Res2013147923899210
- BestallJPaulEGarrodRGarnhamRJonesPWedzichaJUsefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary diseaseThorax199954758158610377201
- JonesPHardingGBerryPWiklundIChenWLeidyNKDevelopment and first validation of the COPD Assessment TestEur Respir J200934364865419720809
- YorgancıoğluAPolatlıMAydemirÖReliability and validity of Turkish version of COPD assessment testTuberk Toraks2011604314320 Turkish
- MillerMRCrapoRHankinsonJGeneral considerations for lung function testingEur Respir J200526115316115994402
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function LaboratoriesATS statement: guidelines for the six-minute walk testAm J Respir Crit Care Med2002166111112091180
- CelliBRCoteCGMarinJMThe body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary diseaseN Engl J Med2004350101005101214999112
- CharlsonMSzatrowskiTPPetersonJGoldJValidation of a combined comorbidity indexJ Clin Med1994471112451251
- NicholasBLSearch for biomarkers in chronic obstructive pulmonary disease: current statusCurr Opin Pulm Med201319210310823361193
- SchutyserERichmondAVan DammeJInvolvement of CC chemokine ligand 18 (CCL18) in normal and pathological processesJ Leukoc Biol2005781142615784687
- KoderaMHasegawaMKomuraKYanabaKTakeharaKSatoSSerum pulmonary and activation-regulated chemokine/CCL18 levels in patients with systemic sclerosis: a sensitive indicator of active pulmonary fibrosisArthritis Rheum20055292889289616142750
- PrasseAPechkovskyDVToewsGBA vicious circle of alveolar macrophages and fibroblasts perpetuates pulmonary fibrosis via CCL18Am J Respir Crit Care Med2006173778179216415274
- BoorsmaCEDraijerCMelgertBNMacrophage heterogeneity in respiratory diseasesMediators inflamm2013201376921423533311
- SchraufstatterIUZhaoMKhaldoyanidiSKDiScipioRGThe chemokine CCL18 causes maturation of cultured monocytes to macrophages in the M2 spectrumImmunology2012135428729822117697
- StahlMSchuppJJägerBLung collagens perpetuate pulmonary fibrosis via CD204 and M2 macrophage activationPLoS One2013811e8138224278429
- DoyleTJPinto-PlataVMorseDCelliBRRosasIOThe expanding role of biomarkers in the assessment of smoking-related parenchymal lung diseasesChest201214241027103423032451
- ShaykhievRKrauseASalitJSmoking-dependent reprogramming of alveolar macrophage polarization: implication for pathogenesis of chronic obstructive pulmonary diseaseJ Immunol200918342867288319635926
- MurrayLAHogaboamCMMechanisms promoting chronic lung diseases: will targeting stromal cells cure COPD and IPF?IrusenEMLung Diseases – Selected State of the Art ReviewsInTech2012 Available from: http://www.intechopen.com/books/lung-diseases-selected-state-of-the-art-reviews/mechanisms-promoting-chronic-lung-diseases-will-targeting-stromal-cells-cure-copd-and-ipf-Accessed July 29, 2016
- BeehKMGlaabTStowasserSCharacterisation of exacerbation risk and exacerbator phenotypes in the POET-COPD trialRespir Res20131411624168767
- MackayAJDonaldsonGCPatelARJonesPWHurstJRWedzichaJAUsefulness of the Chronic Obstructive Pulmonary Disease Assessment Test to evaluate severity of COPD exacerbationsAm J Respir Crit Care Med2012185111218122422281834
- LeeSJLeeSHKimYEClinical features according to the frequency of acute exacerbation in COPDTuberc Respir Dis (Seoul)201272436737323227078
- Al AhmariADPatelAKowlessarBCOPD exacerbation frequency phenotype and exercise capacityAm J Respir Crit Care Med2013187A1440
- MarinJMCarrizoSJCasanovaCPrediction of risk of COPD exacerbations by the BODE indexRespir Med2009103337337819013781
- KollertFProbstCMüller-QuernheimJZisselGPrasseACCL18 production is decreased in alveolar macrophages from cigarette smokersInflammation200932316316819357939
- GroenewegenKHPostmaDSHopWCWieldersPLSchlosserNJWoutersEFIncreased systemic inflammation is a risk factor for COPD exacerbationsChest2008133235035718198263