Abstract
Objective
Older people with reduced respiratory muscle strength may be misclassified as having COPD on the basis of spirometric results. We aimed to evaluate the relationship between lung function and grip strength in older hospitalized patients without known airways disease.
Methods
Patients in acute medical wards were recruited who were aged ≥70 years; no history, symptoms, or signs of respiratory disease; Mini Mental State Examination ≥24; willing and able to consent to participate; and able to perform hand grip and forced spirometry. Data including lung function (forced expiratory volume in 1 second [FEV1], forced vital capacity [FVC], FEV1/FVC, peak expiratory flow rate [PEFR], and slow vital capacity [SVC]), grip strength, age, weight, and height were recorded. Data were analyzed using descriptive statistics and linear regression unadjusted and adjusted (for age, height, and weight).
Results
A total of 50 patients (20 men) were recruited. Stronger grip strength in men was significantly associated with greater FEV1, but this was attenuated by adjustment for age, height, and weight. Significant positive associations were found in women between grip strength and both PEFR and SVC, both of which remained robust to adjustment.
Conclusion
The association between grip strength and PEFR and SVC may reflect stronger patients generating higher intrathoracic pressure at the start of spirometry and pushing harder against thoracic cage recoil at end-expiration. Conversely, patients with weaker grip strength had lower PEFR and SVC. These patients may be misclassified as having COPD on the basis of spirometric results.
Introduction
There is concern that older people with reduced respiratory muscle strength may be misclassified as having COPD on the basis of spirometric results and receive unnecessary and potentially harmful treatment. With increasing age, the smaller pulmonary airways more readily collapse and forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), and forced expiratory flow decrease; there is an increase in functional residual capacity and expiratory reserve volume, residual volume increases, and there is little change in total lung capacity.Citation1–Citation3 In addition with aging, there is a decreased respiratory response to hypoxemia and hypercapnia and a reduced perception of raised resistance of the airway.Citation2 There is a loss of synovial joints between the sternum and the costal cartilages reducing chest wall compliance and tension forces, leading to reduced maximal respiratory pressure and decreased muscle mass and strength of accessory respiratory muscles.Citation4 It has also been observed that there is a significant decrease by 25% in the diaphragm strength in the older compared with young adults.Citation5 One study has observed that inspiratory (mainly diaphragmatic) strength has been considered to be the most relevant in relation to function, fatigue, and training.Citation6
With aging, there is a triad of loss of muscle mass, strength, and function defined as sarcopenia. This is common and has serious consequences including increased risk of current and future falls, dependency, hospitalization, and mortality. Grip strength is recommended as a simple standardized clinical measure used in the diagnosis of sarcopenia.Citation7 Age-associated skeletal muscle changes may impact respiratory muscle function, and a positive correlation between grip strength and inspiratory and expiratory muscle strength has been demonstrated.Citation8–Citation10 Reduced lung function (in particular FEV1 and FVC) after adjusting for age, smoking, and physical activity has been demonstrated with reduced skeletal muscle mass in Korea.Citation11
COPD is defined by the Global initiative for chronic Obstructive Lung Disease (GOLD) by symptoms, exposure to risk factors (namely smoking), family history, and confirmation with spirometry with a postbronchodilator FEV1/FVC <0.70 and postbronchodilator FEV1 (to assess degree of airflow limitation).Citation12
Discord over the standardized definition of COPD across international groups (whether a fixed ratio, use of standardized age-related reference spirometry ranges, or lower limit than normal spirometry values) makes it difficult to compare the prevalence of COPD across populations and across studies due to the lack of standardized protocol.Citation13 FEV1/FVC ratio decreases with aging and is included in the GOLD definition of COPD using the criteria of postbronchodilator FEV1/FVC <0.70. There is a decrease in FEV1 with aging likely to be due to age-related airway compliance changes and this is incorporated in the GOLD definition to assess the severity of airflow limitation. Both criteria have potential to lead to increasing diagnosis of COPD in older nonsmoking patients with no lung pathology.Citation14 Normal reference spirometry values have been defined in older age groups; however, these are not included in the international definition of COPD.Citation15,Citation16
Peak expiratory flow rate (PEFR) in older adults is an inexpensive measure, assessed alongside other respiratory function and used in previous studies evaluating grip strength, respiratory muscle strength, and lung function.Citation17 It measures maximal expiratory flow, is effort dependent, and represents airflow through larger caliber airways.Citation18 PEFR has been used to assess adherence and benefit of treatments for airways disease and one of its limitation is the variability in performance in older persons. Older age, reduced body size, smoking, cardiovascular, respiratory, and cognitive diseases are associated with a reduced PEFR.Citation17,Citation19
Slow vital capacity (SVC) may be easier for some older adults who have difficulty coordinating the more FVC due to factors, such as reduced cognitive ability, coughing during the maneuver, weakness, or fatiguability.Citation20 Again SVC is an inexpensive measure that can be tested alongside other respiratory measures using the same spirometry equipment. However, it is not incorporated in the international definitions of airways obstruction. It is also recognized that some older adults with cognitive impairment may be unable to perform both SVC and FVC.Citation20
There is increasing interest in the relationship between sarcopenia, respiratory muscle strength, and lung function in patients with COPD.Citation21–Citation23 However, there has been very limited evaluation of sarcopenia, respiratory muscle strength, and lung function in older people without known airways disease. This study aimed to evaluate the relationship of grip strength and lung function in older hospital patients without known respiratory disease.
There is an increasing recognition of an association between muscle strength and lung function in people with COPD. It is unknown whether there is a relationship between grip strength and lung function in older non-smoking adults. In this study, older non-smoking patients with weaker grip strength had lower PEFR and SVC. Reduced spirometric lung function measurements in weaker older individuals may contribute to misdiagnosis of COPD.
Materials and methods
Study design and ethics
This was a prospective study on patients aged ≥70 years admitted to acute older people’s wards at a university hospital in the UK over a 6-month period. Southampton and South West Hampshire Research Ethics Committee gave approval for this study, which was registered with ClinicalTrials.gov (NCTO1647204).
Participants
The inclusion criteria for recruitment were age >70 years, a history of never smoking or trivial smoking <1 year, no history, symptoms or signs of respiratory disease, and negative for bronchial obstruction on the respiratory symptom questionnaire.Citation24
Exclusion criteria were met if any participant was unable to meet all of the inclusion criteria, had a Mini Mental State Examination (MMSE) score of <24, or had any contraindication to performing spirometry according to the Association for Respiratory Technology and Physiology (ARTP) guidelines.Citation25 These contraindications included hemoptysis; pneumothorax; unstable angina; myocardial infarction in the last one month; pulmonary embolism; thoracic, abdominal, or cerebral aneurysms; recent eye surgery; nausea or vomiting; and recent thoracic or abdominal surgery. In addition, if participants appeared nonspecifically unwell or nursing staff had concerns about participation, then they were not approached.
A convenience sample of eligible patients (based on the researcher’s availability) were approached for recruitment, then given a patient information sheet and opportunity to ask further questions before written informed consent was obtained. Each participant was taken through the brief respiratory questionnaire to ensure they had no symptoms that would affect carrying out the spirometry or exclude them from the study: any positive response to the questionnaire excluded recruitment to the study. Participants were also asked about any contraindication to performing spirometry according to the ARTP guidelines, and this was confirmed on review of case notes before performing spirometry with the participants’ permission.
Data collection
Participants’ height was calculated from ulna length measurement,Citation26 as the majority of participants were unable to stand. Weight was measured using sitting scales at the bedside. Body mass index was calculated by dividing body weight by the square of height (kg/m2). Cognitive function was assessed using the MMSE,Citation27 which has been an established screening tool in spirometry studies in older people.
A calibrated Jamar dynamometer was used to measure grip strength using a standard protocol. Three measurements were recorded for each hand to the nearest 1 kg and the maximum grip recorded.Citation28 A Microlab Portable spirometer was used to measure FEV1, FVC, PEFR (best of five measurements recorded), and SVC (best of three measurements recorded). The spirometer was calibrated for each assessment. Measurements were recorded in the sitting position, feet on the floor, spine erect, and without support for the upper limbs. Repeatability was considered to be adequate when there was a difference of ≤0.15 L between the maximum and the next largest FVC and between the maximum and next largest FEV1. In patients with FVC ≤1 L, a difference of ≤0.10 L was used. SVC attempts were considered to be acceptable if the individual breathed in to total lung capacity then breathed out until flow had ended for at least 1 second. SVC measurements were considered to be repeatable if the two highest attempts varied by ≤0.2 L. The highest recording was taken for each measurement. However, to assure the quality of these data, two observers reviewed spirograms of each patient separately and together to see if they reflected adequate performance.Citation29
Statistical analysis
Data were entered into a database and analyzed using IBM SPSS Statistics 20 software separately for men and women. Normality of variables was assessed using visual inspection of histograms and skewness. Mean and standard deviation, median and interquartile ranges were used to describe the participants’ demographic and clinical characteristics, grip strength, and spirometry results. Comparison between men and women was conducted using independent sample t-tests and the Mann–Whitney U-test accordingly. The association between lung function variables and grip strength were assessed for men and women separately using linear regression analysis both unadjusted and adjusted for age, height, and weight.
Results
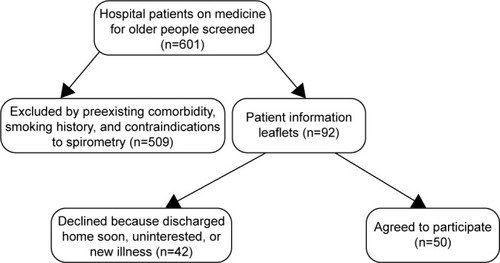
A total of 601 patients were screened over 6 months of which 509 were excluded: 58 patients with acute respiratory illness, 48 with known respiratory disease, 109 patients with more than 1 year of smoking history, 13 with acute illness, and 281 with known moderate or severe cognitive impairment. The 92 eligible patients were approached with information leaflets and of these 50 (54%) consented to take part in the study ().
Patient characteristics are recorded in . Spirometry was difficult to achieve reproducibility of the results and for patients to rehearse the technique without becoming fatigued, to ensure effort in the early part of forced expiration, and to avoid patients stopping mid-expiration. After review of 10 patients, SVC was introduced for the remaining 40 patients. SVC can be easier and more relaxed than FVC, and can avoid coughing triggered by the forced maneuver.Citation20
Table 1 Participant characteristics and their grip strength and spirometry
The association of lung function with grip strength is shown in . There was a wide variation in participants’ PEFR values. In men, grip strength was significantly associated with FEV1 but this was attenuated by adjustment for age, height, and weight. Significant associations were found in women between grip strength and PEFR and between grip strength and SVC, both of which remained robust to adjustment. No other significant relationship was found.
Table 2 Association of grip strength and lung function in the older participants
Discussion
Grip strength was significantly stronger, and lung function was significantly larger in men compared with women probably due to their larger body size allowing them to generate greater intrathoracic pressures and higher lung volumes. Stronger grip strength was significantly associated with a larger FEV1 in men, but the significance was attenuated after adjustment for age, height, and weight.
No significant relationship was found between grip strength and FEV1 in women. In line with previous reports, this study demonstrated variation in PEFR values among the participants.Citation17–Citation19 Reduced PEFR was demonstrated in women with low grip strength. Low FEV1 and low PEFR in weaker individuals could be due to increased parenchymal compliance. PEFR may be a useful measure of airflow obstruction, and change in response to treatment may be less reliable in older women with low grip strength.
Increased grip strength was associated with a larger FVC in both men and women but was not statistically significant. There was no significant association between grip strength and ratio of FEV1/FVC. This result reflected patients with a similar reduction in both FEV1 and FVC and a lack of consistency in spirometry. Importantly, SVC appeared to be a more practical and applicable lung function measure in this older patient group than FVC.
Stronger grip strength was significantly associated with larger PEFR and SVC in women but not in men. PEFR and SVC may be more significant in women in this study reflecting stronger patients generating higher intrathoracic pressure at the start of spirometry and pushing harder against thoracic cage recoil at end-expiration. Differences found between women and men may be related to smaller airways and lung volumes in women compared with men.
A relationship between grip strength and FEV1 in patients who were healthy subjects and with COPD was inferred in a recent study in India. This study demonstrated that a decrease in grip strength was associated with a decrease in FEV1 in women and in FVC in men; however, it did not adjust for age or body size.Citation30 Current studies that report FEV1/FVC do so only in the context of patients with lung pathology, smokers, or a mixed group and do not compare this to grip strength or adjust for body size.Citation31 One study showed a significant correlation between grip strength and PEFR in hospital staff but again did not adjust for age and height.Citation17 A further limitation of current research in the relationship between grip strength and lung function is a lack of standardization of instruments used and methodology particularly in assessing older subjects. There is also a lack of consensus on appropriate spirometry measures and protocols within research and agreement as to defined spirometry measures in clinical practice for diagnosing COPD.
There were limitations to the study. The sample size was small and patients with cognitive impairment, smokers >1 year, or acutely ill were excluded. The significance of this study’s findings has to be taken within this context and are preliminary findings. Recruiting participants based on the researcher’s availability may have led to potential eligible patients not being included but would not have resulted in observer bias.
This study examined individuals far older than in previous studies and this older group had difficulty maintaining the consistency to conform to the American Thoracic Society (ATS) guidelines for spirometry. We reported the maximum spirometry values rather than the mean values recognizing that with repeated testing some patients may fatigue. This could be standardized by setting limits to exclude lung function tests, for example, with FEV1/FVC >90% or <60% and abnormal spirogram patterns. Assessment of SVC in all participants would have been beneficial; however, this was not possible to obtain due to participants being discharged home. Further evaluation of SVC to measure airway obstruction particularly with those limited by coughing may be useful as a research tool and in practice.
There were also several strengths to this study. We performed it with a single researcher with trained competency in collecting data confirmed with intraobserver variability assessment. The study was carried out using calibrated instruments. The use of a standardized method for measuring grip strength was advantageous and is not usually the case in other studies in older persons. Similarly, we performed spirometry in a standardized way that would allow easy comparison to other studies.
We considered the appropriateness of performing spirometry in hospitalized patients given the potential instability of this population. Previous studies have highlighted variability in spirometry results particularly in older participants with cognitive impairment (due to an inability to coordinate or perform the test in a standardized manner), those acutely ill, and smokers (secondary to pathophysiologic changes).Citation20 Therefore, we decided to use rigorous exclusion criteria to standardize recruitment and enable comparison with other studies, although we acknowledge its limitation on sample size.
This study aimed to evaluate the relationship between grip strength and lung function in older persons and whether current guidelines may inadvertently lead to clinicians misdiagnosing and potentially treating older nonsmokers with unnecessary and potentially harmful treatment. A larger community-based study using the same rigorous methodology may provide a better understanding of this relationship.
It could be that a larger number of older persons in the community would benefit from this research due to the increasing screening programs in primary care. It may also be easier to perform grip strength and spirometry within an outpatient setting in a more consistent fashion. It has also been demonstrated in older adults that fixed ratio FEV1/FVC may better identify subjects at risk of death or hospitalization than using the lower limit of normal spirometry values.Citation32 Hence, this area of debate may be more complicated than simply disease classification.
Future work may consider review of grip strength to lung function expressed in terms of the diagnostic cutoff values for COPD using both the lower limit of normal and the fixed ratio criteria.
There may be other avenues of assessing the relationship between grip strength and spirometry in older nonsmokers using additional biochemical markers for aging and measuring FEV at the earlier part of forced expiration to increase accuracy of results before fatigability sets in.
Pulmonary rehabilitation programs are established for patients with COPD. Similarly resistance training has been recognized as important in maintaining muscle mass and strength in older people. There may be the potential for pulmonary rehabilitation programs for older people in the future to maintain respiratory muscle mass and strength.Citation32
Conclusion
Men had significantly stronger grip strength and larger FEV1, FVC, PEFR, and SVC compared with women probably because of larger body size. There was a significant association between grip strength and PEFR and grip strength and SVC after adjustment for age, height, and weight in women, which may reflect stronger patients generating higher intra-thoracic pressure at the start of spirometry and pushing harder against thoracic cage recoil at end-expiration. In men, a significant relationship was found between grip strength and FEV1, which was attenuated after adjustment for age, height, and weight, and this requires further evaluation.
Acknowledgments
SJ Holmes was supported by a British Geriatric Society start-up grant. This study was supported by the National Institute for Health Research (NIHR) Southampton Biomedical Research Centre in Nutrition, the MRC Lifecourse Epidemiology Unit, the University of Southampton and the British Geriatrics Society. HC Roberts is supported by the NIHR Collaboration for Leadership in Applied Health Research and Care (CLAHRC): Wessex. This report is independent research by the BRC and CLAHRC: Wessex. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research, or the Department of Health.
Disclosure
The authors report no conflicts of interest in this work.
References
- BrittoRRVieiraDSBotoniFABotoniALASVellosoMThe presentation of respiratory failure in elderly individualsCurr Geriatr Rep201542166173
- JanssensJPPacheJCNicodLPPhysiological changes in respiratory function associated with ageingEur Respir J199913119720510836348
- PrideNBAgeing and changes in lung mechanicsEur Respir J200526456356516204583
- JanssensJPAging of the respiratory system: impact on pulmonary function tests and adaptation to exertionClin Chest Med200526346948416140139
- TolepKHigginsNMuzaSCrinerGKelsenSGComparison of diaphragm strength between healthy adult elderly and young menAm Journal Respiratory and Critical Care Medicine19951522677682
- KimMJRespiratory muscle training: implications for patient careHeart Lung19841343333406564100
- Cruz-JentoftAJBaeyensJPBauerJMSarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older peopleAge Ageing201039441242320392703
- SummerhillEMAngovNGarberCMcCoolFDRespiratory muscle strength in the physically active elderlyLung2007185631532017917778
- DohertyTJInvited review: aging and sarcopeniaJ Appl Physiol20039541717172712970377
- PollaBD’AntonaGBottinelliRReggianiCRespiratory muscle fibres: specialisation and plasticityThorax200459980881715333861
- JeonYShinMKimMLow pulmonary function is related with a high risk of sarcopenia in community-dwelling older adults: the Korea national health and nutrition examination survey (KNHANES) 2008–2011Osteoporos Int201517
- Global Initiative for Chronic Obstructive Lung Disease (GOLD).Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease2015 Available from: http://www.goldcopd.orgAccessed August 14, 2016
- SwanneyMPRuppelGEnrightPLUsing the lower limit of normal for the FEV1/FVC ratio reduces the misclassification of airway obstructionThorax BMJ20086310461051
- HardieJABuistASVollmerWMEllingsenIBakkePSMørkveORisk of over-diagnosis of COPD in asymptomatic elderly never-smokersEur Respir J20022051117112212449163
- CrapoROMorrisAHGardnerRMReference spirometric values using techniques and equipment that meet ATS recommendationsAm Rev Respir Dis19811236596647271065
- EnrightPLKronmalRAHigginsMSchenkerMHaponikEFSpirometry reference values for women and men 65 to 85 years of age. Cardiovascular health studyAm Rev Respir Dis19931471251338420405
- HornbySTNunesQMHillmanTERelationships between structural and functional measures of nutritional status in a normally nourished populationClin Nutr20052442142615896429
- HegewaldMJLeforMJJensenRLPeak expiratory flow is not a quality indicator: peak expiratory flow variability and FEV1 are poorly correlated in an elderly populationChest200713151494149917400677
- CookNRAlbertMSBerkmanLFBlazerDTaylorJOHennekensCHInterrelationships of peak expiratory flow rate with physical and cognitive function in the elderly: MacArthur Foundation Studies of AgingJ Gerontol A Biol Sci Med Sci1995506M317M3237583803
- AllenSCCharltonCBackenWWarwick-SandersMYeungPPerforming slow vital capacity in older people with and without cognitive impairment–is it useful?Age Ageing2010359588591
- JonesSEMaddockMKonSSSarcopenia in COPD: prevalence, clinical correlates and response to pulmonary rehabilitationThorax20157021321825561517
- Orozco-LeviMStructure and function of the respiratory muscles in patients with COPD: impairment or adaptation?Eur Respir J2003224641s51s
- HeunksLMDekhuiizenPNRespiratory muscle function and free radicals: from cell to COPDThorax20005570471610899251
- VenablesKMFarrerNSharpLGraneekBJNewman TaylorAJRespiratory symptoms questionnaire for asthma epidemiology: validity and reproducibilityThorax1993482142198497818
- CooperBGAn update on contraindications for lung function testingThorax201166871472320671309
- Malnutrition Advisory GroupAlternative measurements: instructions and tables, British Association for Parenteral and Enteral Nutrition2013 Available from: www.bapen.org.ukAccessed August 12, 2016
- FolsteinMFFolsteinSEMcHughPRMini-Mental state: a practical method for grading the cognitive state of patients for the clinicianJ Psychiatr Res19751231891981202204
- RobertsHCDenisonHJMartinHJA review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approachAge Ageing201140442342921624928
- MillerMRHankinsonJBrusascoVStandardisation of spirometryEur Respir J200526231933816055882
- ShahSNaharPVaidyaSSalviSUpper limb muscle strength and endurance in chronic obstructive pulmonary diseaseIndian J Med Res2013138449249624434255
- OzdenOZeynepEKokturkNKaratasGKHand grip strength in patients engaged in pulmonary rehabilitation program during COPD exacerbationEur Respir J2011386 Suppl 551247
- QuanjerPHDiagnosing COPD: high time for a paradigm shiftRespir Care201156111861186322035829