Abstract
Background
Bronchiectasis is characterized by permanent dilatation of the bronchial tree caused by recurrent airway infection and inflammation. The association of atherosclerosis and inflammation is well established. However, studies on the relationship between bronchiectasis and stroke are scant.
Objective
We conducted a population-based cohort study to investigate the incidence and risk of ischemic stroke in patients with bronchiectasis.
Methods
Data of 1,295 patients newly diagnosed as bronchiectasis between 2000 and 2008 were retrieved from the Taiwan National Health Insurance Research Database. A total of 6,475 controls without bronchiectasis at a ratio of 5:1 were randomly selected from the general population based on frequency-matched age and sex to the patients. All participants were followed up to the date of ischemic stroke development, censoring, or the end of 2010. The Cox proportional hazard model was used to identify the risk of ischemic stroke in patients with bronchiectasis compared with those without bronchiectasis.
Results
The patients with bronchiectasis exhibited a higher incidence rate of ischemic stroke (9.18 vs 4.66 per 1,000 person-years) than the patients without bronchiectasis, with an adjusted hazard ratio of 1.74 (95% confidence interval =1.28–2.35). The patients with bronchiectasis and any comorbidities exhibited a 2.66-fold adjusted hazard ratio of ischemic stroke compared with those with neither bronchiectasis nor comorbidity (95% confidence interval =1.85–3.84). The patients with bronchiectasis carried a dose response of ischemic stroke according to the number of emergency visits and hospitalizations per year.
Conclusion
This study indicated that bronchiectasis is an independent risk factor of ischemic stroke.
Plain language summary
Bronchiectasis is characterized by recurrent airway infection and inflammation. The association of atherosclerosis and inflammation is well established. However, studies on the relationship between bronchiectasis and stroke are scant. Therefore, we conducted a population-based cohort study to determine the incidence and risk of ischemic stroke in patients with bronchiectasis.
The patients with bronchiectasis exhibited a higher incidence rate of ischemic stroke (9.18 vs 4.66 per 1,000 person-years) than the patients without bronchiectasis, with an adjusted hazard ratio (aHR) of 1.74 (95% confidence interval [CI] =1.28–2.35). The patients with bronchiectasis carried a dose response of ischemic stroke according to the number of emergency visits and hospitalizations per year.
This study indicated that bronchiectasis is an independent risk factor of ischemic stroke. Clinicians should take proactive strategies to carefully assess risk factors of stroke, and holistically treat patients with bronchiectasis.
Introduction
Bronchiectasis is characterized by a permanent dilatation and thickening of the bronchial tree caused by recurrent airway infection and inflammation. Common symptoms of bronchiectasis include viscid sputum production, hemoptysis, dyspnea, and weight loss.Citation1,Citation2 High-resolution computed tomography (HRCT) is the recognized gold standard for the diagnosis of bronchiectasis.Citation3,Citation4
Bronchiectasis can cause substantial impact not only on patients’ physical and psychosocial well-being but also on morbidity and mortality.Citation2,Citation5 A recent study from the United Kingdom reported an association between bronchiectasis and increased prevalence of coronary heart disease and stroke.Citation6 The probable pathology is that leukocyte recruitment and inflammatory mediators may activate atherogenesis.Citation7,Citation8 Libby reported that leukocyte recruitment and expression of proinflammatory cytokines characterize early atherogenesis and that malfunction of inflammatory mediators mutes atheroma formation in mice.Citation7,Citation8 It was also observed that autoimmune diseases such as rheumatoid arthritis, a chronic systemic inflammation, predispose to atherosclerosis and cardiovascular disease.Citation7,Citation8 Systemic inflammation can increase intima medial thickness in carotid artery and the presence of carotid plaque.Citation9,Citation10 Hence, patients who have bronchiectasis and experience frequent respiratory infections may have an increased risk of ischemic stroke.
Stroke is the rapid development of a focal neurologic deficit caused by a disruption of blood supply to the corresponding area of brain. It can lead to the most devastating impairment of physical and physiological function and therefore result in a great social and economic burden worldwide.Citation11 In addition, stroke remains the second leading cause of death in the world and in Taiwan as well.Citation12–Citation14 Medical comorbid disorders, such as hypertension, diabetes, hyperlipidemia, coronary artery disease (CAD), congestive heart disease (CHF), and atrial fibrillation (AF), are well-established risk factors of stroke.Citation15–Citation19 Recent studies have indicated that chronic obstructive pulmonary disease (COPD) is also associated with an increased risk of stroke.Citation20,Citation21 However, studies on the relationship between bronchiectasis and stroke for an Asian population are scant. Therefore, in this study, we conducted a nationwide population-based cohort study to evaluate the incidence and risk of ischemic stroke in patients with bronchiectasis in Taiwan.
Methods
Data source
Single-payer National Health Insurance (NHI) program started from March 1, 1995, in Taiwan. More than 99.9% of Taiwan’s citizens have been enrolled in this program in 2015.Citation22 The National Health Insurance Research Database (NHIRD) was provided by the National Health Insurance Administration (NHIA, formerly named Bureau of National Health Insurance) and managed by the National Health Research Institute. We used the Longitudinal Health Insurance Database (LHID), a sub-database of NHIRD, comprising data of 1 million randomly selected beneficiaries of the NHI program in 2000. The database has been released for public research after deidentification of the beneficiaries. A variety of outpatient and inpatient medical records are included in the LHID. Diagnoses are coded according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). Previous studies have validated the diagnosis of ICD-9-CM codes in the database.Citation23–Citation25 This study was approved by the Institutional Review Board of Tsaotun Psychiatric Center, Ministry of Health and Welfare (IRB No 105002). The National Health Research Institute de-identified the study participants before NHIRD release for public research. Therefore, the Institutional Review Board waived the requirement for patient written informed consent for this study.
Study patients
The patients with bronchiectasis (ICD-9-CM Code 494) newly confirmed by HRCT examination and with age ranging from 20 to 90 years visiting health care centers (outpatients or inpatients) within 2000–2008 constituted a bronchiectasis cohort. The date of bronchiectasis first diagnosed was used as the index year. The comparison cohort consisted of patients without bronchiectasis randomly selected from general population and 5:1 ratio frequency-matched with bronchiectasis cohort according to sex, age, and index year. Patients with ischemic stroke (ICD-9-CM Code 433-435) diagnosed before the index date were excluded in both cohorts.
Outcome measures
The outcome variable was ischemic stroke (ICD-9-CM Code 433-435) diagnosed and confirmed by CT or magnetic resonance image (MRI) examinations. CT or MRI is widely used to distinguish ischemic stroke from hemorrhagic stroke. The follow-up person-years (PYs) were calculated based on the interval between the index date and the date the ischemic stroke event first occurred or was censored: withdrawal from the NHI program, death, or the end of 2010 when the study terminated.
Covariates and comorbid diseases
The patients were divided into the three groups according to age: age <50 years as young adults, age 50–64 years as middle-aged adults, and age ≥65 years as elderly adults. The comorbid diseases reported to be risk factors of stroke, including hypertension (ICD-9-CM codes 401-405); diabetes (ICD-9-CM codes 250); hyperlipidemia (ICD-9-CM codes 272); CAD (ICD-9-CM codes 410-414) including myocardial infarction (ICD-9-CM codes 410 and 412), ischemic heart disease (ICD-9-CM codes 411 and 414), and angina pectoris (ICD-9-CM code 413); CHF (ICD-9-CM 428); COPD (ICD-9-CM 491, 492, 496); and AF (ICD-9-CM 427.31) were considered in this study.Citation15–Citation19
Statistical analyses
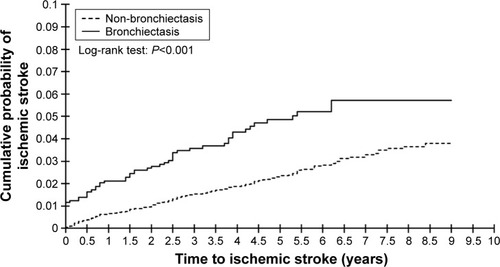
The Statistical Package for the Social Sciences (SPSS) Version 22.0 (IBM Corp., Armonk, NY, USA) was adopted for all statistical analyses. The χ2 test was used to compare and test difference in the proportional distribution of the demographic characteristics and comorbidities in both cohorts. The Student’s two sample t-test was used to measure and compare the mean ages of both cohorts. We evaluated the overall, age-specific, and comorbidity-specific incidence of ischemic stroke in both cohorts by follow-up PYs. Cox proportional hazard regression models were used to compare the hazard ratio (HR) and 95% CI of ischemic stroke development between patients with bronchiectasis and those without bronchiectasis. Nelson–Aalen analysis was adopted to evaluate the difference of cumulated probability of ischemic stroke between the two cohorts using XLSTAT add-on statistic software (Addinsoft Inc., Chicago, IL, USA). The significance level was set at P<0.05 at 2-tail.
Results
Demographic characteristics and comorbidities of patients with and without bronchiectasis
A total of 7,770 patients, including 1,295 patients with bronchiectasis (585 men and 710 women) and 6,475 patients without bronchiectasis (2,925 men and 3,550 women), have 6,312.70 and 34,958.00 follow-up PYs, respectively. The age and sex distribution of the patients in both cohorts were the same. The mean age of the patients in both cohorts was 62.0±15.3 years. The bronchiectasis cohort exhibited a significantly higher prevalence of CAD (16.8% vs 13.1%), CHF (8.0% vs 2.8%), COPD (48.8% vs 8.5%), and AF (1.9% vs 1.1%) than did the non-bronchiectasis cohort (). The patients with bronchiectasis had a significantly lower prevalence of being not comorbid with any medical disorders when compared with the patients without bronchiectasis (28.9% vs 48.7%, P<0.001).
Table 1 Demographic characteristics and comorbidity in patients with and without bronchiectasis
Comparison of incidence and risk of ischemic stroke stratified by sex, age, and comorbidity between bronchiectasis and non-bronchiectasis patients
As indicated in , the patients with bronchiectasis exhibited a higher incidence rate of ischemic stroke (9.18 vs 4.66 per 1,000 PYs) than those without bronchiectasis with a crude HR of 1.93 (95% CI =1.43–2.61) and an adjusted HR (aHR) of 1.74 (95% CI =1.28–2.35) after controlling for age, sex, and comorbidities. The incidence rates of ischemic stroke increased with age in both cohorts. After adjusting for covariates, the risk of stroke was higher in the middle-aged patients (aHR =4.79, 95% CI =1.88–12.17) and elderly patients (aHR =11.76, 95% CI =4.76–29.07) compared to the younger patients. The risk of ischemic stroke was significantly higher in the bronchiectasis cohort than those in non-bronchiectasis cohort in both sexes (crude HR =1.98, 95% CI =1.32–2.97 for men and crude HR =1.89, 95% CI =1.21–2.96 for women). After adjusting for covariates, the risk of stroke was not significantly different in both sexes despite men exhibiting higher incidence of ischemic stroke than women.
Table 2 Comparison of incidence and hazard ratio of ischemic stroke stratified by sex, age, and comorbidity between patients with and without bronchiectasis
Comparison of incidence and HR of ischemic stroke by individual comorbidity between bronchiectasis and non-bronchiectasis patients
The patients with bronchiectasis had a higher incidence of stroke than did the patients without bronchiectasis regardless of comorbidities. The incidence of stroke was higher in patients with one or more comorbidities, including hypertension, diabetes, hyperlipidemia, CAD, CHF, COPD, and AF, compared with the patients without the corresponding comorbidity. However, after adjustment for covariates, hypertension, diabetes, and AF remained independent risk factors of stroke development ().
Table 3 Comparison of incidence and HR of ischemic stroke between patients with and without bronchiectasis by considering individual comorbidities
Joint effect of bronchiectasis and comorbidity on the risk of ischemic stroke
lists the joint effect of bronchiectasis and individual comorbidity on the risk of ischemic stroke. Patients with bronchiectasis comorbid with diabetes, AF, or hypertension exhibited a multiplicative risk of ischemic stroke compared with patients with neither bronchiectasis nor comorbidity. The odds ratios of ischemic stroke associated with bronchiectasis and covariates, including sex, age, and comorbidity, are shown in . Patients with bronchiectasis, older age, or other comorbidity had significantly higher risk of ischemic stroke.
Table 4 Cox proportional hazard regression analysis for the risk of ischemic stroke associated with the joint effect of bronchiectasis and individual comorbidity
Table 5 Odds ratios of ischemic stroke associated with bronchiectasis and covariates
Association of risk of ischemic stroke and number of emergency department visits and hospitalizations in patients with bronchiectasis
presents the incidence and risk of ischemic stroke in patients without bronchiectasis and patients with bronchiectasis based on the number of emergency department visits and hospitalizations a year. The risk of ischemic stroke in patients with bronchiectasis increased with the annual number of emergency department visits and hospitalizations (aHR =4.31, 95% CI =2.53–7.35 for 1–3 times/year; aHR =6.24, 95% CI =2.30–16.89 for >3 times/year) compared with those without bronchiectasis.
Table 6 Comparison of ischemic stroke risk between bronchiectasis and comparison cohorts by annual number of emergency room visits and hospitalization due to acute respiratory infection
Cumulative probability of ischemic stroke between patients with and without bronchiectasis during follow-up periods
illustrated that the cumulative probability of ischemic stroke was significantly higher in the bronchiectasis cohort than in the comparison cohort (log-rank test, P<0.001).
Discussion, limitations, and conclusion
This longitudinal cohort study demonstrated that the incidence of ischemic infarction was higher in the bronchiectasis cohort than in the non-bronchiectasis cohort (9.18 vs 4.66 per 1,000 PYs). The patients with bronchiectasis exhibited a significantly (P<0.05) higher prevalence of CAD, CHF, COPD, and AF than did the patients without bronchiectasis, which is consistent to previous studies.Citation15–Citation19 After adjustment for sex, age, and comorbid disorders, the bronchiectasis cohort had a 1.74-fold increased risk of developing ischemic stroke compared with the non-bronchiectasis cohort. Similarly, Navaratnam et alCitation6 also reported that people with bronchiectasis exhibited a 1.92-fold higher risk of stroke compared with those without bronchiectasis. However, in contrast to our study, they used a cross-sectional design rather than the cohort study to evaluate the prevalence of stroke in patients with bronchiectasis.Citation6
The possible mechanisms for the increased risk of ischemic stroke need further elucidation. Bronchiectasis is characterized by chronic inflammation and inability to clear airway secretion, which results in recurrent infection. Previous studies have reported that patients with bronchiectasis are related to increased systemic inflammation.Citation26,Citation27 Inflammation also plays a pivotal role in the initiation and progression of atherosclerosisCitation28 and is associated with vulnerable atherosclerotic plaque and subsequent thromboembolic events.Citation29,Citation30 The vulnerable atheromatous plaque in carotid arteries is responsible for acute ischemic stroke.Citation31 In addition, observational studies have demonstrated that acute respiratory tract infections like influenza and Chlamydia pneumoniae infection are associated with the increased incidence and risk of stroke.Citation32–Citation36
The bronchiectasis cohort exhibited higher incidence of ischemic stroke than did the non-bronchiectasis cohort irrespective of sex, age subgroups, and comorbidity. Most patients with bronchiectasis were women (54.8%), a finding which is consistent with previous studies.Citation37,Citation38 The incidence of stroke increased with age. As presented in this study, 78.3% (173/221) of ischemic stroke occurred in elderly adults, which is consistent with previous reports.Citation39,Citation40 Compared to the young adults, middle-aged and elderly adults had 4.79- and 11.76-fold increased risks of stroke development, respectively. As evident in a previous study, the elderly have a high incidence of carotid artery stenosis, which is a major risk factor of ischemic stroke.Citation41 In addition, watershed stroke is more common in the elderly adults than in the young adults, which is associated with the fact that the elderly have a higher prevalence of AF, hypertension, cardiovascular dysfunction, and other medical disorders.Citation40,Citation42–Citation44
Hypertension, diabetes, and AF remained the independent risk factors of stroke development in the bronchiectasis and non-bronchiectasis cohorts. Bronchiectasis combined with diabetes, AF, or hypertension exhibited a multiplicative risk of ischemic stroke (). Furthermore, regarding COPD, the incidence rate of stroke was significantly higher in bronchiectasis patients without COPD than in non-bronchiectasis patients without COPD (7.31 vs 4.27 per 1,000 PYs) (). Although not significant, the incidence rate of stroke was also higher in bronchiectasis patients with COPD than in non-bronchiectasis patients with COPD (11.20 vs 8.53 per 1,000 PYs). The bronchiectasis cohort still carried a 1.74-fold increased risk of developing ischemic stroke compared with the non-bronchiectasis cohort after adjustment for covariates, despite 50% of the bronchiectasis cohort having COPD in our dataset.
Furthermore, symptom overlap between COPD and bronchiectasis may complicate discriminative diagnoses of these two diseases. As evident in this study, among the patients with bronchiectasis, up to 48.8% also had COPD (). A similar observation was reported in previous studies that bronchiectasis coexisted in 30%–57% of patients with COPD,Citation45–Citation48 which significantly increased the duration of ICU stay and hospital admissionCitation46 as well as the mortality rate.Citation4,Citation48 On the other hand, a Germany study showed that, with bronchiectasis as the primary diagnosis, 39% of the hospitalized patients were found to be comorbid with COPD and emphysema.Citation49 COPD and bronchiectasis share many features in common, presenting a similar inflammatory profile with symptoms of chronic cough and sputum production, and both sometimes overlap, complicating their discriminative diagnoses and treatments.Citation50 Bronchiectasis is generally diagnosed with the presence of airway dilation and airway wall thickness based on HRCT examination, whereas COPD is diagnosed based on the manifestation of poorly reversible airflow obstruction, symptoms of shortness of breath, and exposure to cigarette smoke and pollutants.Citation50 However, according to a UK study, some COPD patients also exhibited airway wall abnormality, while 81% of patients diagnosed with bronchiectasis were current smokers or had a history of smoking.Citation45 Moreover, a recent study confirmed airway wall abnormality, typically manifested in bronchiectasis, in patients with COPD exacerbation.Citation48 High prevalence rate and great severity of bronchiectasis presented in COPD patients suggested bronchiectasis as a pathological phenotype of COPD, which may have prognostic and therapeutic implications.Citation51
Patients with bronchiectasis who had respiratory infection-related ED visits and hospitalization exhibited a dose–response effect on the risk of ischemic stroke. The finding may explain the relationship of severity of bronchiectasis and frequent respiratory infections with an increased risk of developing stroke.
Several limitations should be addressed in the current study. First, the detailed smoking habits and physical activity levels are not available in the LHID. Hypertension and COPD are well-recognized comorbidities associated with cigarette smoking.Citation52,Citation53 Therefore, we controlled for hypertension and COPD to mediate the influence of smoking. Second, although diagnoses based on ICD-9-CM codes may cause misclassification, we used HRCT to help validate the diagnosis of bronchiectasis and ischemic stroke. Furthermore, the NHIA routinely audits the claims data through an administrative and peer-review process to minimize medical fraud.
The strength of our study is that it is a large population-based sample: this is the first study on Asian people to evaluate the incidence and risk of ischemic stroke in patients with bronchiectasis. All NHI beneficiaries are assigned personal identification numbers that facilitate follow-up of the study patients.
In conclusion, this cohort study of 1,295 patients (6,312.70 PYs) with bronchiectasis and 6,475 patients (34,958.00 PYs) without bronchiectasis demonstrated that bronchiectasis patients carried a 1.74-fold increased risk of ischemic stroke compared with those without bronchiectasis. Patients with bronchiectasis experiencing frequent respiratory infections are at a substantial risk of ischemic stroke. Clinicians should take proactive strategy to carefully assess risk factors of stroke and holistically treat patients with bronchiectasis.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
This study was supported in part by Ministry of Science and Technology of Taiwan (MOST104-2410-H-166-005 and MOST105-2410-H-166-006) Taichung Hospital, Ministry of Health and Welfare, as well as Central Taiwan University of Science and Technology. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- McShanePJNaureckasETTinoGStrekMENon-cystic fibrosis bronchiectasisAm J Respir Crit Care Med2013188664765623898922
- ChalmersJDGoeminnePAlibertiSThe bronchiectasis severity index. An international derivation and validation studyAm J Respir Crit Care Med2014189557658524328736
- DoddJDLavelleLPFabreABradyDImaging in cystic fibrosis and non-cystic fibrosis bronchiectasisSemin Respir Crit Care Med201536219420625826587
- GoeminnePCNawrotTSRuttensDSeysSDupontLJMortality in non-cystic fibrosis bronchiectasis: a prospective cohort analysisRespir Med2014108228729624445062
- LaveryKO’NeillBElbornJSReillyJBradleyJMSelf-management in bronchiectasis: the patients’ perspectiveEur Respir J200729354154717079260
- NavaratnamVMillettERHurstJRBronchiectasis and the risk of cardiovascular disease: a population-based studyThorax201772216116627573451
- LibbyPInflammation in atherosclerosisNature2002420691786887412490960
- Del RinconIO’LearyDHFreemanGLEscalanteAAcceleration of atherosclerosis during the course of rheumatoid arthritisAtherosclerosis2007195235436017097659
- Del RinconIWilliamsKSternMPFreemanGLO’LearyDHEscalanteAAssociation between carotid atherosclerosis and markers of inflammation in rheumatoid arthritis patients and healthy subjectsArthritis Rheum20034871833184012847676
- KobayashiHGilesJTPolakJFIncreased prevalence of carotid artery atherosclerosis in rheumatoid arthritis is artery-specificJ Rheumatol201037473073920110515
- Di CarloAHuman and economic burden of strokeAge Ageing20093814519141505
- MukherjeeDPatilCGEpidemiology and the global burden of strokeWorld Neurosurg201176Suppl 6S85S9022182277
- WHOThe Top 10 Causes of DeathGenevaWorld Health Organization2014
- HsiaoAJChenLHLuTHTen leading causes of death in Taiwan: a comparison of two grouping listsJ Formos Med Assoc2015114867968024457066
- WolfPAD’AgostinoRBBelangerAJKannelWBProbability of stroke: a risk profile from the Framingham StudyStroke19912233123182003301
- AirELKisselaBMDiabetes, the metabolic syndrome, and ischemic stroke: epidemiology and possible mechanismsDiabetes Care200730123131314017848611
- ShindoATomimotoHDiabetes and ischemic strokeBrain Nerve201466210711924523309
- LewisASegalAHyperlipidemia and primary prevention of stroke: does risk factor identification and reduction really work?Curr Atheroscler Rep201012422522920495893
- MitchellABColeJWMcArdlePFObesity increases risk of ischemic stroke in young adultsStroke20154661690169225944320
- DonaldsonGCHurstJRSmithCJHubbardRBWedzichaJAIncreased risk of myocardial infarction and stroke following exacerbation of COPDChest201013751091109720022970
- PortegiesMLLahousseLJoosGFChronic obstructive pulmonary disease and the risk of stroke. The Rotterdam StudyAm J Respir Crit Care Med2016193325125826414484
- NHIANational Health Insurance2015Accessed June 13, 2016
- HsiehCYChenCHLiCYLaiMLValidating the diagnosis of acute ischemic stroke in a National Health Insurance claims databaseJ Formos Med Assoc2015114325425924140108
- ChengCLKaoYHLinSJLeeCHLaiMLValidation of the National Health Insurance Research Database with ischemic stroke cases in TaiwanPharmacoepidemiol Drug Saf201120323624221351304
- ChungWSLinCLKaoCHBronchiectasis and the risk of cancer: a nationwide retrospective cohort studyInt J Clin Pract201569668268825421905
- WilsonCBJonesPWO’LearyCJSystemic markers of inflammation in stable bronchiectasisEur Respir J19981248208249817152
- Martinez-GarciaMAPerpina-TorderaMRoman-SanchezPThe association between bronchiectasis, systemic inflammation, and tumor necrosis factor alphaArchivos de bronconeumologia200844181418221721
- LibbyPRidkerPMMaseriAInflammation and atherosclerosisCirculation200210591135114311877368
- TangTYHowarthSPMillerSRComparison of the inflammatory burden of truly asymptomatic carotid atheroma with atherosclerotic plaques contralateral to symptomatic carotid stenosis: an ultra small superparamagnetic iron oxide enhanced magnetic resonance studyJ Neurol Neurosurg Psychiatry200778121337134317578854
- NighoghossianNDerexLDouekPThe vulnerable carotid artery plaque: current imaging methods and new perspectivesStroke200536122764277216282537
- NaghaviMLibbyPFalkEFrom vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: Part IICirculation2003108151772177814557340
- Paganini-HillALozanoEFischbergGInfection and risk of ischemic stroke: differences among stroke subtypesStroke200334245245712574559
- HeuschmannPUNeureiterDGessleinMAssociation between infection with Helicobacter pylori and Chlamydia pneumoniae and risk of ischemic stroke subtypes: results from a population-based case-control studyStroke200132102253225811588309
- ElkindMSLinIFGraystonJTSaccoRLChlamydia pneumoniae and the risk of first ischemic stroke: The Northern Manhattan Stroke StudyStroke20003171521152510884447
- AsgharZCouplandCSiriwardenaNInfluenza vaccination and risk of stroke: self-controlled case-series studyVaccine201533415458546326296496
- SiriwardenaANAsgharZCouplandCCInfluenza and pneumococcal vaccination and risk of stroke or transient ischaemic attack-matched case control studyVaccine201432121354136124486370
- PasteurMCBiltonDHillATBritish Thoracic Society guideline for non-CF bronchiectasisThorax201065Suppl 1i1i5820627931
- TrowTKClinical year in review II: occupational lung disease, pulmonary vascular disease, bronchiectasis, and chronic obstructive pulmonary diseaseProc Am Thorac Soc20063755756016963533
- FeiginVLLawesCMBennettDAAndersonCSStroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th centuryLancet Neurol200321435312849300
- ChenRLBalamiJSEsiriMMChenLKBuchanAMIschemic stroke in the elderly: an overview of evidenceNat Rev Neurol20106525626520368741
- de WeerdMGrevingJPde JongAWBuskensEBotsMLPrevalence of asymptomatic carotid artery stenosis according to age and sex: systematic review and metaregression analysisStroke20094041105111319246704
- KannelWBBenjaminEJStatus of the epidemiology of atrial fibrillationMed Clin North Am20089211740ix18060995
- HammamiSMehriSHajemSKoubaaNSouidHHammamiMPrevalence of diabetes mellitus among non institutionalized elderly in Monastir CityBMC Endocr Disord2012121522898260
- RuffCTCardiology patient page: stroke prevention in atrial fibrillationCirculation201212516e588e59022529067
- O’BrienCGuestPJHillSLStockleyRAPhysiological and radiological characterisation of patients diagnosed with chronic obstructive pulmonary disease in primary careThorax200055863564210899238
- GurselGDoes coexistence with bronchiectasis influence intensive care unit outcome in patients with chronic obstructive pulmonary disease?Heart Lung2006351586516426936
- PatelISVlahosIWilkinsonTMBronchiectasis, exacerbation indices, and inflammation in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2004170440040715130905
- Martinez-GarciaMAde la Rosa CarrilloDSoler-CatalunaJJPrognostic value of bronchiectasis in patients with moderate-to-severe chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2013187882383123392438
- RingshausenFCde RouxAPletzMWHamalainenNWelteTRademacherJBronchiectasis-associated hospitalizations in Germany, 2005–2011: a population-based study of disease burden and trendsPloS one201388e7110923936489
- HurstJRElbornJSDe SoyzaACOPD-bronchiectasis overlap syndromeEur Respir J201545231031325653262
- StockleyRABronchiectasis with chronic obstructive pulmonary disease: association or a further phenotype?Am J Respir Crit Care Med2013187878678823586376
- VirdisAGiannarelliCNevesMFTaddeiSGhiadoniLCigarette smoking and hypertensionCurr Pharm Des201016232518252520550499
- EisnerMDAnthonisenNCoultasDAn official American Thoracic Society public policy statement: novel risk factors and the global burden of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2010182569371820802169