Abstract
Background and objective
In chronic obstructive pulmonary disease (COPD), accessory respiratory muscles are recruited as a compensatory adaptation to changes in respiratory mechanics. This results in shortening and overactivation of these and other muscles. Manual therapy is increasingly being investigated as a way to alleviate these changes. The aim of this study was to measure the immediate effect on lung function of a soft tissue manual therapy protocol (STMTP) designed to address changes in the accessory respiratory muscles and their associated structures in patients with severe COPD.
Methods
Twelve medically stable patients (n=12) with an existing diagnosis of severe COPD (ten: GOLD Stage III and two: GOLD Stage IV) were included. Residual volume, inspiratory capacity and oxygen saturation (SpO2) were recorded immediately before and after administration of the STMTP. A Student’s t-test was used to determine the effect of the manual therapy intervention (P<0.05).
Results
The mean age of the patients was 62.4 years (range 46–77). Nine were male. Residual volume decreased from 4.5 to 3.9 L (P=0.002), inspiratory capacity increased from 2.0 to 2.1 L (P=0.039) and SpO2 increased from 93% to 96% (P=0.001).
Conclusion
A single application of an STMTP appears to have the potential to produce immediate clinically meaningful improvements in lung function in patients with severe and very severe COPD.
Introduction
Chronic obstructive pulmonary disease (COPD) is a common preventable and treatable disease characterized by progressive airflow limitation that is associated with an inflammatory response to noxious particles or gases.Citation1 The disease has been categorized in to four stages according to severity: mild, moderate, severe and very severe.Citation2 Exacerbations and comorbidities contribute to the overall severity in individual patients with the disease affecting not only the respiratory system but also the musculoskeletal system.Citation2,Citation3
In COPD, changes in the anatomy of the airways and lung parenchyma occur as the result of bronchial hypersecretion and bronchoalveolar instability. These changes cause expiratory flow limitation and air trapping, known clinically as dynamic hyperinflation. This phenomenon leads to increases in expiratory reserve volume, residual volume (RV) and end expiratory lung volume (EEV). The increase in EEV limits tidal and inspiratory reserve volumes resulting in a negative impact on inspiratory capacity (IC).Citation4 The changes alter the position of the ribs causing a state similar to sustained inspiration over time, often referred to as “inspiratory block”. This phenomenon is responsible for the characteristic “barrel chest” commonly seen in patients with COPD. In this state, the position of the diaphragm is flattened and shortened reducing its ability to generate force.Citation5 Accessory respiratory muscles are recruited as a compensatory adaptation leading to shortening and overactivation of these muscles over time (overadaptation).Citation5 The surrounding cervicothoracic fascia contracts producing postural changes, such as anterior projection of the head, neck hyperextension, increased thoracic kyphosis and internal rotation of shoulders. These changes contribute to an increase in chest tightness, a decrease in the ability to generate inspiratory pressures and volumes and an increase in the amount of effort required to breathe.Citation5–Citation7
Current COPD management strategies include physical activity and respiratory muscle training.Citation2 Physical activity improves exercise tolerance, whereas respiratory muscle training increases inspiratory muscle strength. Targeting disturbances in the respiratory pumping mechanism is not part of this approach making the addition of a therapeutic intervention that directly addresses the soft tissues of the chest wall a novel approach.
Manual therapy (MT) has been described as a therapeutic intervention that uses the hands to provide treatment to the musculoskeletal and/or visceral systems.Citation8 MT includes techniques such as massage, myofascial release, muscle energy technique, ligament balance, joint mobilization and joint manipulation. The suggestion that MT can deliver ongoing benefits for people with COPD has been proposed in the literature.Citation9 Since then, a number of small studies have reported improvements in lung function and/or exercise capacity following various forms of MT intervention over the immediate, short- and medium terms.Citation10–Citation15
Two of these studies measured the immediate effect of MT on lung function: one measured the effect of a single session of soft tissue therapy in combination with thoracic mobilization,Citation10 whereas the other measured the effect of six sessions of a single soft tissue technique – the manual diaphragm release technique.Citation13 Neither study was capable of clearly delineating the effect of a single session of soft tissue MT on lung function.
The aim of this study was to measure the immediate effect on lung function of a single session of soft tissue MT.
Patients and methods
Clinical records from patients who attended the outpatient clinic of San José Hospital in Santiago, Chile, were screened for suitability for inclusion in the study. To be included, a patient had to have a diagnosis of severe or very severe COPD (GOLD: Stage III or IV)Citation1 and be medically stable with no exacerbations in the preceding 2 months. Patients were excluded from the study if they had any of the following: a rheumatoid condition, neuromuscular or musculoskeletal pathology, cognitive disability that could affect their understanding or execution of the assessment tests or intervention protocol, supplemental oxygen dependency, or previous or current enrollment in a pulmonary rehabilitation program.
Patients who met these conditions were invited to attend an educational session explaining the purpose of the study, proposed outcome assessments and the soft tissue manual therapy protocol (STMTP) used in the trial. After providing written consent, a patient was enrolled in the study.
Baseline measurements, including age, weight, height and lung volumes, were recorded. Lung volumes were measured using body plethysmography (Sensormedics VMAX 22 Pulmonary Function Test System; SensorMedics Corporation, Yorba Linda, CA, USA) and collected according to the standards and procedures outlined by the American Thoracic Society.Citation3 Lung volumes included total lung capacity (TLC), vital capacity (VC), RV, expiratory reserve volume (ERV), IC and airway resistance (Raw).
Heart rate (HR) was assessed manually through palpation of the radial pulse for 1 minute with the patient at rest. Respiratory rate (RR) was measured using the direct observation method and calculated by counting the number of respiratory cycles in 1 minute while the patient was at rest. Oxygen saturation (SpO2) was measured using a portable finger oximeter (Prince 100I; Heal Force Bio-meditech Holdings Limited, Hong Kong, People’s Republic of China) with the patient at rest. All measurements were taken immediately before and after administration of the STMTP.
MT protocol
The STMTP used in this trial consisted of a pre-determined set of seven soft tissue techniques delivered as part of a single treatment session lasting ~30 minutes (). The techniques and their respective durations were sub-occipital release, 5 minutes; anterior thoracic myofascial and sternum release, 5 minutes; anterior cervical myofascial release, 5 minutes; costal ligament balance, 5 minutes; and muscular energy technique to the following muscles: scalenes, 1 minute and 40 seconds, pectoralis minor, 1 minute and 40 seconds and latisimus dorsi and serratus anterior, 1 minute and 40 seconds. All techniques were administered in the same order and by a single therapist with the patient positioned in Fowler’s position (45°) throughout the session.
Table 1 Soft tissue manual therapy protocol
Statistical analysis was performed using the SPSS 15.0 software (SPSS for Windows Version 15.0; SPSS Inc, Chicago, IL, USA). Normal distributions for HR, RR, SpO2 and lung volumes were assessed using the Shapiro–Wilk test (P>0.05). A Student’s t-test for comparison before and after intervention was used to determine the effect of the STMTP. A P-value of <0.05 was set as the threshold for statistical significance.
The Metropolitan North Health Service of Santiago, Chile, approved the study and all participants provided written informed consent to participate in the study. The trial was registered with the US National Institutes of Health (Trial registration number: NCT2534831). The research was conducted in accordance with the Declaration of Helsinki.
Results
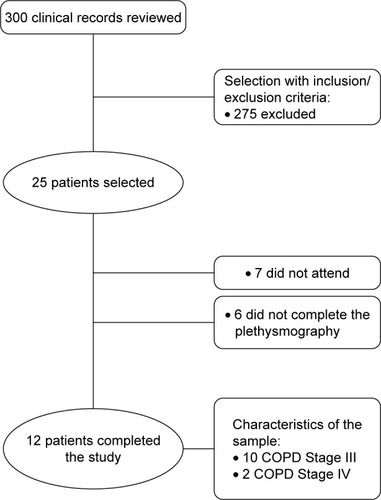
A total of 300 clinical records were reviewed as part of this trial. Twenty-five met the inclusion/exclusion criteria, and these patients were invited to participate in the study. Thirteen participants did not complete the study either through non-attendance or through incomplete assessments. Patient flow through the study is outlined in . Ten patients had severe (GOLD Stage III) and two had very severe (GOLD Stage IV) COPD. Nine were males. The mean age was 62.4±7.8 years, mean weight was 71.8±9.3 kg and mean height was 164±6.1 cm (). shows the pre- and postintervention measurements for HR, RR and SpO2 for all 12 patients who completed the study. Average HR decreased from 83.8±14.1 beats per minute (bpm) preintervention to 76.5±15.3 bpm postintervention (P=0.001); RR decreased from 20.4±4.3 respirations per minute (rpm) preintervention to 15.7±3.8 rpm postintervention (P=0.001) and SpO2 increased from 92.8%±2.8% preintervention to 95.8%±2.4% postintervention (P=0.001). TLC decreased by 0.4 L (pre: 6.8±2.0; post: 6.4±1.8; P=0.031), ERV by 0.05 L (0.33±0.17; 0.28±0.16; P=0.005) and RV by 0.6 L (4.5±1.5; 3.9±1.4; P=0.002), whereas IC increased by 0.1 L (2.0±0.5; 2.1±0.6; P=0.039; ). There were no changes in VC and Raw (P=0.799 and P=0.068, respectively).
Table 2 Demographic and clinical characteristics of participants
Table 3 Pre- and postintervention outcome measurementsTable Footnotea
Discussion
Results from this study show that a single application of a soft tissue MT protocol designed to address the soft tissues of the chest wall has the potential to produce immediate improvements in lung function in patients with severe and very severe COPD. Furthermore, the reduction in RV may prove to be clinically relevant as it was above the threshold for minimal important difference.Citation16
The results from this study are in line with results from a similar study that reported immediate improvements in lung function after a single session of MT.Citation10 However, that trial used an MT protocol that included a combination of soft tissue therapy and thoracic mobilization. In using only soft tissue MT, the most likely cause of the improvements reported in our study is a reduction in chest tightness produced by soft tissue MT intervention. This is in line with results from other studies that showed that soft tissue MT was capable of reducing hypertonicity in myofascial tissues when applied to other areas of the body.Citation17–Citation22 Reduced tonicity in the muscles, fascia and ligaments of the neck and chest would facilitate an improvement in the passive components of expiration by reducing the extent of any inspiratory block. In support of this concept are the results from a recent exploratory study, which reported a correlation between pulmonary function, postural alignment and mobility of the upper quadrant in patients with COPD.Citation23
The decreases in ERV and RV can be directly attributed to the increase in IC as it would return the inspiratory muscles closer to their optimal length, thereby improving mechanical efficiency.Citation4,Citation5 Improvements in mechanical efficiency may also explain the increase in SpO2 and decrease in RR, which if sustainable, could alter input to the central and peripheral chemoreceptors.Citation24,Citation25 The decrease in HR may be the result of a flow-on effect from a decreasing RV where lower pressure within the lungs leads to a reduction in pulmonary hypertension.Citation24,Citation26,Citation27 The absence of any changes in VC and Raw may simply be the result of the small size of the changes in RV, ERV, TLC and IC.
It is worth noting that the TLC values reported in this study were higher than those traditionally reported in patients with severe and very severe COPD. This may be due to two reasons: (1) patients with COPD and lung hyperinflation can have a TLC that is >100% of the predicted value,Citation4 and (2) spirometric values for the Chilean population have been reported as being higher than in other populations.Citation28
Although the findings from a recent systematic review into the effect of MT on COPD were inconclusive with respect to benefiting lung function,Citation29 technique choice may have played a role in influencing this view as MT techniques that use compression/decompression maneuvers can increase airway obstruction by accelerating airflow to the extent that airways collapse.Citation4 Patient positioning during the STMTP may have influenced our results as having the patient supine for an extended period of time can increase the effect of inefficient diaphragm motion. The way lung function was measured may also have influenced the results. Although the previous study used spirometry to assess lung function and focused on measures, such as forced expiratory volume in the first second and forced vital capacity,Citation10 we used plethysmography and were, therefore, able to measure changes in RV accurately, which directly relate to the extent of dynamic hyperinflation.Citation30–Citation32
The MT techniques used in this study were chosen because of their potential to reduce the effects of overactivation and overadaptation in the respiratory muscles. The results reported here are supported by results in other studies, involving the administration of MT to patients with COPD. These studies used a similar approach in producing short-termCitation11–Citation13,Citation15 and medium-termCitation14 improvements in lung function. Notwithstanding, to our knowledge, this is the first study to use plethysmography to report a clinically meaningful reduction in RV following MT intervention.
The STMTP could be used in a repeated manner as part of a pulmonary rehabilitation program for patients with COPD. As it has the potential to reduce overactivation in the respiratory muscles, it may also be beneficial following an exacerbation.
Limitations
Apart from the recognized limitations associated with a study design of this nature, there are a number of other limitations associated with this study. Gender mix differences may have altered the statistical analyses as males and females have different lung volumes. The contribution toward the decreases in HR and RR of leaving the patient in Fowler’s position for an extended period of time (30 minutes) is unclear. By not gathering data on adverse events, the safety of this STMTP remains unknown. As a study aimed at evaluating the immediate effect of a specific intervention, the impact of these limitations should be considered within this context and not measured against other study designs.
Conclusions
A single application of an MT protocol consisting of seven soft tissue techniques has the potential to deliver immediate improvements in lung function for people with severe and very severe COPD. The results from this study support the call for further research in the field on larger cohorts that include multiple measuring points and a control group. Such studies would help to confirm if the benefits reported here can be sustained in patients with advanced COPD.
Authors’ contribution
CCM helped in concept, design, data collection, analysis and interpretation, drafting and revising the manuscript; DGO contributed to design, data collection, analysis and interpretation, drafting and revising the manuscript; FACB performed data analysis and interpretation, drafting and revising the manuscript; PG carried out design, data collection, analysis and interpretation, drafting and revising the manuscript; RTC helped in data analysis and interpretation, drafting and revising the manuscript; LMV carried out design, data collection, analysis and interpretation, drafting and revising the manuscript; RME contributed to data interpretation, drafting and revising the manuscript. All authors gave final approval of this version to be published and agreed to be accountable for all aspects of the work and for ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure
The authors report no conflicts of interest in this work.
References
- VestboJHurdSSAgustíAGGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med2013187434736522878278
- SpruitMAWatkinsMLEdwardsLDEvaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) study investigatorsDeterminants of poor 6-min walking distance in patients with COPD: the ECLIPSE cohortRespir Med2010104684985720471236
- MillerMRHankinsonJBrusascoVATS/ERS Task ForceStandardisation of spirometryEur Respir J200526231933816055882
- O’DonnellDLavenezianaPPhysiology and consequences of lung hyperinflation in COPDEur Respir Rev2006151006167
- Orozco-LeviMStructure and function of the respiratory muscles in patients with COPD: impairment or adaptation?Eur Respir J Suppl20034641s51s14621106
- ChaitowLDeLanyJClinical Application of Neuromuscular Techniques: The Upper Body2nd edEdinburgh, UKElsevier Health Sciences2008
- DiasCKirkwoodRParreiraVSampaioROrientation and position of the scapula, head and kyphosis thoracic in male patients with COPDCan J Resp Ther20094523034
- PettmanEA history of manipulative therapyJ Man Manip Ther201321165174
- EngelRMVemulpadSProgression to chronic obstructive pulmonary disease (COPD): could it be prevented by manual therapy and exercise during the ‘at risk’ stage (stage 0)?Med Hypotheses200972328829019038503
- YelvarGDYÇirakYDemirYPDalkilinçMBozkurtBImmediate effect of manual therapy on respiratory functions and inspiratory muscle strength in patients with COPDInt J Chron Obstruct Pulmon Dis2016111353135727382271
- DoughertyPEEngelRMVemulpadSBurkeJSpinal manipulative therapy for elderly patients with chronic obstructive pulmonary disease: a case seriesJ Manipulative Physiol Ther201134641341721807266
- EngelRMVemulpadSRBeathKShort-term effects of a course of manual therapy and exercise in people with moderate chronic obstructive pulmonary disease: a preliminary clinical trialJ Manipulative Physiol Ther201336849049624053900
- RochaTSouzaHBrandãoDCThe manual diaphragm release technique improves diaphragmatic mobility, inspiratory capacity and exercise capacity in people with chronic obstructive pulmonary disease: a randomised trialJ Physiother201561418218926386894
- EngelRMGonskiPBeathKVemulpadSMedium term effects of including manual therapy in a pulmonary rehabilitation program for chronic obstructive pulmonary disease (COPD): a randomized controlled pilot trialJ Man Manip Ther2016242808927559277
- ZanottiEBerardinelliPBizzarriCOsteopathic manipulative treatment effectiveness in severe chronic obstructive pulmonary disease: a pilot studyComplement Ther Med2012201162222305244
- HartmanJETen HackenNHKloosterKBoezenHMde GreefMHSlebosDJThe minimal important difference for residual volume in patients with severe emphysemaEur Respir J20124051137114122441742
- ChoSHKimSHParkDJThe comparison of the immediate effects of application of the suboccipital muscle inhibition and self-myofascial release techniques in the suboccipital region on short hamstringJ Phys Ther Sci201527119519725642072
- AparicioÉQQuiranteLBBlancoCRSendínFAImmediate effects of the suboccipital muscle inhibition technique in subjects with short hamstring syndromeJ Manipulative Physiol Ther200932426226919447262
- KrauseFWilkeJVogtLBanzerWIntermuscular force transmission along myofascial chains: a systematic reviewJ Anat2016228691091827001027
- WilkeJKrauseFVogtLBanzerWWhat is evidence-based about myofascial chains: a systematic reviewArch Phys Med Rehabil201697345446126281953
- Cruz-MontecinosCCerdaMSanzana-CucheRMartín-MartínJCuesta-VargasAUltrasound assessment of fascial connectivity in the lower limb during maximal cervical flexion: technical aspects and practical application of automatic trackingBMC Sports Sci Med Rehabil201681827403319
- Cruz-MontecinosCGonzalez BlancheALopez SanchezDIn vivo relationship between pelvis motion and deep fascia displacement of the medial gastrocnemius: anatomical and functional implicationsJ Anat2015227566567226467242
- MoraisNCruzJMarquesAPosture and mobility of the upper body quadrant and pulmonary function in COPD: an exploratory studyBraz J Phys Ther201620434535427556391
- ChaouatANaeijeRWeitzenblumEPulmonary hypertension in COPDEur Respir J20083251371138518978137
- WestJBRespiratory Physiology: The Essentials9th edBaltimore, MDLippincott Williams & Wilkins2012
- NaeijeRPulmonary hypertension and right heart failure in chronic obstructive pulmonary diseaseProc Am Thorac Soc200521202216113464
- WrightJLevyRChurgAPulmonary hypertension in chronic obstructive pulmonary disease: current theories of pathogenesis and their implications for treatmentThorax200560760560915994270
- GutiérrezMValdiviaGVillarroelLProposición de nuevas ecuaciones para calcular valores espirométricos de referencia en población chilena adulta: Sociedad Chilena de Enfermedades Respiratorias (SER) [Proposition of new equations for calculating reference spirometric values in the Chilean adult population: Chilean Society of Respiratory Diseases (SRD)]Rev Med Chile20141422143152 Spanish24953101
- HeneghanNRAdabPBalanosGMJordanREManual therapy for chronic obstructive airways disease: a systematic review of current evidenceMan Ther201217650751822703901
- HankinsonJStocksJPeslinRReproducibility of lung volume measurementsEur Respir J19981137877909596139
- HughesJMPrideNBLung Function Tests: Physiological Principles and Clinical ApplicationsLondon, UKBailliere Tindall1999
- PiattiGFasanoVCantarellaGTarantolaCBody plethysmographic study of specific airway resistance in a sample of healthy adultsRespirology201217697698322642668