Abstract
Background and objectives
Patients with chronic obstructive pulmonary disease (COPD) often experience exacerbations of their disease, sometimes requiring hospital admission and being associated with increased mortality. Although previous studies have reported mortality from exacerbations of COPD, there is limited information about prediction of individual in-hospital mortality. We therefore aimed to use data from a nationwide inpatient database in Japan to generate a nomogram for predicting in-hospital mortality from patients’ characteristics on admission.
Methods
We retrospectively collected data on patients with COPD who had been admitted for exacerbations and been discharged between July 1, 2010 and March 31, 2013. We performed multivariable logistic regression analysis to examine factors associated with in-hospital mortality and thereafter used these factors to develop a nomogram for predicting in-hospital prognosis.
Results
The study comprised 3,064 eligible patients. In-hospital death occurred in 209 patients (6.8%). Higher mortality was associated with older age, being male, lower body mass index, disturbance of consciousness, severe dyspnea, history of mechanical ventilation, pneumonia, and having no asthma on admission. We developed a nomogram based on these variables to predict in-hospital mortality. The concordance index of the nomogram was 0.775. Internal validation was performed by a bootstrap method with 50 resamples, and calibration plots were found to be well fitted to predict in-hospital mortality.
Conclusion
We developed a nomogram for predicting in-hospital mortality of exacerbations of COPD. This nomogram could help clinicians to predict risk of in-hospital mortality in individual patients with COPD exacerbation.
Introduction
Chronic obstructive pulmonary disease (COPD) is a common disease worldwide, with the prevalence of stage II or higher stages of COPD reported to be 10.1% in a general population in a previous study.Citation1 COPD was the third most common cause of death (3.1 million deaths) worldwide in 2012.Citation2,Citation3
Exacerbations of COPD are defined as any sustained worsening of respiratory symptoms, including cough, sputum, and breathing difficulty, compared with the baseline situation and beyond normal day-to-day variations and requiring modification of regular medication and hospital treatment.Citation4 COPD exacerbations are crucial events for patients. Approximately 30% of patients with COPD exacerbation require at least one hospital admission.Citation5 COPD exacerbations are associated with worsening of quality of life and increased mortality, reportedly accounting for 23.3% of deaths of COPD patients.Citation5,Citation6 The in-hospital mortality of COPD exacerbations is around 7% worldwide.Citation7–Citation13 Several factors are reportedly associated with increased in-hospital mortality in patients with COPD exacerbations.Citation8–Citation13
Prediction of mortality would help clinicians to provide appropriate clinical information and care to patients and their families; however, there are limited tools for predicting the in-hospital mortality of patients with COPD exacerbations on admission. Nomograms are graphical representations of the relationship between variables and outcome events.Citation14 Many nomograms for predicting clinical outcomes or survival rates have recently been developed.Citation15,Citation16 They can be used to calculate probabilities that can help clinicians to provide appropriate clinical information to patients.
We aimed to obtain information from a nationwide inpatient database in Japan on patient’s characteristics on admission for COPD exacerbations and use those data to examine factors associated with in-hospital mortality in patients with such exacerbations. Using these factors, we then aimed to create and validate a prognostic nomogram for predicting individual in-hospital mortality.
Methods
Data source
We obtained our data from the Diagnosis Procedure Combination (DPC) database, which is a nationwide inpatient database that contains administrative claims data and discharge abstract data from around 1,400 hospitals across Japan. In this database, main diagnoses, primary diagnosis on admission, and comorbidities on admission are recorded using the International Classification of Disease and Related Health Problems, 10th Revision (ICD-10) codes accompanied by text data in Japanese. This database also contains the following patient details: age, sex, body height and weight, levels of consciousness based on the Japan Coma Scale,Citation17 levels of dyspnea based on the Hugh–Jones classification at admission,Citation18 and discharge status including in-hospital death. The Japan Coma Scale is as follows: 0, alert; I, dull; II, somnolent; and III, comatose.Citation17 The Hugh–Jones classification, which is similar to the Medical Research Council (MRC) dyspnea scale and widely used in Japan, is used for patient evaluation on admission and is as follows: I, patient’s breathing is as good as that of other people of their own age and build during work, walking, and climbing hills or stairs; II, patient is able to walk at the pace of normal people of their own age and build on level ground, but is unable to keep up on hills or stairs; III, patient is unable to keep up with normal people on level ground but is able to walk about a mile or more at their own speed; IV, patient is unable to walk more than about 50 yards on level ground without a rest; V, patient is breathless on talking or undressing, or is unable to leave their house because of breathlessness; and Unspecified, patient is unable to be classified into the above grades because of bedridden status.Citation18
This study was approved by the institutional review board of the University of Tokyo, which waived the requirement for patient informed consent because of the anonymous nature of the data.
Patient selection and data
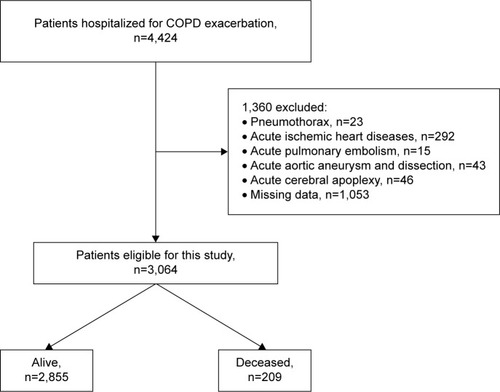
We retrospectively collected data on patients who had been admitted for COPD exacerbations and been discharged between 1 July 2010 and 31 March 2013. We included patients aged 40 years or older who were diagnosed as having COPD exacerbations (ICD-10 code, J441) on admission. We excluded patients who had the following diagnoses on admission: pneumothorax (J93); acute ischemic heart disease (I20–24); acute pulmonary embolism (I26); acute aortic aneurysm and dissection (I71); and acute cerebral apoplexy (I60–63). We also excluded patients for whom data on consciousness level, dyspnea level, or body weight and height were missing. Patient inclusion/exclusion details are presented in .
For this study, we used the following information: age, sex, body mass index (BMI), consciousness level, dyspnea level, and history of intubation. The following comorbidities were also used: bacterial pneumonia (J13–15, J170), atypical pneumonia (A481, J157, J160), aspiration pneumonia (J69), pneumocystis pneumonia (B59), eosinophilic pneumonia (J82), asthma (J45), interstitial pneumonia (J841, J848–9), heart failure (I50), chronic cerebrovascular disease (I69), chronic liver disease (K70–77), and chronic renal failure (N18–19).
Outcome
The outcome of this study was all-cause in-hospital mortality.
Statistical analysis
The χ2 test was used to compare proportions between groups. Multivariable logistic regression analysis was performed to examine the factors associated with all-cause in-hospital mortality. A generalized estimating equation was fitted with the regression model to adjust for within-hospital clustering. Based on these results, we built a nomogram to predict in-hospital death.Citation19 Internal validation was performed by a bootstrap method with 50 resamples, and calibration plots were derived to evaluate the relationship between probabilities predicted by the nomogram and observed rates. The threshold for significance was a P-value <0.05. Statistical analyses were performed using SPSS version 22.0 (IBM SPSS, Armonk, NY, USA), and the nomogram was built using R version 3.1.3 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient characteristics
A total of 4,424 patients were hospitalized for COPD exacerbations during the study period; 3,064 of them were included in this analysis. There were 209 in-hospital deaths (6.8%). The mean age was 76.0 (standard deviation [SD]: 8.9) years, and the proportion of males was 81.9%. The mean BMI was 19.9 (SD: 3.9) kg/m2. Five hundred and thirty-eight patients (17.6%) had a history of admission for COPD exacerbations, and 120 had a history of receiving mechanical ventilation.
All-cause in-hospital mortality in patients with COPD exacerbations
shows that in-hospital mortality was significantly associated with the following patient’s characteristics on admission: older age, being male, lower BMI, disturbance of consciousness, severe dyspnea, and having a history of mechanical ventilation. In-hospital mortality was also significantly associated with pneumonia, asthma, and heart failure.
Table 1 Characteristics of patients with COPD exacerbations and in-hospital mortality
Multivariable logistic regression analysis for all-cause in-hospital mortality
shows the results of the multivariable logistic regression analysis for all-cause in-hospital mortality. Higher mortality was significantly associated with older age, being male, lower BMI, disturbance of consciousness, severe dyspnea, having a history of mechanical ventilation, and pneumonia at admission. Lower mortality was significantly associated with asthma.
Table 2 Multivariable logistic regression analysis for all-cause in-hospital mortality
Nomogram for predicting in-hospital mortality
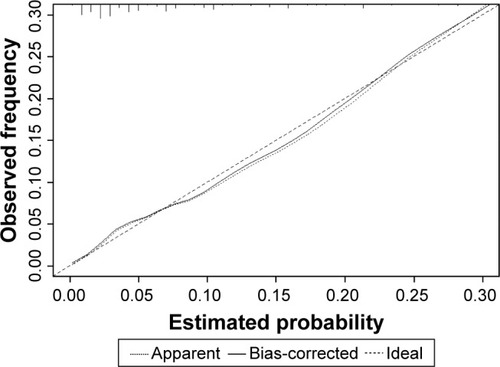
We built a nomogram according to the results of multivariable logistic analysis (). For this purpose, we recategorized Hugh–Jones grades as I–IV and V (grade V in the Hugh–Jones classification is equivalent to grade IV in the MRC dyspnea scale), and levels of consciousness into three groups: alert, dull or somnolent, and comatose. The concordance index of the nomogram was 0.775. Calibration plots are shown in .
Figure 2 Our nomogram for predicting in-hospital mortality in patients with COPD exacerbation.
Notes: The patient’s status for each predictor is plotted on the horizontal scale, and vertical lines are drawn to the resulting line to obtain the corresponding points. After all points have been summed, the total score on the total point line is plotted and a vertical line is drawn down to the bottom line. The point where this line crosses the lowest line indicates the predicted probability of in-hospital death.
Abbreviation: BMI, body mass index.
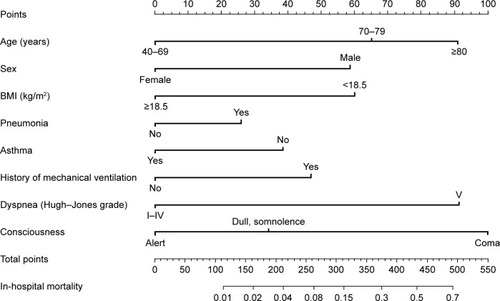
Figure 3 Calibration plot.
Discussion
In this study, we used data obtained from a nationwide inpatient database in Japan to evaluate factors associated with in-hospital mortality of patients with COPD exacerbation on admission. We then generated a prognostic nomogram for COPD exacerbation, using individual patients’ status on admission.
The prognosis of patients with COPD exacerbations requiring admission is generally poor, with in-hospital mortality reportedly being around 7%. In this study, the in-hospital mortality was 6.8%, which is consistent with findings of previous studies.Citation7–Citation13
Many studies have reported an association between lower BMI and higher long-term mortality of patients with COPD exacerbations.Citation20–Citation22 In addition, a previous study demonstrated that lower BMI was associated with higher hospital mortality.Citation10 Our study also demonstrated the association and was consistent with the previous study.
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines point out that previous use of mechanical ventilation is an important factor in the assessment of COPD exacerbations.Citation23 Use of all-cause mechanical ventilation has also been identified as a risk factor for increased in-hospital mortality of patients with COPD exacerbations requiring admission to the ICU.Citation24 In the current study, we found an association between previous use of mechanical ventilation for COPD exacerbations and in-hospital mortality.
Some studies have reported that pneumonia is associated with higher in-hospital or 30-day mortality;Citation25,Citation26 these findings are consistent with the results of our study. However, other studies have failed to show a significant association between pneumonia and mortality; the in-hospital mortality was relatively low in these studies, around 3%.Citation27,Citation28
We also identified a negative association between asthma and in-hospital mortality. Considerable attention has recently been paid to asthma–COPD overlap syndrome (ACOS). Patients with ACOS reportedly have more frequent exacerbations than patients with COPD without asthma, and patients with ACOS are suspected to have a poorer long-term prognosis than those with COPD alone.Citation29 However, a recent study found that patients with ACOS had better short- and long-term prognoses than clinically similar patients with COPD but without asthma.Citation30 In the current study, we confirmed an association between lower short-term mortality of COPD exacerbations and asthma. It has been suggested that systemic corticosteroids administered for asthma may play a part in this, but a definitive explanation has not been identified.Citation31
We also evaluated the association between amount of smoking and in-hospital mortality; however, a univariate analysis showed that there was no significant relation between amount of smoking and in-hospital mortality (P=0.746).
Some tools for predicting in-hospital mortality in patients hospitalized with COPD exacerbations have already been developed.Citation10,Citation11 One of them was the “DECAF” score, which comprises five predictors (stable state dyspnea, eosinopenia, consolidation, acidemia, and atrial fibrillation).Citation10 More recently, a decision tree for predicting 30-day mortality was developed; it uses older age, state of consciousness, stable state dyspnea, cardiopathy, use of inspiratory accessory muscles, and paradoxical breathing.Citation11 Some of these predictors are the same as ours. We believe that our nomogram has the following two advantages over these tools. First, our nomogram is based on easily accessible data and is thus easy for clinicians to use. For example, it does not require any laboratory data. Several prediction tools require laboratory data, such as pH and eosinophil count.Citation10 However, such data are not always readily available in clinical settings. Second, our nomogram only requires data that are available on admission, whereas the other prediction tools require data that may be unavailable on admission (eg, stable state dyspnea).
This study has some limitations. The database does not include the stage of COPD or the forced expiratory volume in 1 second, so we could not evaluate the association between stages of COPD severity and mortality, nor could we indicate the stages of COPD on the nomogram. Additionally, the DPC database does not include data of earlier exacerbations without hospitalizations. For using the nomogram in clinical practice, we would require prospective studies in order to compare the estimated in-hospital mortality with the prospective data.
Conclusion
We have developed a nomogram based on factors that affect in-hospital mortality of COPD exacerbations. This nomogram could help clinicians to predict risk of in-hospital mortality in individual patients with COPD exacerbation and thus help them to provide better care to patients and appropriate clinical information to patients and their families.
Acknowledgments
This study was supported by grants from the Ministry of Health, Labour and Welfare, Japan. We presented this research at the Congress of the Asian Pacific Society of Respirology 2016 (poster presentation) and published the abstract of this research.Citation32
Disclosure
The authors report no conflicts of interest in this work.
References
- BuistASMcBurnieMAVollmerWMBOLD Collaborative Research GroupInternational variation in the prevalence of COPD (the BOLD Study): a population-based prevalence studyLancet2007370958974175017765523
- World Health OrganizationFact sheet No. 310. The top 10 causes of death [updated May 2014] Available from: http://www.who.int/media-centre/factsheets/fs310/en/Accessed May 6, 2016
- World Health OrganizationChronic obstructive pulmonary disease (COPD) Available from: http://www.who.int/respiratory/copd/burden/en/Accessed May 6, 2016
- BurgeSWedzichaJACOPD exacerbations: definitions and classificationsEur Respir J Suppl20034146s53s12795331
- MiravitllesMFerrerMPontÀIMPAC Study GroupEffect of exacerbations on quality of life in patients with chronic obstructive pulmonary disease: a 2 year follow-up studyThorax200459538739515115864
- PływaczewskiRMaciejewskiJBednarekMCauses of deaths in COPD patients in primary care setting – a 6-year follow-upPneumonol Alergol Pol201583319320226050979
- BuckinghamRJLoweDPurseyNAReport of The National Chronic Obstructive Pulmonary Disease Audit 2008: clinical audit of COPD exacerbations admitted to acute NHS units across the UK Royal College of Physicians [updated November 2008] Available from: https://www.rcplondon.ac.uk/projects/outputs/national-copd-audit-2008Accessed October 29, 2016
- Bustamante-FermoselADe Miguel-YanesJMDuffort-FalcóMMuñozJMortality-related factors after hospitalization for acute exacerbation of chronic obstructive pulmonary disease: the burden of clinical featuresAm J Emerg Med200725551552217543654
- ConnollyMJLoweDAnsteyKBritish Thoracic Society and the Royal College of Physicians Clinical Effectiveness Evaluation Unit (CEEu)Admissions to hospital with exacerbations of chronic obstructive pulmonary disease: effect of age related factors and service organisationThorax2006611084384816928716
- SteerJGibsonJBourkeSCThe DECAF Score: predicting hospital mortality in exacerbations of chronic obstructive pulmonary diseaseThorax2012671197097622895999
- EstebanCArosteguiIGarcia-GutierrezSIRYSS-COPD GroupA decision tree to assess short-term mortality after an emergency department visit for an exacerbation of COPD: a cohort studyRespir Res20151615126695935
- HuGZhouYWuYYuYLiangWRanPThe Pneumonia Severity Index as a predictor of in-hospital mortality in acute exacerbation of chronic obstructive pulmonary diseasePLoS One2015107e013316026186637
- HoTWTsaiYJRuanSYThe HINT Study GroupIn-hospital and one-year mortality and their predictors in patients hospitalized for first-ever chronic obstructive pulmonary disease exacerbations: a nationwide population-based studyPLoS One2014912e11486625490399
- LiuRZZhaoZRNgCSStatistical modelling for thoracic surgery using a nomogram based on logistic regressionJ Thorac Dis201688E731E73627621910
- SugiharaTYasunagaHHoriguchiHA nomogram predicting severe adverse events after ureteroscopic lithotripsy: 12,372 patients in a Japanese national seriesBJU Int2013111345946623253797
- SheYZhaoLDaiCPreoperative nomogram for identifying invasive pulmonary adenocarcinoma in patients with pure ground-glass nodule: a multi-institutional studyOncotarget2017810172291723827542241
- OhtaTKikuchiHHashiKKudoYNizofenone administration in the acute stage following subarachnoid hemorrhage. Results of a multi-center controlled double-blind clinical studyJ Neurosurg19866434204263512795
- Hugh-JonesPLambertAVA simple standard exercise test and its use for measuring exertion dyspnoeaBr Med J195214749657114896031
- BalachandranVPGonenMSmithJJDeMatteoRPNomograms in oncology: more than meets the eyeLancet Oncol2015164e173e18025846097
- CaoCWangRWangJBunjhooHXuYXiongWBody mass index and mortality in chronic obstructive pulmonary disease: a meta-analysisPLoS One201278e4389222937118
- StollPFoersterSVirchowJCLommatzschMOverweight is a predictor of long-term survival in hospitalised patients with exacerbations of COPDRespir Med2016116596227296822
- PiquetJChavaillonJMDavidPFrench College of General Hospital Respiratory Physicians (CPHG)High-risk patients following hospitalisation for an acute exacerbation of COPDEur Respir J201342494695523349446
- Goldcopd.orgThe Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) [updated 2016] Available from: http://www.goldcopd.org/Accessed August 10, 2016
- Ai-PingCLeeKHLimTKIn-hospital and 5-year mortality of patients treated in the ICU for acute exacerbation of COPD: a retrospective studyChest2005128251852416100133
- SteerJNormanEMAfolabiOAGibsonGJBourkeSCDyspnoea severity and pneumonia as predictors of in-hospital mortality and early readmission in acute exacerbations of COPDThorax201267211712121896712
- SøgaardMMadsenMLøkkeAHilbergOSørensenHTThomsenRWIncidence and outcomes of patients hospitalized with COPD exacerbation with and without pneumoniaInt J Chron Obstruct Pulmon Dis20161145546527042038
- HuertaACrisafulliEMenéndezRPneumonic and nonpneumonic exacerbations of COPD: inflammatory response and clinical characteristicsChest201314441134114223828375
- AndreassenSLLiaaenEDStenforsNHenriksenAHImpact of pneumonia on hospitalizations due to acute exacerbations of COPDClin Respir J201481939923889911
- AlshabanatAZafariZAlbanyanODairiMFitzGeraldJMAsthma and COPD Overlap Syndrome (ACOS): a systematic review and meta-analysisPLoS One2015109e013606526336076
- CosioBGSorianoJBLópez-CamposJLCHAIN StudyDefining the asthma-COPD overlap syndrome in a COPD cohortChest20161491455226291753
- YamauchiYYasunagaHMatsuiHComparison of in-hospital mortality in patients with COPD, asthma and asthma-COPD overlap exacerbationsRespirology201520694094625998444
- SakamotoYYamauchiYYasunagaHPoster Presentation 1 – Respiratory Infections (Non-Tuberculous) 1. APSR6-0311: Development of a nomogram to predict in-hospital mortality of patients admitted due to exacerbation of COPDRespirology201621S38021327005369