Abstract
Objective
The purpose of this study was to explore the insulin-like growth factor binding protein 7 (IGFBP7) level in the serum of chronic obstructive pulmonary disease (COPD) patients during acute exacerbation (AE).
Methods
The study population consisted of 47 AECOPD patients, including 25 patients enrolled between January 2011 and February 2011 (the first group) and 22 patients enrolled from December 2011 to August 2012 (the second group) and 29 healthy controls. Chemiluminescence–linked immunoassay was used to detect serum IGFBP7 levels. For the second group patients, IGFBP7 and C-reactive protein (CRP) levels were measured both on the admission day and on the discharge day.
Results
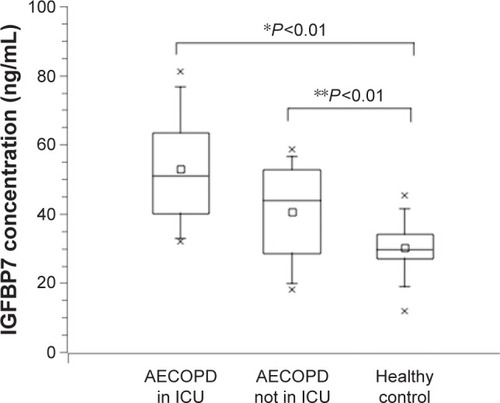
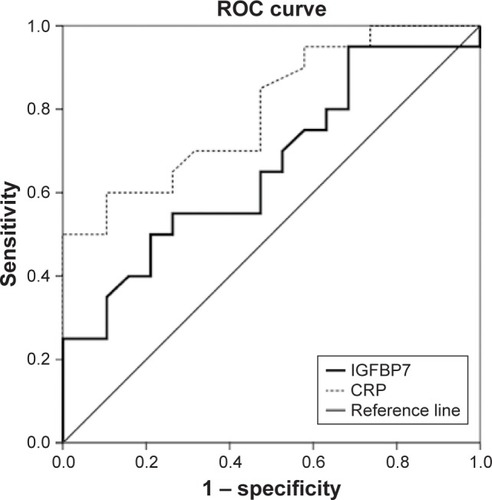
Among the first group AECOPD patients, serum IGFBP7 levels were significantly elevated in AECOPD patients in the intensive care unit (ICU; 52.92±16.32 ng/mL), and in hospitalized AECOPD patients not in ICU (40.66±13.9), compared to healthy subjects (30.3±7.09 ng/mL; P<0.01). For the second group AECOPD patients, the increased IGFBP7 levels reduced after the patients had recovered (34.42±11.88 vs 27.24±7.2 ng/mL; P<0.01). During AE, the correlation coefficient between IGFBP7 and CRP was 0.357. In receiver operating characteristic analysis, the area under the curve was 0.799 for CRP, and 0.663 for IGFBP7 in distinguishing patients with AECOPD on the admission day from the discharge day.
Conclusion
Serum IGFBP7 levels were raised during AECOPD. Similar to the expression pattern of CRP, the IGFBP7 levels reduced after convalescence, suggesting that IGFBP7 might have a candidate role as a biomarker of AECOPD. No significant linear correlation was detected between IGFBP7 and CRP, indicating the probable different role for the two molecules in assessing AECOPD. Further study is needed to explore the value of IGFBP7 in differentiating phenotypes of AECOPD.
Introduction
Acute exacerbation of chronic obstructive pulmonary disease (AECOPD) results in emergency room visits and hospitalizations, which are responsible for most mortality in COPD patients.Citation1 The diagnosis of AE depends on the acute change in the patient’s symptoms, including productive cough and dyspnea.Citation2,Citation3 Multiple growth factors are upregulated during airway inflammation, promoting COPD pathogenesis by causing airway remodeling and disrupting interstitial tissue and alveolar integrity, leading to airway narrowing, parenchymal damage, emphysema, and impaired lung function.Citation4 The systemic low-grade inflammation in stable COPD increases during AE.Citation5,Citation6 Identification of serum biomarkers could help clinicians to better manage and prevent exacerbations. Biomarkers may fluctuate in accordance with disease state, which may provide important clues to the potential signaling pathways of the disease.Citation7
The insulin-like growth factor binding protein (IGFBP) family serves as a group of carrier proteins for insulin-like growth factor-1 (IGF-1). Recently, the role of an IGFBP family member, like IGFBP3, has been reported to function in airway inflammation.Citation8 Among the IGFBP superfamily members, the binding affinity of IGFBP7 to IGFs was lower than conventional IGFBP1–6. On the contrary, the protein had high binding affinity to insulin.Citation9 In recent years, the functional role of IGFBP7 has been explored. The protein is associated with cell growth, senescence, and cell adhesion.Citation10 IGFBP7 was found in unfractionated bronchoalveolar lavage cells (BALC) and in activated human alveolar macrophage precursor peripheral blood monocytes, suggesting the expression pattern of IGFBP7 in normal human airway and alveoli.Citation11 Muller et al reported an increased expression of senescence-associated IGFBP7 in fibroblasts from emphysema patients.Citation12 Airway inflammation is the key character of the human chronic airway diseases.Citation13 The intriguing possibility of involvement of IGFBP7 in AECOPD merits further investigation. This study aimed to investigate the expression level of IGFBP7 in hospitalized COPD patients during AE.
Materials and methods
Study population
The diagnosis of COPD referred to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines. Exacerbations were defined according to the GOLD criteria. Selected COPD patients were excluded if they were diagnosed with active pulmonary tuberculosis, cancer, interstitial lung disease, or clinically significant bronchiectasis. The study population consisted of 47 AECOPD patients. Two independent AECOPD patient groups were included in the study. From January 2011 to February 2011, 25 hospitalized AECOPD patients were enrolled (the first group); among them 11 patients were admitted in intensive care unit (ICU) requiring assisted ventilation owing to severe acute exacerbations. From December 2011 to August 2012, 22 hospitalized AECOPD patients were enrolled (the second group). Twenty-nine age-matched healthy subjects were included in the study. Healthy controls were selected from the population on the basis of routine physical examination. All patients gave written informed consent. The research started after agreement from the Medical Ethics Committee of the Sir Run Run Shaw Hospital.
Study design
A venous blood sample was obtained from each hospitalized AECOPD patient on admission day. Serum IGFBP7 was measured. Arterial blood gases were measured at the same time. For the analysis of the arterial blood gases, the delay between sampling and measurement was <30 minutes. Age, sex, smoking history, and length of hospital stay were recorded.
Owing to a different research goal, for the second group of patients, a sample for the analysis of white blood cell count (WBC), neutrophil count, C-reactive protein (CRP), and procalcitonin (PCT) was obtained at the same time. To detect IGFBP7 and CRP levels in COPD patients who had recovered from AE, follow-up venous blood samples were obtained on the discharge day in the second group of patients. The decisions to discharge were based on the GOLD guidelines.Citation14
Blood sampling
Volume conductivity scatter technology was applied for WBC and differential counts (Coutlet hematology analyzer LH780; Beckman Coulter Inc, Brea, CA, USA). For biochemical measurements, the supernatants were stored at −70°C after centrifugation at room temperature at 2,000× g. The separated serum sample was aliquoted into sterile microcentrifuge tubes (500 µL each vial), then stored at −80°C.
Biochemical measurements
Polyclonal and monoclonal anti-IGFBP7 antibody was purchased from R&D Systems Inc. (Abingdon, UK). Chemiluminescence-linked immunoassay was used to detect serum IGFBP7 levels.Citation15 Enzyme-linked fluorescent assay (ELFA) was used to detect CRP and PCT levels (BioMerieux Vidas, Lyon, France).
Statistical analyses
Quantitative data were expressed as means ± standard deviations (SD). Chi-square test was used to compare the baseline clinical characteristics of the patients. One-way analysis of variance was used to detect the differences between subject groups. P-values <0.05 were considered statistically significant.
Spearman correlation analysis was performed to find the correlations between IGFBP7 and CRP levels in the patients suffering from AE. All statistical analyses were performed using SPSS for Windows, version 20.0 (IBM Corporation, Armonk, NY, USA).
Results
Characteristics of subjects
The baseline characteristics of the 25 AECOPD patients of the first group and healthy control subjects are summarized in . To verify the biomarker candidates, an independent panel of 22 hospitalized AECOPD subjects was used for the second group ().
Table 1 Baseline characteristics of the subjects of the first group
Table 2 Characteristics of the AECOPD subjects in the second group
Serum IGFBP7 increased in AECOPD patients in the first group
We first detected IGFBP7 levels in AECOPD patients in the first group. Among the 25 AECOPD patients, 11 were admitted to the ICU. IGFBP7 level in the ICU group, non-ICU group, and healthy control group were 52.92±16.32, 40.66±13.9, and 30.3±7.09 ng/mL, respectively. The increase in IGFBP7 compared with the healthy control group was significant (P<0.01; ). The level of IGFBP7 in AECOPD patients in ICU was higher than the other AECOPD patients, but not significant (P>0.05).
The increased IGFBP7 levels reduced after clinical recovery in the second group
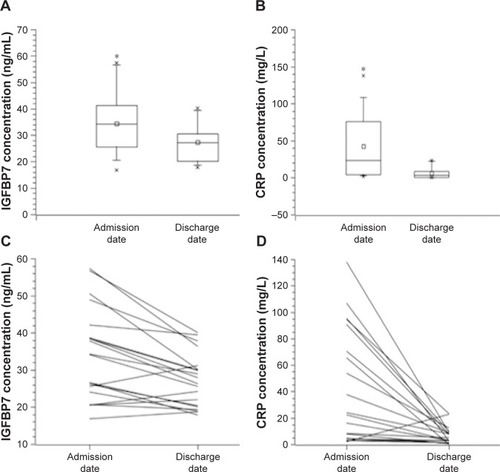
To reduce the potential bias, we verified the results in another population of 22 hospitalized AECOPD patients (the second group). The blood samples were obtained both on the admission day of AE and on the discharge day after recovery. Because of hemolysis during processing on the discharge day in two patients, a total of 20 follow-up samples were obtained. Serum IGFBP7 and CRP levels were both measured. We found that the increased serum IGFBP7 and CRP levels reduced after clinical recovery (IGFBP7: 34.42±11.88 vs 27.24±7.20 ng/mL; CRP: 42.6±43.27 vs 6.61±6.62 ng/mL) (P<0.01; ).
Figure 2 Serum IGFBP7 and CRP concentrations during exacerbations and after clinical improvement in AECOPD patients in the second group.
Abbreviations: AECOPD, acute exacerbation of chronic obstructive pulmonary disease; IGFBP7, insulin-like growth factor binding protein 7; ICU, intensive care unit; CRP, C-reactive protein.
No significant linear correlation existed between IGFBP7 and CRP during AE
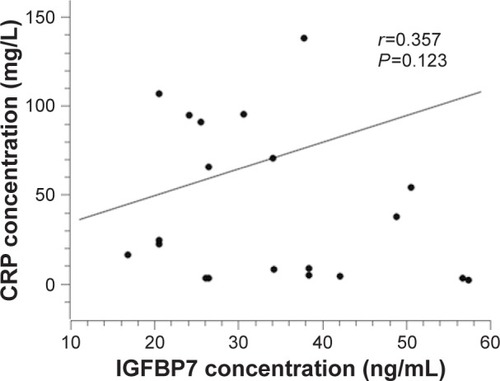
Both IGFBP7 and CRP levels increased during AE and reduced again after clinical recovery. To assess the correlation between IGFBP7 and CRP, Spearman correlation analysis was performed. However, unexpectedly, the correlation analysis between IGFBP7 and CRP showed no significant linear correlation between IGFBP7 and CRP during AE (=0.357, P=0.123).
Figure 3 Correlation of serum IGFBP7 levels with CRP levels in patients with COPD exacerbations in the second group.
Abbreviations: IGFBP7, insulin-like growth factor binding protein 7; CRP, C-reactive protein; COPD, chronic obstructive pulmonary disease.
Distinguishing power of IGFBP7 and CRP in patients with AECOPD
The area under the curve in receiver operating characteristic (ROC) analysis was 0.799 for CRP and 0.663 for IGFBP7 in distinguishing patients with AECOPD on the admission day from the discharge day ().
Figure 4 ROC curve for IGFBP7 and CRP in discrimination of AECOPD patients on the admission day and discharge day in the second group.
Discussion
To our knowledge, this is the first study investigating the expression of IGFBP7 in AECOPD patients. Serum IGFBP7 levels were found to be significantly raised in patients suffering from AE compared to healthy subjects. To reduce the potential bias, we verified the results in another population of hospitalized AECOPD patients. In the second group of AECOPD subjects, the increased IGFBP7 levels reduced after recovery.
A comprehensive approach to biomarkers could potentially revolutionize the diagnosis and management of AECOPD. The increased level of serum biomarkers during AE could help clinicians to identify AECOPD early in the clinical course to enable intervention. In recent years, biomarker candidates have been reported for AECOPD.Citation16–Citation19 Chen et al conducted a systematic review. CRP, interleukin-6, and tumor necrosis factor-alpha were the most frequently studied biomarkers. Compared to convalescence, only CRP levels were found to be consistently increased during AE.Citation16 The increase in CRP during AECOPD and decrease at recovery was confirmed in our study. As in the CRP expression pattern, IGFBP7 concentrations also appeared to be raised during AE compared with recovery, suggesting that IGFBP7 might be a biomarker candidate of AECOPD and a biomarker candidate in the assessment of treatment response.
We then analyzed the relation between IGFBP7 expression and CRP expression during AE of COPD. However, unexpectedly, we were unable to detect any significant linear correlation between IGFBP7 and CRP (r=0.357, P=0.123). We hypothesized that there must be some difference between IGFBP7 and CRP, although they both increased during AE. Although the ROC analysis showed that the diagnostic value of IGFBP7 in AECOPD is weaker than CRP, IGFBP7 probably has its own value in the diagnosis of AECOPD. COPD exacerbations are heterogeneous in etiology, and are almost clinically indistinguishable. Bafadhel et al identified distinct subtypes in AECOPD.Citation20 The subtypes related to bacterial infection, viral infection, and increased eosinophil counts were ~55%, 29%, and 28%, respectively.Citation20 Management of AECOPD should depend on the different phenotype.Citation21 Serum biomarkers capable of identifying different AECOPD phenotypes should guide suitable treatment. Bacterial infection is the main cause for AECOPD.Citation22 CRP is a potentially useful biomarker indicating bacterial infection. The raised CRP in AECOPD may suggest benefit from antibiotic therapy.Citation23 In our study, CRP increased in most AECOPD cases. However for some of the hospitalized AECOPD patients, the CRP levels were almost normal. This phenomenon may be due to viral infection or environmental factors which can also lead to AE. While for these AECOPD patients with normal CRP level, the expression of IGFBP7 increased.Citation20–Citation24
Our study suggests that IGFBP7 expression in patients in ICU needing assistant ventilation was higher than in the patients not in ICU, although the difference was not statistically significant. In the ICU group, one patient, with the highest IGFBP7 expression during AE (81.2 ng/mL), died within 3 days. We wanted to clarify whether the increase in IGFBP7 was due to the severe bacterial infection. Circulating PCT levels are raised in severe bacterial infections, but not in viral infections or in non-specific inflammatory diseases.Citation24 We explored the relationship between IGFBP7 and PCT. As a result, almost no correlation between the two molecules was found (r=0.178, data not shown). We believe that the serum IGFBP7 level during AE of COPD should not be used to indicate severe bacterial infection. We hypothesized that the level of serum IGFBP7 was probably an indication of airway inflammation during AE. The role of IGFBP7 in airway inflammation and airway remodeling needs further exploration. Further study is needed to explore the value of IGFBP7 to distinguish AECOPD phenotypes.
In conclusion, the present study provides the first evidence that serum IGFBP7 levels are raised during AE of COPD. After convalescence, the levels reduced, suggesting that IGFBP7 might be a biomarker candidate of AECOPD and a biomarker candidate in the assessment of treatment response. However, no significant linear correlation between IGFBP7 and CRP was found. There is a considerable need to explore the value of IGFBP7 in differentiating AECOPD phenotypes, while the detailed mechanism of IGFBP7 in airway inflammation and airway remodeling awaits further study.
Author contributions
WR designed the experiments, collected the clinical data, and drafted the manuscript; MW analyzed the data; FL, LS, and LD collected the serum samples; YQ and XW collected the clinical data; KY conceived and designed the experiments. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
This work was supported by the Zhejiang Provincial Natural Science Foundation of China (LY17H160007). We thank Dr Brian Eyden (Manchester, UK) for assistance with English language expression.
Disclosure
The authors report no conflicts of interest in this work.
References
- CelliBRBarnesPJExacerbations of chronic obstructive pulmonary diseaseEur Respir J20072961224123817540785
- Rodriguez-RoisinRToward a consensus definition for COPD exacerbationsChest20001175 Suppl 2398S401S10843984
- RabeKFHurdSAnzuetoAGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med2007176653255517507545
- TuderRMPetracheIPathogenesis of chronic obstructive pulmonary diseaseJ Clin Invest201212282749275522850885
- CreutzbergECWoutersEFVanderhoven-AugustinIMDentenerMAScholsAMDisturbances in leptin metabolism are related to energy imbalance during acute exacerbations of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med20001624 Pt 11239124511029324
- DentenerMACreutzbergECScholsAMSystemic anti-inflammatory mediators in COPD: increase in soluble interleukin 1 receptor II during treatment of exacerbationsThorax200156972172611514694
- YoonHISinDDBiomarkers of therapeutic response in patients with chronic obstructive pulmonary disease: a critical review of the literatureDrugs201171141821183721942975
- LeeHKimSROhYChoSHSchleimerRPLeeYCTargeting insulin-like growth factor-I and insulin-like growth factor-binding protein-3 signaling pathways. A novel therapeutic approach for asthmaAm J Respir Cell Mol Biol201450466767724219511
- YamanakaYWilsonEMRosenfeldRGOhYInhibition of insulin receptor activation by insulin-like growth factor binding proteinsJ Biol Chem19972724930729307349388210
- WilsonHMBirnbaumRSPootMQuinnLSSwisshelmKInsulin-like growth factor binding protein-related protein 1 inhibits proliferation of MCF-7 breast cancer cells via a senescence-like mechanismCell Growth Differ200213520521312065244
- AllenJTBloorCAKediaRKKnightRASpiteriMAExpression of growth hormone-releasing factor, growth hormone, insulin-like growth factor-1 and its binding proteins in human lungNeuropeptides20003429810710985926
- MullerKCWelkerLPaaschKLung fibroblasts from patients with emphysema show markers of senescence in vitroRespir Res200673216504044
- StarkeyMRJarnickiAGEssilfieATMurine models of infectious exacerbations of airway inflammationCurr Opin Pharmacol201313333734423566696
- VestboJHurdSSAgustiAGGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med2013187434736522878278
- LiuYWuMLingJSerum IGFBP7 levels associate with insulin resistance and the risk of metabolic syndrome in a Chinese populationSci Rep201551022725984973
- ChenYWLeungJMSinDDA Systematic review of diagnostic biomarkers of COPD exacerbationPLoS One2016117e015884327434033
- ChoYJMaJEYunEYSerum angiopoietin-2 levels are elevated during acute exacerbations of COPDRespirology201116228429021143700
- BozinovskiSHutchinsonAThompsonMSerum amyloid a is a biomarker of acute exacerbations of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2008177326927818006888
- LeungJMChenVHollanderZCOPD exacerbation biomarkers validated using multiple reaction monitoring mass spectrometryPLoS One2016118e016112927525416
- BafadhelMMcKennaSTerrySAcute exacerbations of chronic obstructive pulmonary disease: identification of biologic clusters and their biomarkersAm J Respir Crit Care Med2011184666267121680942
- BafadhelMMcKennaSTerrySBlood eosinophils to direct corticosteroid treatment of exacerbations of chronic obstructive pulmonary disease: a randomized placebo-controlled trialAm J Respir Crit Care Med20121861485522447964
- SethiSMurphyTFInfection in the pathogenesis and course of chronic obstructive pulmonary diseaseN Engl J Med2008359222355236519038881
- DanielsJMSchoorlMSnijdersDProcalcitonin vs C-reactive protein as predictive markers of response to antibiotic therapy in acute exacerbations of COPDChest201013851108111520576731
- AssicotMGendrelDCarsinHRaymondJGuilbaudJBohuonCHigh serum procalcitonin concentrations in patients with sepsis and infectionLancet199334188445155188094770