Abstract
Severe exacerbations of COPD, ie, those leading to hospitalization, have profound clinical implications for patients and significant economic consequences for society. The prevalence and burden of severe COPD exacerbations remain high, despite recognition of the importance of exacerbation prevention and the availability of new treatment options. Severe COPD exacerbations are associated with high mortality, have negative impact on quality of life, are linked to cardiovascular complications, and are a significant burden on the health-care system. This review identified risk factors that contribute to the development of severe exacerbations, treatment options (bronchodilators, antibiotics, corticosteroids [CSs], oxygen therapy, and ventilator support) to manage severe exacerbations, and strategies to prevent readmission to hospital. Risk factors that are amenable to change have been highlighted. A number of bronchodilators have demonstrated successful reduction in risk of severe exacerbations, including long-acting muscarinic antagonist or long-acting β2-agonist mono- or combination therapies, in addition to vaccination, mucolytic and antibiotic therapy, and nonpharmacological interventions, such as pulmonary rehabilitation. Recognition of the importance of severe exacerbations is an essential step in improving outcomes for patients with COPD. Evidence-based approaches to prevent and manage severe exacerbations should be implemented as part of targeted strategies for disease management.
Introduction
Exacerbations of COPD are important events in the course of the disease that have profound impact on patients’ health status, functional capacity, and lung function.Citation1,Citation2 The severity of exacerbations varies, and the clinical definition of a severe exacerbation is not always uniform; for practical reasons, clinical trials and epidemiological studies normally define severe exacerbations as those resulting in hospitalization.Citation3 Severe exacerbations have a particularly significant clinical and socioeconomic impact. A recent database review of >73,000 patients found that fewer than half of patients hospitalized for an exacerbation survived for a further 5 years.Citation4 Patients who survive severe exacerbations are likely to experience significantly impaired quality of life (QoL), are at increased risk of further exacerbations,Citation5,Citation6 and represent a major contributor to the overall health-care costs associated with COPD.Citation7,Citation8 Therefore, understanding the factors that lead to an exacerbation being so severe that treatment in hospital is needed, and optimization of patient management to reduce the risk of severe exacerbations, are crucial therapeutic goals for patients with stable COPD.
Currently, the prevalence and burden of severe exacerbations remain high,Citation9,Citation10 despite advances in COPD therapies and increased recognition of the importance of preventing exacerbations. This manuscript reviews the risk factors, consequences, and treatment of severe COPD exacerbations, and highlights opportunities to improve the management and prevention of these serious events.
What constitutes a severe exacerbation?
An exacerbation is typically considered an acute episode characterized by worsening of the patient’s respiratory symptoms (ie, baseline dyspnea, cough, and/or sputum production) that is sufficient to require additional therapy.Citation11,Citation12 The American Thoracic Society (ATS)/European Respiratory Society (ERS) guidelines classify any exacerbation that can be managed at home (mild or moderate) as level I, while severe exacerbations are stratified further as those requiring hospitalization (level II) and those leading to respiratory failure (level III).Citation12 For the purposes of this review, severe exacerbations refers to exacerbations requiring hospitalization, accepting that exacerbations requiring hospitalization may be quite varied in terms of the severity of respiratory symptoms and will also reflect the underlying severity of the patient’s lung impairment. In patients with very limited respiratory reserves, less severe exacerbation events may still require hospitalization for effective management. Additional factors that contribute to the decision to admit a patient to hospital include the presence of such comorbidities as heart failure, cardiac arrhythmia, or pneumonia, or the onset of other clinical signs, such as central cyanosis or peripheral edema.Citation11,Citation12 Patients may go into hospital as an acute emergency admission or be admitted only after outpatient management of an exacerbation has failed to produce an adequate response. Psychosocial factors may also be involved: the patient’s ability to cope at home, which may be a product of their age, mental status, and the level of support they have available to them, is an important consideration in deciding whether they should be treated for an exacerbation as an inpatient or outpatient.Citation11–Citation13 Finally, regional differences in local health-care practices and access to health-care services also influence the threshold that determines hospitalization for patients with COPD suffering an exacerbation of COPD.Citation14
What are the likely clinical outcomes of severe COPD exacerbations?
Severe COPD exacerbations have short- and long-term clinical implications, including accelerated loss of lung function, increased mortality, decreased health status, cardiovascular comorbidity, and increased health-care costs.Citation7,Citation15,Citation16 An exacerbation has a significant effect on clinical and patient-centered outcomes, including obstruction, dyspnea, and exercise capacity. Patients take a long time to recover from these effects, and may never return to their preexacerbation state.Citation17
Impact on mortality
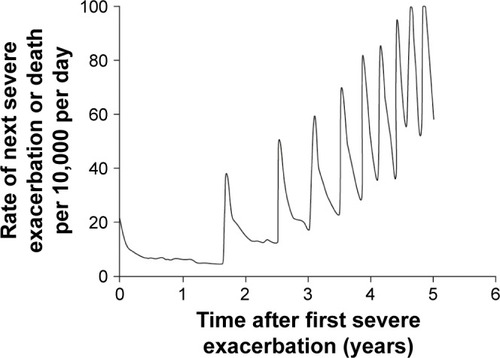
Hospitalization for COPD exacerbations is associated with a high mortality rate. In an EU COPD audit, 5% of patients admitted to hospital with a COPD exacerbation died while in hospital.Citation10 Consistent with this finding, a recent database review of >73,000 patients with up to 17 years’ follow-up found that mortality peaked in the first week and remained high during the first 3 months following hospital admission.Citation4 Fewer than half of patients hospitalized for an exacerbation were still alive after 5 years’ follow-up in this study.Citation4 This is consistent with previous reports of >50% mortality at 5 years following hospitalization for acute exacerbations of COPD.Citation18,Citation19 Long-term posthospitalization mortality rates reported in the literature are quite variable: 12%–33% after 1 year,Citation18–Citation22 26%–39% after 2 years,Citation18,Citation21,Citation22 39%–49% after 3 years,Citation18,Citation21,Citation22 and 45%–47% after 4 years.Citation18,Citation22 It has been suggested that survival following hospitalization for COPD is improving.Citation23 However, mortality associated with COPD may be underestimated, as it is often cited as a contributory, rather than underlying, cause of death, or omitted from death certificates altogether if death is primarily attributed to comorbid conditions.Citation24 The contribution of nonhospitalized exacerbations to mortality rates (ie, unreported exacerbations that should have warranted hospital treatment) has not been well quantified.Citation25 Mortality risk increases with each new exacerbation: there is a fivefold greater risk of mortality after the tenth hospitalization compared with the first ().Citation4
Figure 1 Hazard function of successive hospitalized COPD exacerbations (per 10,000 per day) for a cohort of 73,106 patients from the time of their first ever hospitalization for a COPD exacerbation over the follow-up period, with the time between successive exacerbations estimated using the median inter-exacerbation times as time to the next exacerbation or death, whichever occurs first.
Identified risk factors for mortality associated with severe exacerbation include older age, male sex, prior hospitalizations, weight loss/low body-mass index, poor QoL, physiological parameters (eg, partial pressure of carbon dioxide [PaCO2]), pulmonary hypertension, lung cancer, cardiovascular comorbidity, and need for long-term oxygen therapy at discharge.Citation4,Citation6,Citation9,Citation18,Citation19,Citation22,Citation26–Citation28
Health-related quality of life
Health-related QoL deteriorates in patients experiencing exacerbations; the more frequent and severe the exacerbation, the more rapid and pronounced the decline.Citation29–Citation31 Severe exacerbations lead to impairment of the ability to perform usual activities and reduce work productivity. Activity limitation and reduced work productivity have been found to be strongly correlated with the total number of severe exacerbations in the previous year.Citation30 Assessment of health-related QoL varies considerably between studies, and some measures do not include all domains of health status (physiological functioning, symptoms, functional impairment, and QoL).Citation32
Cardiovascular sequelae
Cardiovascular comorbidities are common in patients with COPD, and particularly in those patients with more severe airflow limitation. A review of studies of patients hospitalized for COPD exacerbations found that up to 55% of patients had a history of cardiovascular disease.Citation33 Exacerbations of COPD have a profound effect on patients’ cardiovascular status,Citation33–Citation35 and the increase in cardiac events after the first exacerbation is irrespective of the patient’s cardiac history.Citation36 Markers of myocardial injury, including raised troponin, chest pain, and serial electrocardiogram changes, are commonly observed in patients admitted to hospital with exacerbations of COPD.Citation33,Citation34 Levels of N-terminal pro–brain natriuretic peptide and cardiac troponin T are elevated during acute exacerbations of COPD and thought to be a predictor of mortality among patients admitted to hospital.Citation37 Arterial stiffness also rises acutely during COPD exacerbations, particularly when associated with airway infection.Citation35 These changes may also be associated with an acute increase in the risk of myocardial infarction (MI): a UK observational database study found a 2.3-fold increase in the risk of MI 1–5 days postexacerbation,Citation38 while analysis from the UPLIFT® study showed 13-fold increased risk of MI in the 30 days postexacerbation compared with preexacerbation periods. A 17-fold increase in the occurrence of atrial fibrillation/flutter was also seen in the 30-day postexacerbation period.Citation36
Increased prevalence of pulmonary embolism has also been reported in patients with COPD exacerbations. Two meta-analyses have reported an overall incidence of pulmonary embolism of 16%Citation39 and 20%,Citation40 increasing to 25% in hospitalized patients, including those hospitalized specifically for a COPD exacerbation.Citation40
What is the epidemiology and economic impact of severe exacerbations?
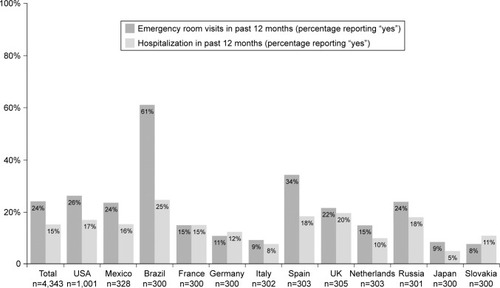
Rates of hospitalization for exacerbations of COPD vary in different countries, which may reflect differences in the organization of health-care systems. A large international survey of more than 4,000 patients with COPD sampled from 12 countries in Europe, the US, and Asia (Continuing to Confront COPD International Patient Survey) found that overall, 15% of patients had been hospitalized for an exacerbation in the previous 12 months, with rates ranging 5%–25% across individual countries ().Citation41 In another large multinational survey of more than 1,000 patients in Germany, France, Italy, Spain, the UK, and the US (PERCEIVE), 21% of patients who reported a COPD exacerbation in the preceding year were hospitalized.Citation42
Figure 2 Emergency room visits and hospitalizations due to COPD exacerbations: Continuing to Confront COPD International Patient Survey.
Severe COPD exacerbations are estimated to account for less than 10% of exacerbations,Citation43,Citation44 but have a disproportionate and significant socioeconomic impact, with hospitalizations estimated to account for approximately 60%–70% of health-care costs associated with COPD, depending on the region.Citation8,Citation45 Illustrative of the costs associated with COPD exacerbations, a recent health-economics analysis conducted in the US, based on a data set from 2006, identified a total of 1,254,703 hospitalizations for COPD exacerbations, with total inpatient costs of $11.9 billion over the year at a mean cost of $9,545 per hospitalized exacerbation.Citation46 The substantial burden of severe COPD exacerbations is apparent when considered in the context of overall health-care resource utilization. In the UK, acute exacerbations account for 115,000 hospital admissions per year, representing one of the most common reasons for emergency admission to hospital,Citation47 while in Spain it is estimated that 1%–2% of all emergency-service visits and 10% of all medical admissions are attributable to COPD exacerbations.Citation18
Despite trends toward an improvement in in-hospital mortality rates and a reduction in average length of hospital stay in the US,Citation9,Citation48 there has been no significant improvement in other indicators, including the number of hospital discharges, emergency-department visits, and 30-day readmissions within the period 2001–2012,Citation48 highlighting considerable room for improvement and opportunities for reduction in the costs associated with admissions for COPD exacerbations. Patients who have been admitted to hospital for a severe exacerbation of COPD are at substantial risk for rehospitalization,Citation19 with up to a quarter of patients readmitted for COPD exacerbations within 1 year following discharge.Citation9,Citation19 Strategies to reduce readmission rates are thus a priority in efforts to reduce the burden of severe COPD exacerbations.
What are the risk factors associated with severe COPD exacerbations?
The majority of COPD exacerbations, including severe exacerbations, are precipitated by respiratory tract infections, either viral or bacterial, or by environmental agents, eg, worsening air pollution.Citation49 Numerous disease-related and demographic characteristics that modify patients’ risk of having an exacerbation have been identified.
Severity of airflow limitation is a key risk factor for exacerbation requiring hospitalization. In a retrospective study of ambulatory COPD patients from general practices, severity of forced expiratory volume in 1 second impairment was a significant predictor for increased risk of hospitalizations, as was the presence of significant comorbidities, such as diabetes or ischemic heart disease.Citation50 The cross-sectional analysis of the PAC-COPD study found that patients with more severe respiratory symptoms, poorer QoL, worse lung function, and lower exercise capacity were at greater than threefold-higher risk of hospitalization for COPD than those with milder airflow limitation, with or without significant comorbidities (hazard ratio 3.28, P<0.001).Citation51
A summary of variables that have been shown to modify the risk of severe exacerbations of COPD is shown in .Citation4,Citation6,Citation18,Citation19,Citation26,Citation50–Citation78 These include lung function, symptoms (ie, severity of dyspnea), QoL, exacerbation history, disease history and treatment, age and sex, body-mass index, smoking status, and comorbidities. Other influences on the risk of severe COPD exacerbations include the patient’s socioeconomic background, education level, and marital status.
Table 1 Risk factors for severe exacerbations in COPD
Exacerbations may occur regardless of the degree of functional impairment, although it is generally agreed that the frequency of exacerbations increases with decreasing lung function.Citation1 A major audit of COPD treatment and outcomes in Europe was conducted by the ERS between 2010 and 2011. This gathered a wealth of data (from more than 16,000 admissions) profiling the demographic and disease characteristics of patients admitted to hospital for exacerbations across the continent.Citation10 The median age of patients admitted to hospital was 72 years.Citation10 Many patients requiring hospitalization due to an exacerbation had severe (Global Initiative for Chronic Obstructive Lung Disease [GOLD] grade 3, 39%) or very severe (GOLD grade 4, 22%) underlying COPD, but the proportion of patients with mild or moderate disease who experienced a severe exacerbation was not insignificant (GOLD grade 1, 15%; GOLD grade 2, 23%).Citation10 Major comorbidities included other pulmonary diseases (21%), congestive heart failure (20%), and diabetes (20%).Citation10
A systematic review of 37 COPD-treatment studies, with mean forced expiratory volume in 1 second percentage predicted lung function of mostly 35%–60%, estimated the annual frequency of severe exacerbations according to GOLD severity at 0.11 (GOLD grade 1, 95% CI 0.02–0.56), 0.16 (GOLD grade 2, 95% CI 0.07–0.33), 0.22 (GOLD grade 3, 95% CI 0.2–0.23), and 0.28 (GOLD grade 4, 95% CI 0.14–0.63).Citation65 In the ECLIPSE study, exacerbations were more frequent and severe with increased severity of disease: the proportion of patients hospitalized for COPD exacerbations with GOLD grade 2–4 (moderate–very severe COPD) was 7%, 18%, and 33%, respectively.Citation66
When we used the GOLD 2017 “ABCD” assessment tool (in which the lettering scale reflects symptom burden and risk of exacerbation)Citation11 to analyze patients included in the UPLIFT® trial, a greater proportion of patients (35%) in GOLD group D with higher symptom burden or exacerbation risk had experienced a severe exacerbation compared with patients with lower symptom burden or exacerbation risk (GOLD group A, 14%; group B, 22%; group C, 21%). Adjusted rates of severe COPD exacerbations (per patient-year) were (mean [95% CI]): GOLD group A, 0.07 (0.05–0.09); group B, 0.13 (0.12–0.14); group C, 0.13 (0.09–0.19); group D 0.28 (0.26–0.31) (Boehringer Ingelheim, data on file, 2017).
What are the recommended treatment strategies for severe COPD exacerbations?
Mortality statistics showing that the risk of death is highest in the first week following admission highlight the importance of prompt and effective intervention for patients admitted to hospital with severe exacerbations.Citation4 Pharmacological treatment options for severe exacerbations include bronchodilators (short-acting β-agonists with or without short-acting anticholinergics), corticosteroids (CSs) (eg, prednisone), and antibiotics when the symptoms are suggestive of bacterial infection (eg, change in sputum characteristics).Citation11,Citation12 Full recommendations for the pharmacological treatment of exacerbations using bronchodilators can be found in published guidelines.Citation11,Citation12
Antibiotics
Based on available evidence that shows a reduced risk of short-term mortality and treatment failure, current GOLD recommendations are for antibiotic treatment in those patients whose exacerbation symptoms indicate likely bacterial infection, ie, increased sputum volume and purulence, as well as increased dyspnea.Citation11 Antibiotics are also recommended for patients with exacerbations requiring mechanical ventilation, as this has been shown significantly to reduce mortality and the risk of secondary pneumonia.Citation11
In this era of increasing antibiotic resistance, two key considerations are avoiding the use of unnecessary antibiotic treatment (ie, in patients who do not show an increase in purulent sputum)Citation13 and ensuring that empiric treatment choices are selected based on knowledge of local bacteria-resistance patterns.Citation11 Treatment selection might also consider how the microbiology may differ in patients with severe exacerbations versus patients with mild or moderate disease.Citation79 The most common pathogens isolated from sputum and bronchoscopic samples are Haemophilus influenzae, Streptococcus pneumoniae, and Moraxella catarrhalis. However, in patients with more severe disease and/or exacerbations, Gram-negative pathogens, such as Pseudomonas aeruginosa, are common,Citation79,Citation80 and may prove more challenging to treat in light of increasing resistance in some regions. The role of procalcitonin as a potential biomarker for optimizing antibiotic-treatment strategy in COPD exacerbations (especially those induced by bacterial infection) is also being investigated; however, as yet its role is unproven.Citation81,Citation82 Further studies are required to guide optimal antibiotic treatment, based on investigation of biomarkers to identify patients expected to benefit, and to establish the optimal duration of treatment.Citation83
Corticosteroids
In the treatment of acute exacerbations of COPD, systemic CSs have been shown to reduce length of stay in hospital, provide earlier improvement in lung function and symptoms, and reduce the risk of treatment failure or relapse.Citation84 However, a US study has noted that critically ill patients admitted directly to an intensive care unit for the treatment of severe exacerbations often receive higher-than-recommended doses of CSs to combat inflammation in the lungs.Citation85 A large cohort study of patients receiving low-dose (methylprednisolone ≤240 mg/day; ~6,000 patients) or high-dose (methylprednisolone >240 mg/day; ~11,000 patients) CS treatment found that outcomes were in fact worse for patients treated with high doses of CSs.Citation85 Higher doses were on average associated with longer hospital stays, longer time in the intensive care unit, and corresponding higher costs, as well as more steroid-related adverse events, compared with patients on lower doses of CSs. No significant difference was observed between patients treated with oral or intravenous CSs in terms of treatment failure, hospital readmissions, or length of hospitalization; however, intravenous therapy might increase the risk of adverse events. Overall, available evidence does not recommend one method of administration over the other.Citation86
Optimal dosing regimens for oral CSs in patients with severe exacerbations have not been studied extensively; however, prolonged CS treatment is not recommended, in consideration of the adverse effects and lack of evidence for benefits of extended treatment. A recent meta-analysis suggested that a 5-day course of oral CSs was likely to be sufficient to treat patients hospitalized with a COPD exacerbation, and outcomes were not inferior to those with longer (10- to 14-day) courses.Citation87
Oxygen therapy
During exacerbations, patients with COPD may become significantly hypoxic.Citation88 Severe exacerbations disrupt the normal ventilation:perfusion ratio in the lungs, resulting in systemic hypoxemia, with poorly oxygenated blood returned to the left atrium.Citation88 In a Spanish cohort of 2,487 patients attending the emergency department due to acute exacerbation of COPD, 50% had hypoxemia (arterial oxygen saturation [SaO2] <90%).Citation89 Oxygen therapy is a key component in hospital treatment of patients with a severe exacerbation.Citation11
There are marked variations in the response of individual patients to oxygen, and oxygen therapy may lead to hypercapnia and acidosis.Citation90 Titrated controlled oxygen treatment for acute exacerbations has been associated with less acidosis, a lower requirement for assisted ventilation, and reduced mortality compared with high-flow oxygen.Citation91,Citation92 GOLD recommends titrating supplemental oxygen therapy to achieve a target saturation of 88%–92%.Citation11 To achieve optimal oxygenation without carbon dioxide retention and/or worsening acidosis, blood gases should be monitored frequently.Citation11
Ventilatory support
Several studies have characterized the physiological changes that occur during or immediately after acute exacerbations, and have shown that lung hyperinflation and worsening airflow obstruction are the critical factors that determine the course of respiratory symptoms.Citation93–Citation95 Ventilatory support for the management of respiratory failure can be provided by either noninvasive or invasive methods, dependent upon patient criteria. Since its introduction in the 1980s, the use of noninvasive ventilation (NIV) has significantly increased, and has been associated with a reduction in mortality of approximately 40% and significantly reduced risk of treatment failure, complications, and endotracheal intubation.Citation96 NIV is indicated in patients with respiratory acidosis (arterial pH ≤7.35), severe dyspnea with clinical indicators of respiratory muscle fatigue, increased work of breathing, or both, and in patients on supplemental oxygen therapy who continue to experience persistent hypoxemia.Citation11
It has been observed that patients who fail NIV and then transition to invasive mechanical ventilation have a higher rate of mortality compared with patients who start directly with invasive ventilation.Citation97 Therefore, it is important to evaluate further the factors that predict early failure of NIV: to date, studies have identified severe acidosis, tachycardia, high APACHE II score, and severe hypoxemia as risk factors for NIV failure in patients with COPD exacerbations.Citation12,Citation97–Citation99 Further guidance on the use of ventilator support can be found in the GOLD report and ATS/ERS guidelines.Citation11,Citation12
Preventing severe COPD exacerbations
The profound impact of severe COPD exacerbations on patients’ well-being and the substantial economic burden associated with hospitalization highlights the importance of risk reduction as a key component of COPD management. Strategies to reduce the risk of subsequent exacerbations following hospitalization might be considered secondary prevention in a similar way to the approach used in cardiology, using the index event as a critical point to review treatment and ensure optimal patient management to minimize the risk of future exacerbations.
Risk-factor modification
Smoking cessation
Smoking cessation has a substantial influence on the natural history of COPD, and is associated with a decrease in symptoms and improved health status. In a large observational cohort study of 23,971 US veterans, ex-smokers had a significantly reduced risk of COPD exacerbation compared with current smokers.Citation100 The magnitude of reduction in risk was dependent on the duration of smoking cessation. Despite the evidence supporting the significant risk reductions that can be achieved through smoking cessation, a substantial proportion of patients continue to smoke. For example, the EU COPD audit data showed that approximately a third of patients admitted to hospital with severe exacerbations in Europe in 2010–2011 were current smokers.Citation10 Reinforcing participation in smoking-cessation programs represents a significant opportunity to reduce exacerbation risk by targeting a modifiable risk factor, particularly at hospital discharge, when patients may be particularly motivated to stop smoking to avoid experiencing another severe exacerbation.
Vaccinations
Vaccination against influenza is a highly cost-effective intervention for exacerbation reduction,Citation101 and is recommended for all patients.Citation11 In a retrospective cohort study of 1,323 patients with COPD, vaccination against seasonal influenza significantly reduced hospitalization due to exacerbation versus patients who were not vaccinated.Citation102 Protection may be enhanced by the addition of pneumococcal vaccine (although additive effects of influenza and pneumococcal vaccinations were only observed during the first year after vaccination).Citation103
Pulmonary rehabilitation
Pulmonary rehabilitation may be offered after a severe exacerbation with the aim of restoring preexacerbation functional status, resuming physical activities in daily life, improving QoL, and reducing the risk of further exacerbations.Citation11,Citation101 The reported benefits of pulmonary rehabilitation on exacerbations of COPD have been mixed, but the balance of evidence supports its use.Citation104,Citation105 In a meta-analysis of nine trials in patients who had been hospitalized for an exacerbation, pulmonary rehabilitation significantly reduced future hospital admissions and mortality and improved QoL compared with usual community care.Citation106 Pulmonary rehabilitation may reduce future exacerbations by targeting modifiable risk factors for readmission, such as physical inactivity, reduced exercise capacity, impaired physical function, central desensitization to dyspnea, anxiety, and depression.Citation73,Citation104 Although the benefits of pulmonary rehabilitation are increasingly recognized and it is recommended in treatment guidelines for the prevention of acute exacerbations,Citation11,Citation13,Citation107 availability of pulmonary rehabilitation programs is often limited. For example, among hospitals surveyed in the EU COPD audit, only half offered a pulmonary rehabilitation program to patients discharged following a severe exacerbation (0%–90% across countries).Citation10 Identifying barriers to availability and uptake of pulmonary rehabilitation would be a useful step toward improving prevention strategies.
Self-management intervention programs
Self-management intervention programs improve outcomes for many chronic diseases. A disease-management plan for COPD should include an action plan for exacerbation prevention, designed in partnership with the physician and the patient, and taking into account the patient’s experience of an acute (severe) exacerbation.Citation101 Evidence for benefits of self-management plans for the prevention of COPD exacerbations is mixed. In one study, a self-management program for patients with COPD (comprising education on the disease, coughing and breathing techniques, energy conservation during daily activities, relaxation exercises, symptom prevention and control, an acute-exacerbation plan of action, and lifestyle advice, including nutrition and exercise) led to a 40% reduction in hospital admissions for exacerbations compared with usual care over 12 months.Citation108 Emergency visits were also reduced by 41% and unscheduled physician visits by 59%.Citation108 Extended follow-up for 2 years demonstrated sustained benefits.Citation62 A similar benefit was observed using a simplified disease-management program (a single education session, action plan for self-management of exacerbations, monthly follow-up calls).Citation109 However, another randomized trial of patients with COPD found that a home education and management program did not result in a reduction in admissions for exacerbations, and in fact showed an unexpected increase in mortality.Citation110 A Cochrane review suggested that overall, the balance of evidence supports the use of self-management programs to reduce the probability of respiratory-related hospitalizations,Citation111 and the American College of Chest Physicians and Canadian Thoracic SocietyCitation107 and ATS/ERS guidelinesCitation12 advocate their use.
Pharmacological strategies
Bronchodilators
Pharmacological agents currently available as maintenance treatment for COPD have varying efficacy for the prevention of COPD exacerbations. Long-term bronchodilator treatment with a long-acting muscarinic antagonist (LAMA), long-acting β2-agonist (LABA), or a combination of both have been shown to reduce the risk of severe exacerbations significantly.Citation25,Citation112,Citation113 provides a summary of large-scale randomized trials comparing the efficacy of inhaled maintenance COPD therapies in reducing exacerbation risk.Citation114–Citation134 The evidence base for LAMAs appears to be strongest, with a recent systematic review demonstrating that tiotropium is beneficial in reducing exacerbation risk versus placebo or other maintenance treatments, with longer time to first exacerbation event and fewer exacerbations (including hospitalizations) than either placebo or most active-comparator treatments.Citation113 A fixed-dose LAMA–LABA combination of glycopyrronium and indacaterol successfully reduced moderate–severe exacerbations in patients of GOLD grade 3 or 4 compared with glycopyrronium alone, but this was not significant for severe exacerbations only.Citation130 The FLAME study found that the combination of indacaterol–glycopyrronium significantly prolonged time to first severe exacerbation compared with salmeterol–fluticasone, although the annual rate of severe exacerbations was not significantly different between the two treatment groups; however, it has to be noted that the FLAME study was not powered to analyze differences in severe exacerbations between groups.Citation133
Table 2 Randomized, controlled clinical trials assessing the effectiveness of inhaled long-acting bronchodilators, ICS, or combination therapy for reducing the risk of severe (hospitalized) exacerbations of COPD
Despite the wealth of evidence to support tiotropium and other LAMAs in reducing the risk of severe exacerbations, data from the EU COPD audit indicate that they may be underutilized. Fewer than half of patients were on LAMA treatment prior to hospitalization, even though this patient population had been hospitalized once on average in the past year.Citation10 Discharge following an exacerbation presents a pivotal opportunity to ensure that maintenance treatment is optimized, in line with goal-directed treatment guidelines to reduce the risk of disease progression, exacerbations, and mortality. Medication review at discharge, and at the same time also ensuring correct inhaler technique, represents a valuable opportunity for improvements in pharmacological approaches to reducing exacerbation risk. Adhering to COPD-treatment guideline recommendations is likely to have a positive impact in terms of reducing the incidence of severe exacerbations. GOLD-adherent prescribing in COPD has been associated with significant reductions in proportions of patients with all-cause hospitalizations and emergency-department visits compared with nonadherent prescribing.Citation135
ICS and ICS combinations
Due to the possible adverse events of pneumonia and fractures resulting from inhaled CS (ICS) treatment, current guidelines recommend ICS-combination therapy only in patients with severe airflow limitation at minimum and/or with frequent exacerbations that are not controlled adequately with long-acting bronchodilators alone.Citation11,Citation13 The 3-year TORCH study found the ICS–LABA fluticasone–salmeterol combination therapy more effective than salmeterol alone in preventing moderate and severe exacerbations combined (rate ratio 0.88), but not for severe exacerbations only.Citation132 The overall lack of significant benefits of ICS–LABA treatment over LABA monotherapy was demonstrated in a systematic review of 18 randomized controlled trials, which failed to show a significant decrease in the number of severe exacerbations.Citation136
Phosphodiesterase-4 inhibitors
Phosphodiesterase-4 inhibitors do not have direct bronchodilator activity, but act as anti-inflammatory agents by inhibiting the breakdown of intracellular cyclic nucleotides.Citation137 Roflumilast is an oral phosphodiesterase-4 inhibitor, indicated as a maintenance treatment for severe COPD associated with chronic bronchitis in adult patients with a history of frequent exacerbations (as add-on to bronchodilator treatment).Citation138 The 1-year REACT study showed that in symptomatic patients with severe COPD and a history of exacerbations, roflumilast significantly reduced the risk of severe exacerbations in those already receiving an ICS–LABA fixed combination, along with a LAMA (tiotropium in this study) as background treatment.Citation139 A pooled analysis of two randomized trials enrolling patients with similar disease characteristics (but where approximately 50% continued with LABA therapy, and ICSs were not permitted) demonstrated that roflumilast reduced the rate of moderate–severe exacerbations versus placebo, but had no significant impact on the rate of severe exacerbations.Citation140 A post hoc analysis of the 52-week RE2SPOND trial showed that roflumilast reduced the rate of severe exacerbations in patients with frequent exacerbations (more than three exacerbations in the previous year) and/or history of hospitalization.Citation141 The RE2SPONDCitation141 and REACTCitation139 studies were performed in patients with severe COPD, and evidence from these trials suggests that the benefits of roflumilast are demonstrated most consistently in patients with severe–very severe COPD associated with chronic bronchitis and a history of frequent exacerbations.Citation142 Concerns have been raised regarding the safety profile of roflumilast, due to higher incidences of adverse events compared to other COPD medications;Citation11 however, a benefit–harm analysis of the use of roflumilast found a net benefit in patients with a high risk of severe exacerbations.Citation143
Mucolytics
Mucolytic agents (specifically N-acetylcysteine [NAC]) may have a beneficial role in exacerbation reduction, with studies indicative of a reduction in exacerbation frequency.Citation144,Citation145 Although a Cochrane systematic review concluded that the small reduction in overall acute exacerbations achieved with mucolytics may have been overestimated,Citation146 some studies suggest that higher doses of mucolytics (NAC 600 mg twice daily) may be particularly effective in patients with stable COPD,Citation144 moderate–severe COPD,Citation147 or at high risk of exacerbations.Citation148 However, these studies were not specifically powered for the analysis of severe exacerbations. The current GOLD report concludes that regular use of mucolytic agents, such as NAC and carbocysteine, reduce the risk of exacerbation when used in appropriate patients.Citation11
Antibiotic prophylaxis
Several studies suggest that the use of certain types of antibiotics may have a role in preventing exacerbations in certain groups of patients for whom the benefits outweigh the risks. Macrolides, which possess both antibacterial and anti-inflammatory effects, and fluoroquinolones are the classes of antibiotics studied most extensively for use in stable COPD, and prophylactic use over 1 year can reduce the rate of hospitalizations for COPD exacerbations compared with placebo.Citation149–Citation153 While a meta-analysis of nine studies showed that macrolides are effective in reducing the overall rate of COPD exacerbations when administered for 6–12 months, the analysis was not able to demonstrate an effect on hospitalization rates, due to the low number of hospitalizations in the studies, which were not powered to detect such differences.Citation151 Prophylactic antibiotic therapy should be applied cautiously, as the evidence remains limited, and further studies will be required to determine the optimal treatment regimen and duration with prophylactic use of antibiotics, and in what patients, to maintain a positive benefit–risk balance.Citation150,Citation151,Citation154
Vitamin D
It has been suggested that vitamin D supplements may help to prevent COPD exacerbations. The ViDiCO study demonstrated that vitamin D3 supplementation reduced the risk of moderate and severe exacerbations in patients with COPD;Citation155 however, findings have been conflicting and the benefits may only be evident in patients with severe vitamin D deficiency.Citation156 The PRECOVID study will be the first randomized trial to evaluate the effects of vitamin D supplementation on exacerbation prevention (primary outcome; rates of hospitalization will be a secondary outcome), and will recruit vitamin D-deficient patients who have recently experienced an exacerbation.Citation157 The results of the study will be beneficial for establishing guidelines for vitamin D supplementation with regard to reducing exacerbation rates.
β-Blockers
β-blocker usage is low in patients with COPD and cardiovascular comorbidities, as blockade of β-adrenergic receptors might induce bronchoconstriction and lead to bronchospasm and worsening of lung function. This is based largely on anecdotal evidence; however, review of the evidence base has indicated that cardioselective β-blockers (ie, those with greater affinity for β1- over β2-receptors) reduce overall mortality in patients with such conditions as coronary artery disease or MI and coexisting mild–moderate COPD, without producing clinically significant adverse respiratory effects, and should not be withheld.Citation158–Citation160 One observational cohort study (COPDGene®), which followed approximately 3,500 patients for a median of 2.1 years, indicated that the use of β-blockers in COPD patients with cardiovascular comorbidities was associated with a significant reduction in exacerbation rates, including severe exacerbations. Effects were most pronounced in patients with severe COPD (GOLD grade 3 and 4 on home oxygen therapy).Citation161 Randomized trials may be warranted to confirm whether this observation represents beneficial effects of β-blockers in COPD and explore the mechanisms underlying potential protective effects.
Readmissions
Patients who have been admitted to hospital for a severe exacerbation of COPD are at substantial risk of rehospitalization.Citation18 In the EU COPD audit, 35% of all patients admitted to hospital with COPD exacerbations were readmitted within 90 days, and approximately three-quarters of readmissions were recorded as COPD-related.Citation10 Readmission is a poor outcome for patients, and presents a significant strain on resources. In some cases, readmission is the result of a poor discharge, while in others it reflects the severity of the underlying COPD or the presence of comorbidities.Citation162 Despite best efforts, many readmissions may not be preventable. The US National COPD Readmissions Summit, as well as a recent systematic review, found that the evidence base to support specific interventions that would significantly reduce 30-day readmission rates in patients hospitalized for COPD exacerbations was inadequate.Citation163,Citation164
Nevertheless, readmission rates are of increasing significance to payers in both the US and the UK, where financial penalties have been imposed on hospitals with higher-than-expected readmission rates, as part of an incentive to promote optimized, value-driven care packages for patients discharged following a COPD exacerbation. From a clinical perspective, it is important to monitor whether these approaches have unintended negative consequences, such as an increase in out-of-hospital mortality resulting from the disincentive to readmit patients who might genuinely benefit from further hospital treatment.Citation163
Since a substantial proportion of readmissions are not due to COPD itself, but relate to comorbidities, effective management of these conditions and COPD is important in attempts to reduce readmission rates.Citation56,Citation162 Ensuring patients are on optimal maintenance treatment known to reduce exacerbation rates (as discussed earlier) at the time of discharge is essential to reduce the risk of further exacerbations and readmission.
Improving overall disease-management strategies
Several studies have revealed the frequency of clinical practices that are nonadherent to treatment guidelines, showing a disparity in treatment choices, overuse of CSs and antibiotics, and underuse of pulmonary rehabilitation.Citation162–Citation167 In a study conducted in the US, review of medical records indicated that patients with COPD received only 58% of the care recommended by guidelines.Citation168 A survey of respiratory specialists in Canada identified important care gaps regarding interventions to prevent future exacerbations, eg, suboptimal vaccinations, care plans, and patient education (39% of patients had never been taught how to recognize the signs and symptoms of an exacerbation). In the Continuing to Confront COPD International Physician Survey (12 countries), only 57% of primary-care physicians and 58% of respiratory specialists provided treatment options concordant with the GOLD report for high-risk (GOLD grade 4) COPD.Citation165 The EU COPD audit showed that COPD treatment received before admission for COPD exacerbation, inpatient treatment, use of mechanical ventilation, and discharge medications (including oxygen) varied widely across Europe.Citation10 In addition, the organization of COPD care and hospital facilities was shown to vary considerably between countries.Citation10
Adherence to therapy is an important factor in successfully preventing exacerbations. Poor adherence to COPD medication detrimentally affects long-term disease outcomes.Citation169 Among inhaled bronchodilators prescribed as maintenance therapy for COPD, adherence varies according to the type of medication, with higher rates of adherence observed with LAMAs (tiotropium in the study quoted) and relatively low adherence to ICSs or ICS–LABA combinations.Citation170
Conclusion
Severe exacerbations are an important cause of morbidity and mortality, and have substantial economic consequences. A large number of potential risk factors are associated with severe exacerbations, many of which are easily identifiable and modifiable with careful patient management. Previous severe exacerbations and hospital readmission are significant risk factors for mortality; therefore, targeted interventions aimed at preventing or reducing severe exacerbations should be a priority for improving patients’ prognoses. Strategies to reduce hospital readmissions for COPD and related comorbidities are also required to reduce the economic burden associated with repeated hospitalizations.
Recent observational studies have reported lower rates of in-hospital mortality, reduced length of hospitalization, and fewer subsequent exacerbations over the past decade, reflecting improvements in care and greater awareness of the impact of COPD exacerbations. Nonetheless, effective prevention of severe exacerbations remains a significant unmet need in COPD. Both pharmacological and non-pharmacological interventions have a role as part of a holistic package to minimize exacerbation risk. Smoking cessation is a key intervention, and improved access to/uptake of pulmonary rehabilitation may be beneficial. Large randomized clinical trials have demonstrated the benefit of long-acting bronchodilators, such as LAMAs or LABAs, either as monotherapies or in combination, in reducing the risk of severe exacerbations in patients with COPD at all stages of severity. Overall, bronchodilators appear to be at least as effective as LABA–ICS therapy in preventing severe exacerbations of COPD. Antibiotics also have a role in selected patients, and influenza and pneumococcal vaccination can help prevent exacerbations. In conclusion, multiple opportunities to improve management of COPD and reduce risk of severe exacerbations are available, and should be considered in all patients with COPD, with particular attention paid to those who have already had a severe exacerbation.
Acknowledgments
Editorial and writing support was provided by Andree Rose, Jennifer Fuchs, and Deepti Sharda at PAREXEL, funded by Boehringer Ingelheim.
Disclosure
DMGH has received personal fees from Almirall, Boehringer Ingelheim, GlaxoSmithKline, Intermune, Pfizer and Novartis, and non-financial support from Boehringer Ingelheim and Novartis. MM has received speaker fees from Almirall, Boehringer Ingelheim, Pfizer, AstraZeneca, Chiesi, Esteve, GlaxoSmithKline, Menarini, Novartis, Talecris-Grifols, Takeda-Nycomed, and Novartis, and consulting fees from Almirall, Boehringer Ingelheim, Pfizer, GlaxoSmithKline, Gebro Pharma, MediImmune, Novartis, Talecris-Grifols and Takeda-Nycomed. NM is an employee of Boehringer Ingelheim. BC has received fees for consulting from AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, MedImmune and Novartis.
References
- DonaldsonGCWedzichaJACOPD exacerbations – 1: epidemiologyThorax200661216416816443707
- AnzuetoALeimerIKestenSImpact of frequency of COPD exacerbations on pulmonary function, health status and clinical outcomesInt J Chron Obstruct Pulmon Dis2009424525119657398
- EffingTWKerstjensHAMonninkhofEMDefinitions of exacerbations: does it really matter in clinical trials on COPD?Chest2009136391892319736196
- SuissaSDell’AnielloSErnstPLong-term natural history of chronic obstructive pulmonary disease: severe exacerbations and mortalityThorax2012671195796322684094
- EstebanCQuintanaJMMorazaJImpact of hospitalisations for exacerbations of COPD on health-related quality of lifeRespir Med200910381201120819272762
- MullerovaHMaselliDJLocantoreNHospitalized exacerbations of COPD: risk factors and outcomes in the ECLIPSE cohortChest20151474999100725356881
- ToyELGallagherKFStanleyELSwensenARDuhMSThe economic impact of exacerbations of chronic obstructive pulmonary disease and exacerbation definition: a reviewCOPD20107321422820486821
- MiravitllesMMurioCGuerreroTGisbertRPharmacoeconomic evaluation of acute exacerbations of chronic bronchitis and COPDChest200212151449145512006427
- LimaFVYenTYPatelJKTrends in in-hospital outcomes among adults hospitalized with exacerbation of chronic obstructive pulmonary diseaseCOPD201512263664226263035
- European Respiratory SocietyAn International Comparison of COPD Care in Europe: Results of the First European COPD AuditLausanne, SwitzerlandERS2012
- Global Initiative for Chronic Obstructive Lung DiseaseGlobal Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary DiseaseBethesda (MD)GOLD2017
- CelliBRMacneeWStandards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paperEur Respir J200423693294615219010
- National Institute for Health and Care ExcellenceChronic Obstructive Pulmonary Disease in Over 16s: Diagnosis and ManagementLondonNICE2010
- ZhongNMoonHSLeeKHTiotropium safety and performance in Respimat (TIOSPIR): analysis of Asian cohort of COPD patientsRespirology20162181397140327490162
- ChennaPRManninoDMOutcomes of severe COPD exacerbations requiring hospitalizationSemin Respir Crit Care Med201031328629420496298
- HalpinDMDecramerMCelliBKestenSLiuDTashkinDPExacerbation frequency and course of COPDInt J Chron Obstruct Pulmon Dis2012765366123055714
- CoteCGDordellyLJCelliBRImpact of COPD exacerbations on patient-centered outcomesChest2007131369670417356082
- Soler-CatalunaJJMartinez-GarciaMARomanSPSalcedoENavarroMOchandoRSevere acute exacerbations and mortality in patients with chronic obstructive pulmonary diseaseThorax2005601192593116055622
- McGhanRRadcliffTFishRSutherlandERWelshCMakeBPredictors of rehospitalization and death after a severe exacerbation of COPDChest200713261748175517890477
- GroenewegenKHScholsAMWoutersEFMortality and mortality-related factors after hospitalization for acute exacerbation of COPDChest2003124245946712907529
- GunenHHacievliyagilSSKosarFFactors affecting survival of hospitalised patients with COPDEur Respir J200526223424116055870
- PiquetJChavaillonJMDavidPMartinFBlanchonFRocheNHigh-risk patients following hospitalisation for an acute exacerbation of COPDEur Respir J201342494695523349446
- AlmagroPSalvadoMGarcia-VidalCRecent improvement in long-term survival after a COPD hospitalisationThorax201065429830220388752
- HalpinDMortality in COPD: inevitable or preventable? Insights from the cardiovascular arenaCOPD20085318720018568843
- PavordIDJonesPWBurgelPRRabeKFExacerbations of COPDInt J Chron Obstruct Pulmon Dis201611Spec Iss213026937187
- FanVSCurtisJRTuSPMcDonellMBFihnSDUsing quality of life to predict hospitalization and mortality in patients with obstructive lung diseasesChest2002122242943612171813
- MolinariNBriandCVachierIHospitalizations for COPD exacerbations: trends and determinants of deathCOPD201512662162726263032
- SteerJGibsonGJBourkeSCPredicting outcomes following hospitalization for acute exacerbations of COPDQJM20101031181782920660633
- MiravitllesMFerrerMPontAEffect of exacerbations on quality of life in patients with chronic obstructive pulmonary disease: a 2 year follow up studyThorax200459538739515115864
- SolemCTSunSXSudharshanLMacahiligCKatyalMGaoXExacerbation-related impairment of quality of life and work productivity in severe and very severe chronic obstructive pulmonary diseaseInt J Chron Obstruct Pulmon Dis2013864165224376348
- NiewoehnerDEThe impact of severe exacerbations on quality of life and the clinical course of chronic obstructive pulmonary diseaseAm J Med200611910 Suppl 1384516996898
- VerhageTBoerLMolemaJHeijdraYDekhuijzenRVercoulenJHDecline of health status sub-domains by exacerbations of chronic obstructive pulmonary disease: a prospective surveyRespiration201385323624322922171
- MacDonaldMIShafuddinEKingPTChangCLBardinPGHancoxRJCardiac dysfunction during exacerbations of chronic obstructive pulmonary diseaseLancet Respir Med20164213814826781000
- McAllisterDAMaclayJDMillsNLDiagnosis of myocardial infarction following hospitalisation for exacerbation of COPDEur Respir J20123951097110322323574
- PatelARKowlessarBSDonaldsonGCCardiovascular risk, myocardial injury, and exacerbations of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med201318891091109924033321
- HalpinDMDecramerMCelliBKestenSLeimerITashkinDPRisk of nonlower respiratory serious adverse events following COPD exacerbations in the 4-year UPLIFT trialLung2011189426126821678045
- ChangCLRobinsonSCMillsGDBiochemical markers of cardiac dysfunction predict mortality in acute exacerbations of COPDThorax201166976476821474497
- DonaldsonGCHurstJRSmithCJHubbardRBWedzichaJAIncreased risk of myocardial infarction and stroke following exacerbation of COPDChest201013751091109720022970
- WangFChengZZWangJLHanWZSunNNIncidence of pulmonary embolism in patients with acute exacerbations of chronic obstructive pulmonary disease: a meta-analysisZhonghua Yi Xue Za Zhi2013932418681871 Chinese24124736
- RizkallahJManSFSinDDPrevalence of pulmonary embolism in acute exacerbations of COPD: a systematic review and metaanalysisChest2009135378679318812453
- LandisSHMuellerovaHManninoDMContinuing to Confront COPD International Patient Survey: methods, COPD prevalence, and disease burden in 2012–2013Int J Chron Obstruct Pulmon Dis2014959761124944511
- MiravitllesMAnzuetoALegnaniDForstmeierLFargelMPatient’s perception of exacerbations of COPD: the PERCEIVE studyRespir Med2007101345346016938447
- DonaldsonGCSeemungalTAPatelISLloyd-OwenSJWilkinsonTMWedzichaJALongitudinal changes in the nature, severity and frequency of COPD exacerbationsEur Respir J200322693193614680081
- CazzolaMMacneeWMartinezFJOutcomes for COPD pharmacological trials: from lung function to biomarkersEur Respir J200831241646918238951
- SullivanSDStrasselsSASmithDHCharacterization of the costs of chronic obstructive pulmonary disease (COPD) in the USEur Respir J20169Suppl 23412S
- PereraPNArmstrongEPSherrillDLSkrepnekGHAcute exacerbations of COPD in the United States: inpatient burden and predictors of costs and mortalityCOPD20129213114122409371
- National Health Service EnglandOverview of potential to reduce lives lost from chronic obstructive pulmonary disease (COPD)2014 Available from: https://www.england.nhs.uk/wp-content/uploads/2014/02/rm-fs-6.pdfAccessed March 11, 2016
- FordESHospital discharges, readmissions, and ED visits for COPD or bronchiectasis among US adults: findings from the nationwide inpatient sample 2001–2012 and Nationwide Emergency Department Sample 2006–2011Chest2015147498999825375955
- CelliBRBarnesPJExacerbations of chronic obstructive pulmonary diseaseEur Respir J20072961224123817540785
- MiravitllesMGuerreroTMayordomoCSanchez-AgudoLNicolauFSeguJLFactors associated with increased risk of exacerbation and hospital admission in a cohort of ambulatory COPD patients: a multiple logistic regression analysisRespiration200067549550111070451
- Garcia-AymerichJGomezFPBenetMIdentification and prospective validation of clinically relevant chronic obstructive pulmonary disease (COPD) subtypesThorax201166543043721177668
- Garcia-AymerichJMonsoEMarradesRMRisk factors for hospitalization for a chronic obstructive pulmonary disease exacerbation: EFRAM studyAm J Respir Crit Care Med200116461002100711587986
- Garcia-AymerichJFarreroEFelezMAIzquierdoJMarradesRMAntoJMRisk factors of readmission to hospital for a COPD exacerbation: a prospective studyThorax200358210010512554887
- Garcia-PoloCAlcazar-NavarreteBRuiz-IturriagaLAFactors associated with high healthcare resource utilisation among COPD patientsRespir Med2012106121734174223058483
- AlcazarBGarcia-PoloCHerrejonAFactors associated with hospital admission for exacerbation of chronic obstructive pulmonary diseaseArch Bronconeumol2012483707622196478
- BahadoriKFitzGeraldJMRisk factors of hospitalization and readmission of patients with COPD exacerbation: systematic reviewInt J Chron Obstruct Pulmon Dis20072324125118229562
- BarnesNCalverleyPMKaplanARabeKFChronic obstructive pulmonary disease and exacerbations: patient insights from the global Hidden Depths of COPD surveyBMC Pulm Med2013135423971625
- BensonVSMüllerováHVestboJWedzichaJAPatelAHurstJRAssociations between gastro-oesophageal reflux, its management and exacerbations of chronic obstructive pulmonary diseaseRespir Med201510991147115426166017
- CaoZOngKCEngPTanWCNgTPFrequent hospital readmissions for acute exacerbation of COPD and their associated factorsRespirology200611218819516548905
- EisnerMDBlancPDOmachiTASocioeconomic status, race and COPD health outcomesJ Epidemiol Community Health2011651263419854747
- FaganelloMMTanniSESanchezFFPelegrinoNRLuchetaPAGodoyIBODE index and GOLD staging as predictors of 1-year exacerbation risk in chronic obstructive pulmonary diseaseAm J Med Sci20103391101419926966
- GadouryMASchwartzmanKRouleauMSelf-management reduces both short- and long-term hospitalisation in COPDEur Respir J200526585385716264046
- GodtfredsenNSVestboJOslerMPrescottERisk of hospital admission for COPD following smoking cessation and reduction: a Danish population studyThorax2002571196797212403880
- GudmundssonGGislasonTJansonCRisk factors for rehospitalisation in COPD: role of health status, anxiety and depressionEur Respir J200526341441916135721
- HoogendoornMFeenstraTLHoogenveenRTAlMMölkenMRAssociation between lung function and exacerbation frequency in patients with COPDInt J Chron Obstruct Pulmon Dis2010543544421191438
- HurstJRVestboJAnzuetoASusceptibility to exacerbation in chronic obstructive pulmonary diseaseN Engl J Med2010363121128113820843247
- KesslerRFallerMFourgautGMennecierBWeitzenblumEPredictive factors of hospitalization for acute exacerbation in a series of 64 patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med199915911581649872834
- KimJLeeJHKimYAssociation between chronic obstructive pulmonary disease and gastroesophageal reflux disease: a national cross-sectional cohort studyBMC Pulm Med2013135123927016
- LauACYamLYPoonEHospital re-admission in patients with acute exacerbation of chronic obstructive pulmonary diseaseRespir Med2001951187688411716201
- NiewoehnerDELokhnyginaYRiceKRisk indexes for exacerbations and hospitalizations due to COPDChest20071311202817218552
- OmachiTASarkarUYelinEHBlancPDKatzPPLower health literacy is associated with poorer health status and outcomes in chronic obstructive pulmonary diseaseJ Gen Intern Med2013281748122890622
- PouwEMTen VeldeGPCroonenBHKesterADScholsAMWoutersEFEarly non-elective readmission for chronic obstructive pulmonary disease is associated with weight lossClin Nutr2000192959910867726
- QureshiHSharafkhanehAHananiaNAChronic obstructive pulmonary disease exacerbations: latest evidence and clinical implicationsTher Adv Chronic Dis20145521222725177479
- RobertsCMLoweDBucknallCERylandIKellyYPearsonMGClinical audit indicators of outcome following admission to hospital with acute exacerbation of chronic obstructive pulmonary diseaseThorax200257213714111828043
- WedzichaJABrillSEAllinsonJPDonaldsonGCMechanisms and impact of the frequent exacerbator phenotype in chronic obstructive pulmonary diseaseBMC Med20131118123945277
- WongAWGanWQBurnsJSinDDvan EedenSFAcute exacerbation of chronic obstructive pulmonary disease: influence of social factors in determining length of hospital stay and readmission ratesCan Respir J200815736136418949105
- MiravitllesMCalleMAlvarez-GutierrezFGobarttELopezFMartinAExacerbations, hospital admissions and impaired health status in chronic obstructive pulmonary diseaseQual Life Res200615347148016547786
- MiravitllesMGarcia-SidroPFernandez-NistalAThe chronic obstructive pulmonary disease assessment test improves the predictive value of previous exacerbations for poor outcomes in COPDInt J Chron Obstruct Pulmon Dis2015102571257926664105
- BeasleyVJoshiPVSinganayagamAMolyneauxPLJohnstonSLMalliaPLung microbiology and exacerbations in COPDInt J Chron Obstruct Pulmon Dis2012755556922969296
- GallegoMPomaresXEspasaMPseudomonas aeruginosa isolates in severe chronic obstructive pulmonary disease: characterization and risk factorsBMC Pulm Med20141410324964956
- CortiCFallyMFabricius-BjerreAPoint-of-care procalcitonin test to reduce antibiotic exposure in patients hospitalized with acute exacerbation of COPDInt J Chron Obstruct Pulmon Dis2016111381138927382274
- SchuetzPMüllerBChrist-CrainMProcalcitonin to initiate or discontinue antibiotics in acute respiratory tract infectionsCochrane Database Syst Rev20129CD00749822972110
- BoersmaWGAntibiotics in acute exacerbations of COPD: the good, the bad and the uglyEur Respir J20124011322753830
- WaltersJATanDJWhiteCJGibsonPGWood-BakerRWaltersEHSystemic corticosteroids for acute exacerbations of chronic obstructive pulmonary diseaseCochrane Database Syst Rev20149CD00128825178099
- KiserTHAllenRRValuckRJMossMVandivierRWOutcomes associated with corticosteroid dosage in critically ill patients with acute exacerbations of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med201418991052106424617842
- WedzichaJAMiravitllesMHurstJRManagement of COPD exacerbations: a European Respiratory Society/American Thoracic Society guidelineEur Respir J2017493160079128298398
- WaltersJATanDJWhiteCJWood-BakerRDifferent durations of corticosteroid therapy for exacerbations of chronic obstructive pulmonary diseaseCochrane Database Syst Rev201412CD00689725491891
- BrillSEWedzichaJAOxygen therapy in acute exacerbations of chronic obstructive pulmonary diseaseInt J Chron Obstruct Pulmon Dis201491241125225404854
- QuintanaJMEstebanCUnzurrunzagaAPredictive score for mortality in patients with COPD exacerbations attending hospital emergency departmentsBMC Med2014126624758312
- PlantPKOwenJLElliottMWOne year period prevalence study of respiratory acidosis in acute exacerbations of COPD: implications for the provision of non-invasive ventilation and oxygen administrationThorax200055755055410856313
- AustinMAWillsKEBlizzardLWaltersEHWood-BakerREffect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in prehospital setting: randomised controlled trialBMJ2010341c546220959284
- WijesingheMPerrinKHealyBPre-hospital oxygen therapy in acute exacerbations of chronic obstructive pulmonary diseaseIntern Med J201141861862220214690
- ParkerCMVoducNAaronSDWebbKAO’DonnellDEPhysiological changes during symptom recovery from moderate exacerbations of COPDEur Respir J200526342042816135722
- Pinto-PlataVMLivnatGGirishMSystemic cytokines, clinical and physiological changes in patients hospitalized for exacerbation of COPDChest20071311374317218554
- StevensonNJWalkerPPCostelloRWCalverleyPMLung mechanics and dyspnea during exacerbations of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2005172121510151616166620
- LightowlerJVWedzichaJAElliottMWRamFSNon-invasive positive pressure ventilation to treat respiratory failure resulting from exacerbations of chronic obstructive pulmonary disease: Cochrane systematic review and meta-analysisBMJ2003326738218512543832
- KoBSAhnSLimKSKimWYLeeYSLeeJHEarly failure of noninvasive ventilation in chronic obstructive pulmonary disease with acute hypercapnic respiratory failureIntern Emerg Med201510785586026341216
- ContouDFragnoliCCordoba-IzquierdoABoissierFBrun-BuissonCThilleAWNoninvasive ventilation for acute hypercapnic respiratory failure: intubation rate in an experienced unitRespir Care201358122045205223737546
- PhuaJKongKLeeKHShenLLimTKNoninvasive ventilation in hypercapnic acute respiratory failure due to chronic obstructive pulmonary disease vs. other conditions: effectiveness and predictors of failureIntensive Care Med200531453353915742175
- AuDHBrysonCLChienJWThe effects of smoking cessation on the risk of chronic obstructive pulmonary disease exacerbationsJ Gen Intern Med200924445746319194768
- DecramerMNiciLNardiniSTargeting the COPD exacerbationRespir Med2008102Suppl 1S3S1518582795
- Montserrat-CapdevilaJGodoyPMarsalJRCruzISolanesMEffectiveness of influenza vaccination in preventing hospital admission due to exacerbations of chronic obstructive pulmonary diseaseEnferm Infecc Microbiol Clin20143227075 Spanish23582192
- FurumotoAOhkusaYChenMAdditive effect of pneumococcal vaccine and influenza vaccine on acute exacerbation in patients with chronic lung diseaseVaccine200826334284428918585831
- MaddocksMKonSSSinghSJManWDRehabilitation following hospitalization in patients with COPD: can it reduce readmissions?Respirology201520339540425529496
- PuhanMAScharplatzMTroostersTSteurerJRespiratory rehabilitation after acute exacerbation of COPD may reduce risk for readmission and mortality: a systematic reviewRespir Res200565415943867
- PuhanMAGimeno-SantosEScharplatzMTroostersTWaltersEHSteurerJPulmonary rehabilitation following exacerbations of chronic obstructive pulmonary diseaseCochrane Database Syst Rev201110CD00530521975749
- CrinerGJBourbeauJDiekemperRLPrevention of acute exacerbations of COPD: American College of Chest Physicians and Canadian Thoracic Society guidelineChest2015147489494225321320
- BourbeauJJulienMMaltaisFReduction of hospital utilization in patients with chronic obstructive pulmonary disease: a disease-specific self-management interventionArch Intern Med2003163558559112622605
- RiceKLDewanNBloomfieldHEDisease management program for chronic obstructive pulmonary disease: a randomized controlled trialAm J Respir Crit Care Med2010182789089620075385
- FanVSGazianoJMLewRA comprehensive care management program to prevent chronic obstructive pulmonary disease hospitalizations: a randomized, controlled trialAnn Intern Med20121561067368322586006
- ZwerinkMBrusse-KeizerMvan der ValkPDSelf management for patients with chronic obstructive pulmonary diseaseCochrane Database Syst Rev20143CD00299024665053
- AaronSDManagement and prevention of exacerbations of COPDBMJ2014349g523725245156
- HalpinDMVogelmeierCPieperMPMetzdorfNRichardFAnzuetoAEffect of tiotropium on COPD exacerbations: a systematic reviewRespir Med20161141827109805
- BatemanEDTashkinDSiafakasNA one-year trial of tiotropium Respimat plus usual therapy in COPD patientsRespir Med2010104101460147220620037
- BatemanESinghDSmithDEfficacy and safety of tiotropium Respimat SMI in COPD in two 1-year randomized studiesInt J Chron Obstruct Pulmon Dis2010519720820714373
- CasaburiRMahlerDAJonesPWA long-term evaluation of once-daily inhaled tiotropium in chronic obstructive pulmonary diseaseEur Respir J200219221722411866001
- ChanCKMaltaisFSigouinCHaddonJMFordGTA randomized controlled trial to assess the efficacy of tiotropium in Canadian patients with chronic obstructive pulmonary diseaseCan Respir J200714846547218060091
- NiewoehnerDERiceKCoteCPrevention of exacerbations of chronic obstructive pulmonary disease with tiotropium, a once-daily inhaled anticholinergic bronchodilatorAnn Intern Med2005143531732616144890
- TashkinDPCelliBSennSA 4-Year trial of tiotropium in chronic obstructive pulmonary diseaseN Engl J Med2008359151543155418836213
- D’UrzoAFergusonGTvan NoordJAEfficacy and safety of once-daily NVA237 in patients with moderate-to-severe COPD: the GLOW1 trialRespir Res2011712156
- BrusascoVHodderRMiravitllesMKorduckiLTowseLKestenSHealth outcomes following treatment for six months with once daily tiotropium compared with twice daily salmeterol in patients with COPDThorax200358539940412728159
- DecramerMChapmanKRDahlROnce-daily indacaterol versus tiotropium for patients with severe chronic obstructive pulmonary disease (INVIGORATE): a randomised, blinded, parallel-group studyLancet Respir Med20131752453324461613
- VogelmeierCHedererBGlaabTTiotropium versus salmeterol for the prevention of exacerbations of COPDN Engl J Med2011364121093110321428765
- WiseRAAnzuetoACottonDTiotropium Respimat inhaler and the risk of death in COPDN Engl J Med2013369161491150123992515
- DohertyDETashkinDPKerwinEEffects of mometasone furoate/formoterol fumarate fixed-dose combination formulation on chronic obstructive pulmonary disease (COPD): results from a 52-week phase III trial in subjects with moderate-to-very severe COPDInt J Chron Obstruct Pulmon Dis20127577122334769
- DonohueJFNiewoehnerDBrooksJO’DellDChurchASafety and tolerability of once-daily umeclidinium/vilanterol 125/25 mcg and umeclidinium 125 mcg in patients with chronic obstructive pulmonary disease: results from a 52-week, randomized, double-blind, placebo-controlled studyRespir Res2014157825015176
- WedzichaJACalverleyPMSeemungalTAHaganGAnsariZStockleyRAThe prevention of chronic obstructive pulmonary disease exacerbations by salmeterol/fluticasone propionate or tiotropium bromideAm J Respir Crit Care Med20081771192617916806
- DransfieldMTBourbeauJJonesPWOnce-daily inhaled fluticasone furoate and vilanterol versus vilanterol only for prevention of exacerbations of COPD: two replicate double-blind, parallel-group, randomised controlled trialsLancet Respir Med20131321022324429127
- SharafkhanehASouthardJGGoldmanMUryniakTMartinUJEffect of budesonide/formoterol pMDI on COPD exacerbations: a double-blind, randomized studyRespir Med2012106225726822033040
- WedzichaJADecramerMFickerJHAnalysis of chronic obstructive pulmonary disease exacerbations with the dual bronchodilator QVA149 compared with glycopyrronium and tiotropium (SPARK): a randomised, double-blind, parallel-group studyLancet Respir Med20131319920924429126
- TashkinDPDohertyDEKerwinEEfficacy and safety characteristics of mometasone furoate/formoterol fumarate fixed-dose combination in subjects with moderate to very severe COPD: findings from pooled analysis of two randomized, 52-week placebo-controlled trialsInt J Chron Obstruct Pulmon Dis20127738622334770
- CalverleyPMAndersonJACelliBSalmeterol and fluticasone propionate and survival in chronic obstructive pulmonary diseaseN Engl J Med2007356877578917314337
- WedzichaJABanerjiDChapmanKRIndacaterol-glycopyrronium versus salmeterol-fluticasone for COPDN Engl J Med2016374232222223427181606
- BuhlRGessnerCSchuermannWEfficacy and safety of once-daily QVA149 compared with the free combination of once-daily tiotropium plus twice-daily formoterol in patients with moderate-to-severe COPD (QUANTIFY): a randomised, non-inferiority studyThorax201570431131925677679
- ManninoDMYuTCZhouHHiguchiKEffects of GOLD-adherent prescribing on COPD symptom burden, exacerbations, and health care utilization in a real-world settingChronic Obstr Pulm Dis20152322323528848845
- RodrigoGJCastro-RodriguezJAPlazaVSafety and efficacy of combined long-acting β-agonists and inhaled corticosteroids vs long-acting β-agonists monotherapy for stable COPD: a systematic reviewChest200913641029103819633090
- RabeKFUpdate on roflumilast, a phosphodiesterase 4 inhibitor for the treatment of chronic obstructive pulmonary diseaseBr J Pharmacol20111631536721232047
- Roflumilast [summary of product characteristics]Luton, UKAstraZeneca UK
- MartinezFJCalverleyPMGoehringUMBroseMFabbritLMRabeKFEffect of roflumilast on exacerbations in patients with severe chronic obstructive pulmonary disease uncontrolled by combination therapy (REACT): a multicentre randomised controlled trialLancet2015385997185786625684586
- CalverleyPMRabeKFGoehringUMKristiansenSFabbriLMMartinezFJRoflumilast in symptomatic chronic obstructive pulmonary disease: two randomised clinical trialsLancet2009374969168569419716960
- MartinezFJRabeKFSethiSEffect of roflumilast and inhaled corticosteroid/long-acting β2-agonist on chronic obstructive pulmonary disease exacerbations (RE2SPOND): a randomized clinical trialAm J Respir Crit Care Med2016194555956727585384
- WedzichaJACalverleyPMRabeKFRoflumilast: a review of its use in the treatment of COPDInt J Chron Obstruct Pulmon Dis201611819026792988
- YuTFainKBoydCMBenefits and harms of roflumilast in moderate to severe COPDThorax201469761662224347460
- TseHNRaiteriLWongKYHigh-dose N-acetylcysteine in stable COPD: the 1-year, double-blind, randomized, placebo-controlled HIACE studyChest2013144110611823348146
- PelaRCalcagniAMSubiacoSIsidoriPTubaldiASanguinettiCMN-acetylcysteine reduces the exacerbation rate in patients with moderate to severe COPDRespiration199966649550010575333
- PoolePBlackPNCatesCJMucolytic agents for chronic bronchitis or chronic obstructive pulmonary diseaseCochrane Database Syst Rev20128CD00128722895919
- ZhengJPWenFQBaiCXTwice daily N-acetylcysteine 600 mg for exacerbations of chronic obstructive pulmonary disease (PANTHEON): a randomised, double-blind placebo-controlled trialLancet Respir Med20142318719424621680
- TseHNRaiteriLWongKYNgLYYeeKSTsengCZBenefits of high-dose N-acetylcysteine to exacerbation-prone patients with COPDChest2014146361162324833327
- AlbertRKConnettJBaileyWCAzithromycin for prevention of exacerbations of COPDN Engl J Med2011365868969821864166
- HerathSCPoolePProphylactic antibiotic therapy for chronic obstructive pulmonary disease (COPD)Cochrane Database Syst Rev201311CD009764
- NiWShaoXCaiXProphylactic use of macrolide antibiotics for the prevention of chronic obstructive pulmonary disease exacerbation: a meta-analysisPLoS One2015103e012125725812085
- PomaresXMontonCEspasaMCasabonJMonsoEGallegoMLong-term azithromycin therapy in patients with severe COPD and repeated exacerbationsInt J Chron Obstruct Pulmon Dis2011644945622003290
- SeemungalTAWilkinsonTMHurstJRPereraWRSapsfordRJWedzichaJALong-term erythromycin therapy is associated with decreased chronic obstructive pulmonary disease exacerbationsAm J Respir Crit Care Med2008178111139114718723437
- MiravitllesMAnzuetoAAntibiotic prophylaxis in COPD: why, when, and for whom?Pulm Pharmacol Ther20153211912324825753
- MartineauARJamesWYHooperRLVitamin D3 supplementation in patients with chronic obstructive pulmonary disease (ViDiCO): a multicentre, double-blind, randomised controlled trialLancet Respir Med20153212013025476069
- LehouckAMathieuCCarremansCHigh doses of vitamin D to reduce exacerbations in chronic obstructive pulmonary disease: a randomized trialAnn Intern Med2012156210511422250141
- RafiqRAlevaFESchrumpfJAPrevention of exacerbations in patients with COPD and vitamin D deficiency through vitamin D supplementation (PRECOVID): a study protocolBMC Pulm Med20151510626399451
- AlbouainiKAndronMAlahmarAEgredMβ-Blockers use in patients with chronic obstructive pulmonary disease and concomitant cardiovascular conditionsInt J Chron Obstruct Pulmon Dis20072453554018268926
- AndellPErlingeDSmithJGβ-Blocker use and mortality in COPD patients after myocardial infarction: a Swedish nationwide observational studyJ Am Heart Assoc201544113
- SalpeterSROrmistonTMSalpeterEECardioselective β-blockers in patients with reactive airway disease: a meta-analysisAnn Intern Med2002137971572512416945
- BhattSPWellsJMKinneyGLβ-Blockers are associated with a reduction in COPD exacerbationsThorax201671181426283710
- ShahTChurpekMMCocaPMKonetzkaRTUnderstanding why patients with COPD get readmitted: a large national study to delineate the Medicare population for the readmissions penalty expansionChest201514751219122625539483
- KrishnanJAGussinHAPrieto-CenturionVSullivanJLZaidiFThomashowBMIntegrating COPD into patient-centered hospital readmissions reduction programsChronic Obstr Pulm Dis201521708025927076
- Prieto-CenturionVMarkosMARameyNIInterventions to reduce rehospitalizations after chronic obstructive pulmonary disease exacerbations: a systematic reviewAnn Am Thorac Soc201411341742424423379
- DavisKJLandisSHOhYMContinuing to Confront COPD International Physician Survey: physician knowledge and application of COPD management guidelines in 12 countriesInt J Chron Obstruct Pulmon Dis201510395525565799
- GlaabTBanikNRutschmannOTWenckerMNational survey of guideline-compliant COPD management among pneumologists and primary care physiciansCOPD20063314114817240616
- Lopez-CamposJLHartlSPozo-RodriguezFRobertsCMAntibiotic prescription for COPD exacerbations admitted to hospital: European COPD auditPLoS One2015104e012437425905726
- MularskiRAAschSMShrankWHThe quality of obstructive lung disease care for adults in the United States as measured by adherence to recommended processesChest200613061844185017167007
- MäkeläMJBackerVHedegaardMLarssonKAdherence to inhaled therapies, health outcomes and costs in patients with asthma and COPDRespir Med2013107101481149023643487
- Koehorst-ter HuurneKMovigKvan der ValkPvan der PalenJBrusse-KeizerMDifferences in adherence to common inhaled medications in COPDCOPD201512664364825775100
