Abstract
Background
COPD has significant psychosocial impact. Self-management support improves quality of life, but programs are not universally available. IT-based self-management interventions can provide home-based support, but have mixed results. We conducted a case series of an off-the-shelf Internet-based health-promotion program, The Preventive Plan (TPP), coupled with nurse-coach support, which aimed to increase patient activation and provide self-management benefits.
Materials and methods
A total of 19 COPD patients were recruited, and 14 completed 3-month follow-up in two groups: groups 1 and 2 with more and less advanced COPD, respectively. Change in patient activation was determined with paired t-tests and Wilcoxon signed-rank tests. Benefits and user experience were explored in semistructured interviews, analyzed thematically.
Results
Only group 1 improved significantly in activation, from a lower baseline than group 2; group 1 also improved significantly in mastery and anxiety. Both groups felt significantly more informed about COPD and reported physical functioning improvements. Group 1 reported improvements in mood and confidence. Overall, group 2 reported fewer benefits than group 1. Both groups valued nurse-coach support; for group 1, it was more important than TPP in building confidence to self-manage. The design of TPP and lack of motivation to use IT were barriers to use, but disease severity and poor IT skills were not.
Discussion
Our findings demonstrate the feasibility of combining nurse-coach support aligned to an Internet-based health resource, TPP, in COPD and provide learning about the challenges of such an approach and the importance of the nurse-coach role.
Plain-language summary
An important part of managing COPD is self-management by the patient. With IT-based self-management programs, patients can do this from their own home, which is easier for them and more cost-effective for the health care provider. Our goal was to explore how a generic Internet-based health-promotion program, The Preventive Plan (TPP), containing programs to support behavior change and health information, combined with support from a specialist nurse, could help patients to manage their COPD. We collected data from and interviewed 19 patients. We found that TPP and nurse support improved patient activation (the belief that one has a role in self-managing care and possession of knowledge and skills to do so), physical function, mood and confidence, and reduced patients’ information needs. Patients with more severe COPD gained the most benefit. Support from the nurse was considered to be more important than the Internet-based program by those with more severe COPD, and lack of motivation to use IT was a barrier to use, but poor IT skills and disease severity were not. Our findings demonstrate that a low-intensity intervention can produce meaningful benefits, and provides learning about the challenges of this approach and the importance of the nurse coach role.
Introduction
COPD is a progressive lung disease causing breathlessness, cough, fatigue, reduced exercise capacity, and frequent infections, with high societal burden.Citation1 Medication optimizes airway function and reduces symptoms, but cannot address the psychosocial impact of the disease, including anxiety and depression,Citation2 social isolation, and loss of independence and self-esteem.Citation3
Self-management support interventions in COPD have been shown to improve health-related quality of life,Citation4,Citation5 exercise capacity,Citation5 and self-efficacyCitation5 and reduce COPD-related hospital admissions.Citation4 However, for those unable or unwilling to attend group classes, IT-based approaches can provide support.Citation6–Citation11 IT-based self-management and lifestyle-change interventions for COPD have reported improved health-related quality of life,Citation9,Citation12–Citation16 physical activity,Citation13,Citation14,Citation17 exercise capacity,Citation12,Citation16 and functional capacityCitation18,Citation19 and reduced number and duration of hospital admissions.Citation9,Citation18,Citation20–Citation23 Participants have shown improved knowledge and awareness of their symptoms and health status,Citation19,Citation24 and qualitative analyses indicate positive effects on self-management, psychological condition, and coping ability.Citation18,Citation25 However, other studies have failed to detect positive changes in quality of life,Citation7,Citation17,Citation22 smoking cessation,Citation6 physical activity,Citation6,Citation7,Citation11 or dyspnea,Citation6,Citation7,Citation11,Citation14 and results for self-efficacy are mixed,Citation7,Citation17,Citation25 which may reflect heterogeneity among interventions: some were complemented with nurse or allied health-professional support,Citation7,Citation8,Citation15–Citation18,Citation20,Citation22 while others offered a stand-alone technological platform.Citation6,Citation12–Citation14,Citation21,Citation24,Citation26
Patient activation is the belief that one has a role in self-managing care and the possession of knowledge and skills to manage one’s condition, maintain functioning, collaborate with health care providers, and access appropriate care.Citation27 Activation impacts on health behavior, clinical outcomes, health care costs, and patient experiences.Citation28 However, little is known about the impact of IT-based interventions on patient activation in COPD.
Using a case-series design, we explored the feasibility of an off-the-shelf Internet-based health-promotion program, the Preventive Plan (TPP), coupled with nurse-coach support for home-based self-management of COPD with a focus on patient activation. We also aimed to identify patient-reported self-management benefits and factors influencing self-management goal achievement, and to generate generic learning to benefit users of ehealth interventions.
Materials and methods
Participants
Patients were recruited between May 2012 and January 2013. Inclusion criteria at the outset were: COPD diagnosis (forced expiratory volume in 1 second [FEV1]/forced vital capacity [FVC] <0.7), FEV1 <50% predicted (GOLD stage 3 and 4), two or more COPD exacerbation-related hospital admissions within the last year, had not attended pulmonary rehabilitation within the last year, and age >18 years. Exclusion criteria were diagnosis of lung cancer within the last year and being under the care of a psychologist for management of anxiety/depression. Eleven patients fulfilling these criteria were recruited (group 1). It was challenging to engage patients who met these criteria, and so to increase the number of participants, we adjusted the inclusion criteria for a second group (group 2) to include: FEV1 <80% predicted (GOLD stage 2–4) and troubled by breathlessness. We imposed no restriction on the number of exacerbation-related hospital admissions for this group. This enabled us to recruit a further eight patients.
Design
This case series employed mixed methods of quantitative outcome assessment and qualitative interviews. The intervention comprised an off-the-shelf Internet-based program, TPP, and nurse-coach support. TPP encompassed primary prevention, secondary prevention, and chronic-condition management. It was a generic tool personalized by uploading personal details, completing a health-risk assessment, and generation of a personalized prevention plan. Users accessed health-information resources and action programs to support behavior change. There was a messaging facility for email contact with the nurse. TPP could be accessed ad libitum by participants. The nurse coach (same for all participants) was a respiratory nurse specialist. She was trained to use TPP by the application developers and received training from a clinical communication skills specialist to use a coproduction consultation model to support self-management.Citation29 Through home visits, telephone, and email she provided self-management support, disease education, assisted participants to use TPP and IT hardware, and “signposted” complementary self-management and COPD-specific resources (Supplementary material). For group 2, she added further disease-specific content through weekly emails of material that replicated the educational content of pulmonary rehabilitation. This addition was made in the context of a pragmatic exploration of how the online platform could be built on for the benefit of patients. We provided laptop computers and Internet connectivity for patients with no existing access. No changes were made to participants’ usual care.
Data collection
Baseline measures, including spirometry, were collected by the nurse. Outcomes were measured at 3-month follow-up. Patient activation for self-management was assessed by the Patient Activation Measure.Citation30 Scores of 0–100 represent four activation levels:
level 1 (<47) – disengaged, overwhelmed, and may not believe patient role is important
level 2 (47.1–55.1) – becoming aware, but lacks confidence and knowledge
level 3 (55.2–67) – beginning to take action
level 4 (>67.1) – making changes, but may have difficulty maintaining behaviors over time.
We also assessed patient health-related quality of life using the Chronic Respiratory Questionnaire (CRQ),Citation31 anxiety and depression using the Hospital Anxiety and Depression Scale (HADS),Citation32 and information needs using the Lung Information Needs Questionnaire (LINQ).Citation33
All participants were interviewed by KH at 1 month after baseline to explore interim progress and at 3-month follow-up. Semistructured interviews explored participants’ self-management aims, benefits achieved, and challenges or enablers to achieving their self-management goals (Table S1). Website activity was logged and time-stamped to identify the number of days on which participants logged in and the number of pages loaded. The nurse recorded the number and duration of contacts by email, phone, and home visit.
Data analysis
Baseline characteristics for groups 1 and 2 were compared using Fisher’s exact, independent t-, and Mann–Whitney U tests. Baseline and follow-up outcome data for each group (14 patients in total) were analyzed with paired t- and Wilcoxon signed-rank tests. Statistical significance was set at P≤0.05. All statistical analysis was performed in SPSS version 23 (IBM, Armonk, NY, USA).
Transcribed interviews were imported into NVivo software and analyzed thematically.Citation34 Transcripts were initially read by FE to gain an overview of patients’ experiences. A deductive coding framework was developed by FE, consisting of codes from the interview-topic areas, and transcripts were coded by FE and ER. During coding, deductive codes were supplemented by inductive codes to capture unexpected findings. Codes were checked for duplication and redundancy and organized into categories. Categories were compared across transcripts and between the groups and summarized in matrices, on which the final interpretation was based.
Ethical considerations
This case series was categorized as a service evaluation by the Research and Development Department at Cambridge University Hospitals NHS Foundation Trust and was subsequently approved and registered as a service evaluation with the Safety and Quality Support Department at the same trust (project registration 570). Patients gave written informed consent to participate in the study to the nurse coach at the first visit. Specific written consent to participate in qualitative interviews was taken by KH at the beginning of the first interview.
Results
Participants
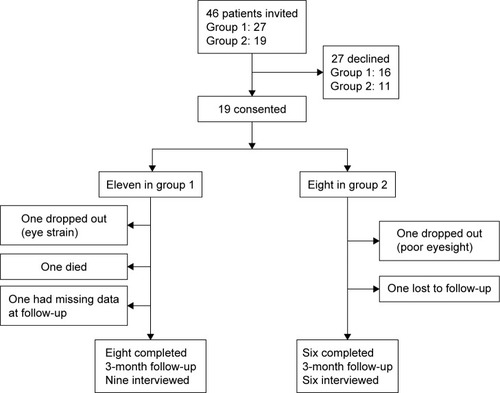
A total of 46 patients were invited and 19 responded (eleven in group 1 and eight in group 2) (). Commonest reasons for declining were not wishing to use the Internet and not needing help. A total of 14 patients completed 3-month follow-up (eight in group 1 and six in group 2). Patients lost to follow-up were older (mean 73.2±11.84 vs 60.64±9.44 years, P=0.028), but did not differ on any other baseline characteristic. Nine patients from group 1 and six from group 2 were interviewed, with interviews lasting 20–58 minutes.
Baseline characteristics
Several indicators of disease severity were more severe in group 1 compared to group 2: lower FEV1, FEV1% predicted and FEV1/FVC, and higher GOLD stage, Medical Research Council dyspnea scale, supplementary oxygen use, and hospital admissions in the previous year (). The mean number of exacerbations in the past year for group 2 was seven, higher than for group 1, despite few hospital admissions. These were self-reported exacerbations that required antibiotics or steroid use for worsening symptoms, and the data for group 2 were skewed by two patients who had 20 and 14 exacerbations (but only zero and one hospital admissions, respectively).
Table 1 Participant characteristics at baseline
Patient activation
Fourteen patients provided baseline and follow-up data (). Baseline activation scores were significantly lower (P=0.043) for group 1 (51.98±7.36) than group 2 (61.22±7.9). At follow-up, group 1 showed a significant increase (P=0.022) in activation from level 2 (51.98±7.36) to 3 (64.11±8.09). Group 2 increased insignificantly (P=0.111) from level 3 (61.22±7.89) to 4 (72.73±16.11).
Table 2 Change in outcome measures
Other outcomes
The only significant difference at baseline between groups 1 and 2 was in mastery (mean 3.44±1.38 vs 5.17±0.61, P=0.015). At follow-up, group 1 showed a clinically meaningful and statistically significant improvement in mastery (mean 3.44±1.38 to 4.38±1.4, P=0.04) and improvement in anxiety (mean 11.38±3.81 to 8.88±4.32, P=0.028). Both groups had reduced information needs (group 1, median [IQR] 5.5 [4.25–6] to 3 [1.25–3.75], P=0.008; group 2, 5.5 [2.26] to 3.33 [1.75], P=0.027).
Interview data
and describe the categories into which the codes were organized. In some cases, common category headings apply across both groups, but the way in which the category is manifested differs between the groups.
Table 3 Aims and benefits
Table 4 Facilitators and challenges in achieving self-management goals and using TPP
Aims
Both groups wished to improve their physical functioning and better manage their health and COPD (). In this regard, group 1 were focused on getting fitter and staying out of hospital, while group 2, with less severe COPD, focused on daily activities and slowing COPD progression. Group 1 also wanted more independence, and group 2 wanted increased motivation.
Benefits
Both groups benefited from improved physical functioning (). For group 1 this was the most commonly reported benefit and enabled more independence. Both groups felt better able to manage their COPD and gained understanding of healthy behaviors, such as healthy eating. Social and emotional functioning improved for both groups. While group 2 gained in self-belief, for group 1 the benefits were wider-ranging, including being able to connect better with others and improved mood and confidence:
I felt good enough to get out the door under me own steam, carrying my oxygen … I walked round the garden … feeling normal for, you know, it could be years actually. [115, group 1]
Some in group 2 benefited from being able to communicate better with health care professionals. One patient was able to be more assertive in explaining why they wanted a hospital referral, and this helped them to get the referral they had long wanted:
I’ve never been referred to the hospital, so [nurse coach] said, “What’s your goal?” Well, I went to [the doctor] and said, “I feel different and I want to know if there’s anything else going on”, so he sent me for chest X-rays … and took my blood … He phoned up [community respiratory nurse] and said about referring me to hospital … I achieved my goals. [122, group 2]
Factors facilitating goal achievement
Nurse-coach support was important for both groups and the benefits similar, although group 1 derived more in terms of emotional support. For this group, it had a greater impact than TPP ():
I was getting depressed and down, so [the nurse] … she suggested about the models … and that was an ideal thing … every time she spoke to me by phone or sent me an email or come round, she’s always asked how it’s going with the models. So yeah, that’s made a difference. [110, group 1]
The most helpful thing is, like, talking to [the nurse] about different things. Computers don’t really answer you back when you ask it a question. [108, group 1]
TPP provided additional support for both groups through information and action plans, eg, healthy eating and smoking cessation, but group 2 found TPP relatively more useful:
[TPP] gives you different ideas, what they class as one serving … it’s made me think about what I’m eating … I would have just thrown steak into a frying pan … whereas now I’ll grill it. [109, group 2]
Both groups used TPP most frequently to contact the nurse. Other facilitating factors relevant to both groups were social support from family and friends, psychological factors relating to the individual’s own feelings of confidence and motivation, and the possession of self-management skills, which in turn were supported by the nurse coach and the use of TPP.
Challenges to achieving goals
Poor physical well-being affected progress and prevented activity for both groups, but particularly so for group 1 ():
I’ve had a couple of chest infections, so I’ve been finding it quite hard. I’ve got a DVD that [the nurse] gave me. I haven’t been able to get into it because of the last few months. My tummy’s quite painful. [101, group 1]
For some in group 1, this reduced their confidence and was compounded by being in hospital. Psychological factors were a challenge for both groups, with anxiety a particular challenge for group 1:
I just get so out of breath that I just sit here because … I’m scared to get out of breath. Even though I know it’s not going to hurt me, it’s just very unpleasant. [105, group 1]
Both groups reported other priorities that made it more difficult to work toward goals. For group 1, there were more health-related commitments, and for group 2 more domestic tasks. Bad weather limited outside activity for both groups. In addition, some in group 1 reported lack of social support and resources for activities, while for some in group 2 behavioral factors, such as trying to do too much and poor housing, presented challenges.
Challenges in using TPP
Orientation toward IT and the design of TPP were challenges for some participants in both groups. In group 1, lack of interest in computers (one patient), poor IT skills and confidence (five) and difficulty using the site (three) made patients less willing or able to use TPP. Two who reported no benefits at all from TPP found it difficult to use, and one had poor IT skills. However, two of the highest users had poor IT skills, and one had found TPP difficult to use. In group 2, two participants reported no benefits from TPP. One found it impersonal and complicated:
I don’t feel that I’m mastering it … perhaps there’s too much in there. [118, group 2]
However, similarly to group 1, of the two highest users in group 2, one had poor IT skills and both found TPP difficult to use. Barriers related to individual circumstances were ill health among group 1 and pain and poor memory for passwords among group 2.
Contact and usage
On average, participants in group 1 accessed TPP 1.21 days/week and had 12.51 minutes of face-to-face contact time/week, 3.53 minutes of phone time/week, and 0.71 emails per week from the nurse coach (). Group 2 accessed TPP 1.32 days per week and had 18.54 minutes of face-to-face contact time/week, 2.67 minutes of phone time/week, and 1.27 emails per week. Both groups used TPP most frequently for messaging the nurse and secondly for action programs. The most frequent users were from both groups.
Table 5 The Preventive Plan usage and nurse-contact time
Discussion
In this case series of a self-management support intervention for COPD patients comprising an Internet-based health-promotion program coupled with nurse-coach support, patients with more advanced COPD (group 1) improved significantly in activation, mastery, and anxiety and reported increased independence and confidence. Both this group and a second group with less advanced disease (group 2) felt better informed about COPD and reported improved physical functioning, though benefits overall were greater for patients with more advanced COPD. This occurred despite group 1 not receiving disease-specific content that was made available to group 2 and having fewer emails from the nurse coach. For group 1, the motivational, emotional, and goal support from the nurse was more important than TPP in building confidence to self-manage; some patients with clear goals used the action plans and information resources in TPP as additional support. Group 2 participants valued the nurse support, but emphasized it less than TPP.
Group 1, with more advanced disease, had lower activation at baseline and achieved more positive outcomes than group 2, despite reporting more challenges, eg, being physically unwell, anxious, and low in confidence. This is consistent with other studies where participants with poorer baseline scores achieved greater gains from self-management and pulmonary rehabilitation programsCitation35 and improvement in self-efficacy following an expert-patients program.Citation36
Our work found benefits in CRQ mastery in group 1, in contrast to a previous study of a self-management program consisting of tailored sessions and telephone support from a nurse, which found no significant change in any CRQ domains or the COPD self-efficacy scale;Citation37 this may have been a result of greater disease severity in our cohort. We also observed significant improvements in HADS – anxiety in group 1, consistent with a supported self-management intervention of initial training sessions followed by nurse home visits in a similar cohort.Citation38 Other studies have found that patient-education programs have the potential to improve health-related quality of life within short time frames (4 months), although results are mixed.Citation39,Citation40
Both groups benefited from the nurse input (which was more important than TPP for group 1) and used TPP most frequently for contacting the nurse. Nurses add value to IT-based interventions by raising awareness of the need for behavior change,Citation17 providing positive feedback and goal supportCitation41 and social and motivational support to persevere with interventions.Citation17 In our intervention, the nurse was reassuring, and talking to her about COPD was supportive for patients. Relationships, including supportive and empathic relationships with healthcare professionals, are one of three core mechanisms for successful ehealth interventions.Citation42
Participants varied in their use of TPP. The most frequent users were from both groups and two of the highest users had poor IT skills, so disease severity and low IT confidence and skills were not necessarily barriers where participants were motivated. Williams et alCitation43 found that patients could use a tablet-based mobile-health application regardless of previous experience, and Cummings et alCitation44 reported that negative previous computer experience did not prevent adoption of an online self-monitoring diary.
Patient preference may be important for engagement in Internet-based interventions.Citation7 Not all participants were enthusiastic about using TPP: some later declared little interest in computers, and it may have differed from their expectations. Common reasons for low usage of ehealth applications are unfamiliarity with technology among elderly populations, insufficiently stimulating applications, lack of change of content over time, and low use by health care professionals.Citation6,Citation19,Citation20 Factors that increase user engagement, such as refreshing content on a regular basis, sending prompts, being able to choose elective components,Citation45 or tailoring health information to personal needs,Citation46 were present in TPP, but still not all participants were engaged. Some found it complex and difficult to navigate, which was a barrier to use. High-quality user-centered design is important for uptake and use of ehealth interventions.Citation43,Citation47 TPP was an off-the-shelf application, previously evaluated in workplace settings in the US,Citation48 and not validated in COPD patients. More engagement may be achieved with a dedicated application designed collaboratively with the target group and technology-design approaches combined with health models.Citation49
Implications for future research, policy, and practice
We found that participants with the lowest levels of activation gained the most. Nurse support was particularly important for those with greater emotional and self-management support needs. This suggests the need for careful assessment of patient needs to enable efficient targeting of specialist nurse support.
Disease severity and lack of IT skills were not necessarily barriers to using the Internet-based program, but lack of motivation to use computers was. It may be helpful for patients to be introduced to an internet-based package before an intervention, in order to assess motivation and manage expectations. Costs of the intervention were nurse-coach training in use of TPP and self-management support skills and nurse–patient contact time. The mean time spent by the nurse per patient was 15.25 minutes/week for group 1 and 21 minutes/week for group 2. However, self-management interventions have the potential to be cost-saving relative to usual careCitation50 and reduce respiratory-related hospitalisations.Citation4
Effing et alCitation51 provided a detailed definition of the requirements for a COPD self-management intervention. Key aspects of the definition include the need for structured personalized support, with an emphasis on motivating and engaging patients. The process requires interactions between patients and health care professionals that focus on identifying needs and motivations, eliciting goals, formulating strategies, and building confidence and competence. The definition emphasizes the importance of the relationship with the health care professional. The importance of this relationship was also apparent in our study, where the input from the nurse coach was key. There were no patients who reported that the online platform was helpful and the nurse coach was not; however, there were some patients who made little use of TPP or used it primarily to contact the nurse coach. The nurse coach was important, and for some the content and functionality of TPP provided additional benefits. Further research is needed on how and under what circumstances Internet-based support can best complement personal relationships with health care providers and how nonmedical factors impact the potential to benefit from such interventions.
Limitations
The total sample size was small, rendering numbers in each of the two groups very small. However, our aim was to explore the potential of combined ehealth support with nurse coaching in COPD, rather than to determine efficacy or establish generalizability. Results are thus presented as a contribution to generic learning in this field. For group 2, a pragmatic decision was made to provide additional structured pulmonary rehabilitation materials, and this could have impacted on outcomes. It is notable, however, that the lack of this extra resource for group 1 did not appear to be detrimental and that they achieved relatively greater benefits despite this. When measuring outcomes over time, regression to the mean can occur. Patients may join because they feel vulnerable and then naturally improve over time; however, improvement was different for the two groups. Data on patients’ treatment regimens and comorbidities were not available for analysis, and these factors may have an impact on patient activation and responses to this type of intervention. A wider study incorporating factors beyond COPD severity would be needed to establish this. Resources only enabled a follow-up period of 3 months, hence it was only possible to explore immediate impact. Sustainability of outcomes from self-management support interventions is an important issue, and a longer-term follow-up would be needed to address this.
Conclusion
This case series demonstrates the feasibility of combining nurse-coach support aligned to an Internet-based health resource, TPP, in COPD. Patients with more advanced disease and lower baseline activation had the largest change in activation. The case series provides knowledge about the challenges of such an approach and the importance of the nurse-coach role.
Author contributions
JF and FE conceived, sought funding for, and designed the study. FE and ER conducted the qualitative data analysis. FE, Ella M, and JF conducted the statistical analysis. JY and Emma M were key contributors to the interpretation of the data. All authors have been involved in drafting and revision of the manuscript for important intellectual content, and have approved the final version to be published. All authors agree to be accountable for aspects of the work. JF is the guarantor of the paper.
Acknowledgments
The Preventive Plan was supplied by UK Preventive Medicine Ltd (Acre House, 11/15 William Road, London NW1 3ER, UK), and we are grateful to Stefan Wisbauer from UK Preventive Medicine for technical support in its use. We thank Kate Homan who conducted the qualitative interviews, Petrea Fagan who supported the nurse coach in developing the self-management support skills necessary for the study, and the patients who participated in this study. The study was funded by NHS East of England Regional Innovation Funding, and delivery of this work was supported by the Cambridge Biomedical Research Centre.
Disclosure
The authors report no conflicts of interest in this work.
Supplementary materials
Further detailed description of the intervention and interview-topic guide are available from the corresponding author.
The Preventive Plan
The Preventive Plan (TPP) was a web-based program encompassing primary prevention (health promotion), secondary prevention (biometric and lab screening and early detection/diagnosis), and tertiary prevention (chronic condition management). TPP was personalized through the uploading of personal details, including medical history, medication, family history, weight, waist measurement, current lifestyle, dietary intake, and activity levels, via a 77 item questionnaire. The application incorporated four elements, described in the following paragraphs.
Following the uploading of personal details, a personalized health-risk assessment was generated, which indicated the individual’s highest risks of developing a range of conditions if no action were taken on current behavior. Risks were graded high, severe, and moderate and calculated using a variety of risk models, such as Framingham heart risk.Citation1 Based on this a personalized prevention plan was generated to address the health risks with a range of pre-programmed recommended action programs. Focusing on health-related behaviors, such as healthy eating, alcohol consumption, exercise, and smoking cessation, these guided the user through behavior change and offered step-by-step recommendations to achieve health benefits, while encouraging users to upload individual goal achievements. The duration of these action programs was around 8 weeks. This process was personalized to the extent that the action plan addressed an identified risk for the individual, but the plans themselves were not patient-led or -formed.
TPP also incorporated information resources, including daily health-news bulletins, which could be preselected relevant to identified health risks and action plans, and a health library/tutorial facility. In addition, local uploads were installed including links to the British Lung Foundation, carer support, local resources, and a COPD self-management personal health plan that included condition-related information, symptom-monitoring, and self-management action-plan templates. Participants also received a handheld copy of this personal health plan. Access was available to health information aimed at enhancing health literacy, an important aspect of self-management. TPP enabled email communication with the nurse coach, who could also monitor when users accessed the program.
Nurse-coach support
Use of the package was integrated with support from a trained respiratory nurse via home visits, telephone, and email contact. The nurse coach assisted participants to use the website and hardware (if provided), and supported patient self-management through individualized patient-led goal-setting. The role comprised user support for TPP, encouragement to use TPP, and “signposting” to other online resources for self-management through supportive email messages.
Patient-centered coaching to enhance confidence to self-manage was also a component. This included agenda-setting, patient-led goal-setting, support for and action planning to complement TPP-generated action plans, problem-solving, goal review, verbal encouragement, and focus on past successes. Patient-led goals could range from specific health-related behaviors, such as healthy eating, to broader lifestyle issues, such as meeting friends. Specifically, the communication style of this role incorporated coproduction, and was distinct from that of the nurse coach’s usual role as a respiratory nurse specialist, in that there was a strong emphasis on support relative to expert medical advice. For example, if a patient were to say that they thought they were having an exacerbation and ask if they should start their rescue pack, the role of the nurse coach was to educate through asking:
Why do you think you are having an exacerbation? What are your symptoms? What advice have you been given about these symptoms previously? Do you have any written instructions, such as a self-management plan?
This required specific skills distinct from medical knowledge. Education to complement information was available through TPP, with condition-specific education as appropriate to each participant’s needs.
When a participant joined the project, the nurse made an initial home visit. During this visit, she introduced the participant to TPP, provided contact details and written information about the program, collected baseline assessment data, supported the patient in completing the health-risk assessment, generated the personal prevention plan, and discussed self-management priorities, patient-led goal-setting, and action plan, and agreed on follow-up contact.
During each subsequent contact, the nurse would support the participant in problem-solving and working toward their goals, agreeing on methods and timing of goal follow-up on each occasion according to patient preference. Participants were asked whether they would like the next contact to be a visit, phone call, or text. If more than 14 days had elapsed since the previous contact, then the nurse coach would text the patient inquiring what progress they were making. If no reply had been received within 3–4 days, then she would telephone. The level of support provided by the nurse coach was flexible and responsive to the patient’s level of engagement with the intervention, eg, more frequent phone calls or emails to encourage contact with patients who were not readily engaging.
Table S1 Interview-topic guide
Reference
- KannelWBDawberTRKaganARevotskieNStokesJ3rdFactors of risk in the development of coronary heart disease: six-year follow-up experienceAnn Intern Med1961551335013751193
References
- British Lung FoundationChronic obstructive pulmonary disease (COPD) statistics Available from: http://statistics.blf.org.uk/copdAccessed January 27, 2017
- YohannesAMBaldwinRCConnollyMJDepression and anxiety in elderly patients with chronic obstructive pulmonary diseaseAge Ageing200635545745916638758
- TomsJHarrisonKLiving with chronic lung disease and the effect of pulmonary rehabilitationPhysiotherapy20028810605619
- ZwerinkMBrusse-KeizerMvan der ValkPDSelf-management for patients with chronic obstructive pulmonary diseaseCochrane Database Syst Rev20143CD00299024665053
- CannonDBuysNSriramKBSharmaSMorrisNSunJThe effects of chronic obstructive pulmonary disease self-management interventions on improvement of quality of life in COPD patients: a meta-analysisRespir Med2016121819027888996
- Voncken-BrewsterVTangeHde VriesHNagykaldiZWinkensBvan der WeijdenTA randomized controlled trial evaluating the effectiveness of a web-based, computer-tailored self-management intervention for people with or at risk for COPDInt J Chron Obstruct Pulmon Dis2015101061107326089656
- NguyenHQDoneskyDReinkeLFInternet-based dyspnea self-management support for patients with chronic obstructive pulmonary diseaseJ Pain Symptom Manage2013461435523073395
- BurkowTMVognildLKØstengenGInternet-enabled pulmonary rehabilitation and diabetes education in group settings at home: a preliminary study of patient acceptabilityBMC Med Inform Decis Mak2013133323496829
- McLeanSNurmatovULiuJLTelehealthcare for chronic obstructive pulmonary diseaseCochrane Database Syst Rev20117CD00771821735417
- WoottonRTwenty years of telemedicine in chronic disease management: an evidence synthesisJ Telemed Telecare201218421122022674020
- LundellSHolmnerARehnBNybergAWadellKTelehealth-care in COPD: a systematic review and meta-analysis on physical outcomes and dyspneaRespir Med20151091112625464906
- LiuFCaiHTangQEffects of an animated diagram and video-based online breathing program for dyspnea in patients with stable COPDPatient Prefer Adherence2013790591324049441
- MoyMLCollinsRJMartinezCHAn Internet-mediated pedometer-based program improves health-related quality-of-life domains and daily step counts in COPD: a randomized controlled trialChest2015148112813725811395
- Barberan-GarciaAVogiatzisISolbergHSEffects and barriers to deployment of telehealth wellness programs for chronic patients across 3 European countriesRespir Med2014108462863724451438
- CummingsERobinsonAPrattHCPathways Home: comparing voluntary IT and non-IT users participating in a mentored self-management projectStud Health Technol Inform2010160Pt 1232720841643
- SticklandMJourdainTWongEYRodgersWMJendzjowskyNGMacdonaldGFUsing telehealth technology to deliver pulmonary rehabilitation in chronic obstructive pulmonary disease patientsCan Respir J201118421622022059179
- van der WeegenSVerweyRSpreeuwenbergMTangeHvan der WeijdenTde WitteLIt’s Life! Mobile and web-based monitoring and feedback tool embedded in primary care increases physical activity: a cluster randomized controlled trialJ Med Internet Res2015177e18426209025
- ZanaboniPLienLAHjalmarsenAWoottonRLong-term telere-habilitation of COPD patients in their homes: interim results from a pilot study in northern NorwayJ Telemed Telecare201319742542924218358
- BotsisTHartvigsenGCurrent status and future perspectives in telecare for elderly people suffering from chronic diseasesJ Telemed Telecare200814419520318534954
- TabakMBrusse-KeizerMvan der ValkPHermensHVollenbroek-HuttenMA telehealth program for self-management of COPD exacerbations and promotion of an active lifestyle: a pilot randomized controlled trialInt J Chron Obstruct Pulmon Dis2014993594425246781
- AuDHMacaulayDSJarvisJLDesaiUSBirnbaumHGImpact of a telehealth and care management program for patients with chronic obstructive pulmonary diseaseAnn Am Thorac Soc201512332333125642649
- CasasATroostersTGarcia-AymerichJIntegrated care prevents hospitalisations for exacerbations in COPD patientsEur Respir J200628112313016611656
- de ToledoPJiménezSdel PozoFRocaJAlonsoAHernandezCTelemedicine experience for chronic care in COPDIEEE Trans Inf Technol Biomed200610356757316871726
- LilholPHHæsumLKHejlesenOKExploring user experience of a telehealth system for the Danish TeleCare North trialStud Health Technol Inform201521030130525991154
- CummingsETurnerPPatient self-management and chronic illness: evaluating outcomes and impacts of information technologyStud Health Technol Inform200914322923419380941
- HardingeMRutterHVelardoCUsing a mobile health application to support self-management in chronic obstructive pulmonary disease: a six-month cohort studyBMC Med Inform Decis Mak2015154626084626
- HibbardJHStockardJMahoneyERTuslerMDevelopment of the Patient Activation Measure (PAM): conceptualising and measuring activation in patients and consumersHealth Serv Res2004394 Pt 11005102615230939
- HibbardJHGilburtHSupporting People to Manage their Health: An Introduction to Patient ActivationLondonKing’s Fund2014
- SharmaSWallaceLMKosmala-AndersonJRealpeATurnerAPerceptions and experiences of co-delivery model for self-management training for clinicians working with patients with long-term conditions at three healthcare economies in UKWorld Hosp Health Serv2011472222422073878
- HibbardJHMahoneyERStockardJTuslerMDevelopment and testing of a short form of the patient activation measureHealth Serv Res2005406 Pt 11918193016336556
- GuyattGHBermanLBTownsendMPugsleySOChambersLWA measure of quality of life for clinical trials in chronic lung diseaseThorax198742107737783321537
- ZigmondASSnaithRPThe Hospital Anxiety and Depression ScaleActa Psychiatr Scand19836763613706880820
- JonesRCWangXHardingSBottJHylandMEducational impact of pulmonary rehabilitation: Lung Information Needs QuestionnaireRespir Med2008102101439144518676136
- BraunVClarkeVUsing thematic analysis in psychologyQual Res Psychol20063277101
- ScottASBaltzanMAFoxJWolkoveNSuccess in pulmonary rehabilitation in patients with chronic obstructive pulmonary diseaseCan Respir J201017521922321037996
- ReevesDKennedyAFullwoodCPredicting who will benefit from an Expert Patients Programme self-management courseBr J Gen Pract20085854819820318318974
- BischoffEWAkkermansRBourbeauJvan WeelCVercoulenJHSchirmerTRComprehensive self management and routine monitoring in chronic obstructive pulmonary disease patients in general practice: randomised controlled trialBMJ2012345e764223190905
- BucknellCEMillerGLloydSMGlasgow supported self-management trial (GSuST) for patients with moderate to severe COPD: randomised controlled trialBMJ2012344e106022395923
- BourbeauJJulienMMaltaisFReduction of hospital utilization in patients with chronic obstructive pulmonary disease: a disease-specific self-management interventionArch Intern Med2003163558559112622605
- RiceKLDewanNBloomfieldHEDisease management program for chronic obstructive pulmonary disease: a randomized controlled trialAm J Respir Crit Care Med2010182789089620075385
- VerweyRvan der WeegenSSpreeuwenbergMTangeHvan der WeijdenTde WitteLA pilot study of a tool to stimulate physical activity in patients with COPD or type 2 diabetes in primary careJ Telemed Telecare2014201293424414397
- VassilevIRowsellAPopeCAssessing the implementability of telehealth interventions for self-management support: a realist reviewImplement Sci2015105925906822
- WilliamsVPriceJHardingeMTarassenkoLFarmerAUsing a mobile health application to support self-management in COPD: a qualitative studyBr J Gen Pract201464624e392e40024982491
- CummingsERobinsonAPrattHCPathways Home: Comparing voluntary IT and non-IT users participating in a mentored self-management projectStud Health Technol Inform2010160Pt 1232720841643
- Voncken-BrewsterVTangeHMoserANagykaldiZde VriesHvan der WeijdenTIntegrating a tailored e-health self-management application for chronic obstructive pulmonary disease patients into primary care: a pilot studyBMC Fam Pract201415424400676
- DijkstraAWorking mechanisms of computer-tailored health education: evidence from smoking cessationHealth Educ Res200520552753915701665
- AhernDKChallenges and opportunities of eHealth researchAm J Prev Med2007325 SupplS75S8217466822
- LoeppkeREdingtonDWBégSImpact of the prevention plan on employee health risk reductionPopul Health Manag201013527528420879909
- PortzJDMillerAFosterBLaudemanLPersuasive features in health information technology interventions for older adults with chronic diseases: a systematic reviewHealth Technol2016628999
- BourbeauJColletJPSchwartzmanKDucruetTNaultDBradleyCEconomic benefits of self-management education in COPDChest200613061704171117166985
- EffingTWVercoulenJHBourbeauJDefinition of a COPD self-management intervention: International Expert Group consensusEur Respir J2016481465427076595