Abstract
Background and objectives
Acute exacerbation of chronic obstructive pulmonary disease (AECOPD) is one of the leading causes of hospitalization and is associated with considerable mortality, for which clinicians are seeking useful and easily obtained biomarkers for prognostic evaluation. This study aimed to determine the potential role of the neutrophil–lymphocyte ratio (NLR) and platelet–lymphocyte ratio (PLR) as prognostic makers for hospital mortality in patients with AECOPD.
Methods
We included 303 patients with AECOPD in this retrospective study. Clinical characteristics, NLR, PLR, and serum levels of C-reactive protein (CRP) and other data were collected. Relationships between NLR/PLR and CRP were evaluated by Pearson’s correlation test. Receiver operating characteristics curve and the area under the curve (AUC) were used to assess the ability of NLR and PLR to predict hospital mortality in patients with AECOPD.
Results
Mean levels of NLR and PLR of all patients with AECOPD were 7.92±8.79 and 207.21±148.47, respectively. NLR levels correlated with serum CRP levels (r=0.281, P<0.05). The overall hospital mortality rate was 12.21% (37/303). Levels of NLR and PLR were signifi-cantly higher among non-survivors compared to survivors of AECOPD (both P<0.05). At a cut-off value of 6.24, the sensitivity and specificity of the NLR in predicting hospital mortality were 81.08% and 69.17%, respectively, with an AUC of 0.803. At a cut-off of 182.68, the corresponding sensitivity, specificity and AUC of PLR were 64.86%, 58.27%, and 0.639. The combination of NLR, PLR, and CRP increased the prognostic sensitivity.
Conclusion
NLR and PLR levels were increased in non-survivor patients with AECOPD, and the NLR may be simple and useful prognostic marker for hospital mortality in patients with AECOPD. More studies should be carried out to confirm our findings.
Introduction
Chronic obstructive pulmonary disease (COPD) is a common chronic airway inflammatory disease characterized by persistent respiratory symptoms and airflow limitation.Citation1 COPD is associated, worldwide, with high morbidity and mortality. In China, the overall incidence of COPD was 8.2% in residents older than 40, based on a cross-sectional survey in seven provinces/cities;Citation2 in the USA, COPD was the third leading cause of mortality in 2011.Citation3 Acute exacerbation of COPD (AECOPD) is associated with an acute worsening of respiratory symptoms that result in additional therapy.Citation1 AECOPD has an independent and significant negative influence on the prognosis of patients with COPD, it increases the frequency of further severe exacerbations, reduces health status and physical activity, speeds the decline of lung function, increases mortality, and places great economic burden on patients – with both high direct and in-direct medical costs.Citation4–Citation6
AECOPD is one of the leading causes of hospitalization, and contributes significantly to mortality among patients with COPD.Citation7 Considering the important role of AECOPD in the prognosis of patients with COPD, early and accurate individual mortality risk assessment during exacerbation is of critical importance for clinical management, and is helpful for optimal allocation of limited medical resources. Clinicians are seeking clinically meaningful predictors of mortality following AECOPD admission, especially for biomarkers which can be easily obtained upon admission.Citation8
AECOPD is associated with increased systemic and airway inflammation, and enhanced inflammation worsens clinical symptoms and decreases lung function of patients, necessitating hospitalized treatment.Citation9,Citation10 The neutrophil–lymphocyte ratio (NLR) is an marker of inflammatory status, representing both the neutrophil and lymphocyte counts;Citation11 the platelet–lymphocyte ratio (PLR) is also accepted as a novel marker in many systemic inflammatory disorders.Citation12 Both NLR and PLR are indicators of general immune response to various stress stimuli, and play an important role in the prognostic evaluation of a series of diseases, including malignant cancers, myocardial infarction, community-acquired pneumonia, and acute pulmonary embolism.Citation13–Citation17 However, limited data have been presented on the relationship between NLR/PLR and clinical outcomes of hospitalized patients with AECOPD. This study sought to investigate the prognostic role of NLR/PLR on in-hospital mortality of patients with AECOPD.
Methods
Patients
Patients with AECOPD who were admitted in Yongchuan Hospital, Chongqing Medical University from March 2014 to June 2016 were retrospectively enrolled in this study. All patients signed an informed consent for scientific research of clinical data during hospitalization, and ethics approval was obtained from the Yongchuan Hospital Ethics Committee.
Patients were included this study if they met the following criteria: 1) primary diagnosis of AECOPD, defined as an acute worsening of respiratory symptoms such as dyspnea, cough, or sputum purulence severe enough to warrant hospital admission;Citation1 2) a COPD diagnosis supported by spirometric data of airflow obstruction even with bronchodilator (forced expiratory volume in 1 second [FEV1]/forced vital capacity [FVC] <0.70) when clinically stable at least for 3 months;Citation1 and 3) age ≥40 years, and admitted from their primary residence. For patients with multiple hospital admissions, only the first admission was recorded. A patient was excluded if AECOPD was not the primary diagnosis, the patient had other acute events such as acute myocardial infarction, or the patient had other end-stage diseases. The treatment plan for each patient was not influenced by participation in current study.
Data collection
Demographic and clinical data were collected from all subjects, including: age, gender, smoking history, lung function test results (FEV1, FEV1%Pred, FVC, and FEV1/FVC), arterial blood gas on admission (SpO2, PaO2, PaCO2, and pH value), serum C-reactive protein (CRP) levels (immunofluorescence and i-CHROMA Reader), routine blood test results on admission before antibiotic treatment (white blood cell, platelets, neutrophils, lymphocytes; Sysmex XN1000), length of hospital stay, and in-hospital mortality. Data collection was completed by two independent authors.
Statistical analysis
Data are represented as mean ± standard deviation. Categorical data are represented as frequencies and percentages. Differences between the survivor and non-survivor groups were compared by chi-squared test for categorical variables and an unpaired t-test for continuous variables. Relationships between NLR/PLR and CRP were evaluated by Pearson’s correlation test. Receiver operating characteristic (ROC) curve analysis was used to evaluate the sensitivity and specificity of different potential predictors of in-hospital mortality. In addition, we assessed the ability of two- or three-marker combinations to predict in-hospital mortality with methods recommended by Creaney et al.Citation18 Data on NLR, PLR, and CRP were transformed with the natural logarithm and then standardized relative to controls; a logistic regression to predict AECOPD death/alive status was used to determine the weight given to each standardized marker. Markers were multiplied by their logistic regression coefficients and added to give a combined marker value, which was used to calculate sensitivity and specificity. The area under the curve (AUC) was used to assess prognostic accuracy, which ranges from 0.5 to 1.0 – with higher values indicating higher discriminatory ability.Citation19 Data analysis was conducted using SPSS 18.0 for Windows (IBM, Chicago, IL, USA). The level of significance for all statistical tests was set as a two-sided P-value of 0.05.
Results
Characteristics of included subjects
Finally, 303 patients with AECOPD met our inclusion criteria and were included in this study. There were 200 men and 103 women, and the mean age was 61 years. The numbers of patients for each class of the Global Initiative for Chronic Obstructive Lung Disease classification were: 44, 132, 102, and 25 for classes I, II, III, and IV, respectively; the mean FEV1%predicted value was 56%, suggesting most patients presented with moderate airflow limitation. Overall, 273 (90%) patients with AECOPD underwent a chest X-ray or chest CT scan examination. The mean length of hospitalization was 15 days, and 33 patients died during hospitalization, corresponding to an in-hospital mortality of 12.21%. The clinical characteristics, lung function data, and main laboratory findings of survivors and non-survivors are listed in .
Table 1 Clinical summary of patients with AECOPD
NLR and PLR levels
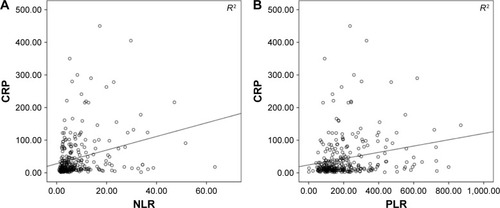
The mean NLR and PLR levels across all patients with AECOPD were 7.92 and 207.21, respectively. NLR levels correlated positively with serum CRP levels (r=0.281, P<0.001), whereas the correlation between PLR and serum CRP levels did not demonstrate a linear association (r=0.219, P<0.001; ). As shown in , levels of NLR and PLR were significantly higher among patients who died in hospital than among those who survived (both P<0.05).
Figure 1 Correlations of the NLR and PLR with C-reactive protein (CRP).
Predictive ability of NLR, PLR, and CRP
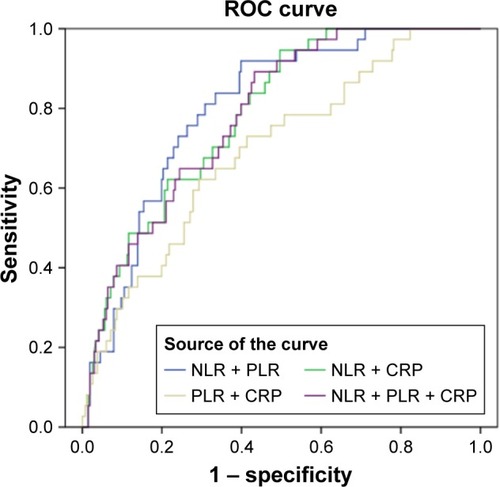
ROC curve analysis for using NLR alone to predict in-hospital mortality indicated an optimal cut-off NLR of 6.24, AUC of 0.803, sensitivity of 81.08%, and specificity of 69.17% (). This predictive ability exceeded that of CRP or PLR individually. Next, we investigated the predictive accuracy of different biomarker combinations: combining NLR with other markers increased predictive sensitivity, with the best AUC of 0.800 obtained using a combination of NLR and PLR (). The predictive accuracy of a single marker or a marker combination is listed in .
Table 2 Prognostic accuracy of the NLR, PLR, and CRP
Figure 2 ROC curves of the NLR, PLR, or CRP for predicting in-hospital mortality of patients with acute exacerbation of chronic obstructive pulmonary disease. The receiver operating characteristic (ROC) curves for single predictors had the following areas: neutrophil–lymphocyte ratio (NLR), 0.803; C-reactive protein (CRP), 0.703; and platelet–lymphocyte ratio (PLR), 0.639.
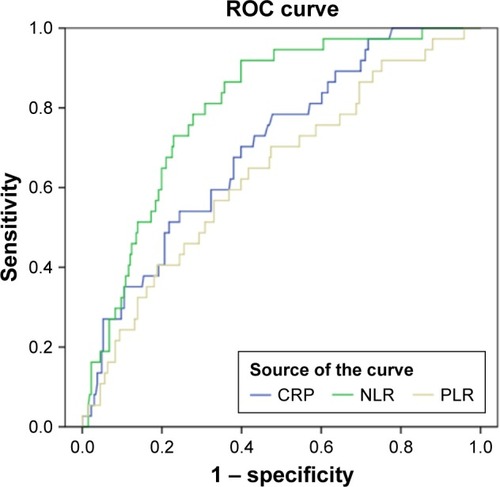
Figure 3 ROC curves of the NLR, PLR, and CRP combinations for predicting in-hospital mortality of patients with acute exacerbation of chronic obstructive pulmonary disease. The receiver operating characteristic (ROC) curves for combined predictors had the following areas: NLR + PLR, 0.800; NLR + CRP, 0.785; PLR + CRP, 0.694; NLR + PLR + CRP, 0.783.
Discussion
AECOPD is an acute event during the clinical course of COPD, and is significantly associated with the clinical outcomes of patients with COPD by worsening clinical symptoms, declining lung function, and increasing mortality.Citation20 Identifying a simple and reliable biomarker that can accurately assess the mortality risk during AECOPD hospitalization is of great importance for the management of patients and rational allocation of medical resources. In this study, we found that NLR levels correlated with CRP – a systemic inflammation maker – in patients with AECOPD, and NLR and PLR levels were higher in non-survivors than in survivors who were patients with AECOPD; the NLR plays a valuable role in predicting the in-hospital mortality of patients with AECOPD.
COPD is associated with both enhanced airway and systemic inflammation and, during states of exacerbation, the severity of inflammation is significantly increased,Citation21 and may stimulate the increase of the NLR and PLR, which may be used as markers of inflammation and as prognostic markers for patients with AECOPD. CRP is a classical inflammatory maker, and has been used to evaluate the systemic inflammation and prognosis of patients with COPD.Citation22 In our study, we observed that serum CRP levels were significantly increased in non-survivor patients with AECOPD. Taylan et al reported that increased NLR is as useful as CRP in the evaluation of elevated inflammation in AECOPD, and the NLR is useful for the early identification of potential acute exacerbations in patients with COPD who have normal levels of traditional markers.Citation23 The NLR is a straightforward and valuable biomarker of AECOPD that may contribute as a predictor for respiratory hospitalization in patients with COPD.Citation24 In this study, we observed that levels of NLR were increased in patients with AECOPD and correlated positively with CRP levels, and NLR levels were higher in non-survivors than in survivor patients with AECOPD. At a cut-off value of 6.24, the sensitivity and specificity of NLR in predicting in-hospital mortality were 81.08% and 69.17%, respectively, with an AUC of 0.800. The results suggest that the NLR is useful as a prognostic biomarker for hospital mortality in patients with AECOPD. In addition, two studies supported that elevated NLR may be associated with long-term mortality in patients with COPD.Citation25,Citation26 Thus, the NLR plays multiple roles in AECOPD as a predictor of hospitalization, inflammation evaluation, and in-hospital/long-term mortality, and is helpful in the clinical management of patients with AECOPD.
Platelet activation is observed in patients with COPD and AECOPD, and represents a novel pathological mechanism in COPD.Citation27 Thus, the PLR, another inflammatory biomarker, is increased in COPD, and PLR levels were also significantly higher in patients with AECOPD compared to those with stable COPD.Citation28 In this study, for the first time, we evaluated the ability of the PLR to determine the clinical outcomes of hospitalized patients with AECOPD, and we found that, at a cut-off value of 182.68, the sensitivity and specificity of the PLR in predicting hospital mortality were 64.86% and 58.27%, respectively, with an AUC of 0.64, which suggests a lower predictive accuracy than with the NLR. In addition, the correlation between the PLR and CRP is not linear (r=0.219); thus, the predictive accuracy of the PLR alone should be revisited and should be explained with caution. The combination of PLR and CRP with NLR increased the prognostic sensitivity for in-hospital mortality in patients with AECOPD. We suggest that results of the NLR and PLR should be explained with a traditional inflammatory maker such as CRP to ensure better prognostic accuracy.
Our study suggests that the NLR is a simple and useful biomarker for predicting in-hospital mortality in patients with AECOPD, as routine blood testing is available and affordable for each patient with AECOPD; the clinic utility of the NLR may be superior to that of other markers, which may need specific equipment or reagent. However, there were several limitations in our study. Our result in this Chinese cohort was from a single medical center, and it should be verified in larger studies with multiple centers and with different ethnic groups. More studies are needed to build a more definite conclusion on the prognostic accuracy of NLR and PLR in patients with AECOPD for both short- and long-term mortality. Second, future work should examine how the predictive power of the NLR and PLR relates to infection, to determine their ability of discriminating bacterial from nonbacterial AECOPD. Further studies with larger patient series are required to highlight the clinical significance of the NLR and PLR in the responses of patients with AECOPD to antibiotic therapy and further exacerbations.
Conclusion
This study suggests that NLR and PLR levels were increased in non-survivor patients with AECOPD, and the NLR is a simple, promising prognostic marker for assessing in-hospital mortality in patients with AECOPD. These findings justify further work into the role of the NLR and PLR in comprehensive management of patients with AECOPD.
Author contributions
CY and XL contributed to data collection, statistical analysis, and drafting the paper; ZT designed the study and revised the manuscript. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- VogelmeierCFCrinerGJMartinezFJGlobal strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summaryAm J Respir Crit Care Med2017195555758228128970
- ZhongNWangCYaoWPrevalence of chronic obstructive pulmonary disease in China: a large, population-based surveyAm J Respir Crit Care Med2007176875376017575095
- HoyertDLXuJQDeaths: preliminary data for 2011Natl Vital Stat Rep2012616165
- Soler-CataluñaJJMartínez-GarcíaMARomán SánchezPSalcedoENavarroMOchandoRSevere acute exacerbations and mortality in patients with chronic obstructive pulmonary diseaseThorax2005601192593116055622
- WedzichaJASinghRMackayAJAcute COPD exacerbationsClin Chest Med201435115716324507843
- OzkayaSFindikSAticiAGThe costs of hospitalization in patients with acute exacerbation of chronic obstructive pulmonary diseaseClinicoecon Outcomes Res20113151821935328
- LimaFVYenTYPatelJKTrends in in-hospital outcomes among adults hospitalized with exacerbation of chronic obstructive pulmonary diseaseCOPD201512663664226263035
- SinganayagamASchembriSChalmersJDPredictors of mortality in hospitalized adults with acute exacerbation of chronic obstructive pulmonary diseaseAnn Am Thorac Soc2013102818923607835
- ZhouXLiQZhouXExacerbation of chronic obstructive pulmonary diseaseCell Biochem Biophys201573234935527352322
- GroenewegenKHPostmaDSHopWCWieldersPLSchlösserNJWoutersEFCOSMIC Study GroupIncreased systemic inflammation is a risk factor for COPD exacerbationsChest2008133235035718198263
- FariaSSFernandesPCJrSilvaMJThe neutrophil-to-lymphocyte ratio: a narrative reviewEcancermedicalscience20161070228105073
- YangWWangXZhangWNeutrophil-lymphocyte ratio and platelet-lymphocyte ratio are 2 new inflammatory markers associated with pulmonary involvement and disease activity in patients with dermatomyositisClin Chim Acta2017465111627965019
- TempletonAJMcNamaraMGŠerugaBPrognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysisJ Natl Cancer Inst20141066dju12424875653
- AzabBShahNAkermanMMcGinnJTJrValue of platelet/lymphocyte ratio as a predictor of all-cause mortality after non-ST-elevation myocardial infarctionJ Thromb Thrombolysis201234332633422466812
- YangTWanCWangHThe prognostic and risk-stratified value of neutrophil–lymphocyte count ratio in Chinese patients with community-acquired pneumoniaEur J Inflamm20171512227
- de JagerCPWeverPCGemenEFThe neutrophil-lymphocyte count ratio in patients with community-acquired pneumoniaPLoS One2012710e4656123049706
- KarataşMBİpekGOnukTAssessment of prognostic value of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in patients with pulmonary embolismActa Cardiol Sin201632331332027274172
- CreaneyJYeomanDMuskAWde KlerkNSkatesSJRobinsonBWPlasma versus serum levels of osteopontin and mesothelin in patients with malignant mesothelioma – which is best?Lung Cancer2011741556021397972
- StreinerDLCairneyJWhat’s under the ROC? An introduction to receiver operating characteristics curvesCan J Psychiatry200752212112817375868
- Rodríguez-RoisinRCOPD exacerbations. 5: managementThorax200661653554416738044
- GanWQManSFSenthilselvanASinDDAssociation between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a meta-analysisThorax200459757458015223864
- LeuzziGGaleoneCTavernaFSuatoniPMorelliDPastorinoUC-reactive protein level predicts mortality in COPD: a systematic review and meta-analysisEur Respir Rev201726143 pii:160070
- TaylanMDemirMKayaHAlterations of the neutrophil-lymphocyte ratio during the period of stable and acute exacerbation of chronic obstructive pulmonary disease patientsClin Respir J201711331131726096858
- LeeSJLeeHRLeeTWUsefulness of neutrophil to lymphocyte ratio in patients with chronic obstructive pulmonary disease: a prospective observational studyKorean J Intern Med201631589189827017385
- SørensenAKHolmgaardDBMygindLHJohansenJPedersenCNeutrophil-to-lymphocyte ratio, calprotectin and YKL-40 in patients with chronic obstructive pulmonary disease: correlations and 5-year mortality – a cohort studyJ Inflamm (Lond)2015122025908927
- XiongWXuMZhaoYWuXPudasainiBLiuJMCan we predict the prognosis of COPD with a routine blood test?Int J Chron Obstruct Pulmon Dis20171261562528243079
- MaclayJDMcAllisterDAJohnstonSIncreased platelet activation in patients with stable and acute exacerbation of COPDThorax201166976977421507906
- KurtipekEBekciTTKesliRSamiSSTerziYThe role of neutrophil-lymphocyte ratio and platelet-lymphocyte ratio in exacerbation of chronic obstructive pulmonary diseaseJ Pak Med Assoc201565121283128726627508
