Abstract
Purpose
A straightforward, noninvasive method is needed to assess emphysema and pulmonary hypertension (PH) in COPD patients. The desaturation–distance ratio (DDR) is an index derived from the distance traveled and level of desaturation during a six-minute walk test (6MWT); it has previously been shown to be associated with percentage of forced expiratory volume in the first second of expiration (%FEV1.0) and percentage of diffusion capacity of the lung for carbon monoxide (%DLCO). The aim of this study was to examine the associations between DDR and emphysema and PH.
Patients and methods
We collected the following data for 74 stable COPD outpatients: lung function tests (%FEV1.0 and %DLCO), 6MWT distance and desaturation, and area of emphysema on computed tomography (percentage of low attenuation area). Enlargement of the pulmonary artery (PA) was assessed by the ratio of the diameter of the PA to that of the aorta (PA:A ratio) as an index of PH. DDR was calculated by the distance traveled and the degree of desaturation reached during a 6MWT. The relationships between study outcomes were assessed with Spearman’s rank-correlation analysis. Receiver operating characteristic (ROC) curves were used to determine the threshold values with the optimum cutoff points for predicting severe or very severe airway obstruction, pulmonary diffusing capacity disorder, moderate or severe emphysema, and enlargement of the PA.
Results
DDR correlated significantly with %FEV1.0, %DLCO, %LAA, and PA:A ratio. DDR showed high accuracy (area under the ROC curve >0.7) for predicting severe or very severe airway obstruction, pulmonary diffusing capacity disorder, moderate or severe emphysema, and enlargement of the PA.
Conclusion
The results suggest that DDR is a good index of emphysema and PH in COPD patients. The 6MWT is widely used to assess COPD, and DDR could help with the early diagnosis of COPD.
Introduction
COPD is characterized by airflow obstruction and emphysema.Citation1,Citation2 These two conditions commonly coexist, often with different degrees of severity;Citation3 indeed, emphysema has been confirmed in smokers without airflow obstruction.Citation4–Citation7 Emphysema affects quality of life and has been shown to be associated with exacerbations of COPD and deteriorating pulmonary function.Citation7 Pulmonary hypertension (PH) is an important serious comorbidity of COPD, which has been shown to be associated with the exacerbation of COPD and mortality.Citation8,Citation9 Right heart catheterization (RHC) is the gold standard method for the diagnosis or evaluation of PH,Citation10,Citation11 but it can be difficult in practice to provide all COPD patients with RHC because of its high degree of invasiveness.Citation9 The ratio of the diameter of the pulmonary artery (PA) to that of the aorta (PA:A ratio), measured by computed tomography (CT), is an index for enlargement of the PA, a condition independently related to exacerbations in COPD patients.Citation12 The PA:A ratio has been reported to be superior to echocardiography in the diagnosis of resting PH in patients with severe COPD.Citation13 Indeed, CT provides a range of information about COPD, including the extent of emphysema and PH, but it cannot be used in all situations. An easier noninvasive method that takes account of the various manifestations of COPD is needed for early diagnosis.
The six-minute walk test (6MWT) is a straightforward and low-cost test used worldwide to evaluate the exercise capacity of patients with COPD.Citation14 The six-minute walk distance (6MWD) and the degree of exercise-induced oxygen desaturation (EID) measured during the 6MWT have been shown to be related to emphysema and PH in COPD patients.Citation15–Citation18 The desaturation–distance ratio (DDR), calculated from the 6MWD and the degree of EID during the 6MWT, has recently been proposed as an index for the assessment of interstitial lung disease.Citation19 The DDR has been shown to be associated with pulmonary function in COPD patients, including the degree of airflow obstruction and pulmonary diffusing capacity.Citation19,Citation20 However, there have been no reports examining whether the DDR was related to the degree of emphysema or PH in COPD patients. The aim of this study, therefore, was to examine whether the DDR could be used to assess emphysema and PH in COPD patients.
Patients and methods
Study subjects
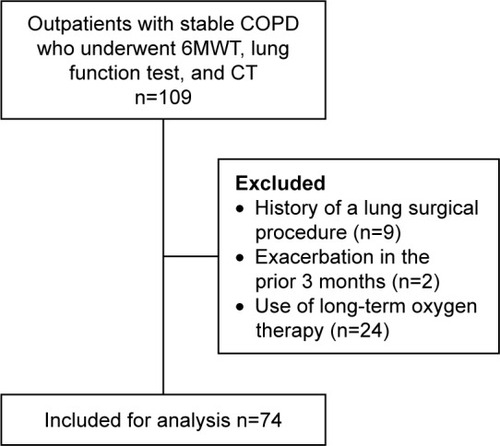
The outpatients with stable COPD who visited Kobe City Medical Center West Hospital between 2014 and 2016 were enrolled in this study. The diagnosis of COPD was based on the following criteria: age >40 years, a smoking history of ≥20 pack-years, and a ratio of the forced expiratory volume in the first second of expiration (FEV1.0) to forced vital capacity (FVC) <70%. The subjects were classified according to the Global initiative for chronic Obstructive Lung Disease (GOLD) airflow limitation. In addition, clinical symptoms such as a chronic cough, sputum, or dyspnea and smoking history, and/or emphysema on CT were included in the physician’s diagnosis of COPD at risk (GOLD stage 0), even if FEV1.0/FVC was >70%.Citation21–Citation25 The following exclusion criteria were applied: a previous lung surgical procedure, exacerbation for at least 3 months prior to undergoing the 6MWT, inability to accurately perform the 6MWT, lung function test, and CT, and the use of long-term oxygen therapy. presents a flow diagram of subject enrollment. The study protocol was approved by the ethics committee of Kobe University (N287, Kobe, Japan). All subjects provided written or verbal informed consent.
Data collection
The following information was collected for each subject: age, sex, body mass index (BMI), modified Medical Research Council dyspnea score, and smoking history in pack-years. In addition, each subject performed the 6MWT and underwent a lung function test and a CT scan to assess the extent of emphysema and evaluate the PA:A ratio.
Six-minute walk test
The 6MWT was administered according to the American Thoracic Society (ATS) guidelines.Citation26 It was performed indoors on a flat square course with 25-m long sides, supervised by a physician and a physical therapist. Each subject was asked to walk as far as possible around the course in six minutes, during which the modified Borg scale was recorded each minute as a measure of dyspnea. Every two seconds, peripheral oxygen saturation (SpO2) and pulse rate were recorded using WristOx (model 3150; Nonin Medical, Plymouth, MN, USA); these data were analyzed by WristOx2 software (Star Product, Tokyo, Japan).
The DDR was calculated as the ratio of the desaturation area (DA) to the 6MWD. We used two versions of the DDR (DDR-original and DDR-simple) based on different ways of calculating DA as proposed in previous studies.Citation19,Citation20 For DDR-original, DA was obtained from the sum of the differences between 100% and the recorded SpO2 sampled every two seconds.Citation19 For DDR-simple, DA was obtained from the sum of the differences between 100% and the recorded SpO2 sampled once a minute.Citation20
Lung function test
The lung function test was performed according to the ATS guidelinesCitation27 and measured FVC, FEV1.0, and the diffusion capacity of the lung for carbon monoxide (DLCO). Each was expressed as percentages of the predicted values (%FVC, %FEV1.0, and %DLCO, respectively).
Extent of emphysema and PA:A ratio
CT was performed using Optima CT 660 Discovery (GE Healthcare, Little Chalfont, UK). Emphysema was identified by the percentage of low attenuation area (%LAA) across all lung fields.Citation28–Citation30 The Goddard Score was used as an index of the severity of emphysema.Citation31
Measurement of the PA:A ratio followed the method described in previous studies.Citation12,Citation13 The diameters of the PA and the aorta at the level of the bifurcation were measured on CT images. Because the diameter of the aorta was not uniform across different measurement points, two measurements were taken 90° apart, and the larger diameter was used in the analysis. The diameter of the PA was measured on the line joining the origin of the left PA to the center of the adjacent ascending aorta on the axial section. Enlargement of the PA was defined as PA:A ratio >1.Citation13
Statistical analysis
The statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan). p-values <0.05 were considered to be significant. Data are presented as counts, percentages, or medians with the range or interquartile range.
Cohen’s κ-coefficient was used to evaluate the intraobserver and interobserver reliability for detecting PA:A ratio >1. Spearman’s rank-correlation analysis was used to assess the relationship between study outcomes in the subjects and FEV1.0/FVC <70%. Receiver operating characteristic (ROC) curves were used to calculate the optimum cutoff values to predict %FEV1.0 <50% as an index of severe or very severe airway obstruction,Citation1 %DLCO <75% as an index of pulmonary diffusing capacity disorder,Citation3,Citation25 Goddard Score ≥8 as an index of moderate or severe emphysema,Citation31 and PA:A ratio >1 as an index of PH.Citation13 The optimum cutoff values were defined as the point on the ROC curve closest to the upper-left corner of the chart.
Results
The final analysis included 74 subjects (16 women and 58 men). presents the subjects’ characteristics. The median age was 73 (range 67–78) years, the median BMI was 22.0 (19.9–23.8) kg/m2, and the median %FEV1.0 was 63.6% (47.0%–76.1%), with 25 of the subjects having FEV1.0/FVC ≥70%. The κ-values for intraobserver and interobserver reliability for detecting PA:A ratio >1 were 0.75 (95% confidence interval [CI] 0.57–0.92) and 0.71 (95% CI 0.53–0.90), respectively.
Table 1 Characteristics of the subjects
presents the results of the linear correlation analysis. DDR-original and DDR-simple correlated significantly with %FEV1.0 (r=−0.312, p=0.006 and r=−0.317, p=0.006, respectively), %DLCO (r=−0.497, p<0.001 and r=−0.518, p<0.001, respectively), %LAA (r=0.381, p=0.001 and r=0.411, p<0.001, respectively), and PA:A ratio (r=0.553, p<0.001 and r=0.567, p<0.001, respectively). 6MWD correlated significantly with %DLCO (r=0.360, p=0.001) and PA:A ratio (r=−0.340, p=0.003). The lowest level of SpO2 correlated significantly with %DLCO (r=0.400, p<0.001), %LAA (r=−0.542, p<0.001), and PA:A ratio (r=−0.562, p<0.001). DDR-original and DDR-simple showed stronger correlations with %FEV1.0 for the subjects with FEV1.0/FVC <70% (r=−0.438, p=0.001and r=−0.455, p=0.001, respectively) than for all the subjects. 6MWD and lowest SpO2 both correlated significantly with %FEV1.0 for the subjects with FEV1.0/FVC <70% (r=0.313, p=0.043 and r=0.348, p=0.014, respectively).
Table 2 Linear correlations of the DDR and 6MWT outcomes with the factors of COPD
shows the results of the ROC analysis. DDR-original, DDR-simple, and lowest SpO2 all showed high accuracy (area under the ROC curve [AUC] >0.7) for predicting %FEV1.0 <50%, %DLCO <75%, Goddard Score ≥8, and PA:A ratio >1. The threshold values to predict %FEV1.0 <50% were determined for DDR-original (best cutoff point 4.0, AUC 0.73, 95% CI 0.62–0.85), DDR-simple (best cutoff point 0.14, AUC 0.74, 95% CI 0.63–0.85), and lowest SpO2 (best cutoff point 89, AUC 0.72, 95% CI 0.60–0.84). The threshold values to predict %DLCO <75% were determined for DDR-original (best cutoff point 2.7, AUC 0.78, 95% CI 0.64–0.91), DDR-simple (best cutoff point 0.09, AUC 0.79, 95% CI 0.66–0.93), and lowest SpO2 (best cutoff point 91, AUC 0.75, 95% CI 0.61–0.89). The threshold values to predict Goddard Score ≥8 were determined for DDR-original (best cutoff point 4.0, AUC 0.71, 95% CI 0.59–0.83), DDR-simple (best cutoff point 0.09, AUC 0.73, 95% CI 0.62–0.85), and lowest SpO2 (best cutoff point 90, AUC 0.79, 95% CI 0.68–0.89). The threshold values to predict PA:A ratio >1 were determined for DDR-original (best cutoff point 2.8, AUC 0.82, 95% CI 0.72–0.91), DDR-simple (best cutoff point 0.1, AUC 0.83, 95% CI 0.73–0.92), and lowest SpO2 (best cutoff point 89, AUC 0.86, 95% CI 0.77–0.95).
Table 3 The optimum cutoff and ROC curve parameters for the prediction of factors related to COPD
Discussion
We investigated the association among DDR, emphysema, and PH in stable COPD patients in this study. This study had two main findings. First, DDR showed to be correlated with emphysema and PH. Second, DDR-original and DDR-simple showed similar results in all the analyses. DDR may become an effective index to assess COPD with a high versatility because it can be calculated from the results of 6MWT used worldwide. Therefore, it was worth to find a new possibility of DDR in this study.
DDR was first proposed in 2010 as a new index for the assessment of interstitial lung diseases,Citation19 with the simple version of DDR proposed in 2014 as an index for the assessment of the exercise capacity of COPD patients.Citation20 These previous studies investigated the associations between DDR and %FEV1.0 or %DLCO but not associations between DDR and the indexes of emphysema and PH.Citation19,Citation20 The present study demonstrated the further usefulness of DDR as an indicator of emphysema or PH in COPD patients. Unlike the individual outcomes of the 6MWT (6MWD and SpO2), DDR was related significantly with all of the parameters associated with COPD (%FEV1.0, %DLCO, %LAA, and PA:A ratio); DDR also demonstrated a strong ability to predict %FEV1.0 <50%, %DLCO <75%, Goddard Score ≥8, and PA:A ratio >1. DDR could, therefore, become a useful index that reflects the degree of not only airflow obstruction and pulmonary diffusing capacity disorder but also emphysema and PH, superior to both 6MWD and the lowest SpO2 individually.
Emphysema is a disorder that involves the destruction of alveoli caused by a decline in alveolar surface area and the elasticity of the lung.Citation32,Citation33 The destruction of alveoli progresses before symptoms appear or the lung function declines.Citation34 Emphysema affects the patient’s quality of life and is associated with exacerbations and deteriorating pulmonary function in subjects without airflow obstruction, even when the degree of emphysema is mild.Citation7 It has been reported that PH can be caused by the combined results of hypoxia, inflammation, and capillary loss in emphysemaCitation35 and that there was an association of PH with exercise capacity and mortality in COPD patients.Citation36,Citation37 The early diagnosis of emphysema and PH is of great importance for COPD patients; however, it is not possible in practice to use CT or RHC for all patients or preliminary groups of COPD patients for the diagnosis of emphysema and PH. 6MWD and SpO2 can be measured noninvasively and easily, and it has been reported that 6MWD and EID were each related to emphysema and PH.Citation15–Citation18 DDR, an index derived from combining 6MWD and EID, was shown in this study to be associated with %LAA and PA:A ratio. Thus, it is suggested that DDR could become a useful index that indicates the extent of a patient’s emphysema and PH.
Both 6MWD and lowest SpO2, which are widely used as indexes of COPD conditions, showed significant correlations with %DLCO, but neither showed a significant correlation with %FEV1.0. This contrasted with previous studies, which demonstrated associations between 6MWD or lowest SpO2 and %FEV1.0.Citation15,Citation20 It is speculated that these results may have been due to including subjects without airflow obstruction in the analysis. As evidence for this, 6MWD and lowest SpO2 showed significant correlations with %FEV1.0 when only subjects with substantial airflow obstruction, indicated by FEV1.0/FVC <70%, were included in the analysis. It has been reported that spirometry used to measure %FEV1.0 underdiagnosed mild or early-stage COPD.Citation38 Conversely, low DLCO was observed in ex-smokers without airflow obstruction, and DLCO has been known to be a sensitive index of early-stage COPD.Citation3,Citation39 In the present study, DDR showed significant correlations with both %FEV1.0 and %DLCO even when subjects without substantial airflow obstruction were included in the analysis. It is therefore suggested that DDR is superior to either 6MWD or lowest SpO2 individually in indicating COPD conditions, regardless of the degree of airflow obstruction.
Finally, the results for DDR-original and DDR-simple were similar in all the analyses. This suggests that DDR-simple is not inferior to DDR-original in screening COPD conditions. DDR-original requires a special device to record SpO2 continuously and analyze DA, whereas DDR-simple can be calculated using a conventional device such as a normal pulse oximeter. This makes DDR useful for the assessment of COPD patients in any situation, such as cases receiving medical treatment at home or at facilities other than hospitals, without the need for special devices.
This study had some limitations. First, it was a retrospective study at a single center, and the sample size was small. The influence of sex was not examined in this study, even though it has been reported that smoking affects women to a greater extent than men. Second, echocardiography was not performed for all the subjects, and medical history information regarding left ventricular dysfunction was not included in this study even though left ventricular dysfunction causes PA enlargement. These findings should be further inspected by a larger, ideal, multicenter, and prospective clinical trial that would take electrocardiography and ventricular function into consideration.
Conclusion
The results of this study suggested that DDR could be a useful index for the assessment of COPD patients. The 6MWT is an easy and low-cost method for the assessment of exercise capacity in these patients. DDR demonstrated a better ability than the other 6MWT measures to predict %FEV1.0 <50%, %DLCO <75%, Goddard Score ≥8, and PA:A ratio >1, so its use could help with the early diagnosis of COPD.
Author contributions
Yukari Fujimoto involved in the conception and design of the study, acquisition of data, analysis and interpretation of data, and drafting the article. Yutaro Oki, Masahiro Kaneko, and Akira Ishikawa involved in the conception and design of the study, acquisition of data, analysis and interpretation of data, and revising the article. Hideki Sakai and Shogo Misu involved in the acquisition of data and revising the article. Takumi Yamaguchi, Yuji Mitani, and Hisafumi Yasuda involved in the conception and design of the study, interpretation of data, and revising the article. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
The authors would like to thank the members of the Department of Rehabilitation, Kobe City Medical Center West Hospital, including Akihiro Honda, Chisato Nagatani, Takashi Kadooka, Shoko Mitani, Haruko Yamamoto, and Kumi Takamori for cooperation in acquisition of data, and the members of the Department of Community Health Sciences, Kobe University Graduate School of Health Sciences, including Akio Yamamoto, Kazuki Takahashi, Shigefumi Murakami, Kaoru Hanaie, Kentaro Iwata, Yoji Yamada, Yu Watanabe, Takuya Sawada, Kanji Yamada, Yusuke Iwata, Ken Umehara, and Keita Ohashi for constructive comments on this paper. The authors also thank Enago (Tokyo, Japan) for text correction.
Disclosure
The authors report no conflicts of interest in this work.
References
- RabeKFHurdSAnzuetoAGlobal Initiative for Chronic Obstructive Lung DiseaseGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med2007176653255517507545
- PauwelsRARabeKFBurden and clinical features of chronic obstructive pulmonary disease (COPD)Lancet2004364943461362015313363
- KirbyMOwrangiASvenningsenSOn the role of abnormal DL(CO) in ex-smokers without airflow limitation: symptoms, exercise capacity and hyperpolarised helium-3 MRIThorax201368875275923604381
- de TorresJPBastarrikaGWisniveskyJPAssessing the relationship between lung cancer risk and emphysema detected on low-dose CT of the chestChest200713261932193818079226
- WilsonDOWeissfeldJLBalkanAAssociation of radiographic emphysema and airflow obstruction with lung cancerAm J Respir Crit Care Med2008178773874418565949
- MadaniAZanenJde MaertelaerVGevenoisPAPulmonary emphysema: objective quantification at multi-detector row CT – comparison with macroscopic and microscopic morphometryRadiology200623831036104316424242
- AlcaideABSanchez-SalcedoPBastarrikaGClinical features of smokers with radiological emphysema but without airway limitationChest2017151235836527818328
- BarberàJAMechanisms of development of chronic obstructive pulmonary disease-associated pulmonary hypertensionPulm Circ20133116016423662194
- WellsJMDransfieldMTPathophysiology and clinical implications of pulmonary arterial enlargement in COPDInt J Chron Obstruct Pulmon Dis2013850952124235822
- SchulmanLLLennonPFWoodJAEnsonYPulmonary vascular resistance in emphysemaChest199410537988058131543
- McLaughlinVVArcherSLBadeschDBACCF/AHAACCF/AHA 2009 expert consensus document on pulmonary hypertension: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association: developed in collaboration with the American College of Chest Physicians, American Thoracic Society, Inc., and the Pulmonary Hypertension AssociationCirculation2009119162250229419332472
- WellsJMWashkoGRHanMKCOPDGene InvestigatorsECLIPSE Study InvestigatorsPulmonary arterial enlargement and acute exacerbations of COPDN Engl J Med20123671091392122938715
- IyerASWellsJMVishinSBhattSPWilleKMDransfieldMTCT scan-measured pulmonary artery to aorta ratio and echocardiography for detecting pulmonary hypertension in severe COPDChest2014145482483224114440
- SciurbaFCrinerGJLeeSMNational Emphysema Treatment Trial Research GroupSix-minute walk distance in chronic obstructive pulmonary disease: reproducibility and effect of walking course layout and lengthAm J Respir Crit Care Med2003167111522152712615634
- AndrianopoulosVCelliBRFranssenFMDeterminants of exercise-induced oxygen desaturation including pulmonary emphysema in COPD: results from the ECLIPSE studyRespir Med2016119879527692154
- BodduluriSBhattSPHoffmanEACOPDGene InvestigatorsBiomechanical CT metrics are associated with patient outcomes in COPDThorax201772540941428044005
- NakaharaYTaniguchiHKimuraTExercise hypoxaemia as a predictor of pulmonary hypertension in COPD patients without severe resting hypoxaemiaRespirology201722112012527471142
- OkiYKanekoMFujimotoYUsefulness of the 6-minute walk test as a screening test for pulmonary arterial enlargement in COPDInt J Chron Obstruct Pulmon Dis2016112869287527920514
- PimentaSPRochaRBBaldiBGKawassaki AdeMKairallaRACarvalhoCRDesaturation – distance ratio: a new concept for a functional assessment of interstitial lung diseasesClinics (Sao Paulo)201065984184621049210
- IjiriNKanazawaHYoshikawaTHirataKApplication of a new parameter in the 6-minute walk test for manifold analysis of exercise capacity in patients with COPDInt J Chron Obstruct Pulmon Dis201491235124025395845
- PaulinLMDietteGBBlancPDSPIROMICS Research GroupOccupational exposures are associated with worse morbidity in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2015191555756525562375
- ReganEALynchDACurran-EverettDGenetic Epidemiology of COPD (COPDGene) InvestigatorsClinical and radiologic disease in smokers with normal spirometryJAMA Intern Med201517591539154926098755
- HarveyBGStrulovici-BarelYKanerRJRisk of COPD with obstruction in active smokers with normal spirometry and reduced diffusion capacityEur Respir J20154661589159726541521
- LutchmedialSMCreedWGMooreAJWalshRRGentchosGEKaminskyDAHow common is airflow limitation in patients with emphysema on CT scan of the chest?Chest2015148117618425539080
- PellegrinoRViegiGBrusascoVInterpretative strategies for lung function testsEur Respir J200526594896816264058
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function LaboratoriesATS statement: guidelines for the six-minute walk testAm J Respir Crit Care Med2002166111111712091180
- MillerMRHankinsonJBrusascoVATS/ERS Task ForceStandardisation of spirometryEur Respir J200526231933816055882
- MüllerNLStaplesCAMillerRRAbboudRT“Density mask”. An objective method to quantitate emphysema using computed tomographyChest19889447827873168574
- MadaniAVan MuylemAGevenoisPAPulmonary emphysema: effect of lung volume on objective quantification at thin-section CTRadiology2010257126026820663967
- BankierAADe MaertelaerVKeyzerCGevenoisPAPulmonary emphysema: subjective visual grading versus objective quantification with macroscopic morphometry and thin-section CT densitometryRadiology1999211385185810352615
- GoddardPRNicholsonEMLaszloGWattIComputed tomography in pulmonary emphysemaClin Radiol19823343793877083738
- ThurlbeckWMInternal surface area and other measurements in emphysemaThorax19672264834965624577
- FinucaneKEColebatchHJElastic behavior of the lung in patients with airway obstructionJ Appl Physiol19692633303385773176
- PrattPCKilburnKHA modern concept of the emphysemas based on correlations of structure and functionHum Pathol1970134434634940289
- ChaouatANaeijeRWeitzenblumEPulmonary hypertension in COPDEur Respir J20083251371138518978137
- SimsMWMargolisDJLocalioARPanettieriRAKawutSMChristieJDImpact of pulmonary artery pressure on exercise function in severe COPDChest2009136241241919318664
- CutticaMJKalhanRShlobinOACategorization and impact of pulmonary hypertension in patients with advanced COPDRespir Med2010104121877188220547449
- ShahabLJarvisMJBrittonJWestRPrevalence, diagnosis and relation to tobacco dependence of chronic obstructive pulmonary disease in a nationally representative population sampleThorax200661121043104717040932
- KleinJSGamsuGWebbWRGoldenJAMüllerNLHigh-resolution CT diagnosis of emphysema in symptomatic patients with normal chest radiographs and isolated low diffusing capacityRadiology199218238178211535900