Abstract
Purpose
The aim of this study was to investigate the comparative risks of budesonide/formoterol, versus placebo or monotherapies, for the treatment of patients with stable COPD.
Materials and methods
We undertook a systematic search of the literature in PubMed, Embase, and the Cochrane Central Register of Controlled Trials, for randomized controlled trials (RCTs) comparing budesonide/formoterol with control regimens for the treatment of patients with stable COPD and at least 12 weeks of follow-up, meeting the inclusion criteria. Studies were reviewed, and OR with corresponding 95% CI was used to pool the results.
Results
A total of eight studies involving 9,254 patients met the inclusion criteria of this meta-analysis. Compared with placebo, combination therapy with budesonide/formoterol was associated with a significantly higher risk of adverse effects including oral candidiasis (OR: 3.09, 95% CI: 1.95–4.91) and dysphonia (OR: 2.76, 95% CI: 1.40–5.44), but not pneumonia (OR: 0.94, 95% CI: 0.64–1.37) or bronchitis (OR: 1.36, 95% CI: 0.95–1.95). A similar pattern was also evident for the comparison of formoterol with budesonide/formoterol, with increased occurrence of oral candidiasis (OR: 2.72, 95% CI: 1.33–5.58) and dysphonia (OR: 4.13, 95% CI: 1.95–8.76); however, there were no significant differences in pneumonia (OR: 1.31, 95% CI: 0.98–1.74) or bronchitis (OR: 1.05, 95% CI: 0.83–1.31). In contrast, compared with budesonide, combined budesonide/formoterol was associated with similar risks of adverse effects, including pneumonia (OR: 1.20, 95% CI: 0.60–2.39), bronchitis (OR: 0.95, 95% CI: 0.41–2.20), oral candidiasis (OR: 0.79, 95% CI: 0.41–1.53), and dysphonia (OR: 1.00, 95% CI: 0.40–2.47).
Conclusion
Combination therapy does not cause more adverse events, including pneumonia and bronchitis, than control (placebo, formoterol, or budesonide) treatment in patients with stable COPD, while there were higher risks of oral candidiasis and dysphonia compared with the non-inhaled corticosteroid group (placebo, formoterol).
Introduction
COPD is a preventable and treatable disease, which is characterized by persistent respiratory symptoms and airflow limitation, and is a leading prevalent and public health issue associated with enormous social and economic burdens.Citation1–Citation5 Inhaled corticosteroids (ICSs), combined with long-acting β2 adrenoceptor agonists (LABAs), are a widely recommended treatment for patients with COPD who have a history of exacerbations.Citation6 Compared with placebo and/or monotherapies, ICS/LABA therapy is effective in reducing COPD flare-ups, improving health-related quality of life, and decreasing the incidence of, and mortality associated with, adverse events.Citation7–Citation10 Furthermore, ICS/LABA, which is not a combination bronchodilator therapy like an LABA/long-acting muscarinic antagonist (LAMA), is associated with increased adverse events such as oral candidiasis and pneumonia,Citation11–Citation13 while compared with ICS alone, the risk of pneumonia is similar.Citation14 Nevertheless, there have been many striking studies providing evidence of increased risks associated with ICS. Mapel et alCitation15 designed a nested case–control analysis, using data derived from three large regional managed-care organizations in the United States; the report found that there were similar risks among COPD patients using fluticasone propionate alone or in combination with salmeterol.
There are three brands of ICS/LABA combination agents available for the current clinical application: budesonide/for-moterol, fluticasone propionate/salmeterol, and mometasone furoate/formoterol. Studies to determine whether the use of ICS increases the risk of pneumonia that are cited in the guidelines for its use are primarily focused on the randomized controlled trials (RCTs) of fluticasone. It is unknown whether budesonide/formoterol increases the risk of pneumonia or the risk of other ICS-related adverse events (bronchitis, oral candidiasis, and dysphonia). The combination of budesonide and formoterol, containing fixed doses of ICS and LABA, was approved as a mainstay drug therapy for patients with COPD in Europe in 2003 and subsequently in the United States in 2009 and shows remarkable clinical efficacy for the treatment of COPD. Previous studies have primarily focused on western populations, reporting that budesonide/formoterol provided benefits, in terms of improving pulmonary function, COPD symptoms, and health-related quality of life, and reduced flare-up rate in COPD patients and that it was generally well tolerated.Citation16–Citation20
The budesonide/formoterol combination exhibits a similar pattern of undesirable effects to its individual components; however, the results regarding the budesonide-related risk of pneumonia are more controversial. Ferguson et alCitation21 suggested that, compared with the formoterol group (pneumonia, 1.0%), there was a lower rate of adverse events in the budesonide/formoterol group (pneumonia, 0.5%). In contrast, Sharafkhaneh et alCitation16 found that the incidence of pneumonia in the combination therapy group (6.4%) was higher than that in the formoterol-alone group (2.7%). Two other studies reported similar rates of pneumonia for the two treatment regimens.Citation17,Citation20
The aim of this meta-analysis was to evaluate the current evidence regarding the risks of pneumonia, and other ICS-related adverse effects, associated with the systematic use of budesonide/formoterol in patients with stable COPD.
Materials and methods
Search strategy
Two reviewers independently and comprehensively searched the Cochrane Central Register, PubMed, and Embase for RCTs from inception to August 31, 2018, using the following terms: (“budesonide” or “formoterol” or “Pulmicort” or “BD 40A” or “Foradil” or “Inhaled corticosteroids” or “long-acting β2 adrenoceptor agonists”) and (“COPD” or “chronic obstructive pulmonary disease”) AND (“randomized controlled trial” or “RCT” or “clinical trial”). The search had no language restrictions and included unpublished studies. To avoid duplication, we only included latest or most complete clinical trial reports. To identify additional publications, we manually searched for reviews in the reference lists of collected papers and retrieved all relevant, or potentially relevant, publications.
Eligibility criteria and exclusion criteria
We used the following criteria to select studies for inclusion in this meta-analysis: 1) methodological criteria: randomized, double-blind, parallel-group design, for at least 12 weeks; 2) study population: recruited patients with stable COPD, consistent with the GOLD 2018 criteria; 3) interventions: inhaled budesonide/formoterol as the intervention drug, compared with placebo or budesonide or formoterol; 4) outcome measures: the ICS-related adverse effects analyzed in this meta-analysis were as follows: pneumonia, bronchitis, oral candidiasis, and dysphonia. The following studies were excluded: repetitive articles, interventions that did not meet inclusion criteria, studies that were not RCTs, studies with unavailable baseline characteristics, not studies of intervention of interest, and studies with insufficient data on the outcome of interest.
Data extraction
Two independent investigators reviewed the articles and extracted the data. If there were any disagreements regarding the relevance of articles, they were resolved by consensus. For each publication, the following information was extracted: the last name of the first author, year of publication, research design, participant number, target population, basic characteristics, treatment arms (dose of budesonide/formoterol and duration of treatment), duration of COPD, and adverse effects data. In some cases, we extracted information from graphs and charts.
Quality assessment
The quality of included studies was independently evaluated by two reviewers, in accordance with the modified 7-point Jadad scale, using the risk assessment of bias tool from the Cochrane Collaboration’s tool,Citation22 regarding the following four aspects: 1) methods for generating random series (0–2 points); 2) randomization concealment (0–2 points); 3) blind method (0–2 points); 4) assessment of withdrawal (0–1 points).
Data synthesis
Stata SE version 14.0 (StataCorp LP, College Station, TX, USA) was used to perform all statistical analyses. For each study, the OR and corresponding 95% CI values were used to pool dichotomous variable. The statistical heterogeneity of data included in this meta-analysis was assessed using chi-square Q and I2 statistics. Results were pooled using a fixed-effect model if p>0.1 or I2<50%, respectively, indicating no substantial heterogeneity; otherwise, a random-effect model was employed. We estimated each of the safety parameters for each control group (placebo, formoterol, and budesonide). When there was an adequate number of RCTs included for evaluation of a clinical outcome parameter, funnel plots and Begg’s test were employed to assess publication bias.Citation23
Results
Search results and study descriptions
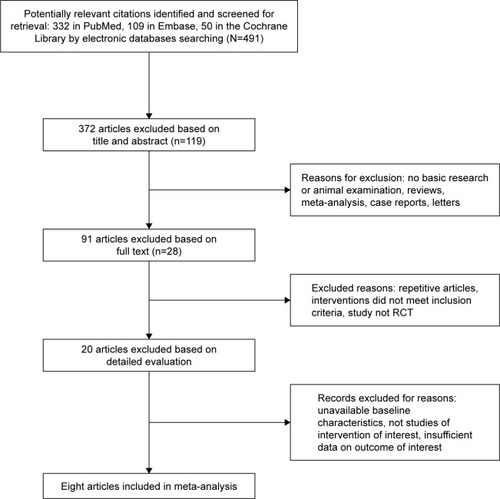
A flowchart outlining the study’s screening process is presented in . Initially, 491 published articles were found in databases and by manual searches. Finally, only eight articles, with 21 treatment arms, including 9,254 participants, were selected based on the inclusion/exclusion criteria.Citation16–Citation21,Citation24,Citation25 The detailed characteristics of studies included in this meta-analysis are summarized in . No significant differences in baseline information were detected between experimental and control arms. Each trial was multicenter, blinded, parallel, and controlled and scored ≥5 on the Jadad scale.
Table 1 Basic characteristics of the studies included in the meta-analysis
Clinical outcomes and results synthesis
Budesonide/formoterol versus placebo alone
Pneumonia
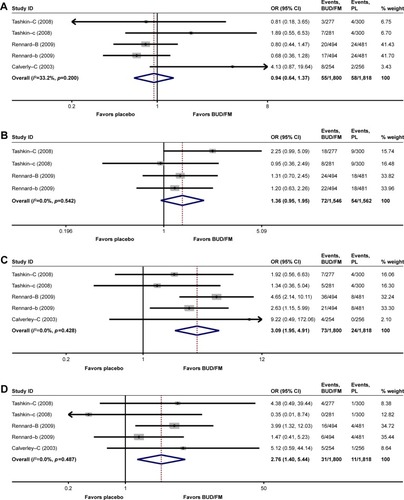
Five treatment arms (budesonide/formoterol group: n=1,800, placebo group: n=1,818) of the eligible studies provided pneumonia data for statistical analysis. Compared with the placebo-alone group, combination bronchodilator treatment showed no significant difference in terms of this adverse event (OR: 0.94, 95% CI: 0.64–1.37; I2=33.2%; p=0.200; ).
Figure 2 Forest plot of pneumonia, bronchitis, oral candidiasis, and dysphonia comparison. (A) Pneumonia in BUD/FM versus placebo. (B) Bronchitis in BUD/FM versus placebo. (C) Oral candidiasis in BUD/FM versus placebo. (D) Dysphonia in BUD/FM versus placebo.
Bronchitis
Four treatment arms (budesonide/formoterol group: n=1,546, placebo group: n=1,562) provided bronchitis adverse event data. According to pooled estimates, compared with the placebo group, the combined drug group demonstrated a higher risk of bronchitis; however, the difference was not statistically significant (OR: 1.36, 95% CI: 0.95–1.95; I2=0.0%; p=0.524; ).
Oral candidiasis
Five treatment arms (budesonide/formoterol group: n=1,800, placebo group: n=1,818) contained oral candidiasis data. According to pooled analysis, combined treatment resulted in significantly higher odds versus placebo alone (OR: 3.09, 95% CI: 1.95–4.71; I2=0.0%; p=0.428; ).
Dysphonia
The five treatment arms (budesonide/formoterol group: n=1,800, placebo group: n=1,818) that reported dysphonia identified a significant higher risk with combined treatment than placebo alone (OR: 2.76, 95% CI: 1.40–5.44; I2=0.0%; p=0.487; ).
Budesonide/formoterol versus formoterol alone
Pneumonia
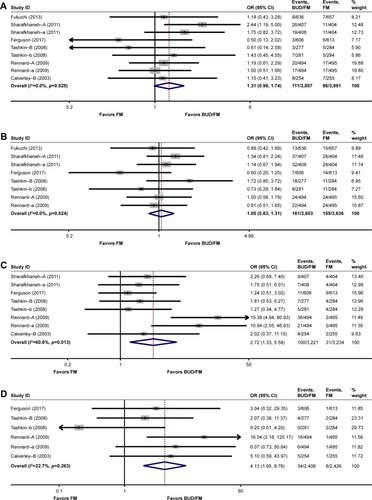
Pneumonia data were provided from nine treatment arms (budesonide/formoterol group: n=3,857, formoterol group: n=3,891). The rate of pneumonia was higher with budesonide/formoterol than with formoterol; however, the difference was well below that required for minimum clinical importance (OR: 1.31, 95% CI: 0.98–1.74; I2=0.0%; p=0.525; ).
Figure 3 Forest plot of pneumonia, bronchitis, oral candidiasis, and dysphonia comparison. (A) Pneumonia in BUD/FM versus FM. (B) Bronchitis in BUD/FM versus FM. (C) Oral candidiasis versus FM. (D) Dysphonia in BUD/FM versus FM.
Abbreviations: BUD, budesonide; FM, formoterol.
Bronchitis
Eight treatment arms (budesonide/formoterol group: n=3,603, formoterol group: n=3,636) reported this clinical safety parameter. Pooled analysis showed that the incidence of bronchitis as an adverse effect was similar for the combination treatment and formoterol groups (OR: 1.05, 95% CI: 0.83–1.31; I2=0.0%; p=0.524; ).
Oral candidiasis
Data on this adverse event were included from eight treatment arms (budesonide/formoterol group: n=3,221, formoterol group: n=3,234). Pooled analysis showed that the rate of oral candidiasis was significantly higher in the combination treatment group than the formoterol-alone group (OR: 2.72, 95% CI: 1.35–5.58; I2=60.6%; p=0.013; ).
Dysphonia
Data regarding dysphonia were included from six treatment arms (budesonide/formoterol group: n=2,406, formoterol group: n=2,426), and pooled analysis showed that the risk was significantly higher in the combined treatment group than in the control group (OR: 4.13, 95% CI: 1.95–8.76; I2=22.7%; p=0.263; ).
Budesonide/formoterol versus budesonide alone
Pneumonia
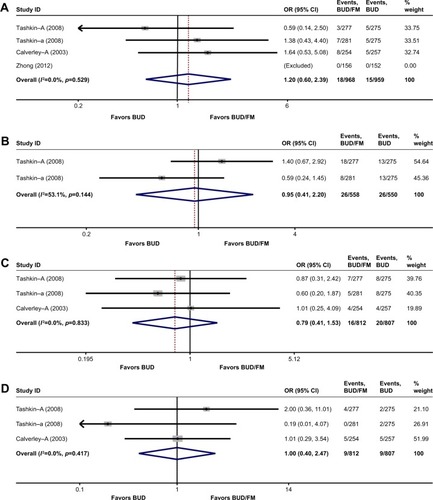
A total of four treatment arms (budesonide/formoterol group: n=968, budesonide group: n=959) reported pneumonia. The risk of pneumonia in the budesonide/formoterol group was not significantly higher than that in the budesonide-alone group (OR: 1.20, 95% CI: 0.60–2.39, I2=0.0%, p=0.529; ).
Figure 4 Forest plot of pneumonia, bronchitis, oral candidiasis, and dysphonia comparison. (A) Pneumonia in BUD/FM versus BUD. (B) Bronchitis in BUD/FM versus BUD. (C) Oral candidiasis in BUD/FM versus BUD. (D) Dysphonia in BUD/FM versus BUD.
Abbreviations: BUD, budesonide; FM, formoterol.
Bronchitis
Two treatment arms (budesonide/formoterol group: n=558, budesonide group: n=550) in the report of Tashkin et alCitation20 reported the risk of bronchitis; no difference was observed between the budesonide/formoterol combination and budesonide-alone arms (OR: 0.95, 95% CI: 0.41–2.20, I2=53.1%, p=0.144; ).
Oral candidiasis
Pooling data from three treatment arms (budesonide/formoterol group: n=812, budesonide group: n=807) showed that the risk of oral candidiasis with budesonide/formoterol was similar to that with budesonide alone (OR: 0.79, 95% CI: 0.41–1.53, I2=0.0%, p=0.833; ).
Dysphonia
Three treatment arms (budesonide/formoterol group: n=812, budesonide group: n=807) used dysphonia to assess risk outcomes. Similar adverse rates were observed between combination therapy and budesonide regimens (OR: 1.00, 95% CI: 0.40–2.47, I2=0.0%, p=0.417; ).
Publication bias
Since there were too few trials available to make a meaningful assessment, no evaluation of the data for publication bias was conducted.
Discussion
Meta-analysis was performed by pooled analysis of data from RCTs to compare the risk of budesonide/formoterol with placebo or monotherapies in patients with stable COPD. The present study, comprising 9,254 patients, demonstrates that, as expected, there are significantly higher risks of local side effects (such as oral candidiasis and dysphonia) with combination treatment than with comparators (placebo or formoterol); nevertheless, no significant differences in adverse events (pneumonia and bronchitis) were noted between budesonide/formoterol and non-ICS (placebo or formoterol) arms. In contrast, compared with budesonide, budesonide/formoterol combination treatment did not contribute to significant risks of pneumonia, bronchitis, oral candidiasis, or dysphonia.
According to previous studies, the safety profile of budesonide/formoterol is similar to that of monotherapies, and no improvement in adverse events is observed by the administration of the combined drug. The results of our study are consistent with those of Nannini et al,Citation26 comparing the ICS/LABA combination with ICS alone, which found that the risk of pneumonia was similar between these two groups. The only described ICS-related adverse event was pneumonia. In contrast, our meta-analysis included more ICS-related parameters (pneumonia, bronchitis, oral candidiasis, and dysphonia) that can better indicate the safety of budesonide/formoterol relative to controls (placebo, formoterol, or budesonide) for the treatment of patients with stable COPD.
Traditionally, because ICS has good anti-inflammatory effect, it has been used as a mainstay drug for the treatment of patients with COPD. Nevertheless, it has various side effects, including the inhibition of host resistance; increasing the incidence of pneumonia, tuberculosis, and oropharyngeal candidiasis; and causing muscle lesions, leading to dysphonia. Our results differ from those of Nannini et al,Citation27,Citation28 which showed an increased risk of pneumonia in patients with COPD receiving any dose of any type of ICS/LABA, compared with the control arm (LABA or placebo). Crim et alCitation12 found that, compared with vilanterol, combined fluticasone furoate and vilanterol significantly increased pneumonia risk. Halpin et alCitation29 observed that budesonide/formoterol was associated with a lower risk of pneumonia than fluticasone/salmeterol when used to treat patients with COPD. Although the exact reasons for the inconsistency of these findings are unclear, they may be related to the following factors. First, compared with fluticasone propionate, budesonide has a higher dissolution rate in lungsCitation30 and increased airway epithelial absorptionCitation31 and leads to increased local immune effectsCitation32 and reduced immunosuppressive efficacy.Citation33 Second, the COPD patients (ABCD classification) included in the study influence the study results; group D (higher acute exacerbation risk/more clinical symptoms) patients taking ICS (with or without LABA) have a greater risk of developing pneumonia.Citation12,Citation13
Budesonide/formoterol is taken twice daily, via a pressurized metered-dose inhaler, and is considered easy to use; therefore, it has become the primary choice for most patients.Citation17,Citation20,Citation24 This treatment is not only economic and effective for patients with symptomatic COPD,Citation34 but a preferable option, based on weighing the benefits and risks of ICS/LABA for the treatment of COPD.
Additional larger, more suitable similar RCTs are needed to evaluate the clinical safety outcomes of budesonide/formoterol more reliably and comprehensively in the future. These studies should be specifically designed to detect ICS-related adverse effects of combined budesonide/formoterol combination.
Limitations
The systematic evaluation approach used for our study has several limitations. To produce reliable results, we identified strict eligibility standards ahead of this meta-analysis, incorporating only RCTs that clearly indicated the inclusion of patients with stable COPD. This meta-analysis was based on a comprehensive and systematic search of medical databases by two independent reviewers, followed by extraction, analysis, and evaluation of the quality of included studies, supervised by third-party assessor. The number of trials available was relatively small, and the total number of participants was also insufficient; hence, the results should be interpreted with a degree of caution. Consequently, we could not perform a subgroup analysis of variables such as drug dose, treatment time, duration of COPD, and sex. The subjects involved in the meta-analysis were mainly Asians and patients from western countries; none of the trials originally recruited Africans. Therefore, the results of this meta-analysis may be of limited suitability for application to the treatment of patients with COPD in the clinic. Finally, none of the included RCTs provided definite clinical, radiological, or microbiological criteria for all adverse events, and none were designed to assess ICS-related adverse effects.
Conclusion
This present meta-analysis provides a useful and comprehensive assessment of the ICS-related risks of budesonide/formoterol in patients with stable COPD. Although the study is not novel, it is of clinical importance, and the results could be used for reference in clinic. Compared with the no-ICS (placebo or formoterol) group, budesonide/formoterol significantly increased ICS-related risks of oral candidiasis and dysphonia, but not pneumonia and bronchitis. There were no significant differences in potential side effects (pneumonia, bronchitis, oral candidiasis, and dysphonia) between patients treated with budesonide/formoterol and budesonide alone. Future robust studies, including larger, long-term RCTs, are warranted to assess the risk of budesonide/formoterol in patients with stable COPD.
Acknowledgments
This work was supported by the Jiangxi Province Science and Technology Support Plan (grant number: 20141BBG70045).
Disclosure
The authors report no conflicts of interest in this work.
References
- LozanoRNaghaviMForemanKGlobal and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010Lancet201230898592095212810.1016/S0140-6736(12)61728-0
- SullivanSDRamseySDLeeTAThe economic burden of COPDChest2000117Suppl 2S5S910.1378/chest.117.2_suppl.5S
- LopezADShibuyaKRaoCChronic obstructive pulmonary disease: current burden and future projectionsEur Respir J200627239741210.1183/09031936.06.0002580516452599
- MathersCDLoncarDProjections of global mortality and burden of disease from 2002 to 2030PLoS Med2006311e44210.1371/journal.pmed.003044217132052
- VosTFlaxmanADNaghaviMYears lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010Lancet201238098592163219610.1016/S0140-6736(12)61729-223245607
- Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD)2018 Available from: http://www.goldcopd.orgAccessed November 15, 2017
- AnzuetoAFergusonGTFeldmanGEffect of fluticasone propionate/salmeterol (250/50) on COPD exacerbations and impact on patient outcomesCOPD20096532032919863361
- CalverleyPMAndersonJACelliBSalmeterol and fluticasone propionate and survival in chronic obstructive pulmonary diseaseN Engl J Med2007356877578910.1056/NEJMoa06307017314337
- FergusonGTAnzuetoAFeiREmmettAKnobilKKalbergCEffect of fluticasone propionate/salmeterol (250/50 microg) or salmeterol (50 microg) on COPD exacerbationsRespir Med200810281099110810.1016/j.rmed.2008.04.01918614347
- JenkinsCRJonesPWCalverleyPMEfficacy of salmeterol/fluticasone propionate by GOLD stage of chronic obstructive pulmonary disease: analysis from the randomised, placebo-controlled TORCH studyRespir Res20091015910.1186/1465-9921-10-3119566934
- YangIAClarkeMSSimEHFongKMInhaled corticosteroids for stable chronic obstructive pulmonary diseaseCochrane Database of Syst Rev20127CD002991
- CrimCDransfieldMTBourbeauJPneumonia risk with inhaled fluticasone furoate and vilanterol compared with vilanterol alone in patients with COPDAnn Am Thorac Soc2015121273410.1513/AnnalsATS.201409-413OC25490706
- VogelmeierCHedererBGlaabTTiotropium versus salmeterol for the prevention of exacerbations of COPDN Engl J Med2011364121093110310.1056/NEJMoa100837821428765
- VestboJAndersonJABrookRDFluticasone furoate and vilanterol and survival in chronic obstructive pulmonary disease with heightened cardiovascular risk (SUMMIT): a double-blind randomised controlled trialLancet2016387100301817182610.1016/S0140-6736(16)30069-127203508
- MapelDSchumMYoodMBrownJMillerDDavisKPneumonia among COPD patients using inhaled corticosteroids and long-acting bronchodilatorsPrim Care Respir J201019210911710.4104/pcrj.2009.0007220082059
- SharafkhanehASouthardJGGoldmanMUryniakTMartinUJEffect of budesonide/formoterol pMDI on COPD exacerbations: a double-blind, randomized studyRespir Med2012106225726810.1016/j.rmed.2011.07.02022033040
- RennardSITashkinDPMcElhattanJEfficacy and tolerability of budesonide/formoterol in one hydrofluoroalkane pressurized metered-dose inhaler in patients with chronic obstructive pulmonary disease: results from a 1-year randomized controlled clinical trialDrugs200969554956510.2165/00003495-200969050-0000419368417
- CalverleyPMBoonsawatWCsekeZZhongNPetersonSOlssonHMaintenance therapy with budesonide and formoterol in chronic obstructive pulmonary diseaseEur Respir J200322691291914680078
- SzafranskiWCukierARamirezAEfficacy and safety of budesonide/formoterol in the management of chronic obstructive pulmonary diseaseEur Respir J2003211748112570112
- TashkinDPRennardSIMartinPEfficacy and safety of budesonide and formoterol in one pressurized metered-dose inhaler in patients with moderate to very severe chronic obstructive pulmonary disease: results of a 6-month randomized clinical trialDrugs200868141975200010.2165/00003495-200868140-0000418778120
- FergusonGTTashkinDPSkärbyTEffect of budesonide/formoterol pressurized metered-dose inhaler on exacerbations versus formoterol in chronic obstructive pulmonary disease: the 6-month, randomized RISE (Revealing the Impact of Symbicort in reducing Exacerbations in COPD) studyRespir Med2017132314110.1016/j.rmed.2017.09.00229229103
- HigginsJPTGreenSCochrane Handbook for Systematic Reviews of Interventions Version 510 The Cochrane CollaborationNew YorkWiley2014 [updated 2011]. Available from: http://handbook.cochrane.orgAccessed August 16, 2014
- BeggCBMazumdarMOperating characteristics of a rank correlation test for publication biasBiometrics1994504108811017786990
- ZhongNZhengJWenFEfficacy and safety of budesonide/formoterol via a dry powder inhaler in Chinese patients with chronic obstructive pulmonary diseaseCurr Med Res Opin201228225726510.1185/03007995.2011.63642022046961
- FukuchiYSamoroRFassakhovRBudesonide/formoterol via Turbuhaler® versus formoterol via Turbuhaler® in patients with moderate to severe chronic obstructive pulmonary disease: phase III multinational study resultsRespirology201318586687310.1111/resp.1209023551359
- NanniniLJPoolePMilanSJKestertonACombined corticosteroid and long-acting beta2-agonist in one inhaler versus inhaled corticosteroids alone for chronic obstructive pulmonary diseaseCochrane Database Syst Rev20138CD006826
- NanniniLJLassersonTJPoolePCombined corticosteroid and long-acting beta2-agonist in one inhaler versus long-acting beta2-agonists for chronic obstructive pulmonary diseaseCochrane Database Syst Rev20129CD006829
- NanniniLJPoolePMilanSJHolmesRNormansellRCombined corticosteroid and long-acting beta-agonist in one inhaler versus placebo for chronic obstructive pulmonary diseaseCochrane Database Syst Rev201311CD003794
- HalpinDGrayJEdwardsSMoraisJSinghDBudesonide/formoterol vs. salmeterol/fluticasone in COPD: a systematic review and adjusted indirect comparison of pneumonia in randomised controlled trialsInt J Clin Pract201165776477410.1111/j.1742-1241.2011.02685.x21676119
- EdsbäckerSWollmerPSelroosOBorgströmLOlssonBIngelfJDo airway clearance mechanisms influence the local and systemic effects of inhaled corticosteroids?Pulm Pharmacol Ther200821224725810.1016/j.pupt.2007.08.00517950641
- van den BrinkKIBoorsmaMStaalvan den BrekelAJEdsbäckerSWoutersEFThorssonLEvidence of the in vivo esterification of budesonide in human airwaysBr J Clin Pharmacol2008661273510.1111/j.1365-2125.2008.03164.x18384442
- SethiSMaloneyJGroveLWronaCBerensonCSAirway inflammation and bronchial bacterial colonization in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2006173999199810.1164/rccm.200509-1525OC16474030
- EkALarssonKSiljerudSPalmbergLFluticasone and budesonide inhibit cytokine release in human lung epithelial cells and alveolar macrophagesAllergy199954769169910442524
- LöfdahlCGEricssonASvenssonKAndreassonECost effectiveness of budesonide/formoterol in a single inhaler for COPD compared with each monocomponent used alonePharmacoeconomics200523436537510.2165/00019053-200523040-0000615853436