Abstract
Background and Objective
Severe chronic obstructive pulmonary disease (COPD) is the terminal stage of the disease characterized by declined lung function, malnutrition, and poor prognosis. Such patients cannot tolerate long-time sports rehabilitation owing to dyspnea and fail to achieve the desired therapeutic effect; therefore, increasing nutritional support will be an important strategy for them. The present study applied metabolomics technology to evaluate the correlation between serum concentrations of polyunsaturated fatty acid (PUFA) metabolites, nutritional status, and lung function in patients with COPD to provide a theoretical basis for accurate nutritional support.
Materials and Methods
We enrolled 82 patients with stable severe COPD in our hospital. The general characteristics including height, weight, and lung function were recorded. Metabolomics was used to detect the concentrations of serum metabolites of n-3 and n-6 at baseline and at 24 and 52 weeks after enrollment. The correlations between nutrition level and pulmonary function and clinical indicators were evaluated.
Results
The concentrations of n-3 and n-6 increased over time along with the progression of COPD. Body mass index (BMI) and percent of ideal body weight (IBW%) decreased with disease development, and BMI was found to be significantly correlated with FEV1% predicted and FEV1/FVC. Serum levels of n-6 metabolites such as linoleic acid (LA), γ-linoleic acid (GLA), and arachidonic acid (ARA) (all P < 0.01) and the n-3 metabolites such as eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) (all P < 0.05) showed significant correlations with BMI and were closely correlated with FEV1% predicted and FEV1/FVC of lung function (all P< 0.05).
Conclusion
This study demonstrates that malnutrition in patients with severe COPD is progressive and is positively correlated with n-3 and n-6 polyunsaturated fatty acids and lung function.
Introduction
Chronic obstructive pulmonary disease (COPD) is a common chronic inflammatory disease of the lungs, characterized by incomplete and persistent limitation of airflow and progressive aggravation over time.Citation1–Citation4 Accumulation of inflammatory cells and inflammatory cytokines in the respiratory tract can have adverse effects on the lungs including in the decline of lung function.Citation5,Citation6 The persistent inflammation and increased effort required for breathing increase patients’ energy expenditure.Citation7 Furthermore, inappetence and anxiety can lead to reduced energy intake, leading to malnutrition.Citation8 Most patients with COPD exist in a state of protein malnutrition, and reductions in muscle mass and myofiber strength mean that the normal function of respiratory muscles are reduced. This leads to a decline in lung compliance, thus accelerating disease progression.Citation9
Pulmonary rehabilitation has become an important strategy in the management of COPD, and can remarkably improve the quality of life and long-term prognosis of patients.Citation10 However, some patients with severe COPD and poor adherence to treatment may not tolerate this treatment.Citation10,Citation11 Therefore, such patients are most suited to drug therapy in clinical practice.Citation11,Citation12 The Global Initiative for Chronic Obstructive Lung Disease (GOLD) suggests that patients with grade 3–4 COPD would benefit from nutritional support during lung rehabilitation.Citation10,Citation13-15 Purposeful adjustment of nutritional intake could improve prognosis and reduce acute episodes and the length of readmissions.Citation16
Studies have shown that high-calorie diets or the maintenance of obesity can improve lung function of some patients with COPD, whereas excessive ingestion result in the obesity will exacerbate hypoxia.Citation8,Citation17,Citation18 Therefore, it is crucial to assess the nutritional level of patients before pulmonary rehabilitation ingestion intervention (the level and ratio of essential fatty acids), which is the basis of targeted nutrient schemes.Citation19–Citation21
As an important branch of systems biology, metabolomics can be used to elucidate the mechanisms underlying disease development, by providing solid biological evidence for personalized and precision medicine.Citation22,Citation23 Metabolomics has obvious advantages for COPD, a disease with a complex phenotype for which the physiological mechanism is unknown. The approach also plays a key role in determining appropriate nutritional support for chronic diseases.Citation24,Citation25 As a non-invasive test, metabolomics has great potential for investigations into the influence nutrient intake and the identification of biomarkers during disease progression.Citation26
For humans, n-3 and n-6 polyunsaturated fatty acids (PUFAs) are indispensable components of the daily diet, and are essential for maintaining normal physiological functions.Citation27,Citation28 The metabolites of n-3 PUFAs possess anti-inflammatory activities, which could attenuate the partial pro-inflammatory effects of n-6; thus, consuming n-3-rich foods can reduce inflammation to some extent.Citation29–Citation31 Furthermore, n-6 PUFAs are involved in a variety of physiological and pathological processes, acting as the immediate precursor of thrombin, leukotriene, and prostacyclin, and are responsible for regulating the persistent inflammation of COPD.Citation27 Interestingly, because of homeostasis, increased intake of n-3 or n-6 does not significantly affect the amount of metabolites produced or the secretion of downstream inflammatory markers.Citation32–Citation37
Materials and Methods
Study Design and Patients
For the present retrospective case-control study, we recruited all consecutive patients with severe stable COPD (the diagnostic criteria met the latest 2020 Global Initiative for Chronic Obstructive Lung Disease reports) who were treated at our institute from October 2016 to June 2017 and met the following inclusion criteria: 1) aged 70–80, 2) forced expiratory volume in 1 second (FEV1) <50% and FEV1/forced vital capacity (FVC) ≤0.7, 3) no history of immune-related respiratory disease or extrapulmonary disease involving the lungs and 4) no history of diabetes or hypertension. Written signed informed consent was obtained from all patients before enrollment. Each patient underwent a 52-week follow-up, and serum samples were taken and clinical data collected from all participants at baseline, 24 weeks and 52 weeks. In addition, 29 healthy volunteers were recruited as healthy control subjects. This experiment was approved by the Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University (NCT4042519). This study follows the ethical principles contained in the current version of the Helsinki declaration.
Lung Function Test
According to the requirements of the American Thoracic Society and the European Respiratory Society (ATS/ERS), pulmonary function tests were performed on participants using the Jaeger lung function instrument (MasterScreen, Leibnizstrasse, Hoechberg, Germany). Parameters included: FEV1, FVC, FEV1/FVC, total vital capacity, and total lung capacity (TLC). These indicators were used to diagnose and monitor COPD progression according to ATS/ERS criteria.Citation37
Collection and Storage of Blood Samples
Participants underwent venous blood collection. Samples were centrifuged at 3000 r/min (1006.2 xg) for 10 min and 20 degrees Celsius. The resulting serum was sub-packed and stored at –80°C which for no longer than 2 years prior to use. Repeated freezing and thawing was avoided for metabolomics research.
Measurement of Metabolites by Ultra-Performance Liquid Chromatography/Time-of-Flight Mass Spectrometry
An Agilent 1290 Infinity LC system (Santa Clara, CA, USA) was used for targeted determination of metabolites in serum samples, and radiolabeled compound hydroxy-eicosatetraenoic acid-d8 and prostaglandin D2-d4 (Ann Arbor, Michigan USA, Caymen) were used. The Metabolites were classified and matched according to the Kyoto Encyclopedia of Genes and Genomes (KEGG, Bioinformatics Center, Institute for Chemical Research, Kyoto University and Human Genome Center, Institute of Medical Science) and The Human Metabolome Database (HMDB4.0, University of Alberta, Edmonton, Canada). We used Agilent MassHunter Workstation Software Qualitative Analysis B.05.00 based on retention time, mass-charge ratio, and other molecular characteristics to analyze metabolite peak areas.
Statistical Analysis
Data were analyzed and graphed using SPSS (Statistics for Windows Version 22.0, IBM Corp, Chicago, IL, USA), GraphPadPrism 5.0 (GraphPad Software, San Diego, CA, USA), MedCalc, version 18.11 (MedCalc Software Inc., Acacialaan, Ostend, Belgium) and R-studio. The website Metaboanalyst (Xia Lab, McGill University) was used to create metabolite diagrams. Data are presented as the median ± standard deviation, evaluated using standardized indicators. Comparison of metabolites at each of the time points was analyzed using analysis of variance (ANOVA). We considered P < 0.05 to be statistically significant.
Results
Participants and Clinical Characteristics
presents the background characteristics of the study population, which included 82 patients with COPD. There were no significant differences in gender, age, or body mass index (BMI) between the two groups. Percent of ideal body weight (IBW%) was significantly different in the COPD group are compared with the normal group (P < 0.05). The pulmonary function parameters, including FVC% predicted, FEV1% predicted, and the FEV1/FVC ratios were significantly lower in patients with COPD than in healthy controls. The COPD group was evaluated at three time points: baseline, 24 weeks, and 52 weeks after enrollment. The BMI and IBW% decreased over time, as did the percentage of FEV1 in the predicted value (FEV1 pred%) and FEV1/FVC. Neutrophil and white blood cell counts were significantly higher in the COPD group than the normal controls (P < 0.05).
Table 1 Participant Characteristics
Nutritional Status of Patients with Chronic Obstructive Pulmonary Disease
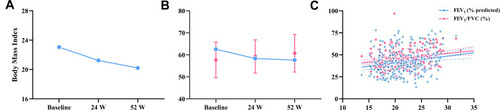
The body mass index (BMI) and ideal body weight percentage (IBW%) of patients with severe stable COPD declined over time (), and BMI was significantly correlated with FEV1% predicted and FEV1/FVC (r=0.18 and r= 0.23 respectively, all P < 0.01).
Metabolites of n-3 and n-6 Polyunsaturated Fatty Acids
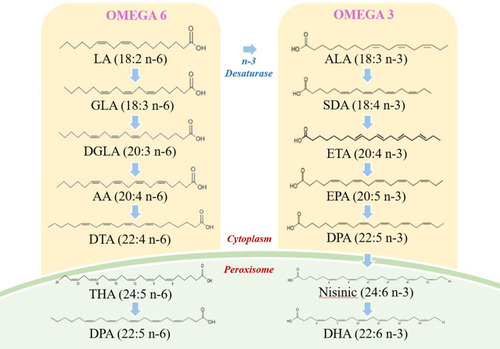
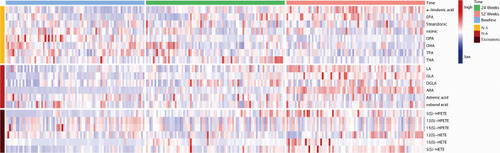
presents the results of analysis of each metabolite at each of the time points. illustrates the general trends of n-3 and n-6 metabolites; the concentration of linoleic acid (LA), gamma-linoleic acid (GLA), and di-homo gamma-linoleic acid (DGLA) increased progressively over the three time points in patients with COPD. The concentration of the eicosanoic acid metabolites 5-hydroperoxyeicosatetraenoic acid (5-HPETE), 5-hydroxyeicosatetraenoic acid (5-HETE), and 12-HETE with arachidonic acid (ARA) as the immediate substrate were also increased over three follow-up time points in the study. The concentration of n-3 alpha-linoleic acid (ALA) and eicosapentaenoic aced (EPA) increased over time, while docosapentaenoic acid (DPA), docosahexaenoic acid (DHA), tetracosapentaenoic acid (TPA) and tetracosahexaenoic acid (THA) declined over time. shows the pathway diagram of the metabolites detected in this study. In addition, the levels of n-3 and n-6 in healthy control subjects were lower than COPD patients.
Table 2 Peak Ratio of n-3 and n-6 Metabolites
Figure 2 Levels of n-3 and n-6 at different stages of COPD progression. The heatmap shows different metabolite levels at baseline, 24 W, and 52 W in patients with severely stable COPD.
Correlation Between Metabolite Levels and Lung Function in Patients with Chronic Obstructive Pulmonary Disease
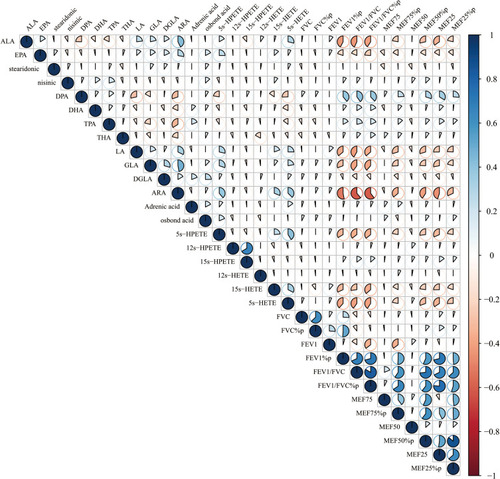
The n-6 metabolites LA, GLA, and ARA showed significant correlations with BMI (r = −0.23, −0.58, and −0.11, respectively, all P < 0.01), while EPA, DHA of n-3 metabolites were also significantly correlated with BMI (r = −0.54, −0.30, respectively, all P < 0.05). All those metabolites including LA, GLA, ARA, EPA and DHA were closely correlated with FEV1% predicted (r = −0.37, −0.35, −0.60, −0.47, −0.19, all P< 0.05) and FEV1/FVC (r = −0.26, −0.13, −0.44, −0.28, −0.72, respectively, all P< 0.05) (). In addition, the total contents of n-3 and n-6 were found to be significantly correlated with FEV1/FVC (all P < 0.05).
Figure 4 Correlation between n-3 and n-6 metabolites and lung function. The n-6 metabolites LA, GLA, and ARA showed significant correlations with BMI (r = −0.23, −0.58, and −0.11, respectively, all P < 0.01), while EPA, DHA of n-3 metabolites were also significantly correlated with BMI (r = −0.54, −0.30, respectively, all P < 0.05). All those metabolites including LA, GLA, ARA, EPA and DHA were closely correlated with FEV1% predicted (r = −0.37, −0.35, −0.60, −0.47, −0.19, all P< 0.05) and FEV1/FVC (r = −0.26, −0.13, −0.44, −0.28, −0.72, respectively, all P<0.05).
Discussion
In this study, we observed at three time points that inflammation levels increased with the progression of COPD and lung ventilation function decreased. Meanwhile, patient nutritional levels declined over time. The total content of n-3 and n-6 PUFAs rose over time, and were significantly correlated with lung function, BMI, and IBW%. Therefore, n-3 and n-6 metabolites may represent novel evaluation indicators for nutritional support during pulmonary rehabilitation in patients with COPD.
The Relationship Between Nutrient Levels and Disease Progression in Patients with Chronic Obstructive Pulmonary Disease
Through the evaluation of BMI and IBW% at three follow-up time points, we found that the nutritional level of patients with severe stable COPD decreased gradually as the disease advanced, and was significantly correlated with the FEV1% predicted and FEV1/FVC. Malnutrition is one of the risk factors for persistent disease progression in patients with COPD.Citation4 Weight loss is a common extrapulmonary manifestation, and BMI and IBW% are simple, precise, and repeatable indicators of nutritional levels.Citation4,Citation39,Citation40 As COPD progresses, respiratory work generally increases, as does anxiety and anorexia, which lead to decreased nutrient intake and impaired lung ventilation.Citation41,Citation42 Furthermore, malnutrition leads to decreased immune function and inflammatory damage to the normal structure of the bronchoalveoli, which result in decreased lung function and accelerated disease progression. Citation38,Citation43,Citation44 Therefore, we believe that nutritional support during pulmonary rehabilitation is crucial to end the negative cycle.
The sources of n-3 PUFAs mainly include deep-sea fish, shrimp, and beef, while n-6 PUFAs are mainly found in sunflower seeds, soybean oil, and meat.Citation45 Saini et alCitation46 reported that eating n-6-rich foods may increase the risk of chronic diseases, which may be antagonized by consumption of n-3 PUFAs. As essential fatty acids, the n-3 and n-6 are closely related to the level of inflammation, especially in the case of COPD. Roman et alCitation47 and Wood et alCitation48 reported that n-3 PUFAs can interfere with the process of chronic airway inflammation due to their anti-inflammatory properties. Many nutrition studies have also suggested the importance of the ratio of n-3 to n-6 in the formula of nutritional support for patients with COPD.Citation4,Citation35,Citation49-51 At present, this is the first longitudinal study to simultaneously evaluate the metabolites of n-3 and n-6 level in severe stable COPD patients.
The Relationship Between n-3 and n-6 Metabolites with Disease Progression
We identified an increase over time in the total content of n-3 and n-6 in serum samples. The anti-inflammatory activity of n-3 has been demonstrated in the context of various chronic inflammatory lung diseases, and can contribute to the reduction of neutrophil numbers in the lungs.Citation28,Citation52,Citation53 The n-6 PUFAs have pro-inflammatory effects and act as immediate precursors for a variety of potent pro-inflammatory mediators (leukotrienes and prostaglandins), which are responsible for airway remodeling and the destruction of alveolar structure.Citation6,Citation54
We identified a correlation between n-3 and n-6 PUFAs and lung function, indicating an imbalance between pro- and anti-inflammatory effects; thus, the total inflammation increases and lung function decreases. The overall concentrations of n-3 and n-6 PUFAs in serum samples reflect the data of their antagonistic actions in metabolism reported by Calder et al and Leuti et al.Citation30,Citation55 The concentration of ALA and EPA increased over time, and we speculated that this upregulation may lead to antagonization of the pro-inflammatory activities of n-6 metabolites, as has been mentioned in a previous study by Duvall et al.Citation52 Notably, because of the mechanisms of homeostasis and the intestinal flora, in spite of the concentration of n-3 is on the rise, it does not mean that all category of lipid metabolites on n-3 pathways are all on the rise.Citation56,Citation57 Although the present study provides some insight, the trends in metabolites of PUFAs in patients with COPD have not been fully elucidated and require further exploration.
Evaluation of n-3 and n-6 Lipid Metabolites and Nutritional Status in Patients with Chronic Obstructive Pulmonary Disease
The key metabolite of n-6 PUFAs (ARA) and the core metabolites of n-3 PUFAs (EPA and DHA) and the total concentrations of n-3 and n-6 PUFAs were found to be significantly correlated with BMI and IBW, respectively. In addition, these concentrations were significantly correlated with FEV1/FVC and FEV1. Therefore, the nutrient levels of patients with moderate-to-severe COPD decreased with disease progression, and we confirmed that n-3 and n-6 concentration reflected the decline in pulmonary function and could be used to evaluate the nutritional status of patients. Personalized medicine plays a key role in improving the symptoms of COPD; nutritional support and the establishment of a rational diet are of particular importance and require accurate assessment of the nutritional status of patients before a regimen is initiated.Citation39 The emergence of metabolomics has led to rapid developments in dietary therapy, which is gradually moving closer to clinical application.Citation58 Initial results and views have been presented in studies on multiple chronic diseases (diabetes, fatty liver, obesity, and cardiovascular disease);Citation59 therefore, metabolite-trend analysis also has immense potential in the evaluation of the nutriture of patients with severe stable COPD. We believe that the n-3 and n-6 lipid metabolites may represent novel indicators for such evaluation; in particular, EPA, DHA, and ARA, which not only reflect the nutriture of patients but also present a significantly negative correlation with lung function.
Conclusion
The EPA (n-3), DHA (n-3) and ARA (n-6), and the total concentration of lipid metabolites of n-3 and n-6 can reflect the nutriture of patients with severe stable COPD, which is closely related to the degree of disease progression. In the future, these may be used as novel indicators for the evaluation of nutrient levels of patients with COPD to inform nutritional support for pulmonary rehabilitation. Future research should focus on establishing a theoretical basis for the development of individualized nutrition programs. Moreover, we found that although there was antagonistic effect between n-3 and n-6, the content of the two does not present a tendency of increasing and decreasing, but that n-3 was also up-regulated to resist the pro-inflammatory effect of n-6. Therefore, the specific trend of metabolites in n-3 and n-6 needs to be further explored.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
This study was funded by Project supported by the Chinese National Natural Science Foundation (81700096; 8196010329; 81871736), Bureau of Traditional Chinese Medicine Scientific Research Project of Guangdong (Project No. 20192048), Science and Technology Innovation Committee Project of Guangzhou (Project No. 201804020043), Key Projects of Guangzhou Education Bureau (Project No. 201831802), and Open Project of State Key Laboratory of Respiratory Disease (Project No. SKLRD-OP-201803, SKLRD-OP-201809). Authors do not intend to share individual deidentified participant data and no study-related documents will be made available.
References
- ObeidatM, SadatsafaviM, SinDD. Precision health: treating the individual patient with chronic obstructive pulmonary disease. Med J Aust. 2019;210(9):424–428. doi:10.5694/mja2.5013830977152
- DuffySP, CrinerGJ. Chronic obstructive pulmonary disease: evaluation and management. Med Clin North Am. 2019;103:453–461. doi:10.1016/j.mcna.2018.12.00530955513
- RabeKF, HurdS, AnzuetoA, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176:532–555. doi:10.1164/rccm.200703-456SO17507545
- PizziniA, LungerL, SonnweberT, et al. The role of omega-3 fatty acids in the setting of coronary artery disease and COPD: a review. Nutrients. 2018;10(12):1864. doi:10.3390/nu10121864
- MaltaisF, DecramerM, CasaburiR, et al. An official American thoracic society/european respiratory society statement: update on limb muscle dysfunction in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2014;189:e15–e62. doi:10.1164/rccm.201402-0373ST24787074
- BarnesPJ. Inflammatory mechanisms in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2016;138:16–27. doi:10.1016/j.jaci.2016.05.01127373322
- ItohM, TsujiT, NemotoK, et al. Undernutrition in patients with COPD and its treatment. Nutrients. 2013;5(4):1316–1335. doi:10.3390/nu504131623598440
- HodsonM. Integrating nutrition into pathways for patients with COPD. Br J Community Nurs. 2016;21:548–552. doi:10.12968/bjcn.2016.21.11.54827809578
- AknerG, CederholmT. Treatment of protein-energy malnutrition in chronic nonmalignant disorders. Am J Clin Nutr. 2001;74:6–24. doi:10.1093/ajcn/74.1.611451713
- GarveyC, BaylesMP, HammLF, et al. Pulmonary rehabilitation exercise prescription in chronic obstructive pulmonary disease: review of selected guidelines: an official statement from the American association of cardiovascular and pulmonary rehabilitation. J Cardiopulm Rehabil Prev. 2016;36:75–83. doi:10.1097/HCR.000000000000017126906147
- IbrahimW, Harvey-DunstanTC, GreeningNJ. Rehabilitation in chronic respiratory diseases: in-hospital and post-exacerbation pulmonary rehabilitation. Respirology. 2019;24:889–898. doi:10.1111/resp.1351630835884
- KimSH, ShinMJ, ShinYB, et al. Sarcopenia associated with chronic obstructive pulmonary disease. J Bone Metab. 2019;26:65–74. doi:10.11005/jbm.2019.26.2.6531223602
- SpruitMA, WoutersEFM. Organizational aspects of pulmonary rehabilitation in chronic respiratory diseases. Respirology. 2019;24:838–843. doi:10.1111/resp.1351230810256
- MachadoA, QuadfliegK, OliveiraA, et al. Exercise training in patients with chronic respiratory diseases: are cardiovascular comorbidities and outcomes taken into account?-A systematic review. J Clin Med. 2019;8. doi:10.3390/jcm8091458
- NiciL, ZuWallackR. Chronic obstructive pulmonary disease-evolving concepts in treatment: advances in pulmonary rehabilitation. Semin Respir Crit Care Med. 2015;36:567–574. doi:10.1055/s-0035-155561326238642
- RochesterCL. Patient assessment and selection for pulmonary rehabilitation. Respirology. 2019;24:844–853. doi:10.1111/resp.1361631251443
- DubeBP, LavenezianaP. Effects of aging and comorbidities on nutritional status and muscle dysfunction in patients with COPD. J Thorac Dis. 2018;10:S1355–S1366. doi:10.21037/jtd.2018.02.2029928518
- Gayan-RamirezG. Relevance of nutritional support and early rehabilitation in hospitalized patients with COPD. J Thorac Dis. 2018;10:S1400–S1414. doi:10.21037/jtd.2018.03.16729928522
- SokolowskiCM, HigginsS, VishwanathanM, et al. The relationship between animal and plant protein intake and overall diet quality in young adults. Clin Nutr. 2019. doi:10.1016/j.clnu.2019.11.035
- BordoniA, CapozziF. Foodomics for healthy nutrition. Curr Opin Clin Nutr Metab Care. 2014;17:418–424. doi:10.1097/MCO.000000000000008925010544
- BaladyGJ, WilliamsMA, AdesPA, et al. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the American heart association exercise, cardiac rehabilitation, and prevention committee, the council on clinical cardiology; the councils on cardiovascular nursing, epidemiology and prevention, and nutrition, physical activity, and metabolism; and the American association of cardiovascular and pulmonary rehabilitation. J Cardiopulm Rehabil Prev. 2007;27:121–129. doi:10.1097/01.HCR.0000270696.01635.aa17558191
- SerkovaNJ, StandifordTJ, StringerKA. The emerging field of quantitative blood metabolomics for biomarker discovery in critical illnesses. Am J Respir Crit Care Med. 2011;184:647–655. doi:10.1164/rccm.201103-0474CI21680948
- CaiC, BianX, XueM, et al. Eicosanoids metabolized through LOX distinguish asthma-COPD overlap from COPD by metabolomics study. Int J Chron Obstruct Pulmon Dis. 2019;14:1769–1778. doi:10.2147/COPD.S20702331496676
- KrishnanJK, MartinezFJ. Lung function trajectories and chronic obstructive pulmonary disease: current understanding and knowledge gaps. Curr Opin Pulm Med. 2018;24:124–129. doi:10.1097/MCP.000000000000045629206658
- Schrimpe-RutledgeAC, CodreanuSG, SherrodSD, et al. Untargeted metabolomics strategies-challenges and emerging directions. J Am Soc Mass Spectrom. 2016;27:1897–1905. doi:10.1007/s13361-016-1469-y27624161
- O’CallaghanN, NoakesM. Meeting report from “frontiers in nutritional science: nutritional metabolomics”. Nutrients. 2014;6:3451–3459. doi:10.3390/nu609345125192025
- DasUN. Ageing: is there a role for arachidonic acid and other bioactive lipids? A review. J Adv Res. 2018;11:67–79. doi:10.1016/j.jare.2018.02.00430034877
- CalderPC, GrimbleRF. Polyunsaturated fatty acids, inflammation and immunity. Eur J Clin Nutr. 2002;56(Suppl 3):S14–S19. doi:10.1038/sj.ejcn.160147812142955
- YatesCM, CalderPC, RaingerG. Pharmacology and therapeutics of omega-3 polyunsaturated fatty acids in chronic inflammatory disease. Pharmacol Ther. 2014;141:272–282. doi:10.1016/j.pharmthera.2013.10.01024201219
- CalderPC. Omega-3 fatty acids and inflammatory processes: from molecules to man. Biochem Soc Trans. 2017;45:1105–1115. doi:10.1042/BST2016047428900017
- ChiltonFH, DuttaR, ReynoldsLM, et al. Precision nutrition and omega-3 polyunsaturated fatty acids: a case for personalized supplementation approaches for the prevention and management of human diseases. Nutrients. 2017;9(11):1165. doi:10.3390/nu9111165
- InnesJK, CalderPC. Omega-6 fatty acids and inflammation. Prostaglandins Leukot Essent Fatty Acids. 2018;132:41–48. doi:10.1016/j.plefa.2018.03.00429610056
- LemoineCM, BrighamEP, WooH, et al. Omega-3 fatty acid intake and prevalent respiratory symptoms among U.S. adults with COPD. BMC Pulm Med. 2019;19(1):97. doi:10.1186/s12890-019-0852-431122230
- JohnsonM, McElhenneyWH, EgninM. Influence of green leafy vegetables in diets with an elevated omega-6: omega-3 fatty acid ratio on rat blood pressure, plasma lipids, antioxidant status and markers of inflammation. Nutrients. 2019;11(2):301. doi:10.3390/nu11020301
- SimopoulosAP. An Increase in the omega-6/omega-3 fatty acid ratio increases the risk for obesity. Nutrients. 2016;8:128. doi:10.3390/nu803012826950145
- FranzosaEA, Sirota-MadiA, Avila-PachecoJ, et al. Gut microbiome structure and metabolic activity in inflammatory bowel disease. Nat Microbiol. 2019;4:293–305. doi:10.1038/s41564-018-0306-430531976
- Pinto-PlataV, CasanovaC, DivoM, et al. Plasma metabolomics and clinical predictors of survival differences in COPD patients. Respir Res. 2019;20:219. doi:10.1186/s12931-019-1167-y31615518
- CelliBR, DecramerM, WedzichaJA, et al. An official American thoracic society/european respiratory society statement: research questions in COPD. Eur Respir Rev. 2015;24:159–172. doi:10.1183/16000617.0000031526028628
- HancuA. Nutritional status as a risk factor in COPD. Maedica (Buchar). 2019;14:140–143. doi:10.26574/maedica.2019.14.2.14031523295
- GeaJ, BarreiroE. Nutritional abnormalities and chronic obstructive pulmonary disease. Int J Tuberc Lung Dis. 2019;23:531–532. doi:10.5588/ijtld.19.016031097058
- OganN, AydemirY, EVT, et al. Diaphragmatic thickness in chronic obstructive lung disease and relationship with clinical severity parameters. Turk J Med Sci. 2019;49:1073–1078. doi:10.3906/sag-1901-16431293145
- JungJW, YoonSW, LeeGE, et al. Poor nutritional intake is a dominant factor for weight loss in chronic obstructive pulmonary disease. Int J Tuberc Lung Dis. 2019;23:631–637. doi:10.5588/ijtld.18.045631097074
- AroraS, MadanK, MohanA, et al. Serum inflammatory markers and nutritional status in patients with stable chronic obstructive pulmonary disease. Lung India. 2019;36(5):393–398. doi:10.4103/lungindia.lungindia_494_1831464210
- Paplinska-GorycaM, RubinsztajnR, Nejman-GryzP, et al. The association between serological features of chronic Chlamydia pneumoniae infection and markers of systemic inflammation and nutrition in COPD patients. Scand J Clin Lab Invest. 2017;77(8):644–650. doi:10.1080/00365513.2017.139369429069917
- RussoGL. Dietary n-6 and n-3 polyunsaturated fatty acids: from biochemistry to clinical implications in cardiovascular prevention. Biochem Pharmacol. 2009;77:937–946. doi:10.1016/j.bcp.2008.10.02019022225
- SainiRK, KeumYS. Omega-3 and omega-6 polyunsaturated fatty acids: dietary sources, metabolism, and significance - a review. Life Sci. 2018;203:255–267. doi:10.1016/j.lfs.2018.04.04929715470
- RomanGC, JacksonRE, GadhiaR, et al. Mediterranean diet: the role of long-chain omega-3 fatty acids in fish; polyphenols in fruits, vegetables, cereals, coffee, tea, cacao and wine; probiotics and vitamins in prevention of stroke, age-related cognitive decline, and alzheimer disease. Rev Neurol (Paris). 2019;175(10):724–741. doi:10.1016/j.neurol.2019.08.00531521398
- WoodLG. Omega-3 polyunsaturated fatty acids and chronic obstructive pulmonary disease. Curr Opin Clin Nutr Metab Care. 2015;18:128–132. doi:10.1097/MCO.000000000000014225581034
- VarrasoR, BarrRG, WillettWC, et al. Fish intake and risk of chronic obstructive pulmonary disease in 2 large US cohorts. Am J Clin Nutr. 2015;101:354–361. doi:10.3945/ajcn.114.09451625646333
- CollinsPF, YangIA, ChangY-C, et al. Nutritional support in chronic obstructive pulmonary disease (COPD): an evidence update. J Thorac Dis. 2019;11(S17):S2230–S2237. doi:10.21037/jtd.2019.10.4131737350
- SimopoulosAP. Evolutionary aspects of diet, the omega-6/omega-3 ratio and genetic variation: nutritional implications for chronic diseases. Biomed Pharmacother. 2006;60:502–507. doi:10.1016/j.biopha.2006.07.08017045449
- DuvallMG, LevyBD. DHA- and EPA-derived resolvins, protectins, and maresins in airway inflammation. Eur J Pharmacol. 2016;785:144–155. doi:10.1016/j.ejphar.2015.11.00126546247
- AbdulnourRE, DalliJ, ColbyJK, et al. Maresin 1 biosynthesis during platelet-neutrophil interactions is organ-protective. Proc Natl Acad Sci U S A. 2014;111:16526–16531. doi:10.1073/pnas.140712311125369934
- RuttingS, PapanicolaouM, XenakiD, et al. Dietary omega-6 polyunsaturated fatty acid arachidonic acid increases inflammation, but inhibits ECM protein expression in COPD. Respir Res. 2018;19:211. doi:10.1186/s12931-018-0919-430390648
- LeutiA, MaccarroneM, ChiurchiuV. Proresolving lipid mediators: endogenous modulators of oxidative stress. Oxid Med Cell Longev. 2019;2019:8107265. doi:10.1155/2019/810726531316721
- LovewellRR, SassettiCM, VanderVenBC. Chewing the fat: lipid metabolism and homeostasis during M. tuberculosis infection. Curr Opin Microbiol. 2016;29:30–36. doi:10.1016/j.mib.2015.10.00226544033
- SharonG, CruzNJ, KangDW, et al. Human gut microbiota from autism spectrum disorder promote behavioral symptoms in mice. Cell. 2019;177:1600–1618 e1617. doi:10.1016/j.cell.2019.05.00431150625
- ShiL, BruniusC, JohanssonI, et al. Plasma metabolites associated with healthy nordic dietary indexes and risk of type 2 diabetes-a nested case-control study in a Swedish population. Am J Clin Nutr. 2018;108:564–575. doi:10.1093/ajcn/nqy14530060042
- ChengS, ShahSH, CorwinEJ, et al. Potential impact and study considerations of metabolomics in cardiovascular health and disease: a scientific statement from the American heart association. Circ Cardiovasc Genet. 2017. doi:10.1161/HCG.0000000000000032