Abstract
Purpose
Cognitive dysfunction is a common impairment associated with COPD. However, little is known about 1) its prevalence among those subjects referred for pulmonary rehabilitation (PR), 2) how it may affect the benefit of PR, 3) whether PR improves cognitive function and 4) whether cognitive dysfunction affects the usability of telehealth technology usually used to deliver in-home PR.
Patients and Methods
Fifty-six subjects with stable COPD (54% females, mean age 62 years (SD 9) and median FEV1 0.9 L (IQR 0.7 to 1.1)) participated in this multicenter observational study and performed 24 sessions of PR. The Montreal Cognitive Assessment tool (MoCA) was used to assess the occurrence of mild cognitive dysfunction (using a screening cutoff <26) at baseline, completion of PR and 3 months of follow-up.
Results
Mild cognitive dysfunction was found in 41 subjects (73% [95% CI: 60 to 83%]). The MoCA score significantly improved following PR for those people with baseline mild cognitive dysfunction (p<0.01). There was no significant difference in clinical outcomes between those people with or without mild cognitive dysfunction following PR nor in the proportion of subjects who were autonomous in using the telemonitoring system (83% compared with 71%, p=0.60).
Conclusion
Mild cognitive dysfunction is highly prevalent among those people with COPD referred for PR but does not affect the benefits of PR nor the usability of a telemonitoring system. PR may improve short- and mid-term cognitive function for those people who experience mild cognitive dysfunction at the time they are referred to PR.
Introduction
Chronic obstructive pulmonary disease (COPD) is a leading cause of death worldwideCitation1 and its prevalence, as high as 10% in adults over 40 years old,Citation2 is planned to increase in the next decade.Citation3 This respiratory disease progressively leads to physical inactivity, muscle deconditioning and worsening dyspnea.Citation4 Pulmonary rehabilitation (PR), including exercise training and education, is therefore recommended for these patients.Citation5,Citation6 The aim of PR is not only to improve exercise capacity, dyspnea and quality of lifeCitation7 but also to promote behavior changes in order to maintain long-term adherence to health-enhancing comportments, including exercise maintenance.Citation5 The behavior changes necessary to maintain an in-home exercise program are driven by the cognitive functions which refer to a high-order neural process that underpins information handling by which a behavior can be adapted.Citation8,Citation9 However, cognitive dysfunction is another systemic feature impairment associated with COPD and may be as prevalent as 88% in hypoxic subjects.Citation9 Although the mechanisms have not been clearly elucidated yet, these may involve chronic hypoxemia, chronic hypercapnia, lung function impairment, systemic inflammation, inactivity, smoking, cerebral atrophy or structural changes and repeated acute exacerbations.Citation8–Citation10
Cognitive dysfunction in COPD is associated with worst outcome such as altered quality of life,Citation11 higher rate of hospitalizationCitation12 or death,Citation8,Citation9,Citation12,Citation13 as well as with unsuitable health behavior, such as poor intake of inhaled treatmentsCitation14 or difficulties in smoking cessation.Citation15 However, little is known about its prevalence among those subjects referred for PRCitation16,Citation17 and how it may affect the benefit or PR.Citation18 Though some studies have shown a potential improvement in cognitive function with PR,Citation19,Citation20 little is known about whether these benefits are subsequently maintained and whether they impact exercise maintenance following PR.Citation21 In addition, because of a limited access to PR (mainly located in urban areas) and a number of barriers to attend or participate in,Citation22–Citation24 PR is often delivered in the home environment with the use of telehealth technologies.Citation25 However, the impact of cognitive function on the usability of telehealth technology usually used to deliver in-home PR has not been studied yet. Therefore, we hypothesized that cognitive dysfunction is highly prevalent among those people with COPD referred for PR but has the potential to improve following PR. Additionally, we hypothesized that cognitive dysfunction may impede with the positive effect of PR as well as with the usability of telehealth technology and exercise maintenance following PR.
The primary aims of this study were to assess the prevalence of cognitive dysfunction among people with COPD referred for PR and the mid-term effects of PR on cognitive function (3 months after completion). Secondary objectives were to assess how cognitive dysfunction may affect the benefit of PR, telehealth technology usability and exercise maintenance following PR.
Methods
Study Design and Participants
This prospective multicenter observational study was approved by the French Ethics Committee Ile de France 1 (2017-juin-14586 ND), was prospectively registered at https://www.clinicaltrials.gov (NCT3244137) and conducted in accordance with the Declaration of Helsinki.
Subjects with a clinical diagnosis of COPD referred for PR at ADIR Association, Rouen University Hospital, France and Jacques Monod Hospital, Le Havre, France, were screened for eligibility between August 2017 and June 2019. They had to be 18 years and over, have a forced expiratory volume in 1 s (FEV1) <50% and be eligible to PR (ie, exertional or rest dyspnea and no medical contraindication to exercise). Subjects were not included if they were hospitalized for an acute exacerbation within the previous 3 months,Citation11,Citation26 had an active alcoholism or had a history of psychiatric or neurovascular disease, cranial trauma, or other known disease associated with cognitive dysfunction. Other non-inclusion criteria included pregnancy or likely to be and guardianship. Subjects were excluded if the PR program was interrupted for more than 14 days due to severe acute exacerbation of COPD,Citation11,Citation26 if they disrupted training before 18 sessions or performed less than 18 sessions in 4 months (non-adherent subjects). Written informed consent was obtained from all patients.
Clinical and Functional Assessment
Before attending the PR program and prior to participating in the study, every subject underwent an evaluation including pulmonary function testsCitation27 and cardiopulmonary exercise testing (CPET).Citation28
Pulmonary Rehabilitation Program
Every subject participated in a 3 times per week for 8 weeks comprehensive outpatient PR program including respiratory physiotherapy, muscle strengthening, endurance training, self-management and nutritional support as necessary.
Peripheral muscle strengthening (3 sets of 12 movements at 70% of the one repetition maximum or using resistive bands) mainly focused on the lower limbs. Endurance training was progressive (from 15 to 45 mins, including a 5 mins warm-up and a 5 mins cool down periods) and the intensity was adjusted at the anaerobic threshold (manually derived from the initial CPET as the average of 4 methods: first break the minute ventilation curve, rise in the minute ventilation to oxygen consumption ratio without modification of the minute ventilation to carbon dioxide production ratio, rise in the end-tidal expired carbon dioxide gas and the Beaver’s methodCitation28,Citation29). Subsequently, the intensity was increased based on perceived exertion (dyspnea or muscular fatigue assessed using the Borg scaleCitation30 as previously describedCitation31).
The self-management program was also individualized and constructed according to the « Living Well with COPD » program,Citation32 as well as with the French « Haute Autorité de Santé » guidelines for COPD self-management.Citation33 It covered the following topics: COPD knowledge, smoking cessation, management of acute exacerbations, inhaled treatments, physical activities, breathing management, healthy lifestyle, oxygen therapy, noninvasive ventilation, hobbies and traveling.
Usability of a Telemonitoring System
The first subjects were also invited to participate in a second prospective observational study aiming to assess whether subjects referred to pulmonary rehabilitation could easily learn to use a system for remote transmission of oximetry data. This second study, offered to every subject with chronic lung disease referred to pulmonary rehabilitation (without any other restriction) took place within the same period in both centres but ended earlier.Citation34
Briefly, an investigator physiotherapist taught the participants how to use the telemonitoring system and subsequent sessions were scheduled to determine when the subjects became autonomous with transmitting their data via the telemonitoring system.Citation34
Outcomes
Outcomes were assessed before PR, at the end of PR and 3 months following the completion of PR.
The primary outcome was cognitive function assessed with the Montreal Cognitive Assessment tool (MoCA).Citation17,Citation35,Citation36 Three versions of the tool are currently available to avoid any learning effects and were used in a cross-over randomized order throughout the evaluations (computer-generated sequence and concealed allocation). The same investigator performed the three evaluations for a given patient. A screening cutoff <26 was used to assess the occurrence of mild cognitive dysfunction.Citation17,Citation36
Secondary outcomes were health-related quality of life using the Saint George’s Respiratory Questionnaire total score and sub-scores,Citation37 anxiety and depression using the Hospital Anxiety and Depression scaleCitation38 and functional capacity (only assessed before and at the end of PR) using the six-minute walk testCitation39 and the six-minute stepper test.Citation40–Citation42 In addition, autonomy in using the telemonitoring system was granted if the procedure was repeated successfully at the first session after initiation.
Statistical Analysis
The normality of the data was assessed using the Kolmogorov–Smirnov test. Categorical data were expressed as counts (% and 95% confidence interval (CI)) and continuous data were expressed as mean (SD) or median (25th–75th percentile) according to the distribution. Comparison of outcomes between baseline, following PR and 3 months following PR was performed using either repeated ANOVA (and Tukey post hoc tests) or a Friedman test (and a Wilcoxon test as a post hoc test for pairwise comparisons) according to the distribution. The change in the proportion of subjects with a MOCA score <26 was assessed using the Cochran test.
To assess the effects of cognitive dysfunction on the benefit of PR, exercise maintenance following PR and telehealth technology usability, subjects were separated into two groups according to their baseline score on the MOCA tool (<26 or ≥26). Difference in outcomes between groups was assessed using either an independent Student’s t-test or a Mann–Whitney test for quantitative data and a Fisher exact test for categorical data. A p-value <0.05 was considered as statistically significant. SPPS software version 25 was used for all analyses.
Results
Subjects
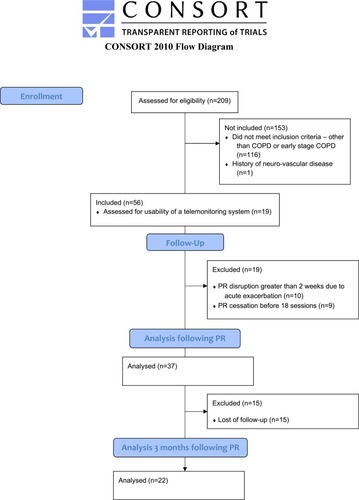
Two hundred nine subjects were screened for eligibility and 56 were included in the study (). Fifty-four percent of the participants were women, their mean age was 62 (SD 9) years, their median FEV1 was 0.9 L (IQR 0.7 to 1.1) and their aerobic capacity was decreased (mean VO2: 12 (SD 3) mL/kg/min). Among them, 19 also participated in the assessment of the usability of a telemonitoring system. Mild cognitive dysfunction was found in 41 subjects (73% [95% CI: 60% to 83%]). Their baseline characteristics were not significantly different from those people without cognitive dysfunction but they had the worst quality of life and a lower educational level (). Thirty-seven subjects were assessed following PR and 22 subjects 3 months thereafter (see for reasons of drop-out). Comparisons between subjects who did complete PR and those who did not, and between subjects that attended the 3 months follow-up and those who did not are shown in Table S1 and Table S2, respectively. The same comparisons for those subjects with a baseline MoCA <26 are shown in Table S3 and Table S4, respectively.
Table 1 Demographic Characteristics of the Patients
Primary Outcome
The MoCA score significantly increased during the follow-up period (p<0.01), mainly due to a significant increase in the median score between baseline and 3 months following PR (from 22 (IQR 20 to 26) to 25 (IQR 23 to 28) respectively, p<0.01). The median MoCA score remained unchanged among those people without baseline mild cognitive dysfunction (p=0.37) while it significantly increased among those people with baseline mild cognitive dysfunction (p<0.01) mainly due to a significant improvement at the end of PR (from 21 (IQR 20 to 24) to 22 (IQR 20 to 26), p<0.01) which was sustained 3 months thereafter (median score: 24 (IQR 21 to 26), p<0.01) ().
Figure 2 Evolution of the Montreal Cognitive Assessment tool total score (A) and sub-score (B). Data are shown as median (25th–75th percentile). Friedman test and Wilcoxon as a post hoc test for pairwise comparison for within-group comparison. Baseline: n=56; following PR: n=37, 3 months following PR: n=22. *p<0.01 **p=0.04.
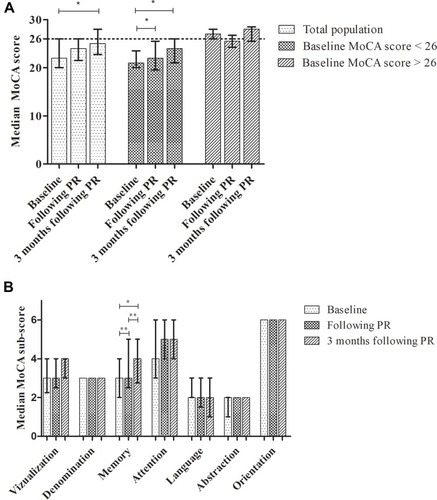
Among the cognitive domains, only the median memory score significantly increased from baseline to post PR (from 3 (IQR 2 to 4) to 3 (IQR 3 to 5), p=0.04) and 3 months thereafter (4 (IQR 3 to 5), p<0.01). It was further improved from post PR to 3 months following PR (p=0.04) (). There was no significant change in the proportion of people with mild cognitive dysfunction during the follow-up (p=0.20).
Secondary Outcomes
In the total population, PR significantly improved exercise capacity (6MST and 6MWT) and the SGRQ impact sub-score. The SGRQ impact sub-score was further improved 3 months thereafter (p=0.02) (). There was no significant difference in outcomes between those people with or without mild cognitive dysfunction either following PR or at 3 months except for the median 6MST which was significantly higher for those people without mild cognitive dysfunction (218 (IQR 162 to 263) steps compared with 182 (IQR 121 to 310) steps, p=0.03) ().
Table 2 Change in Secondary Outcomes Following and 3 Months After PR
The proportion of subjects who maintained a physical activity was not significantly different between those with or without mild cognitive dysfunction following PR (57% compared with 63%, respectively, p=1). The MoCA score 3 months following PR was not significantly different between those people who maintained a physical activity or not (24 (SD 3) and 25 (SD 3) respectively, p=0.71)
Finally, 10 out of 12 subjects (83%) with mild cognitive dysfunction were autonomous in using the telemonitoring system which was not significantly different from those subjects without mild cognitive dysfunction (5 out of 7 (71%), p=0.60).
Relationship Between the MoCA Score and Outcomes
At baseline, the MoCA score was negatively correlated with the SGRQ total score (r= −0.28, p=0.04; ie a higher score on the MoCA tool was associated with a better quality of life). The change in the MoCA score was not significantly associated with a change in any outcome following PR.
Discussion
The present study revealed that mild cognitive dysfunction was highly prevalent among people with severe to very severe COPD referred for PR (about 75%) but may not affect the benefits of PR since there was no statistical or clinically relevant difference in outcomes between those people with or without mild cognitive dysfunction. In addition, PR had the potential to improve short and mid-term cognitive function, particularly for those people who experienced mild cognitive dysfunction at the time they were referred to PR. Finally, mild cognitive dysfunction was not associated with a worst rate of exercise maintenance following PR nor with a worst rate of usability of a telemonitoring system.
Cognitive Function and Pulmonary Rehabilitation
The prevalence of mild cognitive dysfunction was relatively high in the present cohort (73%) compared with previous studies which also used the MoCA score as a screening tool (from 10% to 18%).Citation16,Citation17 This difference may be explained by the severity of the subjects recruited since the worsening of the respiratory function and/or chronic hypoxia (48% of long-term users) have been associated with cognitive dysfunction.Citation43–Citation46 The present results extend those from previous studies showing a positive effect of PR on cognitive functionCitation19,Citation20,Citation47 particularly for those people who experienced mild cognitive dysfunction when attending PR. The physiological explanation underlying this improvement remains unclear but may include repetitive acute bouts of exercise sessions which contribute to increasing cardiac output and neurotransmitters release during exercise,Citation48 benefit of social exchanges during group exercise sessions as well as PR-induced neural changes.Citation49
An additional important finding was that this positive effect was subsequently maintained 3 months following PR. Contrary to Emery et al, who found that the improvement in cognitive function was maintained at 1 year following PR only for those people who continued with a regular program of moderate-intensity exercise,Citation21 we did not find such an association, suggesting a residual effect of the initial program on cognitive function up to 3 months. This is of interest since this period is a hinge between the supervised program and the less or unsupervised long-term maintenance program which requires a cognitive function-directed behavior change. Though the preliminary results of this study suggest that cognitive dysfunction may not negatively affect exercise maintenance following PR, this should further be studied.
On the other hand, in the absence of a known minimal clinical important difference (MCID) for the MoCA score and considering than both the median score remained below 26 and the proportion of subjects with mild cognitive impairment did not significantly change during the follow-up period, the clinical relevance of the present findings remains questionable. Therefore, further study should consider to assess the MCID for the MoCA score, which offers the advantage to be easier to perform in clinical practice than more comprehensive cognitive function battery tests.
Impact of Cognitive Functions on PR Outcomes
Following PR, both those people with or without mild cognitive dysfunction significantly and clinically improved their performance on the 6MST (>20 stepsCitation50). The between-group difference following PR probably reflects the trend observed at baseline towards a lower performance for those people with mild cognitive dysfunction (p=0.08) so that the actual difference in improvement between groups is likely clinically trivial. In addition, the mean improvement in the 6MWT also lied within the range of the established MCID (25 to 33 mCitation39) for the total population (p=0.01) and both subgroups. However, the latter failed to reach statistical significance due to a loss in statistical power. Contrary to Emery et al, we did not find any improvement in psychological wellbeingCitation19,Citation20 but found a clinical improvement (>4 pointsCitation37) in the SGRQ impact sub-score following and 3 months after PR, particularly in those people having a baseline mild cognitive dysfunction. In addition, neither the baseline MoCA score nor the change in the MoCA score was significantly associated with outcomes changes following PR. Altogether, these results extend those from a previous studyCitation18 and suggest that cognitive dysfunction may not alter the progression during PR when subjects are closely supervised.
Implication for Practice and Research
Though cognitive dysfunction may not impede the effectiveness of supervised PR, the access to such programs is limited.Citation22–Citation24 To cope with this difficulty, PR may be delivered in the home environment but this often implies a lower level of supervision.Citation51,Citation52 Alternatively, home-based PR may provide supervision that center-based pulmonary rehabilitation provides if it uses new technologies to allow remote telemonitoring and therapists’ prompt feedback. Reassuringly, this study provides preliminary evidence than people with mild cognitive dysfunction are able to use user-friendly telemonitoring system (83% were autonomous at the first session after initiation which was not significantly different from those people without mild cognitive dysfunction (71%, p=0.60) and within the range of the success rate of the overall cohort (86%)Citation34). Since memory was significantly improved following PR in the present study, this strengthens the idea that subjects should be able to keep using this system throughout the program. Therefore, future studies should now assess the feasibility, safety and effectiveness of a telemonitoring home-based PR for those people with COPD-related mild cognitive dysfunction.
Limits of the Study
The main limitations of this study were the lack of a control group without PR and the small sample size studied. In addition, the dropout rate was relatively high but comparable to the rate in other studies about PR.Citation52–Citation54 However, those people who did not complete PR or did not attend the 3-month follow-up did not significantly differ from those who completed the overall study, suggesting a lack of selection bias. Nonetheless, this high attrition contributed to decreasing the power of the study which may have led to some type 2 statistical errors. Therefore, the lack of difference between those subjects with or without mild cognitive dysfunction on PR outcomes or telehealth system usability should be considered as exploratory.
Conclusion
Mild cognitive dysfunction is highly prevalent among those people with severe to very severe COPD referred for PR (about three quarter) but may not affect the benefits of PR. PR may improve short and mid-term cognitive function, particularly for those people who experience mild cognitive dysfunction at the time they are referred to PR. Finally, mild cognitive dysfunction may not affect exercise maintenance following PR nor the usability of a user-friendly telemonitoring system.
Registration
The protocol was prospectively registered on www.clinicaltrials.gov (NCT3244137).
Abbreviations
CI, confidence intervals; COPD, chronic obstructive pulmonary disease; CPET, cardiopulmonary exercise testing; FEV1, forced expiratory volume in 1 s; MCID, minimal clinical important difference; MoCA, Montreal Cognitive Assessment tool; PR, pulmonary rehabilitation.
Data Sharing Statement
De-identified participant data published in the manuscript will be shared to searcher performing a meta-analysis on request. Data will be available after publication. Please, contact Tristan Bonnevie ([email protected]) for query.
Ethics and Consent Statement
This prospective observational study was approved by the French Ethics Committee Ile de France 1 (2017-juin-14586 ND). Written consent was obtained from all subjects.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
TB reports a grant from Fisher & Paykel outside the submitted work. The authors report no funding and no other possible conflicts of interest for this work.
Acknowledgments
This work was supported by the ADIR Association. We thank Emeline Fresnel and Adrien Kerfourn (KerNel Biomedical, Rouen, France) for statistical support.
References
- LozanoR, NaghaviM, ForemanK, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi:10.1016/S0140-6736(12)61728-023245604
- HalbertRJ, NatoliJL, GanoA, BadamgaravE, BuistAS, ManninoDM. Global burden of COPD: systematic review and meta-analysis. Eur Respir J. 2006;28(3):523–532. doi:10.1183/09031936.06.0012460516611654
- KhakbanA, SinDD, FitzGeraldJM, et al. The projected epidemic of chronic obstructive pulmonary disease hospitalizations over the next 15 years. a population-based perspective. Am J Respir Crit Care Med. 2017;195(3):287–291. doi:10.1164/rccm.201606-1162PP27626508
- RamonMA, Ter RietG, CarsinAE, et al. The dyspnoea-inactivity vicious circle in COPD: development and external validation of a conceptual model. Eur Respir J. 2018;52(3):1800079. doi:10.1183/13993003.00079-201830072504
- SpruitMA, SinghSJ, GarveyC, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–64. doi:10.1164/rccm.201309-1634ST24127811
- VogiatzisI, RochesterCL, SpruitMA, TroostersT, CliniEM. American Thoracic Society/European Respiratory Society Task Force on Policy in Pulmonary R. Increasing implementation and delivery of pulmonary rehabilitation: key messages from the new ATS/ERS policy statement. Eur Respir J. 2016;47(5):1336–1341. doi:10.1183/13993003.02151-201527132269
- McCarthyB, CaseyD, DevaneD, MurphyK, MurphyE, LacasseY. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015;2(2):CD003793.
- DoddJW, GetovSV, JonesPW. Cognitive function in COPD. Eur Respir J. 2010;35(4):913–922. doi:10.1183/09031936.0012510920356988
- CleutjensFA, JanssenDJ, PondsRW, DijkstraJB, WoutersEF. COgnitive-pulmonary disease. Biomed Res Int. 2014;2014:697825. doi:10.1155/2014/69782524738069
- YinM, WangH, HuX, LiX, FeiG, YuY. Patterns of brain structural alteration in COPD with different levels of pulmonary function impairment and its association with cognitive deficits. BMC Pulm Med. 2019;19(1):203. doi:10.1186/s12890-019-0955-y31699064
- DoddJW, CharltonRA, van den BroekMD, JonesPW. Cognitive dysfunction in patients hospitalized with acute exacerbation of COPD. Chest. 2013;144(1):119–127. doi:10.1378/chest.12-209923349026
- ChangSS, ChenS, McAvayGJ, TinettiME. Effect of coexisting chronic obstructive pulmonary disease and cognitive impairment on health outcomes in older adults. J Am Geriatr Soc. 2012;60(10):1839–1846. doi:10.1111/j.1532-5415.2012.04171.x23035917
- Antonelli-IncalziR, CorsonelloA, PedoneC, et al. Drawing impairment predicts mortality in severe COPD. Chest. 2006;130(6):1687–1694. doi:10.1378/chest.130.6.168717166983
- AllenSC, JainM, RagabS, MalikN. Acquisition and short-term retention of inhaler techniques require intact executive function in elderly subjects. Age Ageing. 2003;32(3):299–302. doi:10.1093/ageing/32.3.29912720616
- BregaAG, GrigsbyJ, KookenR, HammanRF, BaxterJ. The impact of executive cognitive functioning on rates of smoking cessation in the San Luis valley health and aging study. Age Ageing. 2008;37(5):521–525. doi:10.1093/ageing/afn12118515287
- PierobonA, RanziniL, TorlaschiV, et al. Screening for neuropsychological impairment in COPD patients undergoing rehabilitation. PLoS One. 2018;13(8):e0199736. doi:10.1371/journal.pone.019973630067787
- PierobonA, Sini BottelliE, RanziniL, et al. COPD patients’ self-reported adherence, psychosocial factors and mild cognitive impairment in pulmonary rehabilitation. Int J Chron Obstruct Pulmon Dis. 2017;12:2059–2067. doi:10.2147/COPD.S13358628790808
- CleutjensF, SpruitMA, PondsR, et al. The impact of cognitive impairment on efficacy of pulmonary rehabilitation in patients with COPD. J Am Med Dir Assoc. 2017;18(5):420–426. doi:10.1016/j.jamda.2016.11.01628108209
- EmeryCF, ScheinRL, HauckER, MacIntyreNR. Psychological and cognitive outcomes of a randomized trial of exercise among patients with chronic obstructive pulmonary disease. Health Psychol. 1998;17(3):232–240. doi:10.1037/0278-6133.17.3.2329619472
- EmeryCF, LeathermanNE, BurkerEJ, MacIntyreNR. Psychological outcomes of a pulmonary rehabilitation program. Chest. 1991;100(3):613–617. doi:10.1378/chest.100.3.6131889242
- EmeryCF, ShermerRL, HauckER, HsiaoET, MacIntyreNR. Cognitive and psychological outcomes of exercise in a 1-year follow-up study of patients with chronic obstructive pulmonary disease. Health Psychol. 2003;22(6):598–604. doi:10.1037/0278-6133.22.6.59814640857
- CoxNS, OliveiraCC, LahhamA, HollandAE. Pulmonary rehabilitation referral and participation are commonly influenced by environment, knowledge, and beliefs about consequences: a systematic review using the theoretical domains framework. J Physiother. 2017;63(2):84–93. doi:10.1016/j.jphys.2017.02.00228433238
- Keating A, Lee A, Holland AE. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chron Respir Dis. 2011;8(2):89–99. doi:10.1177/147997231039375621596892
- KeatingA, LeeAL, HollandAE. Lack of perceived benefit and inadequate transport influence uptake and completion of pulmonary rehabilitation in people with chronic obstructive pulmonary disease: a qualitative study. J Physiother. 2011;57(3):183–190. doi:10.1016/S1836-9553(11)70040-621843834
- TsaiLL, McNamaraRJ, ModdelC, AlisonJA, McKenzieDK, McKeoughZJ. Home-based telerehabilitation via real-time videoconferencing improves endurance exercise capacity in patients with COPD: the randomized controlled TeleR study. Respirology (Carlton, Vic). 2017;22(4):699–707. doi:10.1111/resp.12966
- AmbrosinoN, BrulettiG, ScalaV, PortaR, VitaccaM. Cognitive and perceived health status in patient with chronic obstructive pulmonary disease surviving acute on chronic respiratory failure: a controlled study. Intensive Care Med. 2002;28(2):170–177. doi:10.1007/s00134-001-1165-611907660
- QuanjerPH, TammelingGJ, CotesJE, PedersenOF, PeslinR, YernaultJC. Lung volumes and forced ventilatory flows. Report working party standardization of lung function tests, european community for steel and coal. Official statement of the european respiratory society. Eur Respir J Suppl. 1993;16:5–40. doi:10.1183/09041950.005s16938499054
- American ThoracicS. American College of Chest P. ATS/ACCP Statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2003;167(2):211–277.12524257
- BeaverWL, WassermanK, WhippBJ. A new method for detecting anaerobic threshold by gas exchange. J Appl Physio. 1986;60(6):2020–2027. doi:10.1152/jappl.1986.60.6.2020
- BorgGA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–381. doi:10.1249/00005768-198205000-000127154893
- MaltaisF, LeBlancP, JobinJ, et al. Intensity of training and physiologic adaptation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1997;155(2):555–561. doi:10.1164/ajrccm.155.2.90321949032194
- BourbeauJ, ColletJP, SchwartzmanK, DucruetT, NaultD, BradleyC. Economic benefits of self-management education in COPD. Chest. 2006;130(6):1704–1711. doi:10.1378/chest.130.6.170417166985
- HAS. Guide du parcours de soins - Bronchopneumopathie chronique obstructive. 2014:1–63
- BonnevieT, GravierFE, ElkinsM, et al. People undertaking pulmonary rehabilitation are willing and able to provide accurate data via a remote pulse oximetry system: a multicentre observational study. J Physiother. 2019;65(1):28–36. doi:10.1016/j.jphys.2018.11.00230573441
- KaramanliH, IlikF, KayhanF, PazarliAC. Assessment of cognitive impairment in long-term oxygen therapy-dependent COPD patients. Int J Chron Obstruct Pulmon Dis. 2015;10:2087–2094. doi:10.2147/COPD.S8832626491279
- VilleneuveS, PepinV, RahayelS, et al. Mild cognitive impairment in moderate to severe COPD: a preliminary study. Chest. 2012;142(6):1516–1523. doi:10.1378/chest.11-303523364388
- JonesPW. Interpreting thresholds for a clinically significant change in health status in asthma and COPD. Eur Respir J. 2002;19(3):398–404. doi:10.1183/09031936.02.0006370211936514
- ZigmondAS, SnaithRP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi:10.1111/j.1600-0447.1983.tb09716.x6880820
- Puente-MaestuL, PalangeP, CasaburiR, et al. Use of exercise testing in the evaluation of interventional efficacy: an official ERS statement. Eur Respir J. 2016;47(2):429–460. doi:10.1183/13993003.00745-201526797036
- BorelB, FabreC, SaisonS, BartF, GrosboisJM. An original field evaluation test for chronic obstructive pulmonary disease population: the six-minute stepper test. Clin Rehabil. 2010;24(1):82–93. doi:10.1177/026921550934384820053721
- CoquartJB, LemaitreF, CastresI, SaisonS, BartF, GrosboisJM. Reproducibility and sensitivity of the 6-minute stepper test in patients with COPD. Copd. 2015;12(5):533–538. doi:10.3109/15412555.2014.97473325526322
- GrosboisJM, RiquierC, ChehereB, et al. Six-minute stepper test: a valid clinical exercise tolerance test for COPD patients. Int J Chron Obstruct Pulmon Dis. 2016;11:657–663. doi:10.2147/COPD.S9863527099483
- SchouL, OstergaardB, RasmussenLS, Rydahl-HansenS, PhanarethK. Cognitive dysfunction in patients with chronic obstructive pulmonary disease–a systematic review. Respir Med. 2012;106(8):1071–1081. doi:10.1016/j.rmed.2012.03.01322579108
- CleutjensFA, WoutersEF, DijkstraJB, et al. The COgnitive-Pulmonary Disease (COgnitive-PD) study: protocol of a longitudinal observational comparative study on neuropsychological functioning of patients with COPD. BMJ Open. 2014;4(3):e004495. doi:10.1136/bmjopen-2013-004495
- Dal NegroRW, BonadimanL, TognellaS, BricoloFP, TurcoP. Extent and prevalence of cognitive dysfunction in chronic obstructive pulmonary disease, chronic non-obstructive bronchitis, and in asymptomatic smokers, compared to normal reference values. Int J Chron Obstruct Pulmon Dis. 2014;9:675–683. doi:10.2147/COPD.S6348525061286
- RonceroC, CampuzanoAI, QuintanoJA, MolinaJ, PerezJ, MiravitllesM. Cognitive status among patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2016;11:543–551. doi:10.2147/COPD.S10085027042043
- KozoraE, TranZV, MakeB. Neurobehavioral improvement after brief rehabilitation in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil. 2002;22(6):426–430. doi:10.1097/00008483-200211000-0000812464831
- EmeryCF, HonnVJ, FridDJ, LebowitzKR, DiazPT. Acute effects of exercise on cognition in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;164(9):1624–1627. doi:10.1164/ajrccm.164.9.210413711719300
- HerigstadM, FaullOK, HayenA, et al. Treating breathlessness via the brain: changes in brain activity over a course of pulmonary rehabilitation. Eur Respir J. 2017;50:3. doi:10.1183/13993003.01029-2017
- PichonR, CouturaudF, MialonP, et al. Responsiveness and minimally important difference of the 6-minute stepper test in patients with chronic obstructive pulmonary disease. Respiration. 2016;91(5):367–373. doi:10.1159/00044651727216848
- Holland AE, Mahal A, Hill CJ, et al. Home-based rehabilitation for COPD using minimal resources: a randomised, controlled equivalence trial. Thorax. 2017;72(1):57–65. doi:10.1136/thoraxjnl-2016-20851427672116
- HortonEJ, MitchellKE, Johnson-WarringtonV, et al. Comparison of a structured home-based rehabilitation programme with conventional supervised pulmonary rehabilitation: a randomised non-inferiority trial. Thorax. 2018;73(1):29–36. doi:10.1136/thoraxjnl-2016-20850628756402
- BonnevieT, GravierFE, DebeaumontD, et al. Home-based neuromuscular electrical stimulation as an add-on to pulmonary rehabilitation does not provide further benefits in patients with chronic obstructive pulmonary disease: a multicenter randomized trial. Arch Phys Med Rehabil. 2018;99(8):1462–1470. doi:10.1016/j.apmr.2018.01.02429457998
- BoutouAK, TannerRJ, LordVM, et al. An evaluation of factors associated with completion and benefit from pulmonary rehabilitation in COPD. BMJ Open Respir Res. 2014;1(1):e000051. doi:10.1136/bmjresp-2014-000051