Abstract
Rationale
Chronic obstructive pulmonary disease (COPD) is an increasingly prevalent lung disease linked to dysfunctional balance and an increased risk of falls. The Balance Evaluation Systems Test (BESTest) evaluates the six underlying subcomponents of functional balance. The aim of this study was to determine the specific balance subcomponents and cut-off scores that discriminate between fallers and non-fallers with COPD to guide fall risk assessment and prevention.
Methods
A secondary analysis of cross-sectional data from two prior studies in COPD was performed. Independent samples t-tests were used to explore the differences in the BESTest sub-system scores between fallers and non-fallers. Receiver operating characteristic curves were used to determine the optimal subcomponent cut-off scores that identified fallers, and the area under the curve (AUC) was used to assess test accuracy.
Results
Data from 72 subjects with COPD (mean age, 70.3 ± 7.4y; mean forced expiratory volume in 1 second, 38.9 ± 15.8% predicted) were analyzed. Two BESTest subcomponents, stability limits/verticality (fallers: 75.4%, non-fallers: 83.8%; p=0.002) and postural responses (fallers: 67.5%, non-fallers: 79.7%; p=0.008) distinguished between fallers and non-fallers. Stability limits/verticality had an AUC of 0.70 and optimal cut-off score of 73.8% for identifying fallers; postural responses had an AUC of 0.67 and optimal cut-off score of 69.4%.
Conclusion
The stability limits/verticality and postural responses subcomponents of the BESTest distinguished between fallers and non-fallers with COPD. The stability limits/verticality subcomponent can also be used to identify whether an individual with COPD is at risk of falling using a cut-off score of 73.8%. These findings suggest that specific subcomponents of balance could be targeted to optimize fall risk assessment and prevention in COPD.
Introduction
Chronic obstructive pulmonary disease (COPD) is an increasingly prevalent multi-system diseaseCitation1,Citation2 stemming from chronic airflow limitationCitation3 affecting between 174.5 and 384 million individuals globally.Citation3–Citation5 Symptoms of COPD are predominantly presumed to be respiratory-related such as dyspnea, coughing, sputum production, and wheezing;Citation3 however, secondary symptoms also include poor lower extremity function, decreased muscle strength, and balance impairments.Citation2,Citation6–Citation8 Balance impairments are specifically problematic as individuals with COPD are up to 55% more likely to suffer a fall compared to their non-COPD counterparts.Citation9 Falls are one of the leading causes of accidental injury death worldwide,Citation10 and can lead to devastating consequences such as injuries, decreased functioning, loss of independence, reduced quality of life, and an increased risk of morbidity and mortality.Citation11,Citation12 These risks are especially relevant in people with COPD given they have a high number of comorbidities, specifically osteoporosis,Citation13 which may lead to a greater risk of complications from a fall injury.
Decreasing falls incidence in COPD can be accomplished by conducting a balance assessment to evaluate whether individuals may be at risk for falling and providing balance-specific exercises to those at risk.Citation14 The Balance Evaluation Systems Test (BESTest) is the most comprehensive balance assessment tool available in any population and has strong construct validity in COPD.Citation6,Citation15–Citation17 The BESTest is comprised of six subcomponents to assess various areas of balance consistent with the systems framework for postural control: 1) biomechanical constraints, 2) stability limits/verticality, 3) anticipatory postural adjustments, 4) postural responses, 5) sensory orientation, and 6) stability in gait.Citation18 From these six subcomponents, the underlying systems leading to balance dysfunctions can be determined to guide fall prevention treatment.Citation18
Although previous research has demonstrated that total BESTest scores are able to differentiate between individuals with COPD with and without a fall history,Citation19 studies have not yet examined which specific subcomponents of the BESTest can best identify fallers. By identifying the balance subcomponents associated with fall risk in COPD, fall risk assessment and prevention strategies could be optimized to target the specific balance systems linked to falls in this population. The aim of this study was to determine which BESTest subcomponent scores could discriminate between fallers and non-fallers with COPD and to examine the accuracy and optimal cut-off scores for identifying fallers.
Methods
This study was a secondary analysis of data from 72 subjects who participated in either a randomized controlled trial (RCT) of balance training (n=35)Citation20 or a cross-sectional study on balance systems in COPD (n=37).Citation6 Both studies were conducted at West Park Healthcare Centre in Toronto, Canada, and inclusion/exclusion criteria were similar; participants required a diagnosis of COPD,Citation21 and were excluded if they were unable to communicate or had either neurological or musculoskeletal conditions that limited mobility.Citation6,Citation20 Additionally, participants in the RCT needed to have self-reported balance problems or a fall in the past five years,Citation20 and participants in the cross-sectional study had to have a smoking history of at least ten pack years.Citation6 The RCT had a total of 35 patients with 15 (42.9%) having reported a fall in the past year, and the cross-sectional study had a total of 37 patients with 19 (51.1%) having reported a fall in the past year. Fallers were defined as individuals with a history of at least one fall in the previous 12 months, with a fall being defined as an occasion where you find yourself unintentionally on a lower level.Citation22 Written informed consent was provided by all participants in both studies, study approval was obtained by the Bridgepoint/West Park research ethics board (No. 10–001; 13–011-WP),Citation6,Citation20 and was conducted in accordance with the Declaration of Helsinki.
Participants in both studies were assessed at baseline using the BESTest.Citation6,Citation20 The BESTest is a comprehensive balance assessment tool developed in 2009 to screen for balance impairments in six different postural control systems.Citation18 There are 36 tasks to complete in the BESTest that are divided into the following subcomponents; 5 in biomechanical constraints, 7 in stability limits/verticality, 6 in anticipatory postural adjustments, 6 in postural responses, 5 in sensory orientation, and 7 in stability in gait.Citation18 Each subcomponent of the BESTest assesses different systems of balance, which can be found in .
Table 1 BESTest Subcomponent Descriptions
Individuals are scored in each task by an assessor using a 4-point Likert scale with 0 being “worst performance” and 3 being “best performance”. Scores are calculated per system as well as for the total test, and can then be converted into percentages where the higher the score, the better the balance.Citation18 The BESTest has strong inter-rater reliability and validity in individuals with COPD.Citation19
Analyses
Statistical analyses were conducted using IBM SPSS Statistics version 25 (IBM Corp, Armonk, New York). Descriptive statistics were conducted in the form of means and standard deviations (SD) to summarize the sample. Variables that were explored included: age, body mass index (BMI), 6-minute walk distance, forced expiratory volume in one second (FEV1), forced vital capacity (FVC), FEV1/FVC ratio, males and females, Medical Research Council (MRC) dyspnea, and supplemental oxygen usage.
Two-tailed independent samples t-tests were used to examine whether the BESTest and its different subcomponents were able to discriminate between fallers and non-fallers with COPD. An α value of ≤0.0085 was considered significant based on a Šidák correction to prevent Type I Error for examining differences in the six subcomponents.Citation23 All BESTest scores and sub-scores were based on percentages out of 100. Effect sizes were calculated to understand the magnitude of differences between fallers and non-fallers based on the following equation: Cohen’s d = (M2 - M1) ⁄ SDpooled.Citation24
To identify the optimal cut-off score for identifying fallers for each of the BESTest subcomponent scores, receiver operating characteristic (ROC) curves were used. The datapoint closest to the left-hand corner of the curve was chosen as the cut-off that optimized both sensitivity and specificity. Based on convention, an acceptable area under the curve (AUC) was deemed as 0.7 or greater.Citation25
Results
Subject characteristics are provided in . A total of 34 (47%) participants were categorized as fallers and 38 (53%) as non-fallers. Participants were 70.3 years of age on average (SD=7.4) and had moderate to very severe COPD diagnoses (GOLD stages 2–4)Citation3 with a mean FEV1% predicted of 38.9% (SD=15.8). Participants had an average 6-minute walk test distance of 304.3m (SD=104.5), and 26 (36%) were supplemental oxygen users.
Table 2 Characteristics for Fallers (n=34) and Non-Fallers (n=38)
Results comparing the BESTest sub-scores in fallers versus non-fallers are provided in . Total BESTest scores were significantly different between fallers and non-fallers with a mean difference of 7.9%; p=0.005. Non-fallers had higher (better) BESTest scores within each subcomponent compared to fallers; however, this difference reached statistical significance (p=0.0085) only for stability limits/verticality and postural responses. Within the stability limits/verticality subcomponent of the BESTest, fallers significantly differed from non-fallers by a mean difference of 8.5%; p=0.002. Within the postural responses subcomponent, fallers significantly differed from non-fallers by a mean difference of 12.2%; p=0.008.
Table 3 BESTest Scores in Fallers (n=34) Compared to Non-Fallers (n=38)
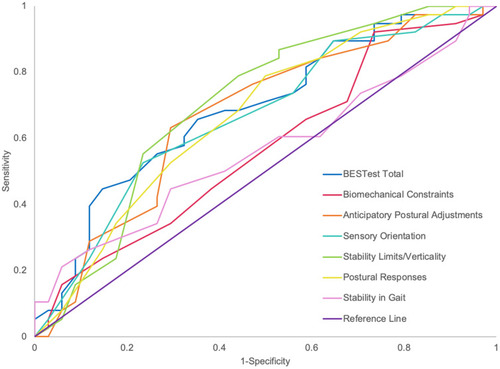
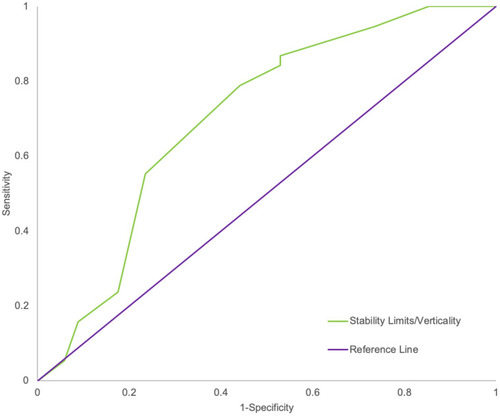
Results of the ROC curve analysis for each of the BESTest subcomponent scores are provided in , and the ROC curves are shown in . The only subcomponent score with an acceptable AUC (≥0.7) for identifying fallers was stability limits/verticality with an AUC of 0.70 (). The optimal cut-off for identifying fallers was 73.8% with a sensitivity and specificity of 0.87 and 0.47, respectively. The remaining subcomponent scores did not achieve an AUC of 0.7.
Table 4 BESTest Total and Subcomponent AUCs and Cut-off Scores
Discussion
Individuals with COPD have known balance dysfunctions and an increased fall risk. To our knowledge, this is the first study to examine the specific subcomponents of the BESTest that discriminate between fallers and non-fallers with COPD. The findings of this study indicate that stability limits/verticality and postural responses were the two subcomponents that best characterized fallers with COPD. Additionally, a cut-off score of 73.8% was found to have acceptable accuracy for identifying fallers within the stability limits/verticality subcomponent. These findings have relevant implications for optimizing fall risk assessment and prevention in COPD.
Consistent with previous work, our study found that the total BESTest score discriminated between fallers and non-fallers with COPD.Citation19 The mean difference between fallers and non-fallers’ total score was 7.9% in the current study with an effect size of 0.68, compared to 10.1% in Jácome (2016) with an effect size of 0.87.Citation19 Additionally, we showed that the stability limits/verticality and postural responses subcomponents of the BESTest were the only subcomponents that differentiate between fallers and non-fallers. Although the other subcomponents were not significantly different between fallers and non-fallers, it is important to note that the magnitude of the difference (8.2%) in anticipatory postural adjustments and sensory orientation subcomponents approached the previously reported clinically important difference on the full BESTest in COPD.Citation26 Taken together, this information may have relevance for informing fall prevention strategies in COPD by allowing therapists to target these specific underlying subsystems within fall prevention exercise programs (eg, functional reaching, perturbation training, body position changes and altering sensory stimuli).
This secondary analysis also determined that the stability limits/verticality subcomponent may be used to identify whether an individual with COPD is at risk of falling using a cut-off score of 73.8% within that subcomponent to identify fallers. The AUC for stability limits/verticality (0.70) was greater than the entire BESTest as well as all other subcomponents; and it was the only subcomponent to attain acceptable accuracy for screening. This suggests it may be possible to administer the stability limits/verticality tasks independent of the other subcomponents; instead of 36 tasks, only 7 tasks would need to be administered to gain similar information on fall risk. However, it is worth noting that the stability limits/verticality subcomponent had relatively low specificity (0.47) for identifying fallers. To our knowledge, this is the first study utilizing ROC curves to explore BESTest subcomponents to determine fall risk in individuals with COPD and thus we are unable to compare our findings to other literature. However, previous work in stroke patients has shown that four BESTest subcomponents (biomechanical constraints, anticipatory postural adjustments, sensory orientation, and stability in gait) had acceptable accuracy in identifying fallers.Citation27 Although these findings need to be validated prospectively, our results suggest that within this COPD cohort, stability limits/verticality sub-scores may have an important role both when trying to identify fall status and implement effective balance interventions. It is worth noting that the full BESTest and three other subcomponents (anticipatory postural adjustments, postural responses, and sensory orientation) demonstrated borderline acceptable accuracy with AUCs of 0.67 to 0.69.
It is interesting to note that the stability in gait subcomponent, which includes the Timed Up and Go Test (TUG), showed poor sensitivity (0.45) for identifying fallers. Although many studies have reported on use of the TUG in patients with COPD, there is very little evidence related to fall risk within this population. To our knowledge, only one prior study with a relatively small sample size has looked at the predictive validity of the TUG for falls in individuals with COPD. In this study (n=50), time to complete the TUG predicted fall recurrence with a sensitivity exceeding 0.90.Citation28 In contrast, a systematic review examining the TUG’s ability to predict fall risk in community-dwelling older adults found limited predictive ability for the TUG with a pooled sensitivity of only 0.31.Citation29 The mixed evidence across populations demonstrates the need for more research exploring the best tests for fall risk prediction in people with COPD.
One interesting finding of this study was supplemental oxygen usage in fallers vs non-fallers; 47% of non-fallers were on supplemental oxygen compared to only 24% of fallers. This finding is similar to a previous prospective cohort study where individuals with COPD who used supplemental oxygen were less likely to fall compared to those who were not supplemental oxygen users.Citation30 However, this is contrary to past cross-sectional and observational studies.Citation7,Citation8 While examining the link between supplemental oxygen usage and falls was not the primary aim of the current study, the conflicting findings highlight the need for further studies to elucidate risk factors for falls in this population.
Several limitations need to be taken into account when interpreting our results. The data were cross-sectional; thus, we are unable to determine whether balance impairments preceded or succeeded fall events. Participants reported falls in the past 12 months retrospectively, potentially leading to recall bias and underestimation of the number of fall events. Additionally, due to being a secondary analysis of two prior studies, the inclusion criteria varied slightly and there were different assessors evaluating BESTest performances, possibly leading to measurement error. This work was retrospective and therefore hypothesis generating; as such, future work would benefit from a prospective study to confirm which BESTest subcomponents accurately identify future fallers. Finally, it is possible there was insufficient power to detect differences in other subcomponents. Based on the data collected, a sample size upwards of 300 would have been needed to detect smaller differences in some subcomponents (eg, stability in gait and biomechanical constraints). However, given the smaller effect sizes noted for these subcomponents, these differences are unlikely to be clinically important.
Conclusion
In summary, the stability limits/verticality and postural responses subcomponents of the BESTest were able to differentiate between fallers and non-fallers with COPD. Additionally, stability limits/verticality may be used to identify whether an individual with COPD is at risk of falling using a cut-off score of 73.8%. However, the specificity of stability limits/verticality was low and prospective studies are needed to draw conclusions on its validity for fall risk assessment. If confirmed prospectively, these findings suggest that the stability limits/verticality and postural responses subcomponents may play a vital role in optimizing fall risk assessment and prevention in individuals with COPD.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
The authors thank the subjects who participated in this research and the respiratory program staff at West Park Healthcare Centre.
References
- FabbriLM, RabeKF. From COPD to chronic systemic inflammatory syndrome? Lancet. 2007;370(9589):797–799. doi:10.1016/S0140-6736(07)61383-X17765529
- EisnerMD, BlancPD, YelinEH, et al. COPD as a systemic disease: impact on physical functional limitations. Am J Med. 2008;121(9):789–796. doi:10.1016/j.amjmed.2008.04.03018724969
- Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease.; 2018.
- GBD. 2015 chronic respiratory disease collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet Respir Med. 2017;5(9):691–706. doi:10.1016/S2213-2600(17)30293-X28822787
- World Health Organization. Chronic Obstructive Pulmonary Disease (COPD).; 2017 https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd). Accessed 617, 2020.
- BeauchampMK, SibleyKM, LakhaniB, et al. Impairments in systems underlying control of balance in COPD. Chest. 2012;141(6):1496–1503. doi:10.1378/chest.11-170822116798
- BeauchampMK, HillK, GoldsteinRS, Janaudis-FerreiraT, BrooksD. Impairments in balance discriminate fallers from non-fallers in COPD. Respir Med. 2009;103(12):1885–1891. doi:10.1016/j.rmed.2009.06.00819592229
- RoigM, EngJJ, MacIntyreDL, et al. Falls in people with chronic obstructive pulmonary disease: an observational cohort study. Respir Med. 2011;105(3):461–469. doi:10.1016/j.rmed.2010.08.01520869227
- HakamyA, BoltonCE, GibsonJE, McKeeverTM. Risk of fall in patients with COPD. Thorax. 2018;73(11):1079–1080. doi:10.1136/thoraxjnl-2017-21100829563161
- World Health Organization. Falls: key facts. 2018 https://www.who.int/news-room/fact-sheets/detail/falls. Accessed 617, 2020.
- World Health Organization. WHO Global Report on Falls Prevention in Older Age. World Health Organization; 2008.
- SocietyAG, SocietyG, OfAA, On Falls PreventionOSP, American Geriatrics Society, British Geriatrics Society, American Academy of Orthopaedic Surgeons Panel on Falls Prevention. Guideline for the prevention of falls in older persons. J Am Geriatr Soc. 2001;49(5):664–672. doi:10.1046/j.1532-5415.2001.49115.x11380764
- ChatilaWM, ThomashowBM, MinaiOA, CrinerGJ, MakeBJ. Comorbidities in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2008;5(4):549–555. doi:10.1513/pats.200709-148ET18453370
- Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148–157. doi:10.1111/j.1532-5415.2010.03234.x21226685
- OliveiraCC, LeeA, GrangerCL, MillerKJ, IrvingLB, DenehyL. Postural control and fear of falling assessment in people with chronic obstructive pulmonary disease: a systematic review of instruments, international classification of functioning, disability and health linkage, and measurement properties. Arch Phys Med Rehabil. 2013;94(9):1784–1799.e7. doi:10.1016/j.apmr.2013.04.01223632285
- BeauchampMK. Balance assessment in people with COPD: an evidence-based guide. Chron Respir Dis. 2019;16:147997311882031. doi:10.1177/1479973118820311
- SibleyKM, BeauchampMK, Van OoteghemK, StrausSE, JaglalSB. Using the systems framework for postural control to analyze the components of balance evaluated in standardized balance measures: A scoping review. Arch Phys Med Rehabil. 2015;96(1):122–132.e29. doi:10.1016/j.apmr.2014.06.02125073007
- HorakFB, WrisleyDM, FrankJ. The balance evaluation systems test (BESTest) to differentiate balance deficits. Phys Ther. 2009;89(5):484–498. doi:10.2522/ptj.2008007119329772
- JacomeC, CruzJ, OliveiraA, MarquesA. Validity, reliability, and ability to identify fall status of the berg balance scale, BESTest, Mini-BESTest, and Brief-BESTest in patients with COPD. Phys Ther. 2016;96(11):1807–1815. doi:10.2522/ptj.2015039127081201
- BeauchampMK, Janaudis-FerreiraT, ParreiraV, et al. A randomized controlled trial of balance training during pulmonary rehabilitation for individuals with COPD. Chest. 2013;144(6):1803–1810. doi:10.1378/chest.13-109323975185
- RabeK, HurdS, AnzuetoA, et al. Global initiative for chronic obstructive lung disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176(6):532–555. doi:10.1164/rccm.200703-456SO17507545
- BidermanA. Depression and falls among community dwelling elderly people: a search for common risk factors. J Epidemiol Community Health. 2002;56(8):631–636. doi:10.1136/jech.56.8.63112118057
- SidakZ. Rectangular confidence regions for the means of multivariate normal distributions. J Am Stat Assoc. 1967;62(318):626–633.
- CohenJ. Statistical Power Analysis for the Behavioral Sciences. Academic press; 2013.
- TerweeCB, BotSDM, de BoerMR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42. doi:10.1016/j.jclinepi.2006.03.01217161752
- BeauchampMK, HarrisonSL, GoldsteinRS, BrooksD. Interpretability of change scores in measures of balance in people with COPD. Chest. 2016;149(3):696–703. doi:10.1378/chest.15-071726203790
- MiyataK, KaizuY, UsudaS. Prediction of falling risk after discharge in ambulatory stroke or history of fracture patients using balance evaluation systems test (BESTest). J Phys Ther Sci. 2018;30(4):514–519. doi:10.1589/jpts.30.51429706697
- ReynaudV, MutiD, PereiraB, et al. A TUG value longer than 11 s predicts fall risk at 6-month in individuals with COPD. J Clin Med. 2019;8(10):1752. doi:10.3390/jcm8101752
- BarryE, GalvinR, KeoghC, HorganF, FaheyT. Is the Timed Up and Go test a useful predictor of risk of falls in community dwelling older adults: a systematic review and meta- analysis. BMC Geriatr. 2014;14(1):14. doi:10.1186/1471-2318-14-1424484314
- OliveiraCC, LeeAL, McGinleyJ, et al. Falls by individuals with chronic obstructive pulmonary disease: a preliminary 12-month prospective cohort study: fall risk in COPD. Respirology. 2015;20(7):1096–1101. doi:10.1111/resp.1260026206432