Abstract
Purpose
Chronic obstructive pulmonary disease (COPD) related to wood smoke exposure is characterized by important inflammation of the central and peripheral airways without significant emphysema. The objective of this study is to describe the bronchial hyperresponsiveness (BHR) level in women with COPD related to wood smoke exposure and to compare it with the BHR in women with COPD related to tobacco smoking.
Materials and methods
Two groups of women with stable COPD were studied: (1) wood smoke exposed (WS-COPD); and (2) tobacco smoke exposed (TS-COPD). A methacholine challenge test (MCT) was performed in all patients according to American Thoracic Society criteria. BHR levels were compared using the methacholine concentration, which caused a 20% fall in the FEV1 (PC20).
Results
Thirty-one patients, 19 with WS-COPD and 12 with TS-COPD, were included. There were no significant differences between the groups in baseline FVC, FEV1, IC, FEF25–75, and FEF25–75/FVC. All 31 patients had a positive MCT (PC20 < 16 mg/mL) and the fall in the FEV1 and IC was similar in both groups. The severity of BHR was significantly higher in the WS-COPD patients (PC20: 0.39 mg/mL) than in the TS-COPD patients (PC20: 1.24 mg/mL) (P = 0.028). The presence of cough, phlegm, and dyspnea during the test were similar in both groups.
Conclusion
We found moderate to severe BHR in women with WS-COPD, which was more severe than in the TS-COPD women with similar age and airflow obstruction. This paper suggests that the structural and inflammatory changes induced by the chronic exposure to wood smoke, described in other studies, can explain the differences with TS-COPD patients. Future studies may clarify our understanding of the impact of BHR on COPD physiopathology, phenotypes, and treatment strategies.
Introduction
Fifty percent of the world population, approximately three billion people, use solid fuels (charcoal or biomass materials) as their main or alternative household energy source.Citation1 In developing countries, especially in the rural areas, the use of wood, dung, and crop residues are common resources for cooking and heating, and even in developed countries, are sometimes used for heating. The indoor air pollution derived from burning biomass fuels causes significant global morbidity and mortality, especially in developing countries,Citation2–Citation4 and has been consistently related to chronic bronchitis, chronic obstructive pulmonary disease (COPD), and acute respiratory infections in children.Citation5–Citation9 Chronic exposure to biomass smoke, including wood smoke, is currently considered to be a risk factor for COPD.Citation7–Citation9
In rural areas in Colombia, wood is widely used for cooking, especially by women. Due to high migration rates from rural to urban settings over the last few decades, wood smoke COPD (WS-COPD) in women has become more frequent in Colombia’s biggest cities.Citation5,Citation10 Previous studies have shown clinical, radiographic, and functional differences between WS-COPD and tobacco smoke COPD (TS-COPD). In WS-COPD, the central and peripheral airways are predominantly affected, with minimal or no emphysema defined by CT scan and functional findings.Citation11,Citation12
Bronchial hyperresponsiveness (BHR), a frequent finding in COPD patients, can precede the symptoms and the diagnosis of COPD, and has been related to a more rapid decline in FEV1.Citation13–Citation15 Therefore, BHR is considered by some researchers to be a risk factor for chronic bronchitis and COPD.Citation16,Citation17 However, the true importance and physiopathological role of BHR in COPD patients has not been clearly established and it is unknown whether its presence and severity is related to the inflammatory changes of the airways.Citation18 The aim of this study is to describe BHR in women with WS-COPD and establish a comparison with TS-COPD.
Material and methods
Patients
This is a cross-sectional study. Therefore, the sample was established from consecutive ambulatory patients of the COPD Program of the Fundacion Neumologica Colombiana (Bogotá, Colombia), with the following inclusion criteria: (1) women older than 40 years; (2) COPD diagnosis based on symptoms, FEV1/FVC < 70%, FEV1 < 80% of the predicted value, and pre–post bronchodilator change of FEV1 ≤ 12% and 200 mL; (3) history of significant exposure to tobacco smoke (>20 packs/year) or wood smoke (>20 years); (4) clinical stability in the last six weeks defined as no changes in treatment and no acute exacerbations. Exclusion criteria included history of exposure to both risk factors (tobacco and wood smoke); less than one year of exposure cessation; contraindications for methacholine challenge test (MCT); a particularly severe airflow obstruction (FEV1 < 50%); and respiratory disease other than COPD, especially asthma (medical diagnosis or high probability: recurrent episodes of wheezing starting before 40 years old) and allergic rhinitis. The patients were divided into two groups: (1) WS-COPD, wood smoke-exposed (no exposure to tobacco smoke); and (2) TS-COPD, tobacco smoke-exposed (no exposure to wood smoke). The study was approved by the Institutional Ethics Committee and all participants signed informed consent forms.
Measurements
Spirometry
A V-MAX 20C (Sensormedics®, Yorba Linda, CA) was used to perform the flow-volume curves and to measure the inspiratory capacity (IC) at baseline and after each methacholine concentration using the ATS (American Thoracic Society)/European Respiratory Society standardized methodsCitation19 and the Crapo’s reference values.Citation20 Patients were instructed and trained to perform the IC maneuvers. IC was selected as the highest value from three acceptable maneuvers done at baseline and after each stage of the MCT. The FEF25–75/FVC quotient was calculated for each patient.
BHR measurement
BHR was evaluated using a MCT that was performed according ATS criteria.Citation21 Any drug that could affect the MCT results was withdrawn. A five-breath dosimeter protocol was used with progressive concentrations of methacholine (Provocholine® Methapharm, Inc): 0.0625 mg/mL, 0.25 mg/mL, 1 mg/mL, 4 mg/mL, and 16 mg/mL. The best FEV1 and IC data from the acceptable and repeatable maneuvers were registered. The test ended when the FEV1 fell ≥20% from baseline or the five-stage protocol was completed. At the end of the test, all patients received salbutamol 400 μg using a dose-metered pressurized inhaler with a space chamber. The presence of cough, phlegm, and wheezing, as well as the respiratory rate, heart rate, and the pulse oxymetry (SpO2) were registered at each stage of the test. Dyspnea during usual daily activities was evaluated immediately before the MCT using the five-stage Medical Research Council scaleCitation22 and during the MCT using the Borg Scale.Citation23
BHR interpretation
The severity of BHR was established according to the methacholine concentration (mg/mL), which produced a 20% fall in the FEV1 (PC20) as follows: normal response, PC20 > 16; borderline BHR, PC20 4.0–16; mild BHR, PC20 1–4.0; and, moderate to severe BHR, PC20 < 1.0.Citation21
Statistical analysis
Mean and standard deviation for continuous variables and proportions for categorical variables were determined using SPSS statistics software (version 10.0; SPSS, Chicago, IL. The geometric mean of PC20 was calculated for each group (WS-COPD and TS-COPD). The differences were estimated using the Student’s t-test for continuous variables with normal distribution and the Mann–Whitney U test for non-normal variables. The chi-square test or the Fisher’s exact test were used for the categorical variables when the expected frequency was smaller than five. Univariate correlation between age and PC20 was also calculated. A two-tailed hypothesis was stated with a significance level of <0.05 (P-value).
Results
Baseline characteristics
Thirty-one women with COPD were included in this study, 19 with WS-COPD and 12 with TS-COPD. The WS-COPD group reported 42 ± 15 years of exposure to wood smoke, and the TS-COPD group reported 43 ± 13 packs/year of smoking. There were no significant differences in age, body mass index, inspiratory capacity, or spirometry values at baseline (). Furthermore, there were no significant differences in the COPD medications such as inhaled salbutamol (WS-COPD: 50% versus TS-COPD: 42%, P = 0.47), inhaled ipratropium bromide (67% versus 67%, P = 1.00), inhaled steroids (33% versus 42%, P = 0.42), and theophylline (22% versus 8%, P = 0.62).
Table 1 Baseline characteristics of patients
Metacholine challenge testing
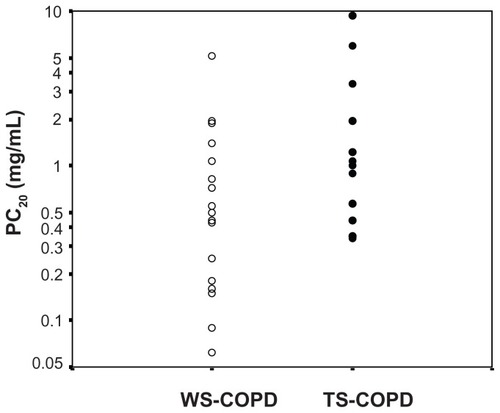
Both WS-COPD and TS-COPD patients had a positive result for the MCT (PC20 < 16 mg/mL). The fall in the FEV1 and the IC at the end of the test was similar in both groups (, ). The BHR level was significantly higher in the WS-COPD group than in the TS-COPD group (0.39 versus 1.24 mg/mL, P = 0.028). The majority of the WS-COPD patients had moderate to severe BHR (PC20 < 1 mg/mL) compared to the TS-COPD patients who were similarly distributed in moderate to severe and in mild BHR (PC20 1–4.0 mg/mL) (). After the administration of salbutamol, the FEV1 and IC similarly returned to the baseline value in both groups. There was no correlation between age and PC20 (r2 = 0.34, P = 0.324).
Table 2 Characteristics at the end of the methacholine challenge test
Figure 1 Decline in FEV1 and IC (% predicted) after the methacholine challenge test for WS-COPD and TS-COPD groups.
Note: Error bars ± 1 SD.
Abbreviations: COPD, chronic obstructive pulmonary disease; WS-COPD, wood smoke COPD; TS-COPD, tobacco smoke COPD; FEV1, forced expiratory volume in the first second; IC, inspiratory capacity; MCT, methacholine challenge test; SD, standard deviation.
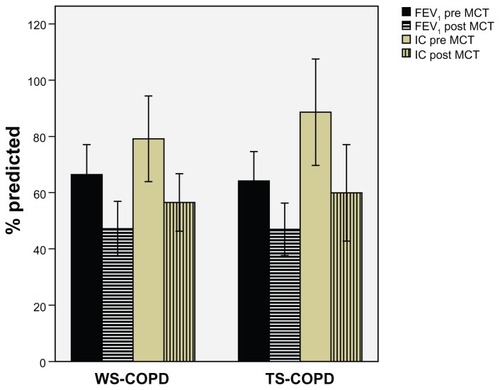
Figure 2 BHR severity according to PC20 for each patient.
Abbreviations: COPD, chronic obstructive pulmonary disease; WS-COPD, wood smoke COPD; TS-COPD, tobacco smoke COPD; BHR, bronchial hyperresponsiveness; PC20, provocative concentration causing a 20% fall in FEV1.
Symptoms and signs
There were no differences between the WS-COPD and TS-COPD groups in terms of chronic dyspnea, which was measured by the Medical Research Council scale (), at the end of the methacholine challenge test according to the Borg Scale (), neither in cough (WS-COPD: 77.8% versus TS-COPD: 63.6%, P = 0.34) nor phlegm (WS-COPD: 22.2% versus TS-COPD: 36.4%, P = 0.34). All the patients showed a significant increase in their respiratory rate, but no significant changes were observed in the heart rate or pulse oximetry (). Although wheezing was found more frequently in the WS-COPD patients (WS-COPD: 44% versus TS-COPD: 27%), the difference was not statistically significant (P = 0.30).
Discussion
This study found that patients with COPD related to wood smoke have more severe BHR than patients with COPD related to tobacco smoke with similar levels of baseline airflow obstruction, age, duration of smoke exposure, respiratory symptoms, and current medication use. All patients had BHR, but among the WS-COPD patients, the BHR was more frequently moderate to severe, while half of the TS-COPD patients had mild hyperresponsiveness.
BHR is related to age, sex, respiratory symptoms, airway size (diameter), baseline lung function, lung size, airway size disproportion, and treatment. Previous studies have found an increase in the prevalence of BHR in older adults.Citation24 However, in this study, the age of the WS-COPD and the TS-COPD patients was similar, and an additional analysis found no correlation between age and PC20. Because women have higher BHR and experience more negative impacts from smoking tobacco than men,Citation25–Citation27 this study only included women as subjects in order to avoid the possible effect of gender. BHR is also linked to airflow obstruction severity, expressed by FEV1, and the disproportion between airway diameter and lung volume, which is indirectly estimated by FEF25–75/FVC – the lower the FEV1 and FEF25–75/FVC, the higher the BHR.Citation28,Citation29 In this study, the FEV1 and the FEF25–75/FVC were similar in both groups. The IC, which is a useful measurement of dynamic hyperinflation during spontaneous and methacholine-induced acute bronchoconstriction in asthmatic patients,Citation30 was also similar at baseline and after the MCT for both groups. During the methacholine test, no differences were observed between the two groups in terms of respiratory symptoms such as changes in cough, phlegm, or dyspnea. Similarly, no significant differences in the recent stable treatment were found. Finally, according to the ATS criteria, the appropriate drugs were withdrawn before the methacholine challenge test.
Therefore, none of the mentioned factors associated with BHR could explain the higher severity of BHR in the WS-COPD group, which suggests that other factors, likely related to different characteristics of the disease in these two groups, could be involved. In previous studies, we have described significant differences between WS-COPD and TS-COPD patients. In an initial study, comparing 86 WS-COPD patients with 53 TS-COPD patients, we found that women with WS-COPD had a less severe decrease in carbon monoxide diffusing capacity (DL,CO) when compared to women with TS-COPD with a nearly normal transfer coefficient (DL,CO/VA).Citation11 This functional pattern suggests a predominance of small airway disease in WS-COPD patients, similar to what has been described in patients with airflow obstruction, compromise of peripheral small airways, and mild or no emphysema.Citation31,Citation32 This hypothesis was confirmed in a further study that used a qualitative evaluation of high-resolution CT scan and found that WS-COPD women frequently had sub-segmentary atelectasis, severe thickening of the bronchial walls, bonchiectasis, and mild or no emphysema in comparison with TS-COPD patients who showed a significantly higher index of emphysema with mild changes in airways.Citation12 These functional and tomographic findings can be correlated with those observed in a retrospective study of 103 autopsies of subjects exposed to wood smoke in which the main findings were hypertensive changes of the pulmonary vessels, peribronchial, perivascular, and interstitial depositions of anthracotic pigment, and the absence of emphysema.Citation33 The descriptions of the bronchoscopic abnormalities found in women exposed to wood smoke include mucosal hyperemia and edema, irregular reduction of the lumen, and in some cases, severe anthracotic plaques.Citation34
Based on the results of this study and previous observations, we speculate that the higher BHR observed in WS-COPD patients could be related to differences in the structure and inflammatory response of their airways, compared to TS-COPD patients. The relationship between BHR and airway inflammation in patients with COPD related to tobacco smoke has not been clearly defined.Citation35 In some studies, the correlation between inflammatory markers like exhaled nitric oxide or sputum eosinophils and the PC20 has been weak, but others have shown that the more severe the airway inflammation, the higher the rate of BHR.Citation36,Citation37 In addition, no functional indexes evaluating the lung parenchyma structure like pressure-volume curves or diffusion capacity (DL,CO) have been related to BHR, which suggests that BHR is more closely related to airway abnormalities (inflammation and lumen reduction) in COPD patients.Citation38 However, no differences have been observed between BHR in patients with chronic bronchitis and those with emphysema.Citation39
BHR is considered a risk factor for COPD as it may precede its symptoms, and is associated with the early decline of lung functions in healthy young adults, accelerated impairment of airflow obstruction in COPD patients, and higher mortality.Citation13,Citation15,Citation17 The cross-sectional design of this study does not allow us to conclude that BHR is a risk factor for COPD related to wood smoke, but the finding of more severe BHR in WS-COPD than in TS-COPD patients suggests that it may play a role in the physiopathology of WS-COPD that is possibly related to airway inflammation.
Some limitations of this study include the relatively small number of patients and the absence of other measurements of airway inflammation such as bronchial biopsies or cellular and biochemical sputum examinations. However, the rigorous selection of the patients according to exposures favored the conformation of very different groups and a reliable comparison. Because WS-COPD is more frequent in women, we excluded males; therefore, the results of this study cannot be generalized to men with COPD.
Conclusion
This study found the occurrence of moderate to severe BHR in women with WS-COPD that was more severe than in TS-COPD women with similar age and airflow obstruction. We speculate that the structural and inflammatory changes induced by the chronic exposure to wood smoke, described in other studies, explains the BHR severity in WS-COPD patients and the differences when compared to TS-COPD patients. Future studies may clarify our understanding of the impact of BHR on COPD physiopathology, phenotypes, and treatment strategies.
Acknowledgments
We thank Dr Juliana Ferreira and Dr Sonia Buist for the manuscript review.
Disclosure
The authors report no conflicts of interest in this work.
References
- World Resources Institute UNEP UNDP World Bank1998–1999 World Resources: a Guide to the Global EnvironmentOxfordOxford University Press1998
- BruceNPerez-PadillaRAlbalakRIndoor air pollution in developing countries: a major environmental and public health challengeBull World Health Organ2000781078109211019457
- SmithKRNational burden of disease in India from indoor air pollutionProc Natl Acad Sci U S A200097132861329311087870
- EzzatiMKammenDMThe health impacts of exposure to indoor air pollution from solid fuels in developing countries: knowledge, gaps, and data needsEnviron Health Perspect20021101057106812417475
- DennisRJMaldonadoDNormanSBaenaEMartinezGWoodsmoke exposure and risk for obstructive airways disease among womenChest19961091151198549171
- Perez-PadillaRRegaladoJVedalSExposure to biomass smoke and chronic airway disease in Mexican women. A case-control studyAm J Respir Crit Care Med19961547017068810608
- PauwelsRABuistASCalverleyPMJenkinsCRHurdSSGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summaryAm J Respir Crit Care Med20011631256127611316667
- Torres-DuqueCMaldonadoDPerez-PadillaREzzatiMViegiGon behalf of the Forum of International Respiratory Societies (FIRS) Task Force on Health Effects of Biomass ExposureBiomass fuels and respiratory diseases: a review of the evidenceProc Am Thorac Soc2008557759018625750
- HuGZhouYTianJRisk of chronic obstructive pulmonary disease from exposure to biomass smoke: a meta-analysisChest2010138203120139228
- CaballeroATorres-DuqueCAJaramilloCPrevalence of COPD in Five Colombian Cities Situated at Low, Medium, and High Altitude (PREPOCOL Study)Chest200813334334917951621
- GonzálezMPáezSJaramilloCBarreroMMaldonadoDEnfermedad pulmonar obstructiva crónica (EPOC) por humo de lena en mujeres. [Chronic obstructive pulmonary disease (COPD) produced by wood smoke in women]Acta Med Colomb2004291725 Spanish
- GonzálezMMaldonadoDPérezJVarónHPseudoenfisema en mujeres con EPOC por humo de lena en Bogotá (2600 m) [Pseudophysiologic emphysema in women with wood smoke COPD in Bogota (2600 m)]Arch Bronconeumol20044031 Spanish
- TashkinDPAltoseMDConnettJEKannerRELeeWWWiseRAMethacholine reactivity predicts changes in lung function over time in smokers with early chronic obstructive pulmonary disease. The Lung Health Study Research GroupAm J Respir Crit Care Med1996153180218118665038
- XuXRijckenBSchoutenJPWeissSTAirways responsiveness and development and remission of chronic respiratory symptoms in adultsLancet1997350143114349371166
- HospersJJPostmaDSRijckenBWeissSTSchoutenJPHistamine airway hyperresponsiveness and mortality from chronic obstructive pulmonary disease: a cohort studyLancet20003561313131711073020
- VestboJPrescottEUpdate on the “Dutch hypothesis” for chronic respiratory diseaseThorax199853Suppl 2S151910193342
- PostmaDSBoezenHMRationale for the Dutch hypothesis. Allergy and airway hyperresponsiveness as genetic factors and their interaction with environment in the development of asthma and COPDChest2004126Suppl 296S104S15302769
- van denBMPolosaRKerstjensHAPostmaDSThe role of endogenous and exogenous AMP in asthma and chronic obstructive pulmonary diseaseJ Allergy Clin Immunol200411473774615480309
- MillerMRHankinsonJBrusascoVStandardisation of spirometryEur Respir J20052631933816055882
- CrapoROMorrisAHGardnerRMReference spirometric values using techniques and equipment that meet ATS recommendationsAm Rev Respir Dis19811236596647271065
- CrapoROCasaburiRCoatesALGuidelines for methacholine and exercise challenge testing-1999. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999Am J Respir Crit Care Med200016130932910619836
- Surveillance for respiratory hazards in the occupational setting [American Thoracic Society]Am Rev Respir Dis19821269529567149469
- BorgGAPsychophysical bases of perceived exertionMed Sci Sports Exerc1982143773817154893
- ScichiloneNMessinaMBattagliaSCatalanoFBelliaVAirway hyperresponsiveness in the elderly: prevalence and clinical implicationsEur Respir J20052536437515684304
- KannerREConnettJEAltoseMDGender difference in airway hyperresponsiveness in smokers with mild COPD. The Lung Health StudyAm J Respir Crit Care Med19941509569617921469
- PrescottEBjergAMAndersenPKLangePVestboJGender difference in smoking effects on lung function and risk of hospitalization for COPD: results from a Danish longitudinal population studyEur Respir J1997108228279150319
- LanghammerAJohnsenRGulsvikAHolmenTLBjermerLSex differences in lung vulnerability to tobacco smokingEur Respir J2003211017102312797498
- LitonjuaAASparrowDWeissSTThe FEF25-75/FVC ratio is associated with methacholine airway responsiveness. The normative aging studyAm J Respir Crit Care Med19991591574157910228129
- UrrutiaICapelasteguiAQuintanaJMAssociation between the forced midexpiratory flow/forced vital capacity ratio and bronchial hyper-responsivenessArch Bronconeumol200440397402 Spanish15458615
- TantucciCEllaffiMDuguetADynamic hyperinflation and flow limitation during methacholine-induced bronchoconstriction in asthmaEur Respir J19991429530110515404
- GelbAFHoggJCMullerNLContribution of emphysema and small airways in COPDChest19961093533598620705
- GelbAFZamelNHoggJCMullerNLScheinMJPseudophysiologic emphysema resulting from severe small-airways diseaseAm J Respir Crit Care Med19981588158199731010
- PalaciosDMendezONeumopatía por humo de lena. Un estudio en autopsias [Pneumopathy due to inhaling firewood smoke. Autopsy findings from the San Juan de Dios Hospital]Biomédica199818153160 Spanish
- RestrepoJReyesPde OchoaPPatinoENeumoconiosis por inhalación de humo de lena [Pneumoconiosis due to inhalation of wood smoke]Acta Med Colomb19838191204 Spanish
- PostmaDSKerstjensHACharacteristics of airway hyperresponsiveness in asthma and chronic obstructive pulmonary diseaseAm J Respir Crit Care Med1998158S1871929817744
- LapperreTSSnoeck-StrobandJBGosmanMMDissociation of lung function and airway inflammation in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med200417049950415172889
- MullenJBWiggsBRWrightJLHoggJCParePDNonspecific airway reactivity in cigarette smokers. Relationship to airway pathology and baseline lung functionAm Rev Respir Dis19861331201253510577
- VerhoevenGTVerbraakAFBoere-van der StraatSHoogstedenHCBogaardJMInfluence of lung parenchymal destruction on the different indexes of the methacholine dose-response curve in COPD patientsChest200011798499010767228
- VermaVKCockcroftDWDosmanJAAirway responsiveness to inhaled histamine in chronic obstructive airways disease. Chronic bronchitis vs emphysemaChest1988944574613409723