Abstract
Background
Patients with chronic obstructive pulmonary disease (COPD) have some limitations during activities of daily living that involve the arms. There is little information on the benefits of shoulder girdle training and its repercussions for activities of daily living in patients with COPD. The purpose of this study was to investigate whether shoulder girdle training with diagonal movements increases upper limb muscle strength and improves performance of activities of daily living in patients with COPD.
Methods
Thirty-five patients with moderate to severe COPD (forced expiratory volume in one second 1.22 ± 0.49 L) and aged 36–80 years were recruited. Endurance time, maximal sustained weight, oxygen saturation, heart rate, respiratory rate, dyspnea, and arm fatigue were evaluated during an incremental upper limb test and eight simulated activities of daily living before and after an 8-week exercise training program.
Results
A significant gain was observed for upper limb strength (P < 0.05). At the peak of the upper limb incremental test, the respiratory rate dropped from 33 to 27 breaths per minute, the Borg dyspnea score decreased from 2 to 0.5, and the upper limb fatigue score decreased from 3 to 2 (P < 0.05). No change was seen in any of these parameters during performance of activities of daily living.
Conclusion
Although shoulder girdle training increased upper limb strength, no improvement was detected in performance of activities of daily living.
Introduction
Patients with chronic obstructive pulmonary disease (COPD) have altered respiratory mechanics and impaired gas exchange, which decrease physical ability and affect activities of daily living (ADL). According to Belman,Citation1 functional loss in COPD patients is also related to gradual loss of muscle conditioning, leading to early anaerobiosis and associated dyspnea at increasingly lower effort levels.
The objective of pulmonary rehabilitation is to reverse the inactivity status of these patients by physical training. Training of the lower limbs has been widely emphasized, but little is known about the effects of upper limb training on ADL,Citation1 and it is important to consider that approximately 80% of ADL are performed using the upper limbs.Citation2
Tangri and WoolfCitation3 reported over three decades ago that patients with COPD have difficulty performing ADL involving the upper limbs, eg, hair combing and tying shoelaces. They observed a change in the respiratory pattern, which became quick, shallow, and irregular in subjects attempting these activities. It has also been shown that patients with severe COPD have asynchronous thoracoabdominal movements during arm exercise, which leads them to stop exercise due to dyspnea.Citation4 Dyspnea is the primary activity-limiting symptom leading to reduced functional ability in patients with COPD. Patients with severe COPD report a marked increase in the sensation of dyspnea during routine tasks that require arm use, especially activities requiring unsupported arm elevation.Citation5
Ries et alCitation6 were the first researchers to evaluate upper body exercise and activities involving the arms in patients with COPD. They showed that training against gravity using an arm cycle ergometer or diagonal movements based on modified proprioceptive neuromuscular facilitation did not bring about any significant change in ability to perform simulated ADL. However, they showed that patients who trained using an arm cycle ergometer had less dyspnea and upper limb muscle fatigue than a control group. Ries et al concluded that specific upper limb training may be beneficial as part of an exercise rehabilitation program for patients with COPD, pointing out that this issue required further study.
Velloso et alCitation7 studied patients with moderate to severe COPD during repetitive tasks involving the arms. While sweeping the floor, erasing a board, lifting pots, and changing a light bulb, the patients became dyspneic and demonstrated high rates of oxygen consumption (43%–61% VO2max) and minute ventilation (51%–62% of maximum voluntary ventilation).
Addition of upper extremity resistance training to a rehabilitation program showed benefits in arm function, muscle strength, and arm exercise capacity in patients with COPD.Citation8 However, it is uncertain how these benefits affect the patient’s capacity to perform ADL. Thus, the objective of the present study was to determine whether shoulder girdle training using diagonal movements in patients with COPD could increase upper limb muscle strength and if this kind of training could change the performance of these patients on eight common ADL.
Materials and methods
This was a nonrandomized clinical trial evaluating 50 patients with COPD referred to the pulmonary rehabilitation program at the Pulmonary Rehabilitation Center of the Federal University of São Paulo/Associação de Assistência à Criança Deficiente (Unifesp/AACD), Brazil. The study was previously approved by the research ethics committee at our institution and patients signed an informed consent form. Inclusion criteria were a diagnosis of COPD according to the Global Initiative for Obstructive Lung Disease 2011,Citation9 no associated limiting disease, including cardiac, orthopedic or neurological problems, and ability to participate in an 8-week exercise training program.
Protocol
The patients were evaluated before and after the 8-week pulmonary rehabilitation program, which included three sessions per week. Each session included 30 minutes of walking on a treadmill at 80% of maximum heart rate, 30 minutes of arm exercises using diagonal movements, and 30 minutes of stretching and relaxing. A 40-minute education class was held weekly. No instructions for home exercise were given because the training program was performed in the rehabilitation center.
Spirometry
Three acceptable maneuvers (Koko® PFT system) were obtained according to American Thoracic Society reproducibility and acceptance criteria. Spirometry was repeated 15 minutes after the use of salbutamol 400 μg.
ADL test
The following activities were evaluated: teeth brushing, face washing, hair combing, taking shirt off, putting shirt on, putting shoes on, taking shoes off, shaving for men, and waxing for women.
Evaluation during ADL test
The following parameters were monitored during the performance of each activity before and after the rehabilitation program:
Oxygen saturation (Healthdyne Oximeter, Marietta, GA, USA), using a finger sensor placed on the middle finger of the nondominant hand of the patient
Heart rate, using a sensor placed around the thorax of the patient (Polar Pulsimeter, Kempele, Finland)
Dyspnea and upper limb fatigue, measured using the Borg scale going from zero (none) to ten (extreme); patients were asked to point out a number that best described what they were feeling at that moment.Citation10
Incremental upper limb test
The incremental upper limb test was designed to determine the maximal weight at which the patients could exercise for 2 minutes. The exercise consisted of lifting a weight with the dominant arm and performing the second diagonal of the proprioceptive neuromuscular facilitation technique.Citation11 This diagonal movement started from the contralateral side over the iliac crest, followed by flexion, abduction, and external rotation of the arm with shoulder and fist flexion. Two-minute bouts of exercise with a one-minute resting interval were repeated until exhaustion. The test started with a 0.5 kg dumbbell which was increased in weight by 0.5 kg at each new bout of exercise. Patients were encouraged to continue exercising until exhaustion. The test could be halted if limiting symptoms occurred, such as dyspnea, fatigue, and/or pain in the upper limb, or any symptom impairing continuation of exercise. The exercise test could be interrupted by the observer if the patient developed compensatory thoracic movements to accomplish the exercise or if the complete amplitude of shoulder movement was not being reached. Heart rate, respiratory rate, oxygen saturation, dyspnea, and upper limb fatigue were measured before and at the end of exercise.
Upper limb training
Each session lasted 30 minutes. The load was individually determined and corresponded to 50% of the maximum load achieved in the incremental upper limb test. Training was performed based on fundamental principles of modified proprioceptive neuromuscular facilitation patterns of movement with the Kabat method, using two functional diagonal movementsCitation11 with the patient in the upright position.
The rationale for use of proprioceptive neuromuscular facilitation is based on the fact that execution of movements in a diagonal-spiral pattern with a rotary component are three-dimensional, involving several joints and recruiting more muscle groups compared with other exercises. When accompanied by resistance, these movements provide muscle recruitment. The first diagonal technique includes flexion-adduction-external rotation of the shoulders, while the second diagonal technique includes flexion-abduction-external rotation.Citation11,Citation12 Others have demonstrated the beneficial effect of the proprioceptive neuromuscular facilitation method in patients with COPD, including improvement in their arm functional capacity and reduction in dyspnea and fatigue ratings.Citation13 Each diagonal exercise lasted one minute and the diagonals were alternated between the two arms. The number of repetitions was individually established for each patient according to their physical capacity.
Statistical analysis
Data are presented as the mean ± standard deviation or median and percentile (25%–75%) depending on the distribution shown by the Kolmogorov-Smirnov test. Training variables before and after exercise training were analyzed using the Wilcoxon test.Citation14 The sample size was calculated based on variability of the time of the incremental test (E/S) where E/S is the magnitude of the expected effect divided by the standard deviation of the outcome variable, with an α error of 5% and a β error of 20%, according to the results from previous studies.Citation15 Thirty patients were required to comply with the established research power requirements. The significance level was set at P < 0.05.
Results
Thirty-five of 50 patients met the inclusion criteria and were entered into the study. The study subjects were of mean age 64.5 ± 8.7 years and comprised 83% males and 17% females (). There was no change in forced expiratory volume in one second or in resting values for oxygen saturation and heart rate after the rehabilitation program. There was a decrease in the median respiratory rate in isoload [22 to 24 respiratory movements per minute (P < 0.05)] during the upper limb incremental test after rehabilitation (). An increase in the maximum load sustained at the end of the upper limb incremental test (P < 0.05) was seen ().
Table 1 Characteristics of 35 patients with chronic obstructive pulmonary disease submitted to a shoulder girdle exercise program
Figure 1 (A) Respiratory rate at isoload during incremental upper limb test before and after training of the upper limbs. (B) Load in kilograms at the end of the incremental test of upper limbs, before and after training. (C) Duration in seconds of the incremental upper limb test, before and after training of the upper limbs.
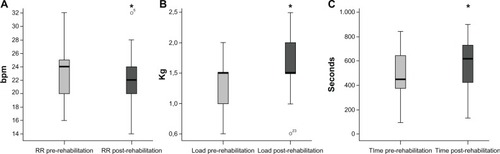
There was no difference in the median maximum load sustained in the upper limb incremental test comparing before and after rehabilitation tests (1.5 kg). However, the 75th percentile was reached significantly more often after rehabilitation than at baseline (P < 0.05), as shown in . Patients also showed an increase in endurance time on the test (616 versus 447 seconds, ).
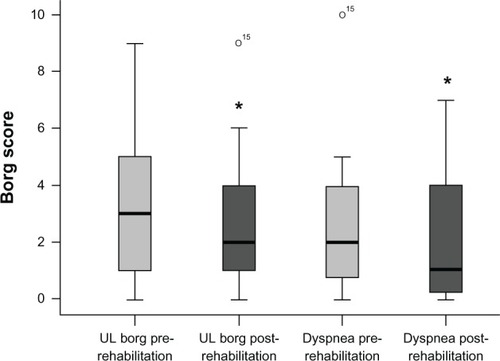
There was a significant (P = 0.033) decrease in median Borg scores for upper limb fatigue in the incremental test, both in isoload (from 3 to 2) and in maximum load achieved (from 9 to 6). There was also a reduction in median Borg dyspnea score in isoload from 2 to 1 ().
Figure 2 Borg score for tiredness of the upper limbs and dyspnea at the end of the incremental upper limb test before and after upper limb training.
The Borg dyspnea score during teeth brushing was the only parameter that showed a significant decrease (P < 0.05) in the post-training period. No difference was found for oxygen saturation, heart rate, or dyspnea after exercise rehabilitation during performance of ADL concerning face washing, hair combing, taking off a shirt, putting a shirt on, putting shoes on, taking shoes off, and shaving.
Although there was an improvement in the load the patients were able to sustain and a decrease in upper limb fatigue during the incremental test, there was no correlation between these variables and performance of ADL. Patients showed good compliance with the training program, with over 80% attendance.
Discussion
The main findings of this study were an increase in maximum load sustained at the end of the upper limb incremental test, a reduction in dyspnea in isoload, and fatigue of the upper limbs during performance of ADL. Patients also showed an increase in maximum load sustained during the incremental upper limb test at the post rehabilitation assessment.
Lower limb muscle weakness has often been reported in patients with COPD, and contributes to lack of exercise tolerance. Controversial information regarding upper limb muscle adaptation and influence of muscle wasting on muscle weakness has been reported. Franssen et alCitation16 evaluated leg and arm muscle function in patients with stable COPD and preserved fat-free mass, and concluded that lower and upper limb muscle dysfunction was observed in COPD patients regardless of preserved fat-free mass depletion.
Generalized muscle weakness suggests systemic muscular involvement, although preserved arm endurance and poor response of arm performance to exercise training is indicative of intrinsic differences between adaptation of leg and arm muscles. It has been shown that the ventilatory pattern of COPD patients is modified when simple activities involving the upper limbs are performed.Citation2,Citation3
Reardon et alCitation17 observed that exertional dyspnea often causes patients with COPD to reduce their ADL unconsciously in order to limit the intensity of their distress. In this situation, reduction in performing ADL leads to sedentary behavior which, in turn, further increases dyspnea. Both dyspnea and fatigue are important factors affecting health-related quality of life in patients with COPD.
Paz-Diaz et alCitation18 evaluated a rehabilitation program that included disease education, energy conservation techniques, relaxation, and exercise comprising 20 minutes of arm elevation with dumb bells three times a week for 8 weeks. They observed that this type of program led to a significant improvement in severity of depression, a decrease in symptoms, an increase in performance of ADL, a decrease in St George’s Respiratory Questionnaire total score, and less dyspnea. However, it may be argued that simple arm elevation does not recruit all the arm muscles required during ADL.
Patients in our study performed specific training of the upper limbs based on modified proprioceptive neuromuscular facilitation principles using two diagonal movements, with 50% of the maximal load detected in the incremental test. These movements are based on physiological principles and follow muscle fiber anatomy, in addition to recruiting a large number of muscles, mainly those of the shoulder girdle.Citation12 We observed that 22 of our 35 patients could support a significantly higher load after exercise rehabilitation, indicating that training using diagonal movements is effective in increasing upper limb strength.
In addition, we observed a significant decrease in Borg dyspnea score and a decrease in the respiratory rate. It may be argued that the patients experienced desensitization to dyspnea after training, but perhaps the lower dyspnea scores are due to the lower respiratory rate. Beyond the decrease in upper limb fatigue, as evaluated by Borg score, we cannot suggest that there was a clinical improvement because no statistically significant benefit was observed. Our results are in agreement with those reported by Ries et al,Citation19 suggesting that although upper limb strength may increase after training, this does not necessarily mean that there is an improvement in fatigability of these limbs.
Just one (brushing teeth) of the eight ADL parameters evaluated showed a significant decrease in dyspnea during its performance after the training period (P < 0.05). No heart rate, respiratory rate, or oxygen saturation changes were statistically significant after training in any of the ADL. This shows that the training proposed in this study was not adequate for the activities performed. Even though the diagonal movements used recruit a large number of muscles of the shoulder girdle, they do not recruit muscles such as brachial biceps and triceps, which are actively involved in many of the ADL evaluated in this study.
Other tests can be used to evaluate the effectiveness of upper limb training, such as the 6-minute pegboard and ring test,Citation20 the disabilities of arms, shoulder and hand (DASH) questionnaire,Citation21 and the unsupported upper limb exercise test.Citation22 However, the 6-minute pegboard and ring test is not functional, which limits evaluation of ADL, the DASH is a subjective tool developed to assess symptoms and physical function in patients with musculoskeletal disorders of the upper extremities, and the unsupported upper limb exercise test is an incremental test of upper limb strength. Given that our objective was to evaluate the ability of our patients to complete activities that best expressed normal ADL, we chose to assess nine activities that our patients performed on a daily basis.
Arm cycle ergometry is still considered to be the gold standard for upper limb training. Although it increases strength, it does not improve performance in ADL.Citation4 Therefore, shoulder girdle training should aim specifically at activities that are performed regularly by individual patients. We strongly suggest that a study should be performed comparing both training methods in order to identify which one would be more appropriate and effective in improving performance of ADL. Our study did not include a control group because it has already been demonstrated that arm training has level A evidence of efficacy.Citation19
We conclude that shoulder girdle training in patients with COPD using diagonal movements is efficient in improving upper limb strength. However, it is not effective in producing a change in the performance of some ADL.
Acknowledgments
The authors are grateful to Carolina Aguiar for her help in reviewing and editing the manuscript. This study was partially funded by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPQ), Brazil.
Disclosure
The authors report no conflicts of interest in this work.
References
- BelmanMJExercise in chronic obstructive pulmonary diseaseChest19867585595
- PotterWAOlafssonSHyattREVentilatory mechanics and expiratory flow limitation during exercise in patients with obstructive lung diseaseJ Clin Invest1971509109195547281
- TangriSWoolfCRThe breathing pattern in chronic obstructive lung disease during the performance of some common daily activitiesChest1973631261294684100
- CelliBRassuroJMakeBJDyssynchronous breathing during arm but not leg exercise in patients with chronic airflow obstructionN Engl J Med1986314148514903702963
- BreslinEHDyspnea-limited response in chronic obstructive pulmonary disease: reduced unsupported arm activitiesRehabil Nurs19921712201535920
- RiesALEllisBHawkinsRWUpper extremity exercise training in chronic obstructive pulmonary diseaseChest1988936886923349825
- VellosoMStellaSGCendonSMetabolic and ventilatory parameters of four activities of daily living accomplished with arms in COPD patientsChest200341047105312684292
- FerreiraTJHillKGoldsteinRSResistance arm training in patients with COPD: a randomized controlled trialChest201113915115820724740
- Global Initiative for Chronic Obstructive Lung Disease. Executive Summary: Global Strategy for the Diagnosis, Management, and Prevention of COPD. Updated Dec 2011 Available from: http://www.ncbi.nlm.nih.gov/pubmed/17507545Accessed November 15, 2012
- BorgGBorg’s Perceived Exertion and Pain ScalesChampaign, ILHuman Kinetics1998
- SurburgPRSchraderJWProprioceptive neuromuscular facilitation techniques in sports medicine: a reassessmentJ Athl Train199732343916558430
- KabatHStudies on neuromuscular dysfunction. XV. The role of central facilitation in restoration of motor function in paralysisArch Phys Med19523352153312977510
- MartinezFJVogelPDDupontDNStanopoulosIGrayABeamisJFSupported arm exercise vs unsupported arm exercise in the rehabilitation of patients with severe chronic airflow obstructionChest1993103139714028486017
- SigelSSiegel S. Nonparametric StatisticsThe American Statistician19571131319
- HulleySBCummingsSRBrownerWSGradyDGNewmanTBDesigning Clinical Research: An Epidemiologic ApproachLippincott Williams & Wilkinssecond edition2000
- FranssenFMBroekhuizenRJanssenPPWoutersEFScholsAMLimb muscle dysfunction in COPD: effects of muscle wasting and exercise trainingMed Sci Sports Exerc2005372915632660
- ReardonJZLareauSCZuWallackRFunctional status and quality of life in chronic obstructive pulmonary diseaseAm J Med2006119323716996897
- Paz-DiazHMontes de OcaMLopezJMCelliBRPulmonary rehabilitation improves depression, anxiety, dyspnea and health status in patients with COPDAm J Phys Med Rehabil200786303617304686
- RiesALBauldoffGSCarlinBWPulmonary rehabilitation: joint ACCP/AACVPR evidence-based clinical practice guidelinesChest200713148428
- ZhanSCernyFJGibbonsWJMadorMJWuYWDevelopment of an unsupported arm exercise test in patients with chronic obstructive pulmonary diseaseJ Cardiopulm Rehabil200626318018716738459
- HudakPLAmadioPCBombardierCThe Upper Extremity Collaborative Group (UECG) development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand)Am J Ind Med19962966026088773720
- TakahashiTJenkinsSCStraussGRWatsonCPLakeFRA new unsupported upper limb exercise test for patients with chronic obstructive pulmonary diseaseJ Cardiopulm Rehabil200323643043714646791