Abstract
Background
Physical inactivity is strongly associated with worse prognosis in Chronic Obstructive Pulmonary Disease (COPD), and assessment of physical function is very important. The six minute walking test (6MWT) is an established test known to predict mortality in COPD, and 30 seconds chair stand test (30sCST) is a potential alternative test. The study aimed to investigate and compare the associations of 6MWT and 30sCSTs with mortality.
Methods
Data on patient demographics, established mortality predictors and results from 6MWT and 30sCST were collected from 2016 to 2019 from 97 consecutively included patients with COPD. In August 2021, mortality data were retrieved from patient records. Correlation analysis of 6MWT and 30sCST was performed. The predictive abilities of 6MWT and 30sCST, respectively, were analyzed using Kaplan Meyer-curves and Cox regression with adjustment for sex, age, body mass index below 22 and comorbid cardiovascular disease.
Results
A positive correlation between 6MWT and 30sCST was shown (r = 0.61, p < 0.0001). Independent associations with mortality were found for 6MWD 250–349 (HR (95% CI) 3.19 (1.12 to 9.10), p = 0.030) and 6MWD <250 (4.27 (1.69 to10.8), p = 0.002) compared with 6MWD ≥350 meters, and for 30sCST <4 (3.31 (1.03 to 10.6), p = 0.045) compared with 30sCST≥11 risings. When both 6MWT and 30sCST were included in the multivariable model, 6MWD 250–349 (3.09 (1.02 to 9.37), p = 0.046) and 6MWD <250 (3.57 (1.26 to 10.1), p = 0.016) compared with 6MWD ≥350 meters predicted mortality.
Conclusion
30sCST and 6MWT correlates moderately and are independently associated with mortality in patients with COPD. Although 6MWT is the best predictor of mortality, 30sCST may be used as an alternative to identify patients at risk.
Introduction
Chronic obstructive pulmonary disease (COPD) is the third most common global cause of death.Citation1 The disease can be caused by tobacco smoking, occupational exposure to smoke, dust and gas and exposure to biomass burning in poorly ventilated indoor areas.Citation2 Another less common but well-studied cause is alpha-1-antitrypsin deficiency.Citation3 Higher age, higher burden of tobacco smoking, more frequent exacerbations, worse health status, lower lung function, lower body mass index (BMI) and comorbid cardiovascular disease (CVD) are all known to be associated with mortality in COPD.Citation2–8 However, physical activity has been reported to be the strongest predictor of increased mortality risk.Citation9
Impaired physical activity in COPD can be caused by respiratory and peripheral skeletal muscle dysfunction, including both sarcopenia and reduced function in the remaining muscles.Citation1,Citation10 Muscular dysfunction, in turn, can arise due to deteriorated nutrition, chronic systemic inflammation, hypoxemia and comorbidity.Citation1 The Global Initiative for Obstructive Lung Disease (GOLD) recommend that skeletal muscles and their impact on physical activity in COPD can be improved regardless of the patient’s lung function.Citation1
Physical function in COPD can be assessed using for example six minute walking test (6MWT) and chair stand test (CST) (also called sit to stand test) during 30 or 60 seconds.Citation10 The 6MWT measures the walking distance for six minutes, can identify an increased risk for mortality or hospitalizationCitation11,Citation12 and evaluate the effect of rehabilitation in COPD.Citation13 CST measures physical function and muscle strength in the lower extremity by assessing a number of risings from sitting on a chair, for 30 or 60 seconds.Citation14 Both CST variants are able to identify low physical function in patients with COPD,Citation15 and 60sCST has been shown to predict mortality.Citation16 30sCST causes less hemodynamic strain than 60sCST and 6MWT and may be an alternative test for patients with COPD and limited physical function due to dyspnoea or gait disabilities. Data on the predictive ability of 30sCST, and comparative studies of 30sCST and 6MWT are still lacking. Thus, our study aimed to investigate the correlation between 6MWT and 30sCST, and to explore and compare their associations with mortality, in patients with COPD.
Methods
Data Collection
This was a cohort study of 97 patients with COPD, consecutively enrolled and examined from 2016 to 2019 at outpatient care at the Department of Respiratory Medicine, Örebro University Hospital, Örebro, Sweden. The inclusion criterion was a clinical COPD diagnosis confirmed by spirometry showing a ratio of forced expiratory volume in one second (FEV1) and forced vital capacity (FVC) below 0.7. Exclusion criteria were metastasized cancer or any other severe disease with an expected survival of fewer than 3 months, and cognitive or linguistic inability to perform function tests and questionnaires. All patients had to be in a stable phase with no exacerbations for the previous four weeks. Data on sex, age, BMI, smoking history, current inhaled maintenance COPD treatment, comorbid cardiovascular disease and exacerbations previous 12 months were collected in connection to the visit by the responsible physician and senior author. A physiotherapist performed spirometry, physical test, and health status assessment. Spirometry was performed after bronchodilator administration of terbutaline 1 mg and health status was measured by the Swedish version of COPD assessment test (CAT). CAT is a validated disease-specific health status instrument including 8 items on symptoms and function. The score ranges from zero to 40, with higher scores indicating worse health status.Citation17 A COPD exacerbation was defined as worsening symptoms requiring an oral steroid course, with or without antibiotics.Citation18 Information on comorbid cardiovascular disease and the number of exacerbations (total and hospitalized) were retrieved from medical record review. Cardiovascular disease (CVD) was defined as a recorded diagnosis of hypertension, ischemic heart disease, heart failure or cerebrovascular disease.
Complete data on all-cause mortality was obtained from the digital record system. The record system is connected to the compulsory update of the Swedish population registration, and subsequently automatically updated on vital status.
Physical Tests
The 6MWT was performed according to the European Respiratory Society/American Thoracic Society (ERS/ATS) protocol, by walking back and forth between two cones at a distance of 30 meters. Patients were instructed to walk for as long as possible, for six minutes, and walking aids such as a walker or cane were allowed if needed. The lowest saturation during the test was noted.Citation13 At the 30sCST, the patient was asked to rise and sit at a chair, with arms crossed and parallel feet, as many times as possible for 30 seconds.Citation15 The order of the physical tests varied randomly between individuals, and the patients were given enough time to recover from dyspnoea and fatigue.
Statistics
Patient characteristics were investigated with cross-tabulations, distributed over vital status at censoring of the study on of August 31st, 2021. Categorical variables were investigated with the chi-2 test and continuous variables with the t-test. Age was categorized as ≤70, 71–80, >80 years and BMI was categorized as < or ≥ 22 kg/m2 based on previous knowledge of mortality risk in COPD.Citation7 Burden of smoking was presented as current smoking status (ex, current or never smoking) and as the number of pack years. COPD severity was presented as spirometric stage 1–4 and groups A to D according to GOLD.Citation2 The walking distance at 6MWT (6MWD) and the number of risings at 30sCST were divided into groups based on previous literature and normal values, ≥350, 250–349 and <250 meters, and <4, 4–10 and ≥11 risings, respectively.Citation13,Citation19
The correlation between 6MWT och 30sCST was investigated using a scatter diagram and Pearson correlation analysis. The degree of correlation was assessed using Cohens proposal where a correlation coefficient <0.45 denotes low correlation, 0.45–0.70 moderate correlation, and >0.70 high correlation.Citation20 The associations of walking distance at 6MWT and number of risings at 30sCST with mortality were analyzed in separate models using Kaplan–Meier curves and Cox regression. In univariable Cox regression analysis, sex, age, and the previously known predictors BMI < 22, number of pack years, present cardiovascular disease, FEV1 in percentage of predicted (FEV1%pred), exacerbation frequency, and CAT score were also investigated.Citation2–8 The multivariable Cox regression adjusted for sex, age and factors that were found to be statistically significant in the univariable analyses. Finally, 6MWT and 30sCST were included in a common multivariable Cox regression model.
Ethics
The study complies with the Declaration of Helsinki and was approved by the Regional Ethical Board in Uppsala, Sweden (Dnr 2015–445). All patients were informed about the purpose of the study and provided written consent before inclusion.
Results
In total, 97 patients were included, with 53% women and a mean age of 72 years. The mean FEV1pred was 50%, the mean 6MWD was 287 meters and the mean 30sCST was 6.8 repetitions. Walking aids during the 6MWT were used by 15 patients (walker, n = 13 or cane, n = 2). After a mean follow-up time of 34 months, 39 (40%) of the patients were deceased ().
Table 1 Patient Characteristics at Baseline
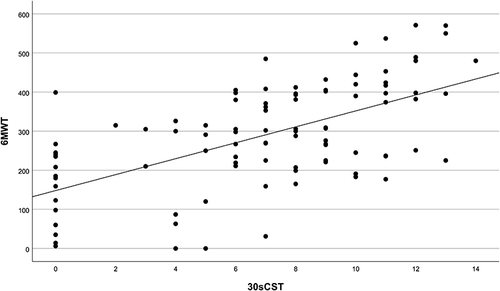
The results from 6MWT and 30sCST showed a statistically significant correlation (r = 0.61, p = 0.0001, ).
Figure 1 Scatterplot of the correlation between 6MWT and 30sCST (r = 0.61, p <0.0001).
The Kaplan-Meyer-curve showed a survival-rate of 83% for 6MWD > 350, 52% for 6MWD 250–349, and 44% for 6MWD <250 meters (). The Kaplan-Meyer-curve for 30sCST showed a survival rate of 80% for >11 repetitions, 63% for 4–11 repetitions, and 30% for <4 repetitions ().
Figure 2 6MWT and mortality. Kaplan–Meier curves showing survival distributed over 6MWT groups.
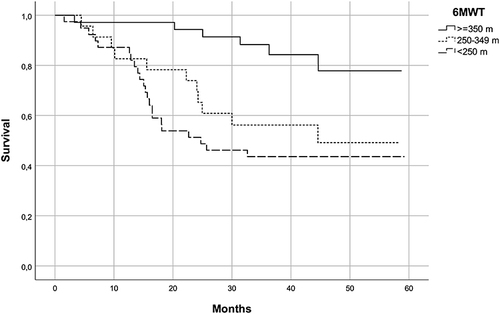
Figure 3 30sCST and mortality. Kaplan–Meier curves showing survival distributed over 30sCST groups.
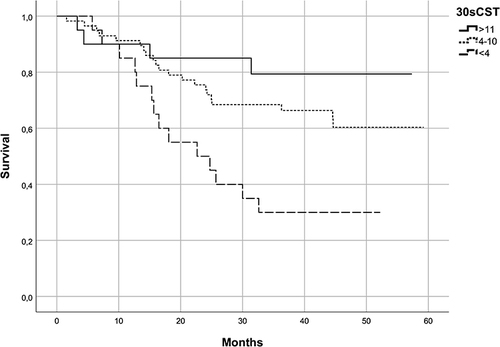
In univariable analyses, statistically significant associations with mortality were found for 6MWD 250–349, and <250 compared with ≥ 350 meters (, ). Significant associations with mortality were also found for 30sCST <4 repetitions compared with ≥11 repetitions (, ). Associations with mortality for age >80 compared with ≤ 70 years and comorbid CVD were also found to be significant (). Multivariable analysis including 6MWD, age and CVD showed independent associations with mortality for 6MWD 250–349 and <250 compared with ≥350 meters (). Multivariable analysis including 30sCST, age, and CVD showed independent associations with mortality for <4 repetitions compared with ≥11 repetitions (). When 6MWD and 30sCST were included in the same multivariable model, the association between 6MWD 250–349 meters and <250 meters and mortality remained statistically significant (HR (95% CI) 3.09 (1.02 to 9.37), p = 0.046 and 3.57 (1.26 to 10.1) p = 0.016, respectively).
Table 2 Cox Regression Analysis of 6MWT, n = 97
Table 3 Cox Regression Analysis of 30sCST, n = 97
Discussion
The primary findings of this study are that both 6MWT and 30CST predict mortality in patients with COPD. Secondary findings are that the tests correlate moderately, and that 6MWT seems to be the better predictor of the two tests. The association of 30sCST and mortality, and the comparison of 6MWT and 30sCST are novel findings.
As a low physical activity level is known to be associated with higher mortality risk in COPD, it is of utmost importance to have appropriate tests for identifying patients at risk and in need of individually adapted rehabilitation, to increase their physical function and thereby decrease the risk for rehospitalization and death.Citation9 6MWT and 30sCST are both examples of such tests. We report a moderate correlation of 6MWT and 30sCST with r = 0.61, which is consistent with previous studies reporting correlations of r = 0.53 between 6MWT and 30sCSTCitation19 and r = 0.75 between 6MWT and 60sCST.Citation22 These results indicate that the 30sCST may be used as a replacement for 6MWT if needed.
Our finding that 6MWD below 350 meters is associated with mortality confirms the reports from several previous studies.Citation12,Citation23 As for 30sCST, our result is consistent with a study showing that 60sCST predicts mortality,Citation16 and with a study assessing the association between mortality and the time used to perform 5 risings at CST.Citation24 However, to our best knowledge, no previous study has reported an association between mortality and the 30sCST. We find it clinically important that this very short, feasible, and easy-to-use version of CST could still identify patients with a higher mortality risk. 30sCST may be a more suitable physical test for patients with severe COPD with limitations due to dyspnoea already at a low level of activity, since 30sCST causes less hemodynamic strain than 6MWT in COPD.Citation22 30sCST could also be considered as a replacement for 6MWT in patients with COPD and gait disabilities such as impaired balance or pain. 30sCST measures leg muscle strength and can identify patients in need of exercise training to improve activities of daily living.Citation19 Finally, 30sCST may be more feasible and easy to use in a stressed clinical situation than 6MWT.
There are shorter versions of the CST, such as the 5-repetition CST mentioned above. The advantage of 30sCST versus 5-repetition CST is that even though the patient cannot perform a single rising from the chair, you will get a result when testing with 30sCST. When using the 5-repetition CST you have to perform 5 risings to get a result, making that version of the CST less appropriate in the population with COPD, that often suffers from skeletal muscle dysfunction.
In our study, 14 patients were not able to perform a single rising when tested with 30sCST but managed to perform at 6MWT. It is known that patients with COPD change their gait biomechanics due to the effect of skeletal muscle dysfunction on the thigh muscle,Citation25,Citation26 which could explain why the patients managed to walk but not rise from a sitting position. At the 6MWT, patients were allowed to use a walking aid which might add to the explanation of why they could perform at the 6MWT but not rise from a sitting position. It is possible that 6MWT is more appropriate for patients with severe skeletal muscle dysfunction and weak thigh muscles.
Our simultaneous Cox regression analysis of 6MWT and 30sCST showed that 6MWT is the best predictor, which confirms previous comparisons.Citation21,Citation22 6MWT is likely more sensible since it explores several aspects of physical function, both muscular endurance and cardiovascular strain, and therefore is more sensitive for finding patients at high risk of mortality.
In summary, both 6MWT and 30sCST measure physical function in patients with COPD but they measure different aspects of physical function. Ideally, they should be used together to complement each other, but as they correlate moderately and 30sCST also predicts mortality, the tests can be used separately.
Our analyses also confirmed the previously well-known predictive ability of high age, BMI below 22 kg/m2, and CVD in COPD.Citation2,Citation4,Citation7 Our study also showed that the patients deceased at the end of the study had a significantly lower oxygen saturation level at 6MWT, which is consistent with previous studies.Citation11 In previous studies, a lower level of physical activity has been shown in patients with COPD and comorbid CVD compared with only COPD,Citation27 which makes the performance of physical tests even more important in patients with both COPD and CVD. The fact that FEV1%pred, CAT score and the number of exacerbations did not differ between patients deceased and alive at censoring of the study is most likely due to the fact that the sample mainly includes patients with severe COPD, with generally poor outcomes in all patients.
Strengths of our study are the generous inclusion criteria and that we collected complete data on several mortality predictors constituting potential confounders. One limitation is that as the patients were recruited in secondary care, the majority of the sample had severe COPD. However, even though the generalizability of the results to patients with mild COPD in primary care may be restricted, all stages of COPD were represented in our study.
The clinical implication of this study is that both 6MWT and 30sCST can be used to identify patients with low physical function and increased mortality risk, with high needs for physical training to improve muscular function and decrease symptoms.Citation10 Future research should focus on identifying the patients with COPD who are most appropriate to test with 30sCST and confirm the optimal cut-off point for mortality prediction in larger populations.
Conclusion
We conclude that 30sCST and 6MWT correlates moderately and are both independently associated with mortality in patients with COPD. Although 6MWT is the best predictor of mortality, 30sCST can be used as a complement or an alternative to identify at-risk patients.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
We thank Maria Petersson and Doris Danielsson for performing data collection and functional tests together with the principal author and Jenny Johansson for performing record reviews.
References
- Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi:10.1016/S0140-6736(12)61728-0
- Vestbo J, Hurd SS, Agusti AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347–365. doi:10.1164/rccm.201204-0596PP
- Pini L, Tiberio L, Venkatesan N, et al. The role of bronchial epithelial cells in the pathogenesis of COPD in Z-alpha-1 antitrypsin deficiency. Respiratory Research. 2014;15(1):112. doi:10.1186/s12931-014-0112-3
- Anthonisen NR, Connett JE, Murray RP. Smoking and lung function of Lung Health Study participants after 11 years. Am J Respir Crit Care Med. 2002;166(5):675–679. doi:10.1164/rccm.2112096
- Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005;60(11):925–931. doi:10.1136/thx.2005.040527
- Casanova C, Marin JM, Martinez-Gonzalez C, et al. Differential effect of modified medical research council dyspnea, COPD assessment test, and clinical COPD questionnaire for symptoms evaluation within the new GOLD staging and mortality in COPD. Chest. 2015;148(1):159–168. doi:10.1378/chest.14-2449
- Landbo C, Prescott E, Lange P, Vestbo J, Almdal TP. Prognostic value of nutritional status in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999;160(6):1856–1861. doi:10.1164/ajrccm.160.6.9902115
- Mannino DM, Thorn D, Swensen A, Holguin F. Prevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPD. Eur Respir J. 2008;32(4):133–147. doi:10.1183/09031936.00012408
- Waschki B, Kirsten A, Holz O, et al. Physical activity is the strongest predictor of all-cause mortality in patients with COPD: a prospective cohort study. Chest. 2011;140(2):331–342. doi:10.1378/chest.10-2521
- Spruit MA, Singh SJ, Garvey C, et al. Rehabilitation, An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–e64. doi:10.1164/rccm.201309-1634ST
- Casanova C, Cote C, Marin JM, et al. Distance and oxygen desaturation during the 6-min walk test as predictors of long-term mortality in patients with COPD. Chest. 2008;134(4):746–752. doi:10.1378/chest.08-0520
- Durheim MT, Smith PJ, Babyak MA, et al. Six-minute-walk distance and accelerometry predict outcomes in chronic obstructive pulmonary disease independent of Global Initiative for Chronic Obstructive Lung Disease 2011 Group. Ann Am Thorac Soc. 2015;12(3):349–356. doi:10.1513/AnnalsATS.201408-365OC
- Singh SJ, Puhan MA, Andrianopoulos V, et al. An official systematic review of the European Respiratory Society/American Thoracic Society: measurement properties of field walking tests in chronic respiratory disease. Eur Respir J. 2014;44(6):1447–1478. doi:10.1183/09031936.00150414
- Newcomer KL, Krug HE, Mahowald ML. Validity and reliability of the timed-stands test for patients with rheumatoid arthritis and other chronic diseases. J Rheumatol. 1993;20(1):21–27.
- Morita AA, Bisca GW, Machado FVC, Hernandes NA, Pitta F, Probst VS. Best protocol for the sit-to-stand test in subjects with COPD. Respir Care. 2018;63(8):1040–1049. doi:10.4187/respcare.05100
- Puhan MA, Siebeling L, Zoller M, Muggensturm P, ter Riet G. Simple functional performance tests and mortality in COPD. Eur Respir J. 2013;42(4):956–963. doi:10.1183/09031936.00131612
- Jones PW, Harding G, Berry P, et al. Development and first validation of the COPD assessment test. Eur Respir J. 2009;34(3):648–654. doi:10.1183/09031936.00102509
- Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007;370(9589):786–796. doi:10.1016/S0140-6736(07)61382-8
- Jones CJ, Rikli RE, Beam WC. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport. 1999;70(2):113–119. doi:10.1080/02701367.1999.10608028
- Cohen J. Statistical Power for the Behavioural Sciences. Mahway, NJ: Lawrence Erlbaum Associates; 1988.
- Zhang Q, Li YX, Li X, et al. A comparative study of the five-repetition sit-to-stand test and the 30-second sit-to-stand test to assess exercise tolerance in COPD patients. Int J Chron Obstruct Pulmon Dis. 2018;13:2833–2839. doi:10.2147/COPD.S173509
- Ozalevli S, Ozden A, Itil O, Akkoclu A. Comparison of the sit-to-stand test with 6 min walk test in patients with chronic obstructive pulmonary disease. Respir Med. 2007;101(2):286–293. doi:10.1016/j.rmed.2006.05.007
- Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(10):1005–1012. doi:10.1056/NEJMoa021322
- Medina-Mirapeix F, Valera-Novella E, Morera-Balaguer J, Bernabeu-Mora R. Prognostic value of the five-repetition sit-to-stand test for mortality in people with chronic obstructive pulmonary disease. Ann Phys Rehabil Med. 2022;65(5):101598. doi:10.1016/j.rehab.2021.101598
- Yentes JM, Blanke D, Rennard SI, Stergiou N. The effect of a short duration, high intensity exercise intervention on gait biomechanics in patients with COPD: findings from a pilot study. Chronic Obstr Pulm Dis. 2014;1(1):133–147. doi:10.15326/jcopdf.1.1.2013.0002
- Yentes JM, Schmid KK, Blanke D, Romberger DJ, Rennard SI, Stergiou N. Gait mechanics in patients with chronic obstructive pulmonary disease. Respir Res. 2015;16:31. doi:10.1186/s12931-015-0187-5
- Black-Shinn JL, Kinney GL, Wise AL, et al. Cardiovascular disease is associated with COPD severity and reduced functional status and quality of life. COPD. 2014;11(5):546–551. doi:10.3109/15412555.2014.898029
