Abstract
Purpose
To develop a potential quadriceps’ index of complication evaluation for patients with chronic obstructive pulmonary disease (COPD) which is simple, convenient, and quantifiable.
Patients and Methods
We conducted a prospective study of 59 patients with COPD and 56 healthy controls recruited by the Chengdu First People’s Hospital. Grayscale ultrasound (US) of the rectus femoris was performed to measure thickness (RFthick) and cross-sectional area (RFcsa). Shear wave elastography was used to determine the mean elasticity index (SWEmean) of the rectus femoris (SWERFmean), vastus lateralis (SWEVLmean) and vastus medialis (SWEVMmean). Clinical features included dyspnea index score (modified British Medical Research Council (MMRC) score), COPD Assessment Test (CAT), the Five-Repetition Sit-to-Stand Test (5STS) and the Six-Minute Walk Test (6MWT). We compared the differences between US parameters and SWEmean in healthy controls and COPD patients. We also described the correlation between US parameters, SWEmean and clinical features of patients with COPD.
Results
The intra-observer repeatability for the performance of using SWE to measure quadriceps stiffness was excellent (intraclass correlation coefficient (ICC)>0.75, p < 0.001). There was a statistically significant difference in the SWEmean of the quadriceps (p < 0.001), but no significant difference in terms of RFthic and RFcsa (p > 0.05) between healthy controls and COPD patients. The SWERFmean was positively correlated with the 6MWT (r = 0.959, p < 0.001), and negatively related to the mMRC (r=−0.825, p < 0.001), CAT (r=−0.993, p < 0.001) and 5STS (r=−0.936, p < 0.001). However, the RFthic, RFcsa, SWEVLmean and SWEVMmean were not correlated with clinical features (p > 0.05).
Conclusion
As a supplement to US, SWE reflects changes of stiffness in the quadriceps of COPD patients, and can expanding the dimension of US for assessing the quadriceps. Furthermore, SWEmean was associated with clinical features, and represents a potential index with which to reflect the clinical features of COPD patients.
Video abstract

Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Chronic obstructive pulmonary disease (COPD) is a chronic respiratory disease which is mainly performed by persistent respiratory symptoms and airflow obstruction that is not fully reversible.Citation1 The prevalence of COPD can be high as 27.4% in people over 60 years-of-age.Citation2 Skeletal muscle dysfunction is one of the recognized extrapulmonary complications of COPD; the quadriceps are the most affected muscle types.Citation3 Previous studies have confirmed that approximately one-third of all patients with COPD have skeletal muscle weakness.Citation4 Quadriceps weakness occurs in 76.5% of patients with mild COPD.Citation5 It has been previously reported that quadriceps dysfunction results in a series of consequences such as aggravated dyspnea symptoms, reduced muscular capacity and endurance.Citation6,Citation7 Various clinical features are commonly used to evaluate the physical performance of a given patient, including the Six-Minute Walk Test (6MWT)Citation8 to assess muscular endurance, the Five-Repetition Sit-to-Stand Test (5STS)Citation9 to reflect the muscle strength, the COPD Assessment Test (CAT)Citation10 and the modified British Medical Research Council score (mMRC) to evaluate the patient’s overall health and dyspnea. Although the translated CAT and mMRC questionnaires are simple and easy to fill in, there are still subjective differences in the understanding of breathing difficulties and physical condition between different patients. Moreover, some patients with poor physical condition have difficulty completing 6MWT and 5STS trials in this study. Thus, it is necessary to introduce a new tool that is simple, convenient, and quantifiable and that can accurately reflect the clinical features.
According to Ramirez Fuentes et al,Citation11 morphological changes may occur in the quadriceps of COPD patients and can be reflected by ultrasound (US) parameters such as thickness of the rectus femoris (RFthick) and cross-sectional area of the rectus femoris (RFcsa). In addition to morphological changes, it would be highly valuable to ascertain if we can acquire further information about the quadriceps in COPD patients.
Shear wave elastography (SWE) is a simple and novel ultrasonography technique that acquires SWE values by emitting and tracking shear waves and dynamically depicting a distribution map of the SWE values of target tissues in real time. SWE has been widely applicated in the diagnosis and treatment of liver, breast, thyroid, and kidney-related lesions.Citation12 Over the last few years, there showed a gradual increase in the application of SWE to evaluate the musculoskeletal system.Citation13 SWE is positively correlated with tissue stiffness and can therefore reflect stiffness in an accurate manner.Citation14 In a previous study, Xu et al showed that SWE can be an useful tool for the reflection of diaphragmatic stiffness in COPD patients.Citation15 However, the clinical value of SWE for assessing the stiffness of quadriceps in COPD patients remains uncertain.
In this study, we evaluated the SWE, and explored the relationship between US parameters, mean elasticity index (SWEmean) and clinical features in healthy controls and COPD patients.
Materials and Methods
Study Design and Patients
Between August 2021 and February 2022, a total of 59 COPD patients (≥55 years-of-age) and 56 matched healthy controls from The Chengdu First People’s Hospital (Chengdu, China) were recruited for this study which was prospective and observational. The inclusion criterion was a diagnosis of stable COPD based on the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria.Citation16 The exclusion criteria were described below: COPD history of acute exacerbations in the last one month; the presence of active lung disease or lung cancer; the concomitant disease that affect the musculoskeletal system; long-term treatment with steroid medications; a history of lower limb trauma or surgery; athletes or long-term manual workers; unable to read and understand the informed consent documents. Clinical characteristics, including age, gender, and BMI, were obtained from medical records. This study was approved by the Research Ethics Committee of The Chengdu First People’s Hospital, and all participants signed the informed consent.
Pulmonary Function Test and the Assessment of Dyspnea Index Score (Modified British Medical Research Council (mMRC) Score) and COPD Assessment Test (CAT)
Pulmonary function tests were performed using a MasterScreen system (MasterScreen, CareFusion Germany). The overall health and dyspnea status of each patient were evaluated by the Chinese improved version of the CATCitation17 and the mMRC dyspnoea scale.Citation18
Five-Repetition Sit-to-Stand Test (5STS)
The participant was told to seat on an armless chair that was 48-cm-high and hold their hands folded in front of their chests, back supported by the chair, and feet on the ground. The participant stood up and sat down at the fastest speed according to the command. We recorded the time taken to complete five repetitions. The participant was given one minute of rest between each test and each test was performed in triplicate to create an overall mean value.
Six-Minute Walk Test (6MWT)
According to the guidelines of American Thoracic Society (ATS),Citation19 we chose a straight and flat corridor for the 6MWT. The participant was told to try their best to walk within six minutes. They were able to slow down or stop to rest when feeling shortness of breath, chest pain or dizziness. If the symptoms above aggravated and did not get relief after rest, stop the test immediately. At the end of the test, the tester recorded the total distance the participant had walked in meters.
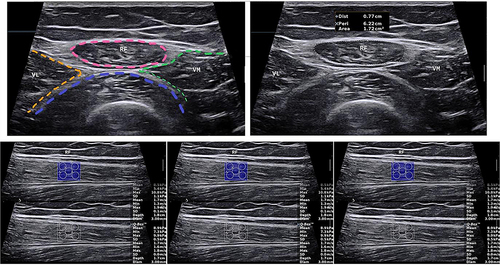
Measurements of the RFthic and RFcsa
Measurements of the RFthic and RFcsa were performed as described in previous studies.Citation20 US was performed with an Aixplorer ultrasound scanning system (SuperSonic Imagine, France) and a 4–15 MHz linear array transducer. The participants were laid in a supine position, with both lower limbs naturally relaxed and knees straight. We reduced muscle deformation caused by external forces by placing the participant’s arms on a fixed countertop. The sensor was perpendicular to the thigh axis, and the point is located at 3/5 of the distance from the anterior superior iliac spine to the upper border of the patella (). We identified the anatomy of the rectus femoris to determine the course and boundaries. We outlined the rectus femoris with a movable cursor after freezing the image and measured the RFthic and RFcsa. We took the mean of five replicate measurements for further analysis.
SWE Measurements
SWE was performed with an Aixplorer ultrasound system (Supersonic Imagine, France), which was equipped with ShearWave™ Elastography and a 4–15MHz linear transducer and was operated as previously described.Citation21
First, US was used to identify muscle alignment and locate the rectus femoris, vastus lateralis, and vastus medialis. Next, we initiated the measurement function for SWE and set the region of interest (ROI) to 3 mm. We selected five points on each image, including the midpoint and the four corners to measure SWEmean. We took the mean of three replicate measurements for further analysis ().
Statistical Analyses
Statistical analysis was performed with SPSS 25.0 software (IBM, United States). Data normality testing was inspected by Shapiro–Wilk. Measurement that conforms to the normal distribution is represented by x ± s, and were compared by the independent sample t-test. Non-normally distributed measurement data are represented by medians and interquartile ranges and were compared by the rank sum test. Numerical data are represented by rates; and compared by the χ2 test. Intra-observer reliability was calculated using the intraclass correlation coefficient (ICC) test; ICC was explained based on relevant guidelines: <0.40, poor reliability; 0.40–0.75, fair to good reliability; and >0.75 for excellent reliability.Citation22
Differences in the US parameters and SWEmean between healthy controls and COPD patients were compared by the rank sum test. p < 0.05 was considered statistically significant. Spearman correlation coefficients were used to analyze the correlations between US parameters, SWEmean and clinical features in patients with COPD.
Results
Basic Characteristics
Finally, 59 patients with COPD and 56 matching healthy controls were analyzed. The basic characteristics of the patients are listed in . There were no significant differences between COPD patients and healthy controls in terms of gender, age, and BMI. However, we did identify significant differences between the two groups in terms of lung function.
Table 1 Basic Characteristics of Healthy Controls and COPD Patients
Reliability and Repeatability Levels of SWE Measurements
Next, we determined the level of reliability and repeatability measured by SWE in the quadriceps. The muscles were measured by the same observer at three different times. The reliability of the SWE for assessing the stiffness of quadriceps was excellent for the healthy controls and the COPD patients (ICC >0.75, p < 0.001). The results demonstrate that the SWE can be a reliable and reproducible tool for stiffness measurement of the quadriceps ().
Table 2 Intra-Observer Group Concordance Analysis
Comparison of the RFthic, RFcsa, and SWEmean of the Quadriceps Between Patients with COPD and Healthy Controls
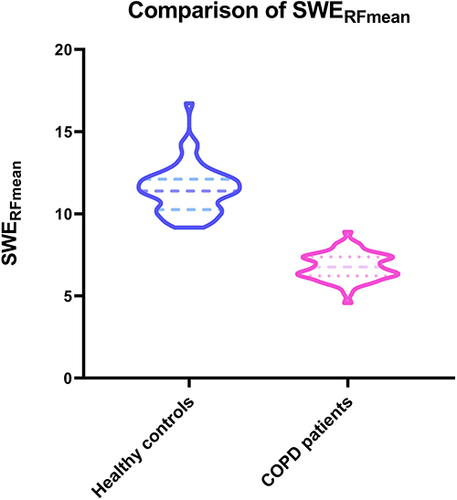
We compared US parameters and the SWEmean between healthy controls and patients with COPD. There was a statistically significant difference in SWEmean (p < 0.001) (), but no significant difference in RFthic and RFcsa (p > 0.05) when compared between healthy controls and COPD patients ().
Table 3 Comparison of RFthic, RFcsa, and SWEmean Between Healthy Controls and COPD Patients
Correlation Between US Parameters and SWERFmean and Clinical Features in COPD Patients
Finally, we explored the correlation between RFthic, RFcsa, and SWEmean with a range of clinical features provided by the 6MWT, 5STS, CAT, and mMRC in COPD patient. According to , the SWERFmean was positively correlated with 6MWT (r = 0.959, p < 0.001), and negatively related to mMRC (r=−0.825, p < 0.001), CAT (r=−0.993, p < 0.001) and 5STS (r=−0.936, p < 0.001). However, the RFthic, RFcsa, SWEVLmean and SWEVMmean were not correlated with clinical features (p > 0.05).
Table 4 Correlation Between US Parameters, SWEmean and Clinical Features in COPD Patients
Discussion
Dysfunction of the quadriceps is an extrapulmonary complication in COPD patients, which can lead to a decreased quality of life and even increase the risk of death. In this study, we investigated SWE in attempt to reflect the clinical features of this condition in a simple, convenient and quantifiable way, and to provide more information about quadriceps in COPD patients, such as muscle stiffness.
First, in this study, we evaluated the reliability of the SWE to assess stiffness of the quadriceps. Compared with previous related studies, which only investigated the rectus femoris when assessing the quadriceps and mostly focused on healthy individuals,Citation23–26 we focused on muscles including not only the rectus femoris but also the vastus medialis and vastus lateralis; furthermore, the selected participants involved healthy controls and COPD patients. The results showed an excellent (ICC >0.75) performance for SWE, thus indicating that SWE can be used as a reliable tool to assess the stiffness of the quadriceps.
Second, we evaluated the differences between SWEmean and US parameters in healthy controls and COPD patients. We identified a statistically significant difference for SWEmean (p < 0.001), but not for RFthic and RFcsa (p > 0.05). The reason for this may be that when there is a significant difference in SWEmean between COPD patients and healthy controls, two-dimensional ultrasound parameters have not changed accordingly. In other words, testing the stiffness of the quadriceps can identify a significant difference between healthy controls and COPD patients when there are no significant morphological differences. That is to say, the assessment of stiffness in the quadriceps by SWE can provide more information about the quadriceps in COPD patients, thus expanding the dimension of muscle assessment compared to US. We also found that the SWERFmean was positively correlated with the 6MWT (r = 0.959, p < 0.001), and negatively correlated with the mMRC (r=−0.825, p < 0.001), CAT (r=−0.993, p < 0.001) and 5STS (r=−0.936, p < 0.001). However, the RFthic, RFcsa, SWEVLmean and SWEVMmean were not correlated with clinical features (p > 0.05). These data mean that SWERFmean can reflect the clinical features of patients with COPD.
There are some limitations in our study that need to be considered. First, previous research has shown that exercise may have an impact on muscle thickness.Citation27 However, in this study, we did not focus on exercise due to the variability between COPD patients and the inability to quantitatively describe exercise in each patient. Second, this study had a small sample size and did not include COPD patients who were very severe or in the acute phase. Whether our findings apply to patients with very severe COPD, those with acute exacerbations, or those undergoing pulmonary rehabilitation remain unclear. Relevant studies on differences in ultrasound parameters in COPD patients of different severities and receiving pulmonary rehabilitation are currently ongoing, and the results need to be further studied. Third, although we verified the repeatability and reliability of measurements obtained by the same operator, the reliability of SWE measurements between different operators remains uncertain. Fourth, patients in this study were old, had a longer duration of illness, and had a vague memory of the specific onset time. Consequently, we were unable to investigate the effects of disease duration. These limitations will be addressed in future research.
Conclusion
As a supplement to US, SWE can reflect changes in the stiffness of the quadriceps in COPD patients, thus expanding the dimension of ultrasound for quadriceps assessment. Furthermore, SWEmean was associated with clinical features and represents a potential index to reflect the clinical features of COPD patients.
Ethics Approval and Informed Consent
The study complies with the Declaration of Helsinki. All participants in this study provided informed consent. The study was conducted in accordance with the ethical standards of the Ethics Committees of Chengdu First People’s Hospital (2022 YNYJ 014).
Disclosure
The authors report no conflicts of interest in this work.
References
- Riley CM, Sciurba FC. Diagnosis and outpatient management of chronic obstructive pulmonary disease: a review. JAMA. 2019;321(8):786–797. doi:10.1001/jama.2019.0131
- Wang C, Xu J, Yang L, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet. 2018;391(10131):1706–1717. doi:10.1016/S0140-6736(18)30841-9
- Man WD-C. Non-volitional assessment of skeletal muscle strength in patients with chronic obstructive pulmonary disease. Thorax. 2003;58:665–669. doi:10.1136/thorax.58.8.665
- Seymour JM, Spruit MA, Hopkinson NS, et al. The prevalence of quadriceps weakness in COPD and the relationship with disease severity. Eur Respir J. 2010;36(1):81–88. doi:10.1183/09031936.00104909
- Kharbanda S, Ramakrishna A, Krishnan S. Prevalence of quadriceps muscle weakness in patients with COPD and its association with disease severity. Int J Chron Obstruct Pulmon Dis. 2015;10:1727–1735. doi:10.2147/COPD.S87791
- Degens H, Gayan-Ramirez G, van Hees HW. Smoking-induced skeletal muscle dysfunction: from evidence to mechanisms. Am J Respir Crit Care Med. 2015;191(6):620–625. doi:10.1164/rccm.201410-1830PP
- Abdulai RM, Jensen TJ, Patel NR, et al. Deterioration of limb muscle function during acute exacerbation of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;197(4):433–449. doi:10.1164/rccm.201703-0615CI
- Chen S, Sierra S, Shin Y, Goldman MD. Gait speed trajectory during the six-minute walk test in multiple sclerosis: a measure of walking endurance. Front Neurol. 2021;12:698599. doi:10.3389/fneur.2021.698599
- Mentiplay BF, Clark RA, Bower KJ, Williams G, Pua YH. Five times sit-to-stand following stroke: relationship with strength and balance. Gait Posture. 2020;78:35–39. doi:10.1016/j.gaitpost.2020.03.005
- Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD assessment test. Eur Respir J. 2009;34(3):648–654. doi:10.1183/09031936.00102509
- Ramirez-Fuentes C, Minguez-Blasco P, Ostiz F, et al. Ultrasound assessment of rectus femoris muscle in rehabilitation patients with chronic obstructive pulmonary disease screened for sarcopenia: correlation of muscle size with quadriceps strength and fat-free mass. Eur Geriatr Med. 2019;10(1):89–97. doi:10.1007/s41999-018-0130-7
- Sigrist RMS, Liau J, Kaffas AE, Chammas MC, Willmann JK. Ultrasound elastography: review of techniques and clinical applications. Theranostics. 2017;7(5):1303–1329. doi:10.7150/thno.18650
- Mihra S, Gimber LH, Becker GW, et al. Shear-wave elastography: basic physics and musculoskeletal applications. Radiographics. 2017;37:855–870. doi:10.1148/rg.2017160116
- Creze M, Nordez A, Soubeyrand M, Rocher L, Maitre X, Bellin MF. Shear wave sonoelastography of skeletal muscle: basic principles, biomechanical concepts, clinical applications, and future perspectives. Skeletal Radiol. 2018;47(4):457–471. doi:10.1007/s00256-017-2843-y
- Xu JH, Wu ZZ, Tao FY, et al. Ultrasound shear wave elastography for evaluation of diaphragm stiffness in patients with stable COPD: a pilot trial. J Ultrasound Med. 2021;40(12):2655–2663. doi:10.1002/jum.15655
- Labaki WW, Rosenberg SR. Chronic Obstructive Pulmonary Disease. Ann Intern Med. 2020;173(3):17–32. doi:10.7326/AITC202008040
- Zhou QT, Mei JJ, He B, et al. Chronic obstructive pulmonary disease assessment test score correlated with dyspnea score in a large sample of Chinese patients. Chin Med J. 2013;126(1):11–15.
- Cui L, Ji X, Xie M, Dou S, Wang W, Xiao W. Role of inspiratory capacity on dyspnea evaluation in COPD with or without emphysematous lesions: a pilot study. Int J Chron Obstruct Pulmon Dis. 2017;12:2823–2830. doi:10.2147/COPD.S142016
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;111–117. doi:10.1164/ajrccm.166.1.at1102
- Maynard-Paquette AC, Poirier C, Chartrand-Lefebvre C, Dube BP. Ultrasound evaluation of the quadriceps muscle contractile index in patients with stable chronic obstructive pulmonary disease: relationships with clinical symptoms, disease severity and diaphragm contractility. Int J Chron Obstruct Pulmon Dis. 2020;15:79–88. doi:10.2147/COPD.S222945
- Andonian P, Viallon M, Le Goff C, et al. Shear-wave elastography assessments of quadriceps stiffness changes prior to, during and after prolonged exercise: a longitudinal study during an extreme mountain ultra-marathon. PLoS One. 2016;11(8):e0161855. doi:10.1371/journal.pone.0161855
- Fleiss PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi:10.1037/0033-2909.86.2.420
- Cortez CD, Hermitte L, Ramain A, Mesmann C, Lefort T, Pialat JB. Ultrasound shear wave velocity in skeletal muscle: a reproducibility study. Diagn Interv Imaging. 2016;97(1):71–79. doi:10.1016/j.diii.2015.05.010
- Lacourpaille L, Hug F, Bouillard K, Hogrel JY, Nordez A. Supersonic shear imaging provides a reliable measurement of resting muscle shear elastic modulus. Physiol Meas. 2012;33(3):N19–28. doi:10.1088/0967-3334/33/3/N19
- Tas S, Onur MR, Yilmaz S, Soylu AR, Korkusuz F. Shear wave elastography is a reliable and repeatable method for measuring the elastic modulus of the rectus femoris muscle and patellar tendon. J Ultrasound Med. 2017;36(3):565–570. doi:10.7863/ultra.16.03032
- Deng M, Zhou X, Li Y, et al. Ultrasonic elastography of the rectus femoris, a potential tool to predict sarcopenia in patients with chronic obstructive pulmonary disease. Front Physiol. 2021;12:783421. doi:10.3389/fphys.2021.783421
- Ruas CV, Brown LE, Lima CD, Gregory Haff G, Pinto RS. Different muscle action training protocols on quadriceps-hamstrings neuromuscular adaptations. Int J Sports Med. 2018;39(5):355–365. doi:10.1055/s-0044-100391