Abstract
Background
Pulmonary emphysema of any etiology has been shown to be strongly and quasidiagnostically associated with a vertical frontal P wave axis. A vertical P wave axis (>60 degrees) during sinus rhythm can be easily determined by a P wave in lead III greater than the P wave in lead I (bipolar lead set) or a dominantly negative P wave in aVL (unipolar lead set). The purpose of this investigation was to determine which set of limb leads may be better for identifying the vertical P vector of emphysema in adults.
Methods
Unselected consecutive electrocardiograms from 100 patients with a diagnosis of emphysema were analyzed to determine the P wave axis. Patients aged younger than 45 years, those not in sinus rhythm, and those with poor quality tracings were excluded. The electrocardiographic data were divided into three categories depending on the frontal P wave axis, ie, >60 degrees, 60 degrees, or <60 degrees, by each criterion (P amplitude lead III > lead I and a negative P wave in aVL).
Results
Sixty-six percent of patients had a P wave axis > 60 degrees based on aVL, and 88% of patients had a P wave axis > 60 degrees based on the P wave in lead III being greater than in lead I.
Conclusion
A P wave in lead III greater than that in lead I is a more sensitive marker than a negative P wave in aVL for diagnosing emphysema and is recommended for rapid routine screening.
Keywords:
Introduction
Emphysema of any etiology is nearly always caused by chronic obstructive pulmonary disease, and has been shown to be strongly and quasidiagnostically associated with a vertical frontal P wave axis.Citation1–Citation11 In previous investigations, we have determined that a vertical P wave axis (>60 degrees) during sinus rhythm can be used as a lone criterion to screen for pulmonary hyperinflation/emphysema, with sensitivity and specificity both being above 90%.Citation4,Citation5,Citation8 Previous studies have also suggested that the degree of P vector verticalization has an inverse correlation with qualitative lung functionCitation8,Citation9 and quantification of radiographic emphysema.Citation12,Citation13 A vertical P vector on a surface 12-lead electrocardiogram can be determined by two methods using limb leads, ie, a P wave amplitude in lead III greater than in lead I or a negative P wave in aVL,Citation1,Citation5,Citation8 although both these electrocardiographic findings suggest a vertical P vector and theoretically both should be simultaneously present in all the patients with a vertical P vector.
However, preliminary observations from our previous investigations had suggested that this is not the case in the clinical setting. Thus, the purpose of our current investigation was to determine which set of limb leads would be better for identifying the vertical P vector of emphysema in adults, given that this has not been investigated previously. A P wave amplitude in lead III greater than in lead I indicates a P axis > 60 degrees, a P wave amplitude in lead III equal to that in lead I indicates a P axis of 60 degrees, and a P wave amplitude in lead III smaller than in lead I indicates a P axis < 60 degrees. A negative P wave in aVL indicates a P axis > 60 degrees, while a flat or equiphasic P wave in aVL indicates a P axis of 60 degrees and a positive P wave in aVL indicates a P axis < 60 degrees.Citation1,Citation2,Citation5,Citation8 Our plan was to conduct this investigation in patients having a known diagnosis of emphysema with a working hypothesis, that the set more often showing P wave verticalization would be a more sensitive (better) marker for diagnosis of emphysema. Thus, we aimed to investigate whether a P wave amplitude in lead III greater than that in lead I is a better marker of emphysema than an inverted P wave in aVL.
Materials and methods
We recorded 12-lead electrocardiograms at rest using a standard technique in unselected consecutive patients with a known diagnosis of emphysema and scheduled for a routine follow-up visit in the pulmonary clinic at our institution between March and April 2012, with the aim of obtaining a total of 100 patient electrocardiograms after application of the exclusion criteria. Inclusion criteria were age > 45 years,Citation5–Citation9 normal sinus rhythm, a prior confirmed diagnosis of emphysema with a documented clinical history, chest radiographs, and pulmonary function tests. We excluded patients aged younger than 45 years, those not in normal sinus rhythm, and those with poor quality tracings. Patients younger than 45 years of age were excluded because a vertical P wave axis may be a normal finding in healthy children and young adults.Citation1,Citation5,Citation8 Paced rhythms were also excluded. The electrocardiograms were then analyzed individually by all the authors using a handheld loop magnifier to determine the frontal P wave axis/frontal P vector by accounting for the P wave amplitudes in leads I, III, and aVL. Any differences in individual observations were resolved by consensus in a conference. All patients enrolled in the investigation had a documented diagnosis of pulmonary emphysema supported by clinical history, chest radiographs (findings of increased radiolucency of the lungs, a flat diaphragm, and a long, narrow heart shadow), and pulmonary function tests. Pulmonary function tests showed an obstructive airway pattern (forced expiratory volume in one second/forced vital capacity ratio [FEV1/FVC] <0.70 and a forced expiratory volume in one second [FEV1] <80% of predicted) without significant bronchodilator reversibility. Electrocardiographic data for the 100 patients were divided into three categories depending on the frontal P wave axis, ie, >60 degrees, 60 degrees, or <60 degrees, by each criterion (ie, accounting for the P amplitude in leads III and I and the P wave in aVL). A correlation between the frontal P axis and FEV1 was also tested for using Pearson’s correlation test.
Results
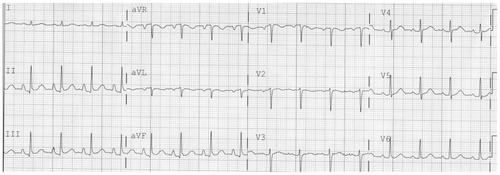
The baseline demographic characteristics of the study population are shown in . The mean (±standard deviation) age of the patients was 68.2 ± 9.9 years, of whom 41% were male. Ninety-four percent of the patients had an active or remote smoking history, with an average of 48.3 ± 28.5 pack-years of smoking. The mean P vector was 68.6 ± 11.4 degrees and did bear an inverse correlation with FEV1 (r = −0.52; P < 0.001). Of 73 study patients who had also undergone a conventional computed tomographic scan of the chest, 66 (90.4%) had evidence of emphysematous changes. shows the P wave axis based on P wave amplitude in leads I and III. Eighty-eight of the 100 patients had a P wave in lead III greater than the P wave in lead I, eight had a P wave in lead I equal to that in lead III, and four had a P wave greater in lead I than in lead III. shows the P wave axis based on P wave morphology in aVL. Sixty-six of the 100 patients had a predominantly negative P wave, 22 had a flat P wave, and 12 had a positive P wave in aVL. Sixtytwo patients had a P axis > 60 degrees by both criteria. An electrocardiographic tracing showing P wave amplitude in lead III greater than in lead I and an unequivocally negative P wave in aVL during sinus rhythm is shown in . The study results demonstrated that a P wave amplitude in lead III greater than in lead I (sensitivity 88%) is a more sensitive marker of emphysema than an inverted P wave in aVL (sensitivity 66%).
Table 1 Baseline characteristics of the study population
Table 2 P axis based on P wave morphology in leads I and III
Table 3 P axis based on P wave morphology in lead aVL
Discussion
Frontal P wave verticalization has been shown to have a close correlation with emphysema and has been extensively studied in previous investigations.Citation1–Citation8 Moreover, increasing verticality of the frontal P vector correlates with increasing degrees of airway obstruction,Citation8,Citation9 degree of depression of the diaphragm,Citation3 and radiographic quantification of the disease.Citation12,Citation13 A possible mechanism of P wave axis verticalization in lung hyperinflation is that the right atrium is firmly attached to the diaphragm by a dense pericardial ligament around the inferior vena cava.Citation3 With progressive flattening of the diaphragm, the right atrium is distorted/displaced inferiorly, causing a significant rightward deviation (verticalization) of the P wave axis. A prospective blinded investigation of patients with purely (fibrotic) restrictive, compared with purely obstructive pulmonary disease showed the P axis to follow the level of the diaphragm, such that patients with restrictive lung disease and high diaphragms had horizontal and leftward P axes, while patients with low diaphragms and obstructive lung disease had vertical P axes.Citation3 In the study by Baljepally et al,Citation5 the sensitivity and specificity of a P axis > 60 degrees for emphysema was found to be 89% and 96%, respectively. In another study by Chhabra et al,Citation8 sensitivity and specificity of a vertical P axis for diagnosing emphysema was 94.7% and 86.4%, respectively. From prior correlation studies,Citation5,Citation8 it is clear that a vertical P axis on an electrocardiogram is the single most common screening tool, which is highly sensitive and specific in diagnosing emphysema at a glance.Citation5,Citation8 Both studiesCitation5,Citation8 used electrocardiographic criteria (a P amplitude in lead III greater than in lead I and/or a dominantly negative P wave in aVL) to determine P wave verticalization. In the present study, we took this further by investigating the percentage of patients with emphysema who have a dominantly negative or inverted P wave in aVL compared with a P wave in lead III greater than that in lead I; 88% of the emphysema patients had a P wave in lead III greater than that in lead I, and only 66% of the patients had an inverted or negative P wave in aVL. In an ideal theoretical setting, the P wave amplitude should be negative in aVL when the P wave amplitude in lead III is greater than in lead I (suggesting a vertical P vector), but this was not found in a practical clinical setting, which could be possibly due to a commonly encountered variable/high skin resistance or poor surface contact at aVL producing a spurious “augmented” extremity (unipolar) lead abnormality.Citation14 Thus, the results suggest that the bipolar lead set is more sensitive for rapid characterization of emphysema than the unipolar set.
Limitations
All patients enrolled had a known diagnosis of emphysema (based on chest radiographs and pulmonary function tests), so the specificity of both these electrocardiographic criteria for diagnosing emphysema could not be estimated in the current study. Emphysema was diagnosed based on clinical history, chest radiographs, and pulmonary function tests. High resolution computed tomographic scanning was not used to confirm the diagnosis, and is known to have a higher sensitivity and specificity for diagnosing structural emphysematous changes.
Conclusion
Electrocardiographic analysis of 100 patients with clinically documented emphysema prompted the following conclusions. The vertical P axis (>60 degrees) on an electrocardiogram is a unique characteristic of obstructive pulmonary disease in adults and is the single most important tool for identifying emphysema by electrocardiogram, and serves as a virtual screening test at a glance. A P wave in lead III larger than in lead I is a more sensitive marker for rapid identification of emphysema compared with an inverted P wave in aVL.
Disclosure
The authors report no conflicts of interest in this work.
References
- SpodickDHElectrocardiographic studies in pulmonary disease. I. Electrocardiographic abnormalities in diffuse lung diseaseCirculation1959201067107213833426
- ZuckermanRCabreraCEFishlederBLSodi-PallaresDThe electrocardiogram in chronic cor pulmonaleAm Heart J19483542142518903667
- ShahNSKollerSMJanowerMLSpodickDHDiaphragm levels as determinants of P axis in restrictive vs obstructive pulmonary diseaseChest19951076977007874939
- ThomasAJApiyasawatSSpodickDHElectrocardiographic detection of emphysemaAm J Cardiol20111071090109221306694
- BaljepallyRSpodickDHElectrocardiographic screening for emphysema: the frontal plane P axisClin Cardiol19992222622810084066
- LittmannDThe electrocardiographic findings in pulmonary emphysemaAm J Cardiol1960533934814417562
- SpodickDHElectrocardiographic studies in pulmonary disease. II. Establishment of criteria for the electrocardiographic inference of diffuse lung diseasesCirculation1959201073107413833427
- ChhabraLSareenPPerliDSrinivasanISpodickDHVertical P-wave axis: the electrocardiographic synonym for pulmonary emphysema and its severityIndian Heart J201264404222572424
- SpodickDHVectorcardiogram in pulmonary emphysema: its relation to scalar electrocardiographic findingsAm Rev Respir Dis1968986346394234113
- ChhabraLSpodickDHTransient Super-Himalayan P-waves in severe pulmonary emphysemaJ Electrocardiol201245262721907999
- ZambranoSSMoussaveMSSpodickDHQRS duration in chronic obstructive lung diseaseJ Electrocardiol1974735364811647
- ChhabraLSareenPGandaguleASpodickDHVisual computed tomographic scoring of emphysema and its correlation with its diagnostic electrocardiographic sign: the frontal P vectorJ Electrocardiol20124513614022244933
- ChhabraLSareenPGandaguleASpodickDComputerized tomographic quantification of chronic obstructive pulmonary disease as the principal determinant of frontal P vectorAm J Cardiol20121091046104922221942
- SchwarzschildMMHoffmanIKissinMErrors in unipolar limb leads caused by unbalanced skin resistances, and a device for their eliminationAm Heart J19544823524813180475