Abstract
Background
Chronic obstructive pulmonary disease (COPD) is a leading cause of mortality worldwide. Identifying both individual and community risk factors associated with higher mortality is essential to improve outcomes. Few population-based studies of mortality in COPD include both individual characteristics and community risk factors.
Objective
We used geocoded, patient-level data to describe the associations between individual demographics, neighborhood socioeconomic status, and all-cause mortality.
Methods
We performed a nationally representative retrospective cohort analysis of all patients enrolled in the Veteran Health Administration with at least one ICD-9 or ICD-10 code for COPD in 2016–2019. We obtained demographic characteristics, comorbidities, and geocoded residential address. Area Deprivation Index and rurality were classified using individual geocoded residential addresses. We used logistic regression models to assess the association between these characteristics and age-adjusted all-cause mortality.
Results
Of 1,106,163 COPD patients, 33.4% were deceased as of January 2021. In age-adjusted models, having more comorbidities, Black/African American race (OR 1.09 [95% CI: 1.08–1.11]), and higher neighborhood disadvantage (OR 1.30 [95% CI: 1.28–1.32]) were associated with all-cause mortality. Female sex (OR 0.67 [95% CI: 0.65–0.69]), Asian race (OR 0.64, [95% CI: 0.59–0.70]), and living in a more rural area were associated with lower odds of all-cause mortality. After adjusting for age, comorbidities, neighborhood socioeconomic status, and rurality, the association with Black/African American race reversed.
Conclusion
All-cause mortality in COPD patients is disproportionately higher in patients living in poorer neighborhoods and urban areas, suggesting the impact of social determinants of health on COPD outcomes. Black race was associated with higher age-adjusted all-cause mortality, but this association was abrogated after adjusting for gender, socioeconomic status, comorbidities, and urbanicity. Future studies should focus on exploring mechanisms by which disparities arise and developing interventions to address these.
Introduction
In 2019, chronic obstructive pulmonary disease (COPD) was the third leading cause of mortality worldwide.Citation1 The progression of COPD displays strong heterogeneity, with some patients living decades with the disease and minimal symptoms, while others experience frequent exacerbations or early death. Most studies identifying predictors of COPD mortality are relatively small cohorts that focus on individual risk factors such as exacerbation rate, hospitalizations, lung function and comorbidities.Citation2 Fewer studies are population based that include community risk factors. Identifying both individual and community risk factors associated with higher mortality in people with COPD is essential to improve outcomes.
Community risk factors such as neighborhood socioeconomic status and urbanicity have been identified as possible factors associated with differences in both respiratory disease severity and mortality.Citation3 Higher COPD-specific mortality is reported in rural areas; however, the variation in death rates among people with COPD has not been assessed across the urban–rural gradient.Citation4 Socioeconomic status (SES) is an additional important risk factor established as influencing COPD outcomes.Citation3 Whether this disparity is attributed to differences in health care access, social risk factors, or environmental exposures is unknown. In addition, few population-level studies relating community risk factors to COPD mortality have included race.
Larger studies examining factors associated with increased mortality in COPD have used population-level aggregated data and are prone to ecological fallacy, when individuals are assigned characteristics representing an average across a broader geographic region. For example, higher rates of COPD may be associated with increased rurality in counties, but this does not necessarily indicate an individual who died in that county lived in a rural area. Exposure misclassification using population-level sociodemographic or health data may be driving variation and bias in research findings. A potential solution is the exploration of mortality in COPD patients using a large population with geographically precise exposures and spatially refined community measures, but few large studies have access to patient-level data.
To address this gap in knowledge, we used geographically precise patient-level data from a large cohort of patients with COPD to describe the associations between demographic characteristics and socioeconomic status with all-cause mortality.
Methods
Study Design, Data Source, and Participants
We performed a nationally representative retrospective cohort analysis of patients enrolled in the Veteran Health Administration (VHA) which provides care to Veterans of the United States and includes over 1000 health care facilities across the country and its territories. Electronic health record data were obtained from the national VHA Corporate Data Warehouse (CDW). The VHA CDW is a system-wide electronic repository of administrative and clinical data. Mortality data came from the CDW, Medicare claims, the Veterans Benefits Administration, and the Social Security Administration. Included were all patients across the United States and its territories, aged ≥35 and less than 100 years with at least one International Classification of Diseases, Ninth (ICD-9) or Tenth (ICD-10) Revision codes for COPD (ICD-9: 490–492, 496; ICD-10: J40, J41.0, J41.1, J41.8, J42, J43.0, J43.1, J43.2, J43.8, J43.9, J44.0, J44.1, J44.9) between 2016 and 2019. Specific age criteria were included to increase the specificity of the diagnosis of COPD. Demographic characteristics (age, gender, race), Charlson Comorbidity Index (CCI),Citation5 and geocoded residential addresses were obtained from the CDW Patient Domain File and Vital Status Files. CCI was calculated prior to COPD diagnosis and therefore does not include COPD. Race and gender were self-reported. Those with a gender other than male or female (N=20) were excluded from analysis due to the relatively small sample size. We used patient’s residential addresses to spatially assign an Area Deprivation Index (ADI) percentile ranking of neighborhood-level socioeconomic status.Citation6 ADI ranking is based on data from the American Community Survey which includes factors for income, education, and housing quality at the census block group level with 1 being the least deprived and 100 being the most deprived neighborhoods. Rurality is defined using the Rural–Urban Commuting Area (RUCA) codes, where “urban” are RUCA codes 1.0 or 1.1, “highly rural” is RUCA code 10.0, and “rural” is all others.Citation7
Statistical Analysis
Descriptive statistics were used to summarize the demographics, comorbidities, quintile-binned ADI, and rurality of the cohort. We used an age-adjusted logistic regression model to assess the associations between sociodemographic and geographic characteristics and all-cause mortality. A second model adjusting for potential confounders including both biologic variables (age, sex, CCI) and socioeconomic variables (race, ADI, and rurality) was performed. Analysis was completed using R Statistical software (version 4.1.2).
Study Oversight
This retrospective study involved no more than minimal risk to the participants and was approved with waiver for informed consent by institutional review boards at the Minneapolis VA Health Care System (VAM-20-00583) and the University of Minnesota (STUDY00011069). All procedures were in accordance with the ethical standards of the Declaration of Helsinki, and participant confidentiality was protected.
Results
Participant Characteristics
Of the 1,106,163 patients with a diagnosis of COPD, 33.4% were deceased as of January 2021. The cohort was predominantly male (95.5%). White (78.3%) and Black/African American (13.2%) proportions were similar to racial breakdowns observed in the US general population (). While most of the cohort lived in urban areas (58.8%), an estimated 39.5% and 1.6% lived in rural and highly rural areas, respectively, which is higher than the general US population.
Table 1 Characteristics of Patients with Chronic Obstructive Pulmonary Disease (COPD)
Association of Race, ADI, and Rurality with All-Cause Mortality
In age-adjusted only models, male gender, Black/African American race, higher CCI score, higher neighborhood deprivation, and living in a more urban area were associated with higher odds of all-cause mortality. In contrast, females (aOR 0.67, [95% CI: 0.65–0.69]), Asian race (aOR 0.64, [95% CI: 0.59–0.70]), and living in a more rural area were associated with lower odds of all-cause mortality ().
Figure 1 Odds ratios for all-cause mortality in COPD patients. Age-adjusted logistic models (A) and model adjusting for all other covariates (age, sex, race, CCI, ADI, rurality; (B)). Higher ADI indicates higher neighborhood disadvantage. Error bars denote 95% confidence intervals.
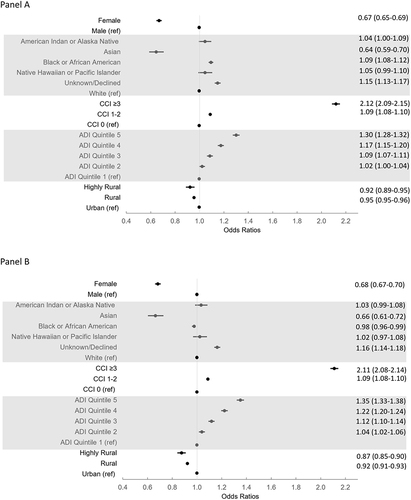
Black/African American race was associated with 9% higher odds of all-cause mortality (95% confidence interval (CI): 1.08–1.11) compared to White race. The odds of all-cause mortality steadily increased with higher ADI quintile (greater neighborhood disadvantage). Compared to patients in ADI quintile 1, patients in ADI quintile 5 had aOR 1.30 [95% CI: 1.28–1.32] for all-cause mortality. Patients living in highly rural areas (aOR 0.92, [95% CI: 0.89–0.95]) had lower odds of all-cause mortality compared to patients living in urban areas.
After adjusting for age, CCI, race, ADI, and urbanicity, the odds of all-cause mortality associated with Black/African American race reversed from aOR 1.09 [95% CI: 1.08–1.11] to aOR 0.98 [95% CI: 0.96–0.99] and was associated with decreased odds of mortality. The odds of all-cause mortality with all other covariates remained similar in both models.
Discussion
The goal of this study was to identify risk factors associated with all-cause mortality in a large, diverse population of patients with COPD. This cohort is diverse by geography, socioeconomic status, and race. Like other studies, we found a significant association of all-cause mortality with co-morbidities and male sex.Citation2 In our age-adjusted model, Black/African American race was also associated with increased mortality. In addition to individual characteristics, we found that higher neighborhood disadvantage and urbanicity were associated with a higher age-adjusted all-cause mortality. Interestingly, when we controlled for all covariates, the association of Black/African American race with all-cause mortality was abrogated.
In this cohort, we found an increase in association with all-cause mortality with increasing neighborhood disadvantage. Lower individual socioeconomic status has widely been accepted to be associated with poorer outcomes in chronic disease. In a systematic review by Gershon et al, five studies described an inverse association of socioeconomic status with COPD mortality.Citation8 All these studies explore socioeconomic status based on individual characteristics, such as occupation, education and income, with one study containing over two million individuals. None were based on community or neighborhood socioeconomic status, as we used for this study. The causal factors of socioeconomic status with increased mortality are not fully understood. Gaps in health equity are associated with socioeconomic status. For example, lower SES has been associated with lower influenza vaccination rate, the latter is associated with higher COPD mortality.Citation9 For our population, all patients were enrolled in the VA Health Care System suggesting financial barriers to healthcare (eg, lack of insurance or high copays) were less likely significant contributors. However, many other factors associated with lower neighborhood SES, including poor air quality and deficient housing, need to be considered.
In our VA patient cohort, we found urban areas to be associated with higher all-cause mortality in people with COPD. This is notable because population studies observe people living in rural areas have higher rates of COPD-related mortality compared to people living in urban areas.Citation4 This difference is likely secondary to a higher baseline prevalence of COPD in rural areas. Urban areas are associated with higher levels of air pollution, as measured by PM2.5, in part due to the proximity to high volume roadways. Living in proximity to major roadways is associated with increased COPD and cardiovascular mortality.Citation10 Measurements of air pollution and/or proximity to major roadways may help define the association of urbanicity with mortality.
An interesting finding in our study was the association of all-cause mortality with race. In our analysis, we found Asian race was associated with lower odds and Black/African American race was associated with a higher odds of all-cause mortality in our age-adjusted model. However, this reversed for Black/African American when adjusted for all covariates including age, CCI, race, ADI, and urbanicity. This implies that race alone is not a determinant in all-cause mortality and that other factors included in our model, such as socioeconomic status, co-morbidities and urbanicity, influence the outcome. Further studies are necessary to evaluate the factors that contribute most to mortality in Black/African Americans with COPD.
The strength of our study includes a large and geographically broad cohort with patient-level data and precise residential geocodes to support spatially accurate assignments of neighborhood characteristics. Unlike other studies, this VA study is not subject to the geographic or age limitations found in insurance or Medicare datasets and supports the investigation of individuals with a pre-existing condition, such as COPD. The choice of all-cause mortality reduces biases in the attribution of the cause of death. The exact cause of death can be imprecise, particularly in people with multiple comorbidities, including chronic respiratory diseases where people often die from cardiovascular causes rather than respiratory failure.
Limitations include a predominantly male population and aggregated RUCA codes, with some suburbs being classified as rural. Since our population is limited to those seeking care in the Veterans Hospital Administration, our service-based cohort is biased towards males and limits our capacity to make conclusions for female populations. As is true in medical practice, the diagnosis of COPD in this study may not be accurate. We have chosen to define COPD as having at least a single encounter with COPD ICD code and age ≥35, rather than multiple encounters or a COPD hospitalization. Prior studies show that although COPD is frequently over-diagnosed, it is also under-diagnosed in a significant proportion of cases.Citation10 One factor contributing to misdiagnosis is underutilization of spirometry which is also a limitation in this observational study. Unexplored environmental exposures and comorbidities may additionally contribute to our associations. Exposure during military deployment may contribute to COPD progression and outcomes, although the long duration between service and COPD in our older population makes this less likely. In addition, smoking status was not available and is a known contributor to COPD outcomes. Air pollution was not explored but is another important contributor to early death and increased cardiovascular events.Citation10
In conclusion, all-cause mortality in patients with diagnosis of COPD is disproportionately higher in patients living in poorer neighborhoods and urban areas, suggesting the impact of social determinants of health on COPD outcomes. Black race was associated with higher age-adjusted all-cause mortality, but this association was abrogated after adjusting for gender, socioeconomic status, comorbidities, and urbanicity. Future studies should focus on exploring mechanisms by which disparities arise and developing interventions to address these.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
All authors declare that they have no conflict of interests related to this study.
Additional information
Funding
References
- World Health Organization. Chronic Obstructive Pulmonary Disease (COPD). World Health Organization; 2022. Available from https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd). Accessed July 17, 2023.
- Celli BR. Predictors of mortality in COPD. Respir Med. 2010;104(6):773–779. doi:10.1016/j.rmed.2009.12.017
- Brigham E, Allbright K, Harris D. Health disparities in environmental and occupational lung disease. Clin Chest Med. 2020;41(4):623–639. doi:10.1016/j.ccm.2020.08.009
- Croft JB, Wheaton AG, Liu Y, et al. Urban-rural county and state differences in chronic obstructive pulmonary disease - United States, 2015. MMWR Morb Mortal Wkly Rep. 2018;67(7):205–211. doi:10.15585/mmwr.mm6707a1
- Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi:10.1097/01.mlr.0000182534.19832.83
- Kind AJH, Buckingham W. Making neighborhood disadvantage metrics accessible: the neighborhood atlas. N Engl J Med. 2018;378:2456–2458. doi:10.1056/NEJMp1802313
- USDA ERS - Rural-Urban Commuting Area Codes. Rural-urban commuting area codes. United States Department of Agriculture; 2020. Available from: https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/. Accessed October 24, 2022.
- Gershon AS, Dolmage TE, Stephenson A, Jackson B. Chronic obstructive pulmonary disease and socioeconomic status: a systematic review. COPD. 2012;9(3):216–226. doi:10.3109/15412555.2011.648030
- Vukovic V, Lillini R, Lupi S, et al. Identifying people at risk for influenza with low vaccine uptake based on deprivation status: a systematic review. Eur J Public Health. 2020;30(1):132–141. doi:10.1093/eurpub/cky264
- Rosenbloom JI, Wilker EH, Mukamal KJ, Schwartz J, Mittleman MA. Residential proximity to major roadway and 10-year all-cause mortality after myocardial infarction. Circulation. 2012;125(18):2197–2203. doi:10.1161/CIRCULATIONAHA.111.085811
