Abstract
Background
Chronic Obstructive Pulmonary Disease (COPD) progression in the elderly is notably influenced by nutritional, immune, and inflammatory status. This study aimed to investigate the impact of adequate energy supply on these indicators in COPD patients.
Methods
COPD patients meeting specific criteria were recruited and categorized into energy-adequate and energy-deficient groups based on their energy supply. Comparable demographic factors such as age, gender, smoking and drinking history, COPD duration, inhaled drug classification, and home oxygen therapy application were observed. Notable differences were found in BMI and inhaled drug use between the two groups.
Results
The energy-adequate group exhibited significant improvements in various health indicators, including lymphocyte count, hemoglobin, CRP, total cholesterol, prealbumin, albumin, PNI, SII, SIRI, CAR, and CONUT scores in the secondary auxiliary examination. These positive changes suggest a notable enhancement in nutritional, immune, and inflammatory status.
Conclusion
This research highlights the substantial benefits of adequate energy supply in elderly COPD patients. The observed improvements in nutritional, immune, and inflammatory markers underscore the importance of addressing energy needs to positively influence disease-related outcomes in this population. These findings have implications for developing targeted interventions to optimize the well-being of elderly individuals with COPD.
Background
Chronic Obstructive Pulmonary Disease (COPD) is an umbrella term encompassing various chronic respiratory conditions characterized by partially reversible airway limitation. Among its principal manifestations are chronic bronchitis and emphysema, as extensively discussed in recent literature.Citation1–3 COPD has become a pressing global public health concern, particularly due to its rising prevalence among the elderly population. The World Health Organization ranks COPD as the third leading cause of death worldwide.Citation4–6 Patients afflicted with COPD frequently present with chronic cough, sputum production, and respiratory distress, significantly diminishing their quality of life.Citation7,Citation8 Furthermore, COPD often brings along a host of complications, including cardiovascular diseases, osteoporosis, and depression, adding to the complexity of patient care and management.Citation9–12
Recent studies have underscored the pivotal role of nutritional status in affecting the quality of life and survival rates of individuals with COPD.Citation13–16 In the realm of nutrition, suboptimal nutritional status has been linked to accelerated pulmonary function decline and an elevated risk of acute exacerbations.Citation17–19 Moreover, immune function plays a central role in the progression of COPD, with patients often experiencing heightened immune system activation, resulting in sustained inflammatory responses and airway remodeling. This systemic inflammation extends beyond the respiratory system, impacting other organ systems and giving rise to a myriad of complications.Citation20–22
Notably, despite the mounting evidence pointing to the association between nutrition and COPD, the specific role of energy supply in COPD management remains an understudied and insufficiently understood aspect. Adequate energy supply holds the potential to enhance patients’ nutritional status and optimize their immune function, thereby reducing inflammatory responses and enhancing the quality of life among elderly COPD patients.Citation23,Citation24 Furthermore, comprehending how energy supply influences the clinical manifestations and progression of COPD can provide valuable insights for optimizing COPD management and treatment strategies through nutritional intervention to enhance patient well-being.
To bridge this knowledge gap and shed light on the impact of energy supply on COPD patients, we have selected key assessment indicators, including the Prognostic Nutritional Index (PNI),Citation25 Systemic Immune-Inflammation Index (SII),Citation26 Systemic Inflammation Response Index (SIRI),Citation27 C-reactive protein/Albumin Ratio (CAR),Citation28 and Control Nutritional Status (CONUT) score.Citation29 These indicators serve as proxies for patients’ nutritional and immune status, offering a comprehensive window through which we can explore their relationship with COPD. By scrutinizing these assessment indicators, we aim to gain deeper insights into how energy supply influences the health status of elderly COPD patients.
This research endeavors to address the existing gap in knowledge concerning the role of energy supply in COPD management. It underscores the significance of ensuring sufficient energy intake in improving the nutritional, immune, and inflammatory status of elderly COPD patients. We aspire to uncover the specific effects of energy supply on this patient population through rigorous analysis and research, providing robust evidence and clinical guidance. This study is poised to offer a novel perspective and a solid theoretical foundation for the treatment of COPD, with the ultimate goal of enhancing the quality of life and increasing survival rates among elderly COPD patients. By unveiling the intricate relationship between energy supply and COPD, we anticipate opening up new avenues for research, thus propelling advancements in COPD treatment and management.
Materials and Methods
Diet and Energy Supply
Upon the initial admission of COPD patients, laboratory examination data were collected. Subsequent admissions of patients also involved the gathering of laboratory examination data. A survey on the dietary habits of patients in the six months prior to their second hospitalization was conducted. The Simplified Food Frequency Questionnaire (FFQ25) was employed to assess the dietary intake over the past half year. The daily nutritional intake was calculated.Citation30 Subsequently, the Basal Energy Expenditure (BEE) was computed using the Harris-Benedict formula, and the required energy was estimated utilizing an energy recommendation formula. Patients were categorized as having inadequate energy supply if they did not meet at least 70% of the required energy intake, otherwise classified as having adequate energy supply.
Selection of Research Subjects
Patients hospitalized in the Respiratory Medicine and General Medicine departments of Tianyou Hospital affiliated with Wuhan University of Science and Technology from July 2022 to May 2023, diagnosed with COPD, were selected. All patients provided informed consent in accordance with the Helsinki Declaration. (1) Inclusion criteria: ① Previously diagnosed with Chronic Obstructive Pulmonary Disease and meeting the GOLD 2023 diagnostic criteria, hospitalized due to an acute exacerbation of COPD; ② Age ≥65 years; ③ Able to cooperate to complete relevant surveys.Citation31 (2) Exclusion criteria: ① Patients with tumors, immune system diseases, and blood-related diseases; ② Patients with metabolic diseases such as thyroid dysfunction, active pulmonary tuberculosis, digestive system diseases; ③ Patients with respiratory failure and cor pulmonale; ④ Patients had not received treatment at this institution in the past 8 to 12 months. The study has been reviewed and approved by the Ethics Committee of Tianyou Hospital affiliated with Wuhan University of Science and Technology, with approval number [LL-2022-11-02-01].
Questionnaire Survey on Dietary Habits of COPD Patients Over the Last Six Months
This dietary survey questionnaire is divided into three parts: (1) Basic personal information, including name, age, gender, and BMI; (2) COPD-related information, including years since diagnosis, medication usage, use of inhalation drugs, and home oxygen therapy status; (3) A dietary survey using the simplified Food Frequency Questionnaire (FFQ25) to evaluate the dietary habits of patients over the past six months.Citation30
Collection of Laboratory Examination Data
Collect the following indicators at the time of the patient’s two admissions: white blood cell count, neutrophil count, lymphocyte count, monocyte count, hemoglobin concentration, platelet count, prealbumin concentration, globulin concentration, albumin concentration, C-reactive protein (CRP) concentration, and total cholesterol concentration.Citation32 For the auxiliary examination results from 8 to 12 months ago, they are defined as the first hospital admission auxiliary examination and labeled as “-1”. For the auxiliary examination results after this admission, they are defined as the second hospital admission auxiliary examination and labeled as “-2”. Calculate the difference between the two auxiliary examination results and label it as “-D-value”.
Calculation of Basal Energy Expenditure (BEE)
BEE is calculated according to the Harris-Benedict formula as follows:
Recommended energy for COPD patients = BEE * C * 1.1 * activity factor, where C is a correction factor (1.16 for men, 1.19 for women), and 1.1 is to correct the weight for patients with BMI below 18.5 kg/m2. Activity factor: 1.2 for bedridden, 1.3 for light activity, 1.5 for moderate activity, and 1.75 for intense activity.Citation33 If the patient does not achieve 70% of the required energy, it is an insufficient energy supply group. Otherwise, it is a sufficient energy supply group.
Scoring Standards
Controlling Nutritional Status (CONUT) ScoreCitation34 is calculated based on albumin, lymphocytes, and total cholesterol levels: Serum albumin level ≥35 g/L scores 0 points, 3034 g/L scores 2 points, 2529 g/L scores 4 points, and <25 g/L scores 6 points; Lymphocytes >1.6×109/L scores 0 points, (1.21.6)×109/L scores 1 point, (0.81.1)×109/L scores 2 points, <0.8×109/L scores 3 points; Total cholesterol >180 mg/dl scores 0 points, 140,179 mg/dl scores 1 point, 100,139 mg/dl scores 2 points, <100 mg/dl scores 3 points. Scores ranging from 01 point indicate normal nutrition, 24 points indicate mild malnutrition, 58 points indicate moderate malnutrition, and 912 points indicate severe malnutrition.
Prognostic Nutritional Index (PNI) = Albumin content (g/L) + 5× Lymphocyte count (109/L).Citation35 Systemic Immune-Inflammation Index (SII) = (Platelet count × Neutrophil count)/Lymphocyte count.Citation36 Systemic Inflammatory Response Index (SIRI) = (Neutrophil count × Monocyte count)/Lymphocyte count.Citation37 C-Reactive Protein/Albumin Ratio (CAR) = C-Reactive Protein concentration/Albumin concentration × 100%.Citation38
Statistical Methods
Data analysis and graphing were performed using SPSS 26.0 software and GraphPad Prism 9. For continuous variables, normality will first be tested. If data are normally distributed, mean ± standard deviation (x ± s) will be used, and independent sample t-tests will be applied to compare the two groups. Non-normally distributed data will be presented as median (interquartile range) [M(Q1, Q3)] and comparisons between groups will be performed using the Mann–Whitney U-test. Count data will be presented in number or percentage, with intergroup comparisons performed using χ2 tests. A P-value <0.05 will be considered statistically significant.
Results
Significant Disparities in BMI and Inhalation Drug Usage Between Elderly COPD Patients with Adequate and Inadequate Energy Supply
In this study, 119 qualified COPD patients were successfully enrolled, dominated by males (71.4%, 85 people), and females accounted for 28.6% (34 people). All study participants were aged between 65 and 99, with an average age of 77.53 and a standard deviation of 8.62, presenting a research group mainly composed of elderly patients.
Based on whether the energy supply met the recommended standards, we classified the subjects into two groups: those meeting energy requirements (77 people) and those who did not (42 people). After a thorough discussion and comparison of both groups in multiple aspects (including age, gender, smoking history, drinking history, COPD duration, classification of inhaled drugs, and the usage of home oxygen therapy), no statistically significant differences were found (P>0.05) in these aspects. However, significant statistical differences were found in BMI and inhaled drug use between the two groups (P<0.05) (), meaning these factors could potentially influence our research outcomes.
Table 1 Comparison of Basic Data Between Group with Energy Met the Standards and Group with Energy Did Not Meet the Standards
In summary, our sample population exhibited certain diversities, yet most aspects (except BMI and inhalation drug usage) demonstrated no significant difference between the two groups, providing a relatively balanced basis for exploring the impact of energy adequacy on elderly COPD patients.
First Admission Auxiliary Examination Reveals No Significant Differences in Multiple Biochemical Indicators Between Elderly COPD Patients Meeting and Not Meeting Energy Standards
While exploring the results of a preliminary auxiliary examination before patients’ admission, we conducted a thorough analysis of the performance of two groups of patients (those meeting energy requirements and those not meeting energy requirements) across multiple biochemical markers and scoring systems. Specifically, we considered the following parameters: white blood cell count, neutrophil count, lymphocyte count, platelet count, monocyte count, hemoglobin, C-reactive protein (CRP), total cholesterol, prealbumin, albumin, globulin, and several scores based on these parameters, including the CONUT score, Prognostic Nutritional Index (PNI), Systemic Immune-Inflammation Index (SII), Systemic Inflammatory Response Index (SIRI), and C-reactive protein/Albumin Ratio (CAR).
Upon detailed analysis of these data, we discovered no statistically significant differences between the two groups across all these markers and scoring systems, with all P-values exceeding 0.05. This study indicates no notable disparities between elderly COPD patients who met energy requirements and those who did not in these particular health and nutritional markers (). This finding implies that, from the perspective of this suite of biochemical markers and scoring systems, whether or not the energy supply was met did not exhibit a significant impact in this pre-admission examination. It also provides a relatively stable and balanced baseline to further explore the potential impacts of meeting energy requirements on other aspects of elderly COPD patients.
Table 2 Comparison of Initial Auxiliary Examinations Between Group with Energy Met the Standards and Group with Energy Did Not Meet the Standards
Second Admission Auxiliary Examination Shows Elderly COPD Patients Meeting Energy Standards Perform Better on Multiple Key Biochemical Indicators
Upon delving into the results of the secondary auxiliary examination upon readmission, we meticulously compared the performance of the energy-meeting group and the non-energy-meeting group across a range of biochemical markers and scoring systems. This phase of examination allowed us to gain deeper insights into the differences and similarities in biochemical parameters between these two groups of patients.
Following careful analysis, we discovered no statistically significant differences between the two groups in white blood cell count, neutrophil count, platelet count, monocyte count, and globulin (P>0.05), indicating a relative consistency in these particular markers between elderly COPD patients who met energy requirements and those who did not. However, we also noted that there were significant statistical differences between the two groups in lymphocyte count, hemoglobin, C-reactive protein (CRP), total cholesterol, prealbumin, albumin, CONUT score and rating, Prognostic Nutritional Index (PNI), Systemic Immune-Inflammation Index (SII), Systemic Inflammatory Response Index (SIRI), C-reactive protein/Albumin Ratio (CAR), and total protein (P<0.05), suggesting that the status of energy provision significantly influences these markers ().
Table 3 Comparison of Secondary Auxiliary Examination Data Between Group with Energy Met the Standards and Group with Energy Did Not Meet the Standards
The percentage of lymphocyte count reduction is related to the risk of deterioration.Citation39 C-reactive protein (CRP) serves as an inflammation marker.Citation40 Prealbumin is sensitive to acute changes in nutritional status and has become the preferred indicator of malnutrition in critically ill patients.Citation41 Patients who met their energy requirements showed significantly higher levels of lymphocyte percentage, hemoglobin concentration, total cholesterol concentration, prealbumin concentration, and albumin concentration compared to those who did not meet their energy requirements, indicating sufficient nutrition in the former group. Furthermore, patients who met their energy requirements had markedly lower levels of C-reactive protein (CRP) than those who did not, suggesting a lower level of inflammation in the former group ().
In summary, the results of the secondary auxiliary examination upon readmission indicate that while certain biochemical markers exhibited no differences between the two groups, the majority of indicators and scoring systems displayed significant disparities, underscoring the importance of ensuring elderly COPD patients receive adequate energy supply to optimize their biochemical parameters and potentially improve their prognosis.
Elderly COPD Patients Meeting Energy Requirements Demonstrate More Positive Changes in Key Biochemical and Immune Indicators Between Two Consecutive Hospital Admissions
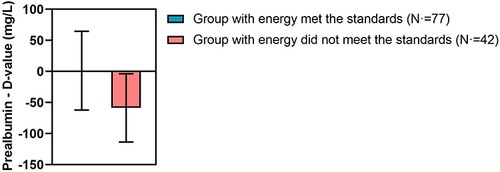
We further investigated the changes in various indicators between the two groups of patients during two hospital admissions. Initially, we calculated the differences in indicators between the two admissions and compared the changes in these differences between the groups to better understand the long-term effects of meeting energy requirements on elderly COPD patients. Our data revealed significant statistical differences (P < 0.05) between the two groups in prognostic nutritional index (PNI), systemic immune inflammation index (SII), systemic inflammation response index (SIRI), C-reactive protein to albumin ratio (CAR), albumin, CONUT score, and prealbumin (). Specifically, there were minimal differences in PNI (), albumin concentration (), and prealbumin concentration () before and after in the energy-adequate group, whereas these indicators showed significant changes in the energy-inadequate group compared to the energy-adequate group. This outcome indicates a significant difference in the trend of changes in these specific indicators between the energy-adequate and energy-inadequate groups, suggesting that energy supply status can significantly impact the biochemical and immune parameter changes in elderly COPD patients over a period of time. This difference underscores the crucial role of sufficient energy supply in maintaining and improving some key physiological indicators in elderly COPD patients, serving as an effective intervention strategy to aid in managing the health and well-being of this population.
Table 4 Comparison of the Difference in Auxiliary Examination Between Group with Energy Met the Standards and Group with Energy Did Not Meet the Standards
Figure 1 Bar graph of PNI differences between the Energy Standard Group and the Non-Energy Standard Group across two auxiliary examinations.
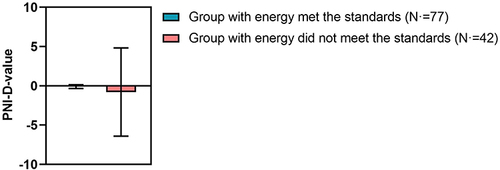
Figure 2 Bar graph of Albumin differences between the Energy Standard Group and the Non-Energy Standard Group across two auxiliary examinations.
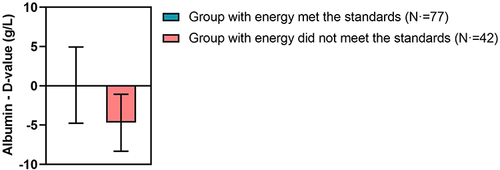
Figure 3 Bar graph of Prealbumin differences between the Energy Standard Group and the Non-Energy Standard Group across two auxiliary examinations.
Overall, by comparing the differences between the two admissions, we can observe that meeting or not meeting energy standards impacts a series of important indicators in elderly COPD patients, highlighting the central role of nutritional intervention in COPD management.
Discussion
Chronic Obstructive Pulmonary Disease (COPD) has long been recognized as a complex condition closely intertwined with the nutritional and immune status of affected individuals.Citation17,Citation42 In this study, we undertake a comprehensive exploration of the impact of meeting energy supply standards on various facets of elderly COPD patients, encompassing their nutritional status, immune function, and inflammatory response. We will delve into these findings, emphasizing their implications in the context of existing research.
A noteworthy development in the 2023 GOLD guidelines is the reclassification of COPD, shifting from the previous ABCD system to the new ABE classification.Citation43,Citation44 While groups A and B remain unchanged, the merger of the previous C and D groups into the new E group underscores the unique challenges faced by E group patients. These individuals contend with heightened respiratory resistance, leading to increased resting respiratory effort. This not only triggers a heightened systemic inflammatory response but also exacerbates overall oxidative stress. The oxidative stress amplifies energy expenditure, a factor compounded by the often compromised digestive function seen in elderly COPD patients. Collectively, these factors unequivocally emphasize the critical importance of adequate energy supply, particularly for those in the E group.Citation45
Our study unearths significant differences between two admissions, specifically in lymphocyte count, hemoglobin, CRP, total cholesterol, prealbumin, albumin, CONUT score, PNI, SII, SIRI, CAR, and total protein indicators. Furthermore, the variations in these indicators between the two admissions highlight that sufficient energy supply can markedly improve numerous nutritional and immune-inflammatory parameters in patients.
Initial observations establish a significant association between BMI and adequate energy supply. While our current data does not directly demonstrate improved BMI due to sufficient energy intake, prior studies have convincingly illustrated that adequate nutrition can effectively enhance BMI.Citation46–48 The CONUT score, originally designed to assess malnutrition, has evolved to predict the prognosis of patients with tumors and severe infections, capitalizing on clinical correlations between hypoproteinemia, lymphopenia, cholesterol, and infection.Citation25,Citation34 Notably, the primary distinction between PNI and the COUNT score lies in cholesterol concentration, with PNI demonstrating predictive value in the prognosis of acute exacerbation of COPD.Citation49
Moreover, during acute infection episodes, clinicians frequently employ albumin and C-reactive protein (CRP) in tandem to assess overall nutritional status.Citation28,Citation50,Citation51 Under stressful conditions, catabolic metabolism surges, leading to a decline in plasma protein levels. Integrating CRP levels enables the analysis of inflammation degree and the understanding of body protein wear due to infection.Citation52 Our study affirms that adequate energy supply effectively ameliorates CAR levels, indicating reduced protein wear under equivalent inflammation levels. This underscores the pivotal role of ample energy supply in enhancing the nutritional, immune, and inflammatory states of elderly COPD patients.
COPD is inherently a chronic inflammatory disease, with elevated inflammatory cytokine levels observed even during stable periods, impacting neutrophil, platelet, and lymphocyte levels.Citation53,Citation54 This provides valuable diagnostic and treatment opportunities through accessible auxiliary examinations. SII and SIRI, indicative of systemic inflammation and immune status, are elevated in cases of heightened systemic inflammation, known to be associated with COPD exacerbations and severe deteriorations. Adequate energy supply, as per our research, demonstrates observable improvements in inflammatory indicators.Citation55
While our study offers valuable insights, it is not without limitations. The gender imbalance in the study population, with a predominance of male patients, likely reflects higher smoking rates among males. Additionally, the lack of age variation between patient groups can be attributed to effective dietary education or the repeated admissions of some participants. Future research endeavors should aim to validate and expand our findings with larger sample sizes and a broader spectrum of variables. Moreover, exploring other facets of nutritional structure could offer a more comprehensive understanding of its potential value in COPD management.
Conclusion
In summation, our study underscores the paramount importance of meeting energy supply standards in the management of elderly COPD patients (). Adequate energy supply contributes to better immune levels and lower inflammation response in elderly COPD patients, which in turn facilitates disease recovery. Our findings unequivocally demonstrate that meeting these standards significantly enhances nutritional status, immune function, and inflammatory responses in this patient population. While our study has certain limitations, it lays a robust foundation for future research, showcasing the potential efficacy of nutritional intervention in improving the prognosis of elderly COPD patients. We eagerly anticipate further validation and expansion of our findings, which will undoubtedly contribute to the refinement of clinical COPD management practices.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethical Statement
The study has been reviewed and approved by the Ethics Committee of Tianyou Hospital affiliated with Wuhan University of Science and Technology, with approval number [LL-2022-11-02-01].
Disclosure
The authors declare no competing interest in this work.
Additional information
Funding
References
- Buhr RG, Barjaktarevic IZ, Quibrera PM, et al. Reversible airflow obstruction predicts future chronic obstructive pulmonary disease development in the SPIROMICS cohort: an observational cohort study. Am J Respir Crit Care Med. 2022;206(5):554–562. doi:10.1164/rccm.202201-0094OC
- Labaki WW, Rosenberg SR. Chronic obstructive pulmonary disease. Ann Intern Med. 2020;173(3):ITC17–ITC32. doi:10.7326/AITC202008040
- Christenson SA, Smith BM, Bafadhel M, Putcha N. Chronic obstructive pulmonary disease. Lancet. 2022;399(10342):2227–2242. doi:10.1016/S0140-6736(22)00470-6
- Adeloye D, Song P, Zhu Y, et al. Global, regional, and national prevalence of, and risk factors for, chronic obstructive pulmonary disease (COPD) in 2019: a systematic review and modelling analysis. Lancet Respir Med. 2022;10(5):447–458. doi:10.1016/S2213-2600(21)00511-7
- Stolz D, Mkorombindo T, Schumann DM, et al. Towards the elimination of chronic obstructive pulmonary disease: a lancet commission. Lancet. 2022;400(10356):921–972. doi:10.1016/S0140-6736(22)01273-9
- Lareau SC, Fahy B, Meek P, Wang A. Chronic Obstructive Pulmonary Disease (COPD). Am J Respir Crit Care Med. 2019;199(1):P1–P2. doi:10.1164/rccm.1991P1
- MacLeod M, Papi A, Contoli M, et al. Chronic obstructive pulmonary disease exacerbation fundamentals: diagnosis, treatment, prevention and disease impact. Respirology. 2021;26(6):532–551. doi:10.1111/resp.14041
- Landt E, Çolak Y, Lange P, Laursen LC, Nordestgaard BG, Dahl M. Chronic cough in individuals with COPD: a population-based cohort study. Chest. 2020;157(6):1446–1454. doi:10.1016/j.chest.2019.12.038
- Regard L, Burgel PR, Roche N. Inhaled therapy, cardiovascular risk and benefit-risk considerations in COPD: innocent until proven guilty, or vice versa? Eur Respir J. 2023;61(2):2202135. doi:10.1183/13993003.02135-2022
- André S, Conde B, Fragoso E, et al. COPD and Cardiovascular Disease. Pulmonology. 2019;25(3):168–176. doi:10.1016/j.pulmoe.2018.09.006
- Chen YW, Ramsook AH, Coxson HO, Bon J, Reid WD. Prevalence and risk factors for osteoporosis in individuals with COPD: a systematic review and meta-analysis. Chest. 2019;156(6):1092–1110. doi:10.1016/j.chest.2019.06.036
- Iyer AS, Sullivan DR, Lindell KO, Reinke LF. The role of palliative care in COPD. Chest. 2022;161(5):1250–1262. doi:10.1016/j.chest.2021.10.032
- Ferrera MC, Labaki WW, Han MK. Advances in chronic obstructive pulmonary disease. Annu Rev Med. 2021;72:119–134. doi:10.1146/annurev-med-080919-112707
- Vizza CD, Hoeper MM, Huscher D, et al. Pulmonary hypertension in patients with COPD: results From the Comparative, Prospective Registry of Newly Initiated Therapies for Pulmonary Hypertension (COMPERA). Chest. 2021;160(2):678–689. doi:10.1016/j.chest.2021.02.012
- Tramontano A, Palange P. Nutritional State and COPD: effects on Dyspnoea and Exercise Tolerance. Nutrients. 2023;15(7):1786. doi:10.3390/nu15071786
- van Beers M, Rutten-van Mölken MPMH, van de Bool C, et al. Clinical outcome and cost-effectiveness of a 1-year nutritional intervention programme in COPD patients with low muscle mass: the randomized controlled NUTRAIN trial. Clin Nutr. 2020;39(2):405–413. doi:10.1016/j.clnu.2019.03.001
- Scoditti E, Massaro M, Garbarino S, Toraldo DM. Role of diet in chronic obstructive pulmonary disease prevention and treatment. Nutrients. 2019;11(6):1357. doi:10.3390/nu11061357
- Espírito Santo C, Caseiro C, Martins MJ, Monteiro R, Brandão I. Gut microbiota, in the halfway between nutrition and lung function. Nutrients. 2021;13(5):1716. doi:10.3390/nu13051716
- Manuel SS, Luis GM. Nutrition, obesity and asthma inception in children. the role of lung function. Nutrients. 2021;13(11):3837. doi:10.3390/nu13113837
- Cho SJ, Stout-Delgado HW. Aging and lung disease. Annu Rev Physiol. 2020;82:433–459. doi:10.1146/annurev-physiol-021119-034610
- Voynow JA, Shinbashi M. Neutrophil elastase and chronic lung disease. Biomolecules. 2021;11(8):1065. doi:10.3390/biom11081065
- Radzikowska U, Ding M, Tan G, et al. Distribution of ACE2, CD147, CD26, and other SARS-CoV-2 associated molecules in tissues and immune cells in health and in asthma, COPD, obesity, hypertension, and COVID-19 risk factors. Allergy. 2020;75(11):2829–2845. doi:10.1111/all.14429
- Xue M, Zeng Y, Lin R, et al. Metabolomic profiling of anaerobic and aerobic energy metabolic pathways in chronic obstructive pulmonary disease. Exp Biol Med. 2021;246(14):1586–1596. doi:10.1177/15353702211008808
- Wingårdh ASL, Göransson C, Larsson S, Slinde F, Vanfleteren LEGW. Effectiveness of Energy Conservation Techniques in Patients with COPD. Respiration. 2020;99(5):409–416. doi:10.1159/000506816
- Okadome K, Baba Y, Yagi T, et al. Prognostic nutritional index, tumor-infiltrating lymphocytes, and prognosis in patients with esophageal cancer. Ann Surg. 2020;271(4):693–700. doi:10.1097/SLA.0000000000002985
- Keit E, Coutu B, Zhen W, et al. Systemic inflammation is associated with inferior disease control and survival in stage III non-small cell lung cancer. Ann Transl Med. 2021;9(3):227. doi:10.21037/atm-20-6710
- Song M, Zhang Q, Song C, et al. The advanced lung cancer inflammation index is the optimal inflammatory biomarker of overall survival in patients with lung cancer. J Cachexia Sarcopenia Muscle. 2022;13(5):2504–2514. doi:10.1002/jcsm.13032
- Choe H, Kobayashi N, Abe K, Hieda Y, Tezuka T, Inaba Y. Evaluation of serum albumin and globulin in combination with C-reactive protein improves serum diagnostic accuracy for low-grade periprosthetic joint infection. J Arthroplasty. 2023;38(3):555–561. doi:10.1016/j.arth.2022.09.011
- Kleckner AS, Culakova E, Kleckner IR, et al. Nutritional Status predicts fatty acid uptake from fish and soybean oil supplements for treatment of cancer-related fatigue: results from a phase II Nationwide Study. Nutrients. 2021;14(1):184. doi:10.3390/nu14010184
- Ahmed S, Rahman T, Ripon MSH, et al. A food frequency questionnaire for hemodialysis patients in Bangladesh (BDHD-FFQ): development and validation. Nutrients. 2021;13(12):4521. doi:10.3390/nu13124521
- Venkatesan P. GOLD COPD report: 2023 update. Lancet Respir Med. 2023;11(1):18. doi:10.1016/S2213-2600(22)00494-5
- Escobedo-Monge MF, Barrado E, Parodi-Román J, Escobedo-Monge MA, Torres-Hinojal MC, Marugán-Miguelsanz JM. Magnesium status and Ca/Mg ratios in a series of children and adolescents with chronic diseases. Nutrients. 2022;14(14):2941. doi:10.3390/nu14142941
- Byerly S, Vasileiou G, Qian S, et al. Early hypermetabolism is uncommon in trauma intensive care unit patients. JPEN J Parenter Enteral Nutr. 2022;46(4):771–781. doi:10.1002/jpen.1945
- Ignacio de Ulíbarri J, González-Madroño A, de Villar NG, et al. CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp. 2005;20(1):38–45.
- Pinato DJ, North BV, Sharma R. A novel, externally validated inflammation-based prognostic algorithm in hepatocellular carcinoma: the prognostic nutritional index (PNI). Br J Cancer. 2012;106(8):1439–1445. doi:10.1038/bjc.2012.92
- Yang YL, Wu CH, Hsu PF, et al. Systemic immune-inflammation index (SII) predicted clinical outcome in patients with coronary artery disease. Eur J Clin Invest. 2020;50(5):e13230. doi:10.1111/eci.13230
- Li S, Yang Z, Du H, Zhang W, Che G, Liu L. Novel systemic inflammation response index to predict prognosis after thoracoscopic lung cancer surgery: a propensity score-matching study. ANZ J Surg. 2019;89(11):E507–E513. doi:10.1111/ans.15480
- Yamauchi Y, Safi S, Muley T, et al. C-reactive protein-albumin ratio is an independent prognostic predictor of tumor recurrence in stage IIIA-N2 lung adenocarcinoma patients. Lung Cancer. 2017;114:62–67. doi:10.1016/j.lungcan.2017.11.002
- Chen TT, Lee KY, Chang JH, et al. Prediction value of neutrophil and eosinophil count at risk of COPD exacerbation. Ann Med. 2023;55(2):2285924. doi:10.1080/07853890.2023.2285924
- Lv MY, Jin LL, Sang XQ, et al. Abhd2, a Candidate gene regulating airway remodeling in COPD via TGF-β. Int J Chron Obstruct Pulmon Dis. 2024;19:33–50. doi:10.2147/COPD.S440200
- Sneh A, Pawan T, Randeep G, et al. Acute phase proteins as predictors of survival in patients with acute exacerbation of chronic obstructive pulmonary disease requiring mechanical ventilation. COPD. 2020;17(1):22–28. doi:10.1080/15412555.2019.1698019
- Agustí A, Melén E, DeMeo DL, Breyer-Kohansal R, Faner R. Pathogenesis of chronic obstructive pulmonary disease: understanding the contributions of gene-environment interactions across the lifespan. Lancet Respir Med. 2022;10(5):512–524. doi:10.1016/S2213-2600(21)00555-5
- Agustí A, Celli BR, Criner GJ, et al. Global initiative for chronic obstructive lung disease 2023 report: GOLD executive summary. Eur Respir J. 2023;61(4):2300239. doi:10.1183/13993003.00239-2023
- Soriano JB, Horner A, Studnicka M, et al. The GOLD 2023 proposed taxonomy: a new tool to determine COPD etiotypes. Eur Respir J. 2023;61(6):2300466. doi:10.1183/13993003.00466-2023
- Agustí A, Celli BR, Criner GJ, et al. Global initiative for chronic obstructive lung disease 2023 report: GOLD executive summary. Am J Respir Crit Care Med. 2023;207(7):819–837. doi:10.1164/rccm.202301-0106PP
- Bianchi VE, Herrera PF, Laura R. Effect of nutrition on neurodegenerative diseases. A systematic review. Nutr Neurosci. 2021;24(10):810–834. doi:10.1080/1028415X.2019.1681088
- Holmes CJ, Racette SB. The utility of body composition assessment in nutrition and clinical practice: an overview of current methodology. Nutrients. 2021;13(8):2493. doi:10.3390/nu13082493
- Miele MJ, Souza RT, Calderon IM, et al. Maternal nutrition status associated with pregnancy-related adverse outcomes. Nutrients. 2021;13(7):2398. doi:10.3390/nu13072398
- Kaluźniak-Szymanowska A, Krzymińska-Siemaszko R, Deskur-śmielecka E, Lewandowicz M, Kaczmarek B, Wieczorowska-Tobis K. Malnutrition, sarcopenia, and malnutrition-sarcopenia syndrome in older adults with COPD. Nutrients. 2021;14(1):44. doi:10.3390/nu14010044
- Rathore SS, Oberoi S, Iqbal K, et al. Prognostic value of novel serum biomarkers, including C-reactive protein to albumin ratio and fibrinogen to albumin ratio, in COVID-19 disease: a meta-analysis. Rev Med Virol. 2022;32(6):e2390. doi:10.1002/rmv.2390
- Seoudy H, Shamekhi J, Voigtländer L, et al. C-reactive protein to albumin ratio in patients undergoing transcatheter aortic valve replacement. Mayo Clin Proc. 2022;97(5):931–940. doi:10.1016/j.mayocp.2021.11.022
- Sheriff A, Kayser S, Brunner P, Vogt B. C-reactive protein triggers cell death in ischemic cells. Front Immunol. 2021;12:630430. doi:10.3389/fimmu.2021.630430
- Herrero-Cervera A, Soehnlein O, Kenne E. Neutrophils in chronic inflammatory diseases. Cell Mol Immunol. 2022;19(2):177–191. doi:10.1038/s41423-021-00832-3
- Yang A, Wu Y, Yu G, Wang H. Role of specialized pro-resolving lipid mediators in pulmonary inflammation diseases: mechanisms and development. Respir Res. 2021;22(1):204. doi:10.1186/s12931-021-01792-y
- Liu X, Ge H, Feng X, et al. The combination of hemogram indexes to predict exacerbation in stable chronic obstructive pulmonary disease. Front Med. 2020;7:572435. doi:10.3389/fmed.2020.572435