Abstract
Introduction
While cross-national studies have documented rates of chronic obstructive pulmonary disease (COPD) misdiagnosis among patients in primary care, US studies are scarce. Studies investigating diagnosis among uninsured patients are lacking.
Objective
The purpose of this study is to identify patients who are over diagnosed and thus, mistreated, for COPD in a federally qualified health center.
Methods
A descriptive study was conducted for a retrospective cohort from February 2011 to June 2012. Spirometry was performed by trained personnel following American Thoracic Society recommendations. Patients were referred for spirometry to confirm previous COPD diagnosis or to assess uncontrolled COPD symptoms. Airway obstruction was defined as a forced expiratory volume in the first second of expiration (FEV1) to forced vital capacity ratio less than 0.7. Reversibility was defined as a postbronchodilator increase in FEV1 greater than 200 mL and greater than 12%.
Results
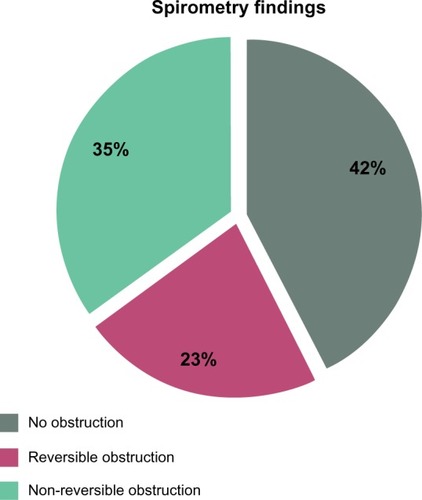
Eighty patients treated for a previous diagnosis of COPD (n = 72) or on anticholinergic inhalers (n = 8) with no COPD diagnosis were evaluated. The average age was 52.9 years; 71% were uninsured. Only 17.5% (14/80) of patients reported previous spirometry. Spirometry revealed that 42.5% had no obstruction, 22.5% had reversible obstruction, and 35% had non-reversible obstruction.
Conclusion
Symptoms and smoking history are insufficient to diagnose COPD. Prevalence of COPD over diagnosis among uninsured patient populations may be higher than previously reported. Confirming previous COPD diagnosis with spirometry is essential to avoid unnecessary and potentially harmful treatment.
Introduction
Chronic obstructive pulmonary disease (COPD) is a common, preventable, and treatable disease characterized by progressive airflow limitation. Associated with airway chronic inflammatory response and by lung noxiousness to particles or gases, COPD is the third leading cause of death in the US and has an estimated worldwide prevalence of 10% in people over 40 years.Citation1 The annual cost of treatment per COPD patient in the US is $4,119 (USD); additionally, indirect nonmedical care costs of $1,527 (USD) per patient are known.Citation2 While other leading causes of death in the US have declined steadily, COPD death rates have doubled since 1970.Citation3
COPD disproportionately afflicts those of lower socioeconomic status and older adults, creating reluctance to diagnose and treat patients.Citation4 The Global Initiative for Chronic Obstructive Lung Disease report in 2011, emphasizing the significance of this disease, confirmed that spirometry is a requirement for COPD case definition.Citation5
Spirometry has the distinct advantage of being a reproducible measurement of lung function that is superior to peak expiratory flow because of greater reliability and specificity.Citation6 Symptom based and clinical diagnosis contributes to misdiagnosis and mistreatment.Citation7,Citation8 Additionally, spirometry can distinguish between asthma and COPD.Citation9
Only one US study has investigated the prevalence of COPD misdiagnosis with spirometry.Citation10 However, generalizability of this study was limited: patients were gathered from primary care practices in Colorado and Scotland.Citation10 Studies investigating COPD diagnosis among the uninsured are absent. The purpose of this study is to evaluate clinically diagnosed COPD patients with spirometry to ascertain COPD misdiagnosis in an underserved population.
Methods
A descriptive study was conducted at a federally qualified health center following institutional review board approval. The retrospective cohort from February 2011 to June 2012 included all patients who were referred by primary care providers for spirometry testing available at the health center to confirm a previous COPD diagnosis or for better management of uncontrolled COPD symptoms. Spirometry was done according to procedures recommended by the American Thoracic Society using the Burdick SpiroCard® (Cardiac Science, Hannover, Germany).Citation11 Spirometry for each patient was performed by personnel who had undergone training on how to use the spirometry program. Personnel were also trained on device calibration, as well as recording all procedure relevant data. A series of questions was asked to the patients to identify contraindications for spirometry testing. Patients with acute respiratory illness were rescheduled after infection resolution and symptom improvement. All referred patients did not use a short acting beta agonist within 6 hours, a long acting beta agonist within 12 hours, ipratropium within 6 hours, tiotropium within 24 hours, or theophylline within 24 hours of the test. A forced expiratory volume in the first second of expiration to forced vital capacity (FEV1/FVC) ratio above or equal to 0.7 was designated as no obstruction.Citation5 FEV1/FVC ratio below 0.7 required further evaluation with postbronchodilator testing.
For postbronchodilator testing, 400 μg of beta2 agonist (albuterol) with a spacer was administered. Following the administration of the beta2 agonist and a 15 minute waiting period, postbronchodilator spirometry values were reassessed. Increased FEV1 > 12% and >200 mL when compared with baseline confirmed reversibility.Citation12
Patients were categorized as either no obstruction, reversible obstruction, or nonreversible obstruction. Differences by age and pack year history for each group were assessed using analysis of variance and tabulation of mean and standard deviation. Statistical significance was assumed at P ≤ 0.05.
Results
Eighty patients were referred for spirometry testing. Out of the 80 patients referred, 72 had a previous diagnosis of COPD (72 out of 444 patients at the clinic) and eight were on anticholinergic inhalers but had no previous COPD diagnosis (eight out of 51 patients at the clinic). The average age was 52.9 ± 7.7 years. The majority of patients were self-pay patients (71.3%), Caucasians (88.8%), and females (60%). Across all patients, average pack years was 37.9 ± 26.1. Five patients in this study never smoked, three had previous COPD diagnosis, and two were on anticholinergic inhalers but had no previous COPD diagnosis. All five patients had spirometry results consistent with no obstruction. In the group of patients with previous COPD diagnosis, three patients claimed that COPD diagnosis was made prior to the age of 35 years. Spirometry results showed no obstruction for two of those patients and reversible obstruction for the third patient. Additionally, in the group of patients with previous COPD diagnosis, 18 patients did not remember when they were first diagnosed with COPD, and only 14 patients remembered having spirometry or pulmonary function testing. includes all characteristics of patients referred for spirometry.
Table 1 Characteristics of patients referred for spirometry
Spirometry revealed 34 patients (42.5%) with no obstruction, 18 patients (22.5%) with reversible obstruction, and 28 patients (35%) with nonreversible obstruction (). Younger patients (P = 0.004) and patients who had fewer pack years of exposure (P = 0.013) were more likely to be in the no obstruction group. Patients in the nonreversible obstruction group were more likely to be older and had 1.7 times more tobacco exposure.
Discussion
Spirometry confirms COPD diagnosis in the primary care setting.Citation13–Citation15 However, a Vermont survey found that only 66% of primary care respondents owned a spirometer and that spirometry was only performed on half of COPD patients.Citation16 In our study, only 14 patients (17.5%) reported a previous spirometry or pulmonary function testing. When spirometry is not used, practitioners use smoking history and clinical features for COPD diagnosis which lacks sensitivity.Citation17 Additionally, spirometry differentiates between asthma and COPD which have different therapy goals and treatment plans. Reliance on nonspecific symptoms of dyspnea, cough, and wheezing has resulted in health practitioners responding to two physiologically different diseases in the same manner.Citation5,Citation18,Citation19 Inappropriate diagnosis leads to inappropriate symptom management and ignorance of underlying etiology. Unnecessary medications, poor management, and side effects associated with inappropriate medications increase the overall cost while potentially harming the patient. Known side effects associated with medications used by these patients may include angioedema, anaphylaxis, bronchospasm, arrhythmia, glaucoma, and adrenal suppression.Citation20
The presence of over diagnosis in the current series of COPD patients − 42.5% – is consistent with reports outside of the US. International studies have examined the prevalence of COPD misdiagnosis due to lack of spirometry. COPD misdiagnosis was 31% in Australia,Citation7 28.6% in Belgium,Citation9 25.8% in Norway,Citation21 27.2% in the UK,Citation22 and 49.8% in Greece.Citation23 One study which combined patients from Colorado and Scotland documented a 51.6% COPD misdiagnosis ().Citation10
Table 2 Comparison of studies that highlighted the magnitude of chronic obstructive pulmonary disease over diagnosis
Studies vary in their definition of reversible obstructions. Due to literature inconsistency and discrepant guidelines, we decided to only consider results that showed no obstruction (FEV1/FVC ≥ 0.7) as a clear COPD misdiagnosis. Although being diagnosed with or treated for COPD, 42.5% of our patients showed no obstruction on spirometry. Given that some of the patients who had reversible obstruction could have asthma and not COPD, prevalence of COPD misdiagnosis could be higher in this series. Since the only study performed in the US included patients from Scotland and Colorado,Citation10 the prevalence of COPD misdiagnosis in the US remains unclear. Additionally, our results may be more representative of uninsured and underserved patients.
Lower European COPD misdiagnosis could be linked to emphasis on spirometry in ambulatory settings.Citation18 Low utilization of spirometry in the US may be attributed to factors such as unawareness of the value of spirometry, lack of access, busy settings, and lack of device training.Citation16 Another major challenge is provider perception of test uncertainty and the inability to interpret spirometry data.Citation24 Incorporating training seminars to educate health professionals has shown promise, increasing spirometry use by 59% in a 3 month period following training.Citation16
This study is the first to examine COPD misdiagnosis and prevalence of spirometry in a group of solely American patients. Study limitations include patient recall bias and data entry errors in the medical record. The current series was only referred for spirometry based on the individual provider’s preferences to manage uncontrolled COPD or to confirm previously diagnosed COPD. Therefore, current data may not be representative and should be viewed as a pilot investigation to assess COPD in an underserved population. However, current data suggest that there is a problem with COPD over diagnosis in the underserved population and that problem could be significant due to the lack of resources. The underserved population may have more risk for fragmented care and lack of access to health care resources which could make them more vulnerable to such issues. More research in this area is needed, especially in the underserved population. Justification of offering free or discounted spirometry service could be explored based on anticipated cost avoidance of misdiagnosed COPD cases.
Conclusion
Symptoms and smoking history are insufficient to diagnose COPD. Prevalence of COPD over diagnosis in uninsured patient populations may be higher than previously reported. Confirming COPD diagnosis with spirometry is essential to avoid unnecessary and potentially harmful over treatment.
Disclosure
The authors report no conflicts of interest in this work
References
- BuistASMcBurnieMAVollmerWMBOLD Collaborative Research GroupInternational variation in the prevalence of COPD (the BOLD Study): a population-based prevalence studyLancet2007370958974175017765523
- HalpernMTStanfordRHBorkerRThe burden of COPD in the USA: results from the Confronting COPD surveyRespir Med200397Suppl CS81S8912647946
- JemalAWardEHaoYThunMTrends in the leading causes of death in the United States, 1970–2002JAMA2005294101255125916160134
- BarnesPJKleinertSCOPD – a neglected diseaseLancet2004364943456456515313342
- Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2011 [homepage on the Internet] Available from: http://www.goldcopd.org/Accessed August 20, 2013
- JacksonHHubbardRDetecting chronic obstructive pulmonary disease using peak flow rate: cross sectional surveyBMJ2003327741665365414500437
- WaltersJAWaltersEHNelsonMFactors associated with misdiagnosis of COPD in primary carePrim Care Respir J201120439640221687918
- AverameGBonaviaMFerriP“Alliance Project” Study GroupOffice spirometry can improve the diagnosis of obstructive airway disease in primary care settingRespir Med2009103686687219200705
- BuffelsJDegryseJLiistroGDecramerMDifferential diagnosis in a primary care population with presumed airway obstruction: a real-life studyRespiration2012841445422094827
- TinkelmanDGPriceDBNordykeRJHalbertRJMisdiagnosis of COPD and asthma in primary care patients 40 years of age and overJ Asthma2006431758016448970
- MillerMRHankinsonJBrusascoVATS/ERS Task Force. Standardisation of spirometryEur Respir J200526231933816055882
- PellegrinoRViegiGBrusascoVInterpretative strategies for lung function testsEur Respir J200526594896816264058
- National Collaborating Centre for Chronic ConditionsChronic obstructive pulmonary disease. National clinical guideline on management of chronic obstructive pulmonary disease in adults in primary and secondary careThorax200459Suppl 11232
- SchermerTRJacobsJEChavannesNHValidity of spirometric testing in a general practice population of patients with chronic obstructive pulmonary disease (COPD)Thorax2003581086186614514938
- WenFQHeB[Interpretation of Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease (GOLD) (revised 2011).]Zhonghua Yi Xue Za Zhi20129214939940 Chinese22781562
- KaminskyDAMarcyTWBachandMIrvinCGKnowledge and use of office spirometry for the detection of chronic obstructive pulmonary disease by primary care physiciansRespir Care200550121639164816318645
- GriffithsCFederGWedzichaJFosterGLivingstoneAMarloweGSFeasibility of spirometry and reversibility testing for the identification of patients with chronic obstructive pulmonary disease on asthma registers in general practiceRespir Med1999931290390810653053
- CelliBRThe importance of spirometry in COPD and asthma: effect on approach to managementChest2000117Suppl 215S19S10673468
- National Asthma Education and Prevention ProgramExpert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007J Allergy Clin Immunol2007120Suppl 5S94S13817983880
- GrimesGCManningJLPatelPViaRMMedications for COPD: a review of effectivenessAm Fam Physician20077681141114817990836
- MelbyeHDrivenesEDalbakLGLeinanTHoegh-HenrichsenSOstremAAsthma, chronic obstructive pulmonary disease, or both? Diagnostic labeling and spirometry in primary care patients aged 40 years or moreInt J Chron Obstruct Pulmon Dis2011659760322135492
- JonesRCDickson-SpillmannMMatherMJMarksDShackellBSAccuracy of diagnostic registers and management of chronic obstructive pulmonary disease: the Devon primary care auditRespir Res200896218710575
- SichletidisLChlorosDSpyratosDThe validity of the diagnosis of chronic obstructive pulmonary disease in general practicePrim Care Respir J2007162828817377688
- BoltonCEIonescuAAEdwardsPHFaulknerTAEdwardsSMShaleDJAttaining a correct diagnosis of COPD in general practiceRespir Med200599449350015763457