Abstract
Chronic obstructive pulmonary disease (COPD) is an obstructive and progressive airway disease associated with an important reduction in daily physical activity and psychological problems that contribute to the patient’s disability and poor health-related quality of life (HRQoL). Nowadays, pulmonary rehabilitation (PR) plays an essential role in the management of symptomatic patients with COPD, by breaking the vicious circle of dyspnea–decreased activity–deconditioning–isolation. Indeed the main benefits of comprehensive PR programs for patients with COPD include a decrease in symptoms (dyspnea and fatigue), improvements in exercise tolerance and HRQoL, reduction of health care utilization (particularly bed-days), as well as an increase in physical activity. Several randomized studies and meta-analyses greatly established the benefits of PR, which additionally, is recommended in a number of influential guidelines. This review aimed to highlight the impact of PR on COPD patients, focusing on the clinical usefulness of PR, which provides patients a good support for change.
Introduction
The prevalence of Chronic Obstructive Pulmonary Disease (COPD) is constantly increasing,Citation1 while its incidence is growing in old age.Citation2,Citation3 COPD is also a leading cause of morbidity worldwide, particularly in developing countries.Citation1 Whereas COPD is an obstructive and progressive airway disease, it is also associated with a significant reduction in physical activity, and psychological problems, all of which contribute to the patient’s disability and poor health-related quality of life (HRQoL).Citation3 Recently, emphasis has been placed on questionnaires designed to assess health status and prognosis in COPD.Citation4
For a long time, the treatment of COPD has focused mainly on pharmacological improvement of the airway obstruction. However over the last two decades, growing evidence of systemic manifestations in COPD patients and their negative effects on the functioning of these patients has accelerated the development and use of nonpharmacological treatments, such as pulmonary rehabilitation (PR). PR and pharmacological therapy are not competitive but rather, must work closely together, if they are to result in a more successful outcome. One particular study has shown that a better outcome (exercise tolerance) of PR can be obtained when it is associated with long-acting anticholinergic bronchodilators.Citation5 Moreover, PR has been shown to be the most effective nonpharmacological intervention for improving health status in COPD patients and has become a standard of care for COPD patients.Citation3
Many PR programs have been developed and provided by multidisciplinary teams and typically include components such as patient assessment, exercise training, education, nutritional intervention, and psychosocial support.
The benefit of PR in patients with COPD in improving exercise capacity and HRQoL, and in reducing breathlessness and health care utilization (particularly bed days) has been widely established by randomized studies, summarized in reviews, and by meta-analyses.Citation6–Citation10 PR is now recommended in several influential guidelines.Citation3,Citation11 Unfortunately the practical use of rehabilitation in COPD is virtually nonexistent or under-resourced in most countries. Misunderstanding on the usefulness of a PR program, in addition to the high cost has hindered the widespread distribution of comprehensive PR centers.
This review aimed to present the use of PR in COPD and to highlight the impact of PR on patients with COPD, focusing on the clinical usefulness of PR, which provides patients a favorable environment for optimizing therapy. We also hoped to stimulate or persuade pulmonary physicians to use PR more often.
COPD: a systemic disease with effort limitation
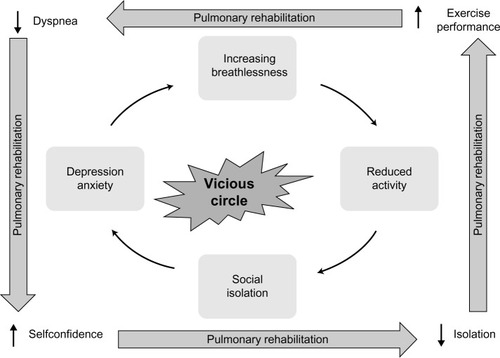
For a long time, COPD was considered to be a respiratory disease, mainly caused by tobacco smoking and leading to progressive dyspnea. However, additionally, COPD produces inactivity, which promotes further loss of exercise capacity (deconditioning) through the loss of muscle mass, creating a “vicious” circle (). Indeed, COPD has substantial manifestations beyond the lungs − the so-called systemic effects, such as unintentional weight loss and skeletal muscle dysfunction. The chronic systemic inflammation that is linked to COPD may also initiate or exacerbate comorbid diseases, such as cardiovascular disease, osteoporosis, anemia, type 2 diabetes, lung cancer, and depressionCitation3,Citation12,Citation13 and is one of the key mechanisms underlying these extrapulmonary effects.Citation12–Citation14 Consequently, COPD patients are disabled by the systemic manifestations of the disease, the most significant systemic dysfunction in COPD patients being the peripheral muscle dysfunction resulting from both physical inactivity and systemic inflammation,Citation15,Citation16 to which we can add hypoxemia, undernutrition, oxidative stress, and systemic corticosteroid therapy.Citation16 This peripheral muscle dysfunction is related to diverse pathophysiological changes in the skeletal muscle, namely reduced oxidative capacity with early lactic acidemia and oxidative stress,Citation17–Citation19 decrease in the volume of muscular fibers,Citation20 fiber type redistribution (shift from type 1 to type 2 fibers),Citation20–Citation22 and altered capillarization of these fibers.Citation22 These alterations lead to higher concentrations of lactate for a given work, which stimulate ventilation, provoking dynamic hyperinflation and increasing ventilatory burden. Moreover, they induce an increasing susceptibility to muscular fatigue and a too early termination of exercise. The limitation of activity also promotes a sedentary lifestyle and the social isolation of COPD patients, with an increased risk of depression and anxiety, leading to further inactivity due to fear of breathlessness and consecutively further physical deconditioning. Exacerbations of COPD also promote the reduction of exercise performance, dyspnea, and the loss of HRQoL, accelerating the path of this vicious circle.Citation23
In summary, inactivity leads to deconditioning, mainly caused by breathlessness. This breathlessness leads to an increased fear of exertion and an avoidance of physical and social activities, thrusting the patient into a vicious circle leading to further isolation and depression, accompanied by a reduced HRQoL ().
What is pulmonary rehabilitation?
The updated statement by the American Thoracic Society and the European Respiratory Society (ATS/ERS) Task Force on PR gives the following definition of PR:
Pulmonary rehabilitation is a comprehensive intervention based on a thorough patient assessment followed by patient-tailored therapies, which include, but are not limited to, exercise training, education and behavior change, designed to improve the physical and emotional condition of people with chronic respiratory disease and to promote the long-term adherence of health-enhancing behaviors.Citation24
This definition emphasizes that PR is a well-proven structured and multidisciplinary treatment approach including patient assessment, physical training and peripheral muscle strengthening, occupational therapy, education of the patient, smoking cessation intervention, nutritional intervention, and psychosocial support. PR thus establishes a personalized and global treatment for the symptomatic COPD patient. A PR program is not a stand-alone therapy, but rather, should be integrated into a management program in which the general practitioner as well as the patient’s pulmonary specialist take an active part. By using a holistic approach centered on the patient, PR aims to reverse the systemic manifestations of COPD as well as to relieve the fears and anxiety associated with social and exterior activities, thereby leading to a change in the patient’s day-to-day life. Finally, PR aims to break the aforementioned vicious circle in COPD ().
Who should attend a pulmonary rehabilitation program?
PR offers benefits for all patients suffering from a chronic respiratory disease of whatever origin, who have a decrease of pulmonary function, who are symptomatic, and who have intolerance to effort, in spite of an optimal pharmacological treatment.Citation6,Citation8,Citation9 Even candidates for lung volume reduction surgery for severe emphysema or for lung transplantation are good candidates for PR.Citation25 A program of PR may be proposed in stable COPD as well as immediately after COPD exacerbation.Citation26 In agreement with the joint statement of the ATS/ERS of 2006, all patients suffering from the systemic consequences of COPD are good candidates for PR.Citation8 According to the new Global initiative for Obstructive Lung Disease (GOLD) guidelines, COPD patients (groups B−D) will benefit from a PR program.Citation3 However, a recent evidence-based practice guideline from the American College of Physicians supports the use of PR for symptomatic severe COPD patients (FEV1 <50% of predicted: strong recommendation) and for symptomatic or exercise-limited patients with FEV1 ≥50% of predicted (weak recommendation).Citation11
Usually COPD patients are referred to a PR center by their chest physician or directly by their general practitioner, after which the pneumologist, center manager, or one of the team assesses the appropriateness of the indication for a multidisciplinary PR program. If a home-based PR program is considered, a close coordination between the different care providers is essential, if possible, in a care network. However, the reimbursement of the PR costs in the various modalities depends on the financial situation of the patient and their social security, as well as the rules of each country’s particular health care system.
Contraindications and barriers to pulmonary rehabilitation
The main contraindications are lack of motivation and nonadherence, psychiatric illness or dementia, uncontrolled cardiovascular diseases, inability to do exercise (for orthopedic or other reasons), and unstable diseases (eg, hepatic, diabetes).Citation6 In some countries, active cigarette smoking is considered as a relative contraindication. While it has been proven that current smokers obtain the same benefits from PR, they will nevertheless be encouraged to undergo a smoking cessation program. However, the adherence to PR by smokers generally remains less than that of ex-smokers.Citation27–Citation29
Nevertheless, we believe that excluding smoking patients would deprive them of a potential opportunity to quit smoking.Citation30 AgeCitation31 as well as the degree of the bronchial obstructionCitation32,Citation33 do not constitute contraindications to PR; neither does continuous or intermittent noninvasive ventilation. Exertional severe hypoxemia must be corrected beforehand, by oxygen therapy.
Few studies have established the predictive factors of nonadherence to PR. However, besides active smoking, there is social isolation,Citation29 depression, and lower quadriceps strength.Citation27 Furthermore, a retrospective analysis has shown that COPD patients are less likely to complete a PR program if they are current smokers, attend a long-lasting program, have suffered frequent exacerbations requiring hospital admission in the preceding year, have a long journey time to reach the center, and higher Medical Research Council (MRC) dyspnea score.Citation34 In a more recent review, Keating et al identified travel and transport, a lack of perceived benefit of PR, being current smoker, illness, and depression as barriers to completion of a PR program.Citation28 For such reasons, the dropout rate from PR reported in most of these studies was within the order of 20%−30%. The aforementioned reasons are often intercurrent illnesses (severe exacerbations of COPD and COPD-related and non-COPD-related hospitalizations) and logistical problems (such as transport facilities, cost for the patient, and distance from the center).
Evidence of the effectiveness of pulmonary rehabilitation in COPD
Based on various published RCTs and on meta-analyses, numerous evidence-based reviews have evaluated the effect of PR programs on symptomatic COPD patients. These have demonstrated the effectiveness and utility of PR. The main outcomes, including exercise performance, dyspnea, HRQoL, psychosocial benefits, cost effectiveness, reduced health care utilization, and survival ( and ) have been reported. Some of these reviews and meta-analyses are summarized in and along with some comments.Citation3,Citation7,Citation9,Citation26,Citation35–Citation39 The ben efits on many laboratory and clinical parameters associated with PR are produced without demonstrable improvements in pulmonary function. This apparent contradiction could be explained by the fact that we know that PR acts mainly on the systemic effects of the disease.
Table 1 Main outcomes of pulmonary rehabilitation in COPD patients
Table 2 Main outcomes of pulmonary rehabilitation in COPD patients
Among the multiple benefits of PR, we would like to examine the reduction of exacerbations, followed by the cost effectiveness. Indeed, a reduction in the use of the health care system is an important goal of PR because COPD patients are heavy users of health care resources. A large study examining health care utilization following a 6-week PR program found that, in comparison with a control group who received “usual care,” patients in the rehabilitation group had the same number of hospital admissions but spent less time in hospital (10 versus 21 days) during the 1-year follow up.Citation40 A reduction of health care utilization with PR was also confirmed in another randomized, controlled trial (RCT) study with a follow up of 2 yearsCitation41 and in nonrandomized clinical studies.Citation42–Citation44 Moreover, in two meta-analyses involving respectively 230 and 432 COPD patients, PR following the exacerbation of COPD significantly reduced hospital admission and mortality.Citation26,Citation36 Finally, Griffiths et al reported that PR was found to be cost effective and resulted in financial benefits.Citation45 A more recent Canadian study suggested that PR is cost effective for patients with relatively high utilization of emergency and hospital-based services.Citation46
Components in pulmonary rehabilitation
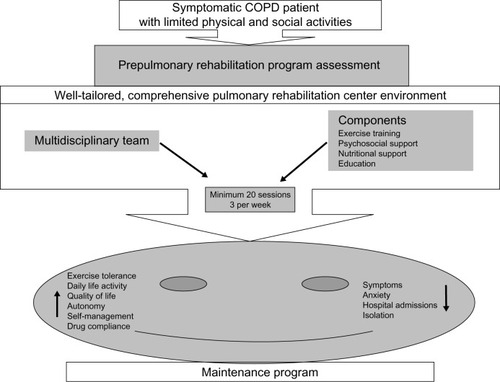
PR is a comprehensive, multidisciplinary (), multicomponent, patient-centered intervention, consisting of a prerehabilitation assessment program, exercise and muscle training, self-management education, occupational therapy, psychosocial support, and nutritional intervention. Although most PR programs include these aspects, they may vary considerably from one center to another. Most programs involve 2 to 3 hours of education and exercise, three times weekly for at least 6 weeks. summarizes the steps and benefits of PR.
Figure 2 Multidisciplinary team involved in comprehensive pulmonary rehabilitation centered on the COPD patients.
Abbreviation: COPD, chronic obstructive pulmonary disease.
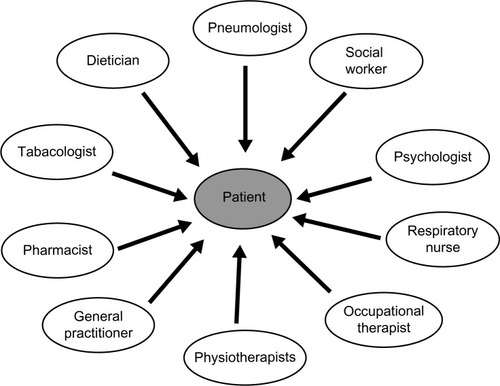
Figure 3 Summary of the steps and benefits of pulmonary rehabilitation.
Setting and length for pulmonary rehabilitation programs
The structure and the setting of PR vary widely around the world. PR programs can be conducted with benefits in inpatient, hospital, or community-based outpatient or home-based settings.Citation8,Citation47,Citation48 However, most of the evidence for PR has been obtained from studies performed in a hospital-based outpatient setting.Citation6,Citation8,Citation9 In the case of home-based PR, patients do not benefit from the group dynamics or from the same safety as can be found in the other modalities. Home-based PR remains limited to exercise training, without the numerous benefits gained from a multidisciplinary team, and in addition, can be inferior in efficacy to the out-and inpatient supervised programs.Citation8,Citation49 Nevertheless, a recent study by Maltais et al boosted the interest in home-based PR as an alternative equivalent to hospital outpatient PR.Citation48 Finally, the choice setting remains a question of patient motivation, disease severity and complex morbidities, local program availability, and available resources.
The minimum duration of an effective ambulatory PR program is currently unknown,Citation9 but the GOLD guidelines suggest 6 weeks.Citation3 It appears that a minimum of 20 sessions is needed to achieve physiological benefits,Citation8,Citation9 although longer programs are associated with better results.Citation3,Citation50,Citation51 A recent review concluded that prolonged PR programs tend to have more favorable effects on HRQoL, but the results for exercise capacity are less clear.Citation52 Furthermore the limited number of RCTs comparing different lengths of PR prevents a more definitive conclusion on the optimal duration of PR.Citation52 Conversely, an interesting meta-analysis concluded that patients with mild or moderate COPD benefit from short-and long-term rehabilitation, whereas patients with severe COPD may benefit from rehabilitation programs of at least 6 months.Citation53 On the other hand, inpatient PR programs have a shorter duration and may result in physical performance improvement within 2 weeksCitation47 but are generally more expensive.Citation54 Inpatient PR can be particularly reserved for more disabled patients with severe comorbidities, patients with limited transportation to the outpatient setting, or patients residing in areas where outpatient PR program facilities are limited.Citation8
Prerehabilitation assessment program
Assessment of the patient, prior to initiation of PR but also, during and at the end of PR, is an essential element in the practice of PR. It allows the patient to have an individually tailored treatment based on their needs and problems and for adaptation of the program of PR according to the progress obtained.Citation8,Citation10 This assessment is carried out under the direction of the pulmonary physician specialized in rehabilitation. The pulmonary physician leads and coordinates the multidisciplinary team and is responsible for the medical treatment and rehabilitation program and for investigating comorbidities that could contraindicate or interact with PR (as described previously).Citation6,Citation9,Citation55 The possible assessments include past medical history (including comorbidities), physical examination, cycling cardiopulmonary exercises (incremental workload), the 6-minute walk test, the shuttle walking test, pulmonary function tests, maximal expiratory and inspiratory pressure evaluations, measurement of peripheral muscle forces, disease-specific questionnaires, and nutritional and psychological evaluations.
Exercise training
Continuous and interval training as well as strength training may be regarded as the major exercise components of PR.Citation56
Continuous and interval training
Endurance training is the most common exercise modality in COPD patients. The main objective is to improve aerobic exercise capacity as aerobic activities are part of many tasks.Citation56 The exercise training is guided by the following three parameters: intensity, frequency, and duration.Citation9
Lower extremity exercise training at a higher exercise intensity produces greater physiologic benefits than does training at a lower intensity, in patients with COPD.Citation9 Nonetheless, both low-intensity and high-intensity exercise training produce clinical benefits for patients with COPD.Citation9 Indeed, muscular functional disorders are reversible with moderate-to high-intensity rehabilitation exercise,Citation8,Citation57,Citation58 with the same magnitude changes across GOLD stages II to IV.Citation59 Low-intensity training results in improvements in symptoms, HRQoL, and some aspects of performance of the activities associated with daily living;Citation8 moreover, the long-term adherence seems to be better with low-intensity training. However, training programs should attempt to achieve maximal physiologic effects.Citation8 So high-intensity training is proposed in PR centers. High-intensity training targets have been defined to be at least 60% to 80% of the peak work rate achieved in an incremental maximal exercise test.Citation9 This intensity seems sufficient to elicit some physiologic training effects.Citation8 The total effective training time should ideally be over 30 minutes.Citation8 Endurance exercise of the leg muscles is the main focus, with walking, stationary cycling, and treadmill exercise being commonly performed.Citation55 In clinical practice, symptom scores can be used to adjust the training load (eg, a Borg score of 4 to 6 for dyspnea).Citation8,Citation60
Most programs involve three sessions per week, of which a minimum of two sessions should be supervised,Citation8 with a duration of at least 6–8 weeks.Citation3,Citation61
For severely breathless patients, it is not possible to achieve the above training targets. In such cases, an interval training regime may be preferred.Citation55,Citation62 Here, the continuous exercise session is substituted by a succession of shorter high-intensity exercise periods alternated with low-to moderate-intensity exercise recovery periods.Citation62 This form of training may be more comfortable for patients with more severe dynamic hyperinflation,Citation10 and adherence to the treatment may be better.Citation63 Patients with severe COPD may also increase the total exercise duration with lower metabolic and ventilatory stress.Citation56
During the training sessions, oxygen saturation, heart rate, and blood pressure are measured. Supplementary oxygen is given in order to maintain an oxygen saturation of above 90%.Citation6,Citation9,Citation31 All the measured parameters are recorded in the medical file. As the rehabilitation program proceeds, therapists should be encouraged to adjust the training intensity. Retesting may provide physiological evidence that a training response has occurred and may be useful in the adjustment of intensity levels during the program.Citation64
Strength training
Strength training (resistance exercises) would be particularly indicated for patients with significant muscle atrophy and marked dyspnea on minimal exertion.Citation8 For each patient, the physiotherapist chooses the optimal resistance, frequency of exercise, speed, and mode of training and also, the implementation during the PR program. The addition of the strength training component increases muscle mass and strength.Citation9 The combination of endurance and strength training generally has multiple beneficial effects and is well tolerated.
Upper limb training
PR programs have traditionally focused on the lower extremities, but many patients report dyspnea during daily activities that involve use of their arms, such as dressing, washing, and carrying groceries. Accordingly, upper limb exercises should be incorporated into the training program,Citation8 using an arm cycle ergometer, free weights, or elastic bands. All modes of arm exercise have been shown to increase arm endurance capacity by a clinically significant level compared with no arm training.Citation65,Citation66
Adjunct to the exercise training
Neuromuscular electrical stimulation
Neuromuscular electrical stimulation (NMES) may be an adjunctive therapy for patients with severe chronic respiratory diseases who are bedbound or suffering from extreme skeletal muscle weakness.Citation9 NMES can be conducted at home and is safe and relatively inexpensive.Citation10 NMES was shown to enhance walking performance in patients with severe COPD.Citation67
Respiratory muscle training
Inspiratory muscle training (IMT) is not recommended as a routine component of a PR programCitation9 but should be considered in COPD patients with ventilatory muscle weakness.Citation8 Normocapnic hyperpnea resistive training and threshold loading have been described as training modalities.Citation8 The use of a threshold loading device can be recommended for training the inspiratory muscles.Citation37,Citation68 Moreover, a meta-analysis of 25 studies that assessed the efficacy of IMT in patients with stable COPD found significant increases in inspiratory muscle strength, exercise capacity, and one measure of quality of life, and a significant decrease in dyspnea.Citation69
Alternative treatment
Beyond the classical modes of training, such as walking, cycling, stepping, and arm training, there have been a few recently published papers on the effects of alternative exercise training modalities, in people with COPD. Among these, we have found two alternative modes − water-based rehabilitation (in patients with physical comorbidities, including musculoskeletal, peripheral vascular disease, and neurological conditions or obesity)Citation70 and Tai Chi − that seem to be well tolerated and enjoyed by patients.Citation71,Citation72
Education
Patient education, incorporating self-management training, remains an important component of any comprehensive PR program, despite the difficulties in measuring its direct contribution to overall outcome.Citation8,Citation9 The content of the education program varies depending on local resources, but the topics commonly covered are aspects of the disease, physiotherapy skills, nutrition interventions, energy conservation, and psychosocial interventions.
Disease education
All patients should receive disease education to improve their compliance with medication regimens,Citation10 oxygen therapy, smoking cessation, nutritional interventions, exercise, and health preservation, all of which contribute to the overall autonomy of the patient. Patient education includes relevant topics associated with COPD (eg, anatomy, pathophysiology, nutritional advice, disease education, breathing techniques and pharmacology, oxygen therapy, smoking cessation, inhalation techniques, symptom management, chest clearance techniques, energy conservation, daily exercise, psychological interventions, anxiety management, relaxation, goal setting, travelling with COPD, sexuality issues, prevention and early recognition/management of COPD exacerbation, end of life issues, etc). Patient education aims to equip the patient with the knowledge and skills they need to manage their disease and to change their lifestyle, which is the ultimate aim of PR. All the multidisciplinary team members participate in educational programs.
Physiotherapy skills
Chest physiotherapy represents a nonessential component of PR but proves its usefulness in patients with a marked bronchial hypersecretion.Citation55 Relaxation exercises, flexibility and stretching exercises, breathing techniques (eg, pursed lip and diaphragmatic breathing) are often coupled with an exercise training session.Citation35,Citation73 These are administered for a brief period (5–10 minutes) and are recommended to maintain muscle length and to prevent injury and soreness.
Energy conservation
Occupational therapists contribute to the evaluation of a patient’s autonomy and may recommend technical support and energy conservation techniques, depending on the type of disability. They also educate the oxygen-dependent patient.
Nutritional intervention
In COPD, nutritional depletion is common and has a negative impact on respiratory as well as on skeletal muscle functions, and contributes to the morbidity and mortality of COPD patients.Citation74 Achievement of optimal nutritional status should help to maximize the patient’s state of health, respiratory muscle function, and overall sense of wellbeing.Citation55 The dietician’s role is to establish a dietary history, evaluate the body mass index (BMI), measure the body fat percentage (eg, by impedancemetry), and ensure dietary follow up. Underweight patients may require nutritional advice (caloric supplements may be required) prior to commencing a PR program to ensure that the extra physical activity does not lead to further weight loss. Overweight patients may also need nutritional advice regarding weight loss, but the challenge here, is to not lose fat-free mass.Citation10 Current scientific evidence does not support the routine use of anabolic agents in PR for patients with COPD.Citation9
Psychosocial support
Anxiety and depression are important comorbidities of COPD,Citation3,Citation12,Citation13,Citation75 and a significant proportion of COPD patients referred to PR centers suffer from these psychiatric disorders.Citation13,Citation75 The psychologist can be helped to evaluate for anxiety−depression disorders by means of tools such as the Hospital Anxiety and Depression Scale (HADS), as symptoms of anxiety in COPD have been demonstrated to have a negative impact on quality of life (QoL).Citation76
QoL can be assessed with a disease-specific questionnaire, such as the Chronic Respiratory Disease Questionnaire (CRQ)Citation77 or the St George’s Respiratory Questionnaire (SGRQ).Citation78,Citation79 The psychosocial interventions for patients include disability evaluation, vocational counseling, and continued education of patient and family. In addition, psychological support can facilitate the adjustment process by encouraging adaptive thoughts and behavior − coping strategies that help patients to reduce their negative emotions, which in turn, may improve compliance with PR. Psychological support helps in overcoming addictions, especially tobacco smoking and, along with medical treatment for smoking cessation, is an important intervention in PR programs.Citation10 In some instances, the social worker provides assistance to the patient in securing financial support.
Maintenance program
The benefits of a PR program tend to diminish over the months following its discontinuation. PR programs are usually not associated with sustained benefits beyond 12 months.Citation40,Citation43,Citation80,Citation81 However, programs lasting for at least 6 months have been more successful in maintaining outcomes, even in the absence of structured maintenance programs.Citation41,Citation82 Maintenance of the benefits of PR – such as physical activity and lifestyle changes – is an important challenge for those who have undergone a comprehensive PR program.
Many centers currently offer maintenance programs in the hope of consolidating and prolonging the benefits of a successful rehabilitation program. However, the optimal strategy to meet this aim has not yet been described. Among the available options, we find telephone contacts and monthly supervised reinforcement sessions,Citation83,Citation84 home exercise training (with or without a weekly supervised outpatient session),Citation85 and recurrent PR programs.Citation86,Citation87
A systematic review concluded that after 8 weeks of supervised physical exercise training, maintenance programs consisting of weekly telephone calls and monthly reinforcement sessions for 1 year were unsuccessful in altering behavior and maintaining the treatment effects.Citation35 Moreover a recent meta-analysis has suggested that post-PR exercise programs for COPD patients are superior to traditional care in maintaining exercise capacity in the medium term (6 months) but not in the long term (≥1 year) and have no sustained effect at all with regard to the HRQoL.Citation88 These results should be interpreted with caution, given the heterogeneity in interventions, follow-up intervals, and outcomes measures.
The best and the most effective maintenance program currently remains to be found. Beyond post-PR exercise programs, the PR center staff, as well as family members and general practitioners, should encourage and motivate the patient to follow the maintenance program and continue with a more active lifestyle, in order to retain the gains. This advice is supported by the 12-month follow-up data taken from a cohort of COPD patients who had completed a 10-week comprehensive PR program and who were invited to follow a structured home program at the end of the PR program.Citation89 At the 1-year follow-up evaluation, only the patients who had continued with the “prescribed” exercise routine had maintained the gains achieved in physical endurance, and psychological and cognitive functioning during the initial intervention.
Pulmonary rehabilitation and effect on physical activity
Patients with COPD are typically less active in daily life than are healthy older adults.Citation90 In addition, inactivity is associated with poor functional status and higher risk of hospital admissions and mortality.Citation91 It appears obvious that COPD patients would be more physically and socially active after PR. However, there is currently no strong evidence that patients translate the benefits obtained from PR into a more active lifestyle in real life.
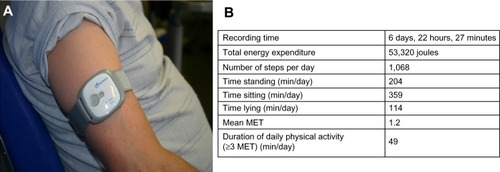
Cindy et alCitation92 recently published the first meta-analysis evaluating the effect of exercise training on measures of physical activity. This meta-analysis pointed out that supervised exercise training confers a significant but small effect on physical activity. The principal limitation of the meta-analysis was that the majority of the included studies did not use the same method to measure physical activity; moreover, it is well known that questionnaires and pedometers are an insufficiently sensitive means of detecting changes in physical activity in this particular clinical (slow-walking) population.Citation90,Citation93,Citation94 When the authors considered only those studies that utilized a multisensory accelerometer to measure physical activity, they obtained more significant improvements in physical activity.Citation92 Accelerometers or activity monitors are small devices carried on the arm, leg, or waist that measure energy expenditure, movement pattern, and body position over a period of time (24 hours to 7 days) and provide objective measurements of daily life activity (). Two parameters appear to be crucial to enhancing physical activity in COPD patients after PR: the frequency of supervised exercise training and the duration of the program. Indeed, in the meta-analysis by Cindy et al,Citation92 the studies that proposed an exercise training regimen of three times per week showed a significant increase in physical activity, in contrast with those that offered exercise only two times a week. Moreover, in a study measuring physical activity with an accelerometer, Pitta et alCitation93 showed that a 6-month, supervised exercise training program was required to obtain a significant effect on physical activity, while three months was shown to be insufficient. This is consistent with the recent concept that 6 months are needed for most people to change behavior.Citation95 The recording of spontaneous daily physical activity provides a new dimension in patient assessment that goes beyond any measurement of physiological capacity. Daily activity and the completion of domestic tasks are more important for the patient than an improvement in the 6-minute walk test, total CRQ score, or maximal load achieved during ergospirometry. Thus clinicians should take into account what people actually do (eg, walking, climbing stairs, dressing, etc), rather than what they are capable of doing since it is the natural level of physical activity that seems to best determine the prognostic benefit.Citation96
Figure 4 Use of a multisensory accelerometer.
Abbreviations: MET, metabolic equivalent; COPD, chronic obstructive pulmonary disease; GOLD, Global initiative for Obstructive Lung Disease; min/day, minutes per day.
As mentioned above, a study showed that a better outcome of PR can be obtained by its association with long-acting anticholinergic bronchodilators.Citation5 This treatment appears to amplify the effectiveness of PR, as seen by greater improvements (beyond that obtained with PR alone) in patient self-reported participation in physical activities outside of the PR program, during the 8 weeks of PR and the 12 weeks following.Citation97
Finally, new studies using accelerometers are needed to validate their useCitation98 and to go further in this crucial domain linking PR and physical activity, since we know that physical activity levels determine the survival in COPD patients.
Conclusion
Tailored pulmonary rehabilitation programs should be considered for COPD patients of all stages, who have respiratory symptoms and/or who have intolerance to physical effort despite optimal pharmacological treatment.
PR has certainly been demonstrated to provide beneficial effects on dyspnea, improvement in muscle strength and endurance, improvement of psychological status, reduction of hospital admissions, and improvement of HRQoL in COPD patients, with a gradual increase in daily physical activity and autonomy.
Successful PR therefore requires behavioral changes. To achieve this, patients’ skill and adherence may be facilitated if they are enrolled in longer, comprehensive programs comprising interactions with a multidisciplinary team offering support, council, encouragement, and coaching. These changes rest on the following: exercise training; psychosocial support; nutritional intervention; self-management; and education, as well as pacing and energy conservation strategies, all of which are intended for motivated COPD patients. Therefore, PR embodies a very important and safe therapeutic option that aims to reverse the systemic manifestations of COPD and which, along with pharmacological therapy, can be used to obtain optimal patient management, leading to a favorable change in the daily life of our COPD patients. Accordingly, with the increasing burden of COPD patients in the world, there is an urgent need for advocacy with the concerned authorities, for a more widespread reimbursement of PR programs worldwide.
Acknowledgments
We would like to thank Mark Denham for his assistance in reviewing the English for this article.
Disclosure
The authors report no conflicts of interest in this work.
References
- MurrayCJLopezADAlternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease StudyLancet19973499064149815049167458
- LopezADShibuyaKRaoCChronic obstructive pulmonary disease: current burden and future projectionsEur Respir J200627239741216452599
- VestboJHurdSSAgustíAGGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med2013187434736522878278
- LouisRCorhayJLHealth status instrument vs prognostic instrument for assessing chronic obstructive pulmonary disease in clinical practiceInt J Clin Pract201064111465146620846191
- CasaburiRKukafkaDCooperCBWitekTJJrKestenSImprovement in exercise tolerance with the combination of tiotropium and pulmonary rehabilitation in patients with COPDChest2005127380981715764761
- HillNSPulmonary rehabilitationProc Am Thorac Soc200631667416493153
- LacasseYGoldsteinRLassersonTJMartinSPulmonary rehabilitation for chronic obstructive pulmonary disease [review]Cochrane Database Syst Rev20064CD00379317054186
- NiciLDonnerCWoutersEATS/ERS Pulmonary Rehabilitation Writing CommitteeAmerican Thoracic Society/European Respiratory Society statement on pulmonary rehabilitationAm J Respir Crit Care Med2006173121390141316760357
- RiesALBauldoffGSCarlinBWPulmonary Rehabilitation: Joint ACCP/AACVPR Evidence-Based Clinical Practice GuidelinesChest2007131Suppl 54S42S17494825
- TroostersTCasaburiRGosselinkRDecramerMPulmonary rehabilitation in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med20051721193815778487
- QaseemAWiltTJWeinbergerSEAmerican College of PhysiciansAmerican College of Chest PhysiciansAmerican Thoracic SocietyEuropean Respiratory SocietyDiagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory SocietyAnn Intern Med2011155317919121810710
- AgustiASorianoJBCOPD as a systemic diseaseCOPD20085213313818415812
- BarnesPJCelliBRSystemic manifestations and comorbidities of COPDEur Respir J20093351165118519407051
- FabbriLMRabeKFFrom COPD to chronic systemic inflammatory syndrome?Lancet2007370958979779917765529
- American Thoracic SocietyEuropean Respiratory SocietySkeletal muscle dysfunction in chronic obstructive pulmonary disease. A statement of the American Thoracic Society and European Respiratory SocietyAm J Respir Crit Care Med19991594 Pt 2S1S4010194189
- WüstRCDegensHFactors contributing to muscle wasting and dysfunction in COPD patientsInt J Chron Obstruct Pulmon Dis20072328930018229567
- BarreiroEGeaJCorominasJMHussainSNNitric oxide syntheses and protein oxidation in the quadriceps femoris of patients with chronic obstructive pulmonary diseaseAm J Respir Cell Mol Biol200329677177812816735
- GoskerHRHesselinkMKDuimelHWardKAScholsAMReduced mitochondrial density in the vastus lateralis muscle of patients with COPDEur Respir J2007301737917428811
- MaltaisFSimardAASimardCJobinJDesgagnésPLeBlancPOxidative capacity of the skeletal muscle and lactic acid kinetics during exercise in normal subjects and in patients with COPDAm J Respir Crit Care Med199615312882938542131
- WhittomFJobinJSimardPMHistochemical and morphological characteristics of the vastus lateralis muscle in patients with chronic obstructive pulmonary diseaseMed Sci Sports Exerc19983010146714749789845
- GoskerHRZeegersMPWoutersEFScholsAMMuscle fibre type shifting in the vastus lateralis of patients with COPD is associated with disease severity: a systematic review and meta-analysisThorax2007621194494917526675
- JobinJMaltaisFDoyonJFChronic obstructive pulmonary disease: capillarity and fiber-type characteristics of skeletal muscleJ Cardiopulm Rehabil19981864324379857275
- AnzuetoAImpact of exacerbations on COPDEur Respir Rev20101911611311820956179
- SpruitMASinghSJGarveyCAn official american thoracic society/european respiratory society statement: key concepts and advances in pulmonary rehabilitationAm J Respir Crit Care Med20131888e13e6424127811
- RiesALMakeBJLeeSMNational Emphysema Treatment Trial Research GroupThe effects of pulmonary rehabilitation in the national emphysema treatment trialChest200512863799380916354848
- PuhanMAScharplatzMTroostersTSteurerJRespiratory rehabilitation after acute exacerbation of COPD may reduce risk for readmission and mortality – a systematic reviewRespir Res200565415943867
- GarrodRMarshallJBarleyEJonesPWPredictors of success and failure in pulmonary rehabilitationEur Respir J200627478879416481381
- KeatingALeeAHollandAEWhat prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic reviewChron Respir Dis201182899921596892
- YoungPDewseMFergussonWKolbeJRespiratory rehabilitation in chronic obstructive pulmonary disease: predictors of nonadherenceEur Respir J199913485585910362053
- PaoneGSerpilliMGirardiEThe combination of a smoking cessation programme with rehabilitation increases stop-smoking rateJ Rehabil Med200840867267719020702
- CorhayJLNguyenDDuysinxBShould we exclude elderly patients with chronic obstructive pulmonary disease from a long-time ambulatory pulmonary rehabilitation programme?J Rehabil Med201244546647222549658
- NgaageDLHasneyKCowenMEThe functional impact of an individualized, graded, outpatient pulmonary rehabilitation in end-stage chronic obstructive pulmonary diseaseHeart Lung200433638138915597292
- NiedermanMSClementePHFeinAMBenefits of a multidisciplinary pulmonary rehabilitation program. Improvements are independent of lung functionChest19919947988042009777
- SabitRGriffithsTLWatkinsAJPredictors of poor attendance at an outpatient pulmonary rehabilitation programmeRespir Med2008102681982418337077
- LangerDHendriksEBurtinCA clinical practice guideline for physiotherapists treating patients with chronic obstructive pulmonary disease based on a systematic review of available evidenceClin Rehabil200923544546219389745
- PuhanMAGimeno-SantosEScharplatzMTroostersTWaltersEHSteurerJPulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease [review]Cochrane Database Syst Rev201110CD00530521975749
- QaseemASnowVShekellePClinical Efficacy Assessment Subcommittee of the American College of PhysiciansDiagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline from the American College of PhysiciansAnn Intern Med2007147963363817975186
- SinDDMcAlisterFAManSFAnthonisenNRContemporary management of chronic obstructive pulmonary disease: scientific reviewJAMA2003290172301231214600189
- WiltTJNiewoehnerDMacDonaldRKaneRLManagement of stable chronic obstructive pulmonary disease: a systematic review for a clinical practice guidelineAnn Intern Med2007147963965317975187
- GriffithsTLBurrMLCampbellIAResults at 1 year of outpatient multidisciplinary pulmonary rehabilitation: a randomised controlled trialLancet2000355920136236810665556
- GuellRCasanPBeldaJLong-term effects of outpatient rehabilitation of COPD: A randomized trialChest2000117497698310767227
- California Pulmonary Rehabilitation Collaborative GroupEffects of pulmonary rehabilitation on dyspnea, quality of life, and healthcare costs in CaliforniaJ Cardiopulm Rehabil2004241526214758104
- FoglioKBianchiLBrulettiGBattistaLPaganiMAmbrosinoNLong-term effectiveness of pulmonary rehabilitation in patients with chronic airway obstructionEur Respir J199913112513210836336
- HuiKPHewittABA simple pulmonary rehabilitation program improves health outcomes and reduces hospital utilization in patients with COPDChest20031241949712853508
- GriffithsTLPhillipsCJDaviesSBurrMLCampbellIACost effectiveness of an outpatient multidisciplinary pulmonary rehabilitation programmeThorax2001561077978411562517
- GolmohammadiKJacobsPSinDDEconomic evaluation of a community-based pulmonary rehabilitation program for chronic obstructive pulmonary diseaseLung2004182318719615526757
- CliniEFoglioKBianchiLPortaRVitaccaMAmbrosinoNIn-hospital short-term training program for patients with chronic airway obstructionChest200112051500150511713126
- MaltaisFBourbeauJShapiroSChronic Obstructive Pulmonary Disease Axis of Respiratory Health Network, Fonds de recherche en santé du QuébecEffects of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: a randomized trialAnn Intern Med20081491286987819075206
- Puente-MaestuLSánzMLSánzPCubilloJMMayolJCasaburiRComparison of effects of supervised versus self-monitored training programmes in patients with chronic obstructive pulmonary diseaseEur Respir J200015351752510759446
- GreenRHSinghSJWilliamsJMorganMDA randomised controlled trial of four weeks versus seven weeks of pulmonary rehabilitation in chronic obstructive pulmonary diseaseThorax200156214314511209104
- RossiGFloriniFRomagnoliMLength and clinical effectiveness of pulmonary rehabilitation in outpatients with chronic airway obstructionChest2005127110510915653969
- BeauchampMKJanaudis-FerreiraTGoldsteinRSBrooksDOptimal duration of pulmonary rehabilitation for individuals with chronic obstructive pulmonary disease – a systematic reviewChron Respir Dis20118212914021596893
- SalmanGFMosierMCBeasleyBWCalkinsDRRehabilitation for patients with chronic obstructive pulmonary disease: meta-analysis of randomized controlled trialsJ Gen Intern Med200318321322112648254
- GoldsteinRSGortEHGuyattGHFeenyDEconomic analysis of respiratory rehabilitationChest199711223703799266871
- de BlasioFPolverinoMCurrent best practice in pulmonary rehabilitation for chronic obstructive pulmonary diseaseTher Adv Respir Dis20126422123722563010
- GloecklRMarinovBPittaFPractical recommendations for exercise training in patients with COPDEur Respir Rev20132212817818623728873
- MaltaisFLeBlancPJobinJIntensity of training and physiologic adaptation in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med199715525555619032194
- SalaERocaJMarradesRMEffects of endurance training on skeletal muscle bioenergetics in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med199915961726173410351910
- VogiatzisITerzisGStratakosGEffect of pulmonary rehabilitation on peripheral muscle fiber remodeling in patients with COPD in GOLD stages II to IVChest2011140374475221493697
- MahlerDAWardJMejia-AlfaroRStability of dyspnea ratings after exercise training in patients with COPDMed Sci Sports Exerc20033571083108712840626
- RingbaekTJBroendumEHemmingsenLRehabilitation of patients with chronic obstructive pulmonary disease. Exercise twice a week is not sufficient!Respir Med200094215015410714421
- BeauchampMKNonoyamaMGoldsteinRSInterval versus continuous training in individuals with chronic obstructive pulmonary disease – a systematic reviewThorax201065215716419996334
- PuhanMABüschingGSchünemannHJVanOortEZauggCFreyMInterval versus continuous high-intensity exercise in chronic obstructive pulmonary disease: a randomized trialAnn Intern Med20061451181682517146066
- LacasseYMartinSLassersonTJGoldsteinRSMeta-analysis of respiratory rehabilitation in chronic obstructive pulmonary disease. A Cochrane systematic reviewEura Medicophys200743447548518084170
- Janaudis-FerreiraTHillKGoldsteinRWadellKBrooksDArm exercise training in patients with chronic obstructive pulmonary disease: a systematic reviewJ Cardiopulm Rehabil Prev200929527728319935139
- McKeoughZJByePTAlisonJAArm exercise training in chronic obstructive pulmonary disease: a randomised controlled trialChron Respir Dis20129315316222452973
- VivodtzevIDebigaréRGagnonPFunctional and muscular effects of neuromuscular electrical stimulation in patients with severe COPD: a randomized clinical trialChest2012141371672522116795
- HillKCecinsNMEastwoodPRJenkinsSCInspiratory muscle training for patients with chronic obstructive pulmonary disease: a practical guide for cliniciansArch Phys Med Rehabil20109191466147020801269
- GeddesELO’BrienKReidWDBrooksDCroweJInspiratory muscle training in adults with chronic obstructive pulmonary disease: an update of a systematic reviewRespir Med2008102121715172918708282
- McNamaraRJMcKeoughZJMcKenzieDKAlisonJAWater-based exercise in COPD with physical comorbidities: a randomised controlled trialEur Respir J20134161284129122997217
- LeungRWMcKeoughZJPetersMJAlisonJAShort-form Sun-style t’ai chi as an exercise training modality in people with COPDEur Respir J20134151051105722878879
- YanJHGuoYZYaoHMPanLEffects of Tai Chi in patients with chronic obstructive pulmonary disease: preliminary evidencePLoS One201384e6180623626732
- JenkinsSHillKCecinsNMState of the art: how to set up a pulmonary rehabilitation programRespirology20101581157117320920127
- FerreiraIBrooksDLacasseYGoldsteinRNutritional intervention in COPD: a systematic overviewChest2001119235336311171709
- Putman-CasdorphHMcCroneSChronic obstructive pulmonary disease, anxiety, and depression: state of the scienceHeart Lung2009381344719150529
- HillKGeistRGoldsteinRSLacasseYAnxiety and depression in end-stage COPDEur Respir J200831366767718310400
- GuyattGHBermanLBTownsendMPugsleySOChambersLWA measure of quality of life for clinical trials in chronic lung diseaseThorax198742107737783321537
- JonesPWQuirkFHBaveystockCMThe St George’s Respiratory QuestionnaireRespir Med199185Suppl BS25S31 discussion 33–37
- JonesPWInterpreting thresholds for a clinically significant change in health status in asthma and COPDEur Respir J200219339840411936514
- BestallJCPaulEAGarrodRGarnhamRJonesRWWedzichaAJLongitudinal trends in exercise capacity and health status after pulmonary rehabilitation in patients with COPDRespir Med200397217318012587969
- RiesALKaplanRMLimbergTMPrewittLMEffects of pulmonary rehabilitation on physiologic and psychosocial outcomes in patients with chronic obstructive pulmonary diseaseAnn Intern Med1995122118238327741366
- TroostersTGosselinkRDecramerMShort-and long-term effects of outpatient rehabilitation in patients with chronic obstructive pulmonary disease: a randomized trialAm J Med2000109320721210974183
- BrooksDKripBMangovski-AlzamoraSGoldsteinRSThe effect of postrehabilitation programmes among individuals with chronic obstructive pulmonary diseaseEur Respir J2002201202912166571
- RiesALKaplanRMMyersRPrewittLMMaintenance after pulmonary rehabilitation in chronic lung disease: a randomized trialAm J Respir Crit Care Med2003167688088812505859
- SpencerLMAlisonJAMcKeoughZJMaintaining benefits following pulmonary rehabilitation: a randomised controlled trialEur Respir J201035357157719643944
- FoglioKBianchiLAmbrosinoNIs it really useful to repeat outpatient pulmonary rehabilitation programs in patients with chronic airway obstruction? A 2-year controlled studyChest200111961696170411399693
- HillKBansalVBrooksDGoldsteinRSRepeat pulmonary rehabilitation programs confer similar increases in functional exercise capacity to initial programsJ Cardiopulm Rehabil Prev200828641041419008697
- BeauchampMKEvansRJanaudis-FerreiraTGoldsteinRSBrooksDSystematic Review of Supervised Exercise Programs After Pulmonary Rehabilitation in Individuals With COPDChest201314441124113323429931
- EmeryCFShermerRLHauckERHsiaoETMacIntyreNRCognitive and psychological outcomes of exercise in a 1-year follow-up study of patients with chronic obstructive pulmonary diseaseHealth Psychol200322659860414640857
- PittaFTroostersTSpruitMAProbstVSDecramerMGosselinkRCharacteristics of physical activities in daily life in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2005171997297715665324
- Garcia-AymerichJLangePBenetMSchnohrPAntóJMRegular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: a population based cohort studyThorax200661977277816738033
- Cindy NgLWMackneyJJenkinsSHillKDoes exercise training change physical activity in people with COPD? A systematic review and meta-analysisChron Respir Dis201291172622194629
- PittaFTroostersTProbstVSLangerDDecramerMGosselinkRAre patients with COPD more active after pulmonary rehabilitation?Chest2008134227328018403667
- StortiKLPetteeKKBrachJSTalkowskiJBRichardsonCRKriskaAMGait speed and step-count monitor accuracy in community-dwelling older adultsMed Sci Sports Exerc2008401596418091020
- WempeJBWijkstraPJThe influence of rehabilitation on behaviour modification in COPDPatient Educ Couns200452323724114998592
- MorganMLife in slow motion: quantifying physical activity in COPDThorax200863866366418663063
- KestenSCasaburiRKukafkaDCooperCBImprovement in self-reported exercise participation with the combination of tiotropium and rehabilitative exercise training in COPD patientsInt J Chron Obstruct Pulmon Dis20083112713618488436
- Van RemoortelHGiavedoniSRasteYPROactive consortiumValidity of activity monitors in health and chronic disease: a systematic reviewInt J Behav Nutr Phys Act201298422776399
- RedelmeierDABayoumiAMGoldsteinRSGuyattGHInterpreting small differences in functional status: the Six Minute Walk test in chronic lung disease patientsAm J Respir Crit Care Med19971554127812829105067