 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
The functional work capacity of chronic obstructive pulmonary disease (COPD) patients is usually assessed with walk tests such as the 6-minute walk test (6MWT) or the shuttle test. Because these exercise modalities require a controlled environment which limits their use by pulmonologists and severely restricts their use among general practitioners, different modalities of a short (1 minute or less) sit-to-stand test were recently proposed. In this study, we evaluated a new modality of a semipaced 3-minute chair rise test (3CRT) in 40 patients with COPD, and compared the reproducibility of physiological responses and symptoms during the 3CRT and their interchangeability with the 6MWT. The results demonstrate that physiological variables, heart rate, pulse oxygen saturation, work done, and symptoms (Borg dyspnea and fatigue scores), during the 3CRT were highly reproducible, and that the physiological responses and symptoms obtained during the 3CRT and the 6MWT were interchangeable for most patients. Moreover, these preliminary data suggest that patients able to perform more than 50 rises during 3 minutes had no significant disability. The simplicity and ease of execution of the 3CRT will facilitate the assessment of exercise symptoms and disability in COPD patients during routine consultations with pulmonologists and general practitioners, and will thus contribute to the improved management of COPD patients.
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
The six-minute walk test (6MWT) is an established procedure to estimate functional exercise capacity in patients with a variety of diseases. For patients suffering from chronic obstructive pulmonary disease (COPD), the 6MWT is commonly applied as the exercise component of the BODE prognostic index.Citation1 It retains satisfactory prognostic value and has recently been recommended to general practitioners to assess the functional status of COPD patients.Citation2 In COPD patients, a reduced 6MWT distance is associated with increased mortality,Citation3,Citation4 a higher risk of exacerbations,Citation5 and reduced levels of activities of daily living.Citation6,Citation7 In clinical practice, the 6MWT is an important method used to objectively evaluate improvement of symptomatic (dyspnea or fatigue) and physiological responses such as distance walking, pulse oxygen saturation (SpO2), and heart rate (HR) after a therapeutic intervention.
Despite the use of standardized procedures, however, a recent multicenter study identified high variability in the 6MWT performance among the centers.Citation4 Moreover, many factors unrelated to the patient’s physical performance can influence the test outcome, including the mood, attitude, and motivation of both patient and technician. Moreover, the 6MWT is difficult to implement as a routine clinical activity, where it is often difficult to maintain the quality criteria of the test.
For these reasons, sit-to-stand tests (STST) are used by clinicians to evaluate a variety of medical conditions.Citation8–Citation10 The brevity of the test and its ability to measure physiological outcomes are of particular interest.Citation11 Several variants of the STST exist, but in general, patients are instructed to rise and sit as many times as possible within a short period (10 to 60 seconds). Overall, the simplicity and low cost of the STST provide advantages over other potential field substitutes such as the grocery shelving task or the paced step test, which require standardized environments.Citation12,Citation13 Usually, these STST showed significant correlations with established tests for exercise capacity such as the distance walked during 6 minutes (r=0.75)Citation14 or lower limb muscular strength (r=0.38),Citation15 suggesting a link between simple exercise tests and clinical outcomes. For example, Puhan et alCitation16 recently confirmed in a prospective cohort of 409 COPD patients that patients with a maximal performance of 11.8±6.3 rises during 1 minute had a higher 2-year risk of mortality (but not of exacerbations) than those with 19.5±8.7 rises. These authors concluded that availability of such a simple test may close an important gap in the evaluation of the prognosis of COPD patients across different settings. However, readers must realize that patients who were not able to perform more than 12 rises during 1 minute had a very limited maximal mechanical and metabolic power, estimated near 40 watts or 10 mL O2 · min−1 · kg−1 (for 75 kg), respectively, which is a clinically evident condition to suspect a high risk of mortality. Therefore, in addition to short STST, it would be extremely valuable to have an alternative walking test that could realistically be performed during a standard consultation and that would provide physiological and symptomatic responses comparable to those observed during the 6MWTCitation16 (or shuttle test). In addition to the predictive clinical outcomes, such a test would facilitate identification of COPD-related physical disability and thus improve routine clinical management of the disease.
We hypothesized that a 3-minute chair rise test (3CRT) elicits symptomatic and physiological responses similar to those observed with walking tests, notably the 6MWT. To test this hypothesis and the feasibility of this kind of exercise, we performed three modalities of a 3CRT in a convenient and limited sample of 40 patients with stable COPD. The three modalities differed only in the number of chair rises imposed during the first minute (12, 15, or 20 [3CRT-12, 3CRT-15, and 3CRT-20, respectively]), and the tests were repeated 10 days later to ensure reproducibility. The choice to fix a rhythm over the first minute is only based on our observation that this modality can reduce the variability due to patient comportment at the time of the start of an exercise test. We also compared the patients’ physiological and symptomatic responses during the 3CRT and 6MWT performed on the same day. This initial report strives to provide physiological rational and experimental evidence to find the best compromise between simplicity and robustness for a repeatable functional evaluation exercise with potential clinical and physiological consistency.
Materials and methods
Patients
The study was approved by the ethical committee of the University Hospital Grenoble. Patients received detailed information about the study and gave written consent to participate. shows the anthropometric measurements and functional status (for at least 8 weeks) of the 40 stable COPD patients recruited during a current consultation. Only patients with a functional limitation of the lower limbs were excluded from the study. These patients were mainly classified as Global Initiative for Chronic Obstructive Lung Disease (GOLD) II and III, and three patients were GOLD IV and I. Therefore, we pooled the results of GOLD I + II and GOLD III + IV.Citation17
Table 1 Anthropometric, clinical, and functional characteristics of the COPD patients
Study design
Patients made two visits (V1 and V2) separated by 2 to 10 days. At each visit, patients were examined to assess clinical and functional respiratory stability and then asked to perform the 6MWT, 3CRT-12, 3CRT-15, and 3CRT-20 in succession.
The order of the tests was not randomized, but each exercise test was separated by at least 20 minutes, even if HR and SpO2 had returned to baseline values before the end of the interval.
At V1, patients completed three self-reported instruments to assess 1) dyspnea according to the modified Medical Research Council dyspnea scale for the calculation of BODE index,Citation18 2) health impairment status using the St George’s Respiratory Questionnaire,Citation19 and 3) disability due to dyspnea with the DIsability RElated to Copd Tool (DIRECT).Citation20 The latter questionnaire, which assesses the deficiency due to dyspnea in COPD patients, was recently validated in comparison with other references (Saint George’s Respiratory Questionnaire activity and the London Handicap Scale) with a high Cronbach’s alpha coefficient (0.95).
Resting pulmonary function and 6MWT
Resting pulmonary function and the 6MWT were performed at V1 and V2. The 6MWT was performed, according to American Thoracic Society statement,Citation21 twice during V1 to assess immediate repeatability, and the best result was used for comparisons and as a reference for subsequent analysis.
Description of the 3CRT
While the patient was sitting at rest on a standard chair (floor to seat height 48 cm), the instructions for the conduct of the exercise and for the comprehensive use of the Borg scaleCitation22 (dyspnea and fatigue) were explained as follows:
The exercise is to stand and sit during 3 minutes. Throughout the test you must keep your hands on your hips. I’ll give you the rhythm during the first minute by a simple verbal order: “sit”, “stand” (or by doing the sit-to-stand with you). During the last 2 minutes you will try to rise and sit as many times as possible. I will tell you the remaining time verbally: “only another minute and 30 seconds”, “only another minute”, “only another 30 seconds”. At any time, you can slow down or speed up. If the exercise is too difficult, you can also stop and start again. You can also decide to permanently stop the test before the end of 3 minutes if you feel too tired or breathless.
At the end of the exercise, physiological data (SpO2, HR) and symptoms (dyspnea and leg fatigue with the Borg scale) were recorded.
Statistical analysis
Distribution symmetries were assessed graphically using box plots, and normality was verified using the Shapiro–Wilk test, as necessary. Quantitative data are presented as means and standard deviations. The characteristics of the patients in the two groups (GOLD I-II and GOLD III-IV) were compared with the nonpaired Student’s t-test for normal variables and with the Mann–Whitney test for other variables. After completion of the 3CRT, patients were divided into four groups according to the quartiles (quartiles are values and not ranges) of the frequency distribution of the total number of rises, and analysis of variance was used to compare the respiratory parameters among the four groups.
To assess repeatability, we modeled the observations by a two-way mixed-effect analysis of variance (ANOVA) model where a measurement on a subject at time j (V1 or V2) is regarded as the sum of a random subject effect, a fixed time effect, a random subject–time interaction effect, and a random error. When the above ANOVA model proved to be adequate, repeatability was evaluated via the intraclass correlation coefficient. We have also assessed repeatability between the measurements at the two times by looking for systematic differences or biases between the two via the method of differences proposed by Bland and Altman.Citation23
In studies comparing two methods, generally, the main objective is to quantify the extent of agreement between the methods and determine if they agree sufficiently well to justify their interchangeable use. Among the several statistical approaches for evaluating agreement and interchangeability between two methods of measurements, those based on linear least squares regression are very popular.Citation24,Citation25 Hence, to determine if maximal physiological responses (SpO2, HR) were interchangeable between the 6MWT and 3CRT, we evaluated the agreement between these responses using a Bland–Altman plot.Citation23 To strengthen the conclusion of the similarities between physiological variables measured at the end of the two exercises, we applied two others regressions: the Deming and the Passing–Bablok regressions.Citation26,Citation27
Wilcoxon tests were used to determine whether maximal Borg rating symptoms (range 0–10) were different at the end of the 6MWT and 3CRT. Finally, baseline parameters were tested as predictive factors of the 3CRT-12 and 3CRT-20 results with a multivariate linear regression model using stepwise backward elimination to select the significant parameters. All statistical tests were done with Stata 12 (StataCorp LP, College Station, TX, USA), except for the comparison of methods, which was performed with the R package MethComp (Bland–Altman, Deming, and PBreg).Citation28
Results
All patients were able to perform all of the exercise tests (3CRT and 6MWT). Anthropometric, clinical, and functional characteristics of the COPD patients are shown in .
Feasibility and repeatability of performance in the 3CRT
ANOVA mixed-effect modeling seemed adequate and showed that for the 3CRT (12, 15, 20) and the 6MWT, the visit factor had no effect (no significant differences between the readings of any subject across visits) and reflected only the variability between subjects (rows 4 to 6 of ). This was also confirmed by the nonsignificant bias in the difference between the readings at the two visits (row 3 of ).
Table 2 Repeatability of the 6MWT and each modality of the 3CRT
The repeatability of the total number of rises was very high, with an intraclass correlation (ICC) >0.80 for all modalities (). Three patients (all GOLD IV) were unable to follow the imposed 20-rise rhythm (two due to breathlessness and one for knee pain), and they stopped before the end of the third minute. In contrast, for the 3CRT-12 and 3CRT-15 modalities, all patients were able to follow the rhythm of rises during the first minute and to complete the test (; ).
Table 3 Repeatability of SpO2, HR, dyspnea, fatigue, and number of rises
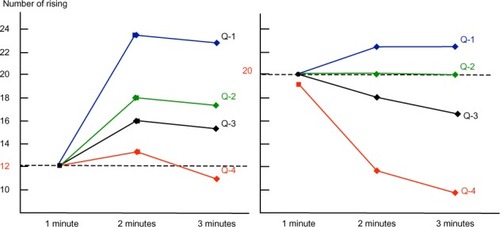
Figure 1 Number of rises per minute in patients grouped by quartiles (Q) for the 3CRT-12 and 3CRT-20.
Abbreviations: 3CRT-12, 3-minute chair rise test – 12 rises; 3CRT-20, 3-minute chair rise test – 20 rises.
Repeatability and interchangeability of maximal physiological and symptomatic responses in the 3CRT and 6MWT
shows that for this population, the maximal physiological responses (SpO2, HR) were similar at the end of the 6MWT and the three 3CRT modalities. The repeatability of SpO2 and HR was good for all four tests (ICC >0.80). The repeatability of the symptomatic responses was better for the 3CRT (12, 15, 20) modalities than the 6MWT, but the ICC values were less than 0.80 (). The interchangeability of the maximal values for SpO2 and HR was confirmed by each statistical test described in the methods (an example of these regression analyses is shown for maximal SpO2 at the end of the 3CRT-20 in ). shows that for the majority of patients, the intensity of dyspnea was higher after the 3CRT than after the 6MWT. Notably, 56% of patients had higher Borg dyspnea scores, and 64% had higher fatigue scores at the end of the 3CRT-20 than after the 6MWT.
Table 4 End exercise values for SpO2 and HR during the 6MWT and each 3CRT modality performed at V2
Table 5 Borg dyspnea and fatigue scoresCitation22 at the end of the 6MWT and each 3CRT modality
Outcomes of the 3CRT classified by performance quartiles (total number of rises)
reports the main clinical and functional characteristics of patients classified in quartiles (least [Q1] to most severely [Q4] impaired) of the maximal performance in the 3CRT-20 (number of rises in 3 minutes). Only the functional parameters, including the 6MWT, BODE index, and DIRECT score, were significantly different between each quartile. and show the spontaneous number of rises at the end of each minute of each modality. The most severely impaired patients (Q4) were able to sustain the 12-rise rhythm over the second and third minutes but showed a dramatically reduced spontaneous rhythm (below 12) in the final 2 minutes of the 3CRT-20. As a consequence of the spontaneous rhythm adjustments, the total number of chair rises for the Q4 patients was similar in the three modalities. Conversely, Q1 patients immediately increased their spontaneous rhythm during the 3CRT-12 and 3CRT-15 to approximately the same rhythm observed during the 3CRT-20, resulting in a significantly better total performance in the 3CRT-20 than in the 3CRT-12. This trend was also observed for the Q2 patients during the 3CRT-20. The maximal number of rises in the 3CRT was predicted by a multivariate linear regression model including age, body mass index, transfer factor for carbon monoxide (%), and DIRECT score (r2=0.50 and 0.56 for 3CRT-12 and 3CRT-20, respectively) ().
Table 6 Main clinical and functional characteristics for each quartile of the overall performance in the 3CRT-20
Discussion
This exploratory study demonstrated that 1) the 3CRT, an adapted STST, elicited reproducible sensory and physiological responses in a convenient sample of patients with COPD, and 2) physiological responses measured at the end of the 3CRT were similar to and interchangeable with those obtained at the end of the 6MWT, whereas Borg dyspnea and fatigue scores were generally higher after the 3CRT. Thus, the 3CRT has the potential to be at least as successful as the 6MWT for evaluating exercise symptoms and detecting a significant loss of work capacity, the two being major components of disability in an individual COPD patient.
Detecting disability in COPD
The International Classification of Functioning, Disability and Health promoted by the World Health Organization noted that reduced functional capacity is a pivotal determinant of disability and can contribute to activity restriction and reduced participation during chronic disease.Citation29 In COPD patients in particular, such restrictions are relatively independent of the decline in respiratory functionCitation30 and are the strongest predictor of all-cause mortality.Citation31 Two of the major treatment goals for COPD patients are to improve their functional status and their participation and performance in physical activities, which are both independent predictors of exacerbations, hospital admissions, quality of life, and mortality.Citation31,Citation32 It is therefore essential that the general practitioner or lung specialist is able to easily detect disability and evaluate its magnitude and determinants. Activity and participation restrictions are generally explored by questionnaires and activity monitors for research purposes.Citation33 To complement these, the patient’s work capacity is assessed with different maximal exercise tests (cycling or walking oxygen consumption [VO2]) or with simpler and less expensive field exercise tests in standardized environments. Many field exercise tests have been developed to estimate maximal or submaximal work capacity and classify patients according to the mean metabolic power attained. For example, the average power is expressed as the distance traveled during a set time for the 6MWT, and as the time required to perform a specific task for the grocery shelving test.Citation12 Regardless of their specific modalities, most field tests are more or less repeatable and correlate logically with the physiological responses. In addition to the physiological and methodological requirements (repeatability, validity, and responsiveness), a field stress test must be easily performed. In this regard, a recent review by Kocks et aCitation12 pointed out that although the 6MWT is the most reliable semi-laboratory tool to assess the global functional capacity of COPD patients, its use is limited by its impracticality. Indeed, the 6MWT requires a corridor without passages that might influence the patient’s walking pace. The final performance and reproducibility of the 6MWT depend on the manner in which the investigator conducts the test and the severity of the patient’s disease, both of which affect the maximal response. Because these influences are difficult to codify, the 6MWT is moderately repeatable, and the clinically significant threshold varies with the nature and severity of the medical condition. Finally, for a field test to be widely adopted, it must be feasible within the usual environment of the medical consultation, and the patient’s physiological and sensory responses must be reproducible.
Repeatability of the physiological and sensory responses of the 3CRT
To define the most appropriate protocol in terms of feasibility, repeatability, and physiological responses, we developed three 3CRT modalities that varied in the imposed rhythm during the first minute (12, 15, or 20 rises).
We hypothesized that imposing the frequency of rises during the first minute would reduce the variability associated with different patient behaviors at the start of the test. In addition, the rhythm could be adjusted in the final 2 minutes if the initial rhythm was too high for severely impaired patients. Conversely, for subjects who were less limited by ventilatory constraints and symptoms, the verbal announcement every 30 seconds during the final two minutes encouraged them to increase the rise frequency and allowed them to approach their maximal aerobic power by the end of the 3 minutes. Our results (; ) confirm that the less limited patients did indeed make these adjustments. Under these test conditions, we observed a significant repeatability for the number of rises, maximal SpO2, HR, and dyspnea and muscle fatigue scores. These results suggest that the 3CRT may have better interindividual reproducibility than the 6MWT, and this needs to be confirmed in a larger population of COPD patients and in a multicenter study.
Interchangeability of physiological responses and symptoms between the 3CRT and 6MWT
The significant correlations (R=0.54–0.65) between the distance covered during the 6MWT and the maximal number of rises during the 3CRT (12, 15, 20) demonstrate that the maximal or submaximal power generated by the two tests are more or less correlated, as has been reported in another sit-to-stand study.Citation14 The physiological responses at the end of the two tests were also highly correlated, and the mean maximal SpO2 and HR were not statistically different, except for HR in 3CRT-20 (). However, correlations do not signify interchangeability. R measures the linear relationship between the tests, but it cannot detect a bias constant or proportional bias and therefore does not measure the agreement. Furthermore, the R-value can be artificially high if the range of data values is wide, as has frequently been observed in previous studies. Other coefficients (intraclass or concordance correlation coefficient) are often used, but these indexes depend on the variability between subjects. Because of these limitations, we tested Deming and Passing–Bablok regressions to examine the interchangeability beyond the statistical power of the regression coefficient.Citation28 Indeed, the Deming regression is an orthogonal least squares regression used when measurement errors are present in the two conditions.Citation26 Because neither the 6MWT nor 3CRT can be considered as the gold standard for each other, the Deming regression 1) assesses the regression of each measured variable (SpO2 and HR) on the other and 2) determines if the slope and intercept of the two regression lines are equal to 1 and 0, respectively. The Deming regression provides an unbiased estimate of the slope. To implement this, the procedure requires the variance ratio of the two methods to be known. In our case, we have used the data from V1 to estimate this ratio. The Passing–Bablok regressionCitation27 is a nonparametric rank regression, where the slope of the regression line is calculated as the median of all possible slopes (). It is resistant to outliers but gives an unbiased slope estimate only if the standard deviations for the two methods are of equal size. In this study, all of these complementary approaches converged to predict high interchangeability between physiological responses induced by the 6MWT and 3CRT. If the interchangeability observed during this single center study is confirmed by the results of an ongoing multicenter study, we will conclude that the functional responses induced by these two types of exercise are individually interchangeable. On the other hand, the 3CRT-15 and 3CRT-20 modalities resulted in higher Borg dyspnea and fatigue scores than the 6MWT. These findings may reflect the different types of muscular work required for the 3CRT versus 6MWT and the subsequent effects on ventilatory responses and the perceived quantity (or quality) of dyspnea and fatigue. These hypotheses must be confirmed by a study with therapeutic interventions or a rehabilitation program.
Physiological characteristics of 3CRT
An advantage of an STST is it provides the ability to estimate the mechanical and metabolic power performed. The supplied work (joules) is the product of the movement of the mass and the distance. The raised mass is the total body mass less 12% for the mass of the feet and legs: M×0.88. For a subject of 175 cm, sitting with horizontal thighs, the sit-to-stand movement from a standard chair represents work of,
In terms of VO2, each 1 W · kg−1 increase in metabolic spending represents an additional spending of 12 mL O2 · min−1 · kg−1 (for a delta efficiency of 24%). If the internal work is negligible (in healthy subjects), the total VO2 is estimated to be ~15 mL O2 · min−1 · kg−1 (total VO2 = rest VO2 [3.5 mL O2 · kg−1] + exercise VO2). These estimates remain to be confirmed in an ongoing study conducted in a large population of COPD patients and age-matched healthy subjects.
Limits and weaknesses of the study
This proof-of-concept study needs to be extended to a larger population of COPD patients to evaluate a potential ceiling effect of the 3CRT. A control group could also help to detect significant exercise intolerance notably in age-paired, mild COPD patients or in smokers suspected to have an obstructive pulmonary disease. As for other field tests, it may be interesting to explore if the 3CRT is reflective of activities of daily living. However, a recent study demonstrates that simple tests such as the 6MWT and the STST (and the Zutphen Physical Activity Questionnaire) cannot be used to reliably predict physical activity.Citation35
Practical recommendations and further validations
Because an exercise test gives only partial information on disability, the test should be complemented with specific questionnaires exploring the effects of functional impairment. From the results of this preliminary study, it could be suggested that the patient should first complete a self- administered questionnaire to detect a possible functional impairment (DIRECT)Citation20 and then undergo the 3CRT to confirm the questionnaire screening and to estimate the patient’s functional capacity. Not only are these two assessments easy to combine, but the multivariate linear analysis indicated that the DIRECT score was one of the main determinants of the final performance of the 3CRT, together with age, body mass index, and transfer factor for carbon monoxide. Using a combination of DIRECT (or other similar questionnaires) and the 3CRT, a significant handicap would be suggested by a DIRECT score greater than 12 and an inability to achieve more than 50 rises during the 3CRT. Moreover, it appears that the 3CRT-20 modality can discriminate between patients who are able to sustain the rhythm imposed during the first minute and those who are not. Thus, these preliminary results suggest that the 3CRT-12 modality should be reserved for patients with more impaired functional status and a DIRECT score of less than 12. However, these assumptions are putative and await further evaluation and validation by a planned study to test the validity and the responsiveness of 3CRT and DIRECT in a standard program of rehabilitation.
Acknowledgments
We thank Professor Anestis Antoniadis for his valuable statistical advice and Anne M O’Rourke, PhD for editing the manuscript.
Supplementary materials
Figure S1 Evaluation of the interchangeability of maximal oxygen desaturation at the end of the 6MWT and 3CRT-20 in COPD patients.
Notes: Complementary statistical tests were as follows: Bland–Altman plot (bias and limits of agreement [±1.96 SD]), Bland–Altman plot with smoothed regression (regression curve and 95% CI), Deming regression (regression of each method on the other in black, Deming regression line in red), and Passing–Bablok plot (regression line with 95% CI; the blue color of the figure indicates that all data are in the CI).
Abbreviations: 3CRT-20, 3-minute chair rise test – 20 rises; 6MWD, 6-minute walk distance; 6MWT, 6-minute walk test; CI, confidence interval; COPD, chronic obstructive pulmonary disease; SD, standard deviation.
![Figure S1 Evaluation of the interchangeability of maximal oxygen desaturation at the end of the 6MWT and 3CRT-20 in COPD patients.Notes: Complementary statistical tests were as follows: Bland–Altman plot (bias and limits of agreement [±1.96 SD]), Bland–Altman plot with smoothed regression (regression curve and 95% CI), Deming regression (regression of each method on the other in black, Deming regression line in red), and Passing–Bablok plot (regression line with 95% CI; the blue color of the figure indicates that all data are in the CI).Abbreviations: 3CRT-20, 3-minute chair rise test – 20 rises; 6MWD, 6-minute walk distance; 6MWT, 6-minute walk test; CI, confidence interval; COPD, chronic obstructive pulmonary disease; SD, standard deviation.](/cms/asset/7440ba9f-0b67-4a18-ad6b-eb1f6a97b934/dcop_a_59855_sf0001_c.jpg)
Table S1 Number of rises attained at the end of each minute for the three modalities of the 3CRT
Table S2 Multivariate linear regression model predicting the final performance (number of rises) for 3CRT-12 and 3CRT-20
Disclosure
The authors report no conflicts of interest in this work.
References
- CelliBRCoteCGMarinJMThe body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary diseaseN Engl J Med2004350101005101214999112
- KocksJWAsijeeGMTsiligianniIGKerstjensHAvan der MolenTFunctional status measurement in COPD: a review of available methods and their feasibility in primary carePrim Care Respir J201120326927521523316
- Pinto-PlataVMCoteCCabralHTaylorJCelliBRThe 6-min walk distance: change over time and value as a predictor of survival in severe COPDEur Respir J2004231283314738227
- CasanovaCCelliBRBarriaPSix Minute Walk Distance Project (ALAT)The 6-min walk distance in healthy subjects: reference standards from seven countriesEur Respir J201137115015620525717
- MarinJMCarrizoSJCasanovaCPrediction of risk of COPD exacerbations by the BODE indexRespir Med2009103337337819013781
- PittaFTroostersTSpruitMAProbstVSDecramerMGosselinkRCharacteristics of physical activities in daily life in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2005171997297715665324
- ChaoPWRamsdellJRenvallMVoraCDoes a history of exercise in COPD patients affect functional status? A study using a lifetime physical activity questionnaire investigates a correlation between exercise and functional status as evidenced by six-minute walk distanceCOPD20118642943622149403
- BohannonRWReference values for the five-repetition sit-to-stand test: a descriptive meta-analysis of data from eldersPercept Mot Skills2006103121522217037663
- BuatoisSMiljkovicDManckoundiaPFive times sit to stand test is a predictor of recurrent falls in healthy community-living subjects aged 65 and olderJ Am Geriatr Soc20085681575157718808608
- BrodinELjungmanSSunnerhagenKSRising from a chair: a simple screening test for physical function in predialysis patientsScand J Urol Nephrol200842329330018432536
- NetzYAyalonMDunskyAAlexanderN‘The multiple-sit-to-stand’ field test for older adults: what does it measure?Gerontology200450312112615114032
- HillCJDenehyLHollandAEMcDonaldCFMeasurement of functional activity in chronic obstructive pulmonary disease: the grocery shelving taskJ Cardiopulm Rehabil Prev200828640240919008696
- PerraultHBarilJHenophySRycroftABourbeauJMaltaisFPaced-walk and step tests to assess exertional dyspnea in COPDCOPD20096533033919863362
- OzalevliSOzdenAItilOAkkocluAComparison of the Sit-to-Stand Test with 6 min walk test in patients with chronic obstructive pulmonary diseaseRespir Med2007101228629316806873
- JonesSEKonSSCanavanJLThe five-repetition sit-to-stand test as a functional outcome measure in COPDThorax201368111015102023783372
- PuhanMASiebelingLZollerMMuggensturmPter RietGSimple functional performance tests and mortality in COPDEur Respir J201342495696323520321
- Global initiative for chronic obstructive lung diseaseGlobal strategy for the diagnosis, management and prevention of chronic obstructive lung disease2011 http://www.goldcopd.com
- BestallJPaulEGarrodRGarnhamRUsefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary diseaseThorax19995458158610377201
- BouchetCGuilleminFHoang ThiTHCornetteABrianconSValidation du questionnaire St Georges pour mesurer la qualite de vie chez les insuffisants respiratoires chroniquesRev Mal Respir1996134346 French8650415
- AguilaniuBGonzalez-BermejoJRegnaultADisability related to COPD tool (DIRECT): towards an assessment of COPD-related disability in routine practiceInt J Chron Obstruct Pulmon Dis2011638739821760726
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function LaboratoriesATS statement: guidelines for the six-minute walk testAm J Respir Crit Care Med2002166111111712091180
- BorgGAPsychophysical bases of perceived exertionMed Sci Sports Exerc19821453773817154893
- BlandJMAltmanDGMeasuring agreement in method comparison studiesStat Methods Med Res19998213516010501650
- JohnsonRAssessment of bias with emphasis on method comparisonClin Biochem Rev200829Suppl 1S37S4218852855
- LinLHedayatASSinhaBYangMStatistical methods in assessing agreement: models, issues, and toolsJ Am Stat Assoc200297257270
- LinnetKEvaluation of regression procedures for methods comparison studiesClin Chem19933934244328448852
- PassingHBablokA new biometrical procedure for testing the equality of measurements from two different analytical methods. Application of linear regression procedures for method comparison studies in clinical chemistry, Part IJ Clin Chem Clin Biochem198321117097206655447
- CarstensenBComparing methods of measurement: Extending the LoA by regressionStat Med201029340141019998394
- UstünTBChatterjiSBickenbachJKostanjsekNSchneiderMThe International Classification of Functioning, Disability and Health: a new tool for understanding disability and healthDisabil Rehabil20032511–1256557112959329
- EisnerMDIribarrenCBlancPDDevelopment of disability in chronic obstructive pulmonary disease: beyond lung functionThorax201166210811421047868
- WaschkiBKirstenAHolzOPhysical activity is the strongest predictor of all-cause mortality in patients with COPD: a prospective cohort studyChest2011140233134221273294
- Garcia-AymerichJHernandezCAlonsoAEffects of an integrated care intervention on risk factors of COPD readmissionRespir Med200710171462146917339106
- PittaFTroostersTProbstVSSpruitMADecramerMGosselinkRQuantifying physical activity in daily life with questionnaires and motion sensors in COPDEur Respir J20062751040105516707399
- AsmussenEBonde-PetersenFApparent efficiency and storage of elastic energy in human muscles during exerciseActa Physiol Scand19749245375454455009
- van GestelAJClarenbachCFStöwhasACPredicting daily physical activity in patients with chronic obstructive pulmonary diseasePLoS One2012711e4808123133612
