Abstract
Patients with chronic obstructive pulmonary disease (COPD) fall frequently, although the risk of falls may seem less important than the respiratory consequences of the disease. Nevertheless, falls are associated to increased mortality, decreased independence and physical activity levels, and worsening of quality of life. The aims of this systematic review was to evaluate information in the literature with regard to whether impaired postural control is more prevalent in COPD patients than in healthy age-matched subjects, and to assess the main characteristics these patients present that contribute to impaired postural control.
Methods
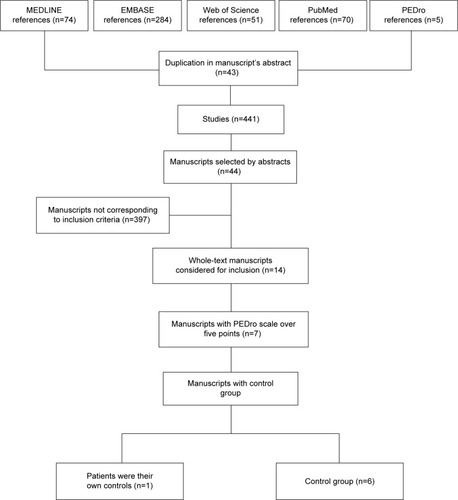
Five databases were searched with no dates or language limits. The MEDLINE, PubMed, EMBASE, Web of Science, and PEDro databases were searched using “balance”, “postural control”, and “COPD” as keywords. The search strategies were oriented and guided by a health science librarian and were performed on March 27, 2014. The studies included were those that evaluated postural control in COPD patients as their main outcome and scored more than five points on the PEDro scale. Studies supplied by the database search strategy were assessed independently by two blinded researchers.
Results
A total of 484 manuscripts were found using the “balance in COPD or postural control in COPD” keywords. Forty-three manuscripts appeared more than once, and 397 did not evaluate postural control in COPD patients as the primary outcome. Thus, only 14 studies had postural control as their primary outcome. Our study examiners found only seven studies that had a PEDro score higher than five points. The examiners’ interrater agreement was 76.4%. Six of those studies were accomplished with a control group and one study used their patients as their own controls. The studies were published between 2004 and 2013.
Conclusion
Patients with COPD present postural control impairment when compared with age-matched healthy controls. Associated factors contributing to impaired postural control were muscle weakness, physical inactivity, elderly age, need for supplemental oxygen, and limited mobility.
Introduction
Chronic obstructive pulmonary disease (COPD) is a preventable and treatable illness with effects on the whole body that can contribute to loss of functional capacity for the patient.Citation1
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) document (2011)Citation1 advises proper attention to not only respiratory treatment but also to extrarespi-ratory consequences in COPD patients. According to some studies, impaired balance may be one important extrarespiratory morbidity leading to loss of functional independence and falls.Citation2 However, postural control does not figure in the GOLD report as an important disease-related association, and this is an important aspect that should be assessed.
Loss of postural control is one of the most common comorbidities in elderly subjects.Citation2 It is known that 30% of subjects over 60 years of age fall at least once a year, and that the fall rate increases up to 45% in subjects over 70 years of age.Citation2 Impaired postural control is more frequent when the elderly person has a chronic disease. The PLATINO study showed that the prevalence of COPD increases in older subjects.Citation3 Thus, there is some evidence that can explain a possible association between aging, COPD, and impaired postural control that might predispose these patients to an increased risk of falls.
Falls in elderly subjects have serious consequences in terms of functional independence, social interaction, and life expectancy.Citation4,Citation5 Risk factors for falls in the elderly, such as lower limb muscle weakness, labyrinthine disease, functional performance deficit, and the capacity to align the body once out of balance are well documented.Citation4,Citation5 These risk factors are also common in COPD patients.Citation6,Citation7 Although the risk of falls may seem less important than the respiratory consequences of the disease, falls are associated with increased mortality, decreased independence and level of physical activity, and worsening of quality of life in both COPD patients and healthy age-matched subjects.Citation8–Citation10 In addition, the consequences of falls are expensive for the health care system.Citation10 Therefore, assessment of the causes of impaired postural control in COPD patients may contribute to preventing the consequences of such falls. Roig et alCitation2 and Beauchamp et alCitation9 have already shown that COPD patients may have impaired postural control, but the relevant risk factors are still unknown.
Therefore, the aim of this systematic review was to evaluate the literature to determine if impaired postural control is more prevalent in COPD patients than in healthy age-matched subjects, and as the novel finding, we also aimed to assess the main characteristics that contribute to impaired postural control in these patients.
Methods
This study was a systematic review of the prevalence of impaired postural control in COPD patients, without meta-analysis. The protocol was submitted and approved by the ethics committee of our University and all patients gave their written consent. Postural control is usually assessed by means of the force platform, being the center of vertical force calculated from the ground-reaction forces projected from the body, and is the center of the distribution of the total force applied to the supporting surface.Citation4 It reflects the trajectory of the center of mass and the amount of torque applied at the support surface to control body mass acceleration.Citation9 Measurement of certain variables in COPD patients enables us to detect and qualify sudden changes, and is clinically useful for detecting and qualifying sensorimotor postural deficiencies (eg, impaired postural control) such as increased postural sway. Usually, the higher the mean radius of the distribution of center of vertical force, the poorer the ability to control balance.Citation4,Citation9
Search strategy
Seven databases (LILACS, MEDLINE, PubMed, SciELO, EMBASE, Web of Science, and PEDro) were searched with no dates or language limits. However, only English language studies were found at the time of searching. We used Boolean logic with AND and OR operators, the MeSH terms of the Health Care subheading within the MeSH Tree Structures, and “balance”, “postural control”, and “COPD” as the MeSH terms that best fit our search strategy. The searches were guided by a health science librarian and performed on March 27, 2014.
Studies yielded by the database search strategy were assessed independently in a blinded manner by two researchers. Both researchers closely evaluated the inclusion and exclusion criteria, treatment methods, interventions, target sample, and study design. Studies without diagnostic criteria for COPD and studies with qualitative assessments were excluded. All studies were firstly screened by title and abstract. After eliminating duplicated studies, the two independent examiners read the paper abstracts following the previous established criteria. The agreement rate on study exclusion was 89%. The included manuscripts were read and assessed according to the PEDro criteria. For this analysis, the examiners’ interrater agreement was 89.7%. Any disagreement between the examiners was resolved by a technical discussion.
Only studies that evaluated postural control in COPD patients as their main outcome and that scored more than five points on the PEDro scale were included.Citation11 The five-point score was established as the threshold on the PEDro scale because this limit is considered to determine whether a study is well designed or not.
Assessment of methodological quality
We used the PEDroCitation11 scale to assess the methodological quality of the studies. This scale was developed to validate clinical trials and is one of the most commonly used scales worldwide.
The total score on the PEDro scale may reach eleven points. For every criterion on this scale, a one or zero score is attributed. “The score can only be attributed when a criteria is clearly fulfilled. If there is a no possibility to fulfill it no score are to be given.”Citation11 The PEDro score uses the following assessment criteria: specific eligibility; intergroup randomization; hidden group allocation; similarity of intergroup prognostic indicators; blinded groups; blinded examiners; blinded assessors; a dropout rate lower than 15%; treatment or, at least, intention to treat; intergroup statistical comparison; cutoff points and variability for at least one key outcome. Every criterion is considered as one score except for the first one.
Results
shows the manuscript selection procedure from screening to final analysis. Initially, 484 manuscripts were found using the keywords “balance in COPD” or “postural control in COPD”. Of those, 397 studies were excluded because they did not evaluate postural control in COPD patients as their main outcome and did not score more than five points on the PEDro scale. Only 14 studies had postural controls as their primary outcome.Citation1,Citation2,Citation7,Citation10,Citation12,Citation13–Citation23 shows the manuscriptsCitation9,Citation12,Citation13,Citation16,Citation17,Citation20,Citation22 that were included in the final analysis. According to the PEDro scale, the manuscript scores ranged from six to nine points. Cross-sectional studies comprised 87.5% of the trials, and the most commonly assessed outcome variables were postural control, mobility, coordination, strength muscle, exercise tolerance, physical activity, and risk of falling. The methods most frequently used to assess the impairment of postural control were the Berg Balance Scale (BBS), the Balance Evaluation Systems Test (BESTest), the Tinetti scale, the strength platform, and posturography. Descriptions of these methods can be found elsewhere.Citation4,Citation18,Citation23
Table 1 Characterization of studies included in the final analysis
shows the main characteristics of the studies including main author, subject age, forced expiratory volume in the first second, fall rates, and correlations with impaired postural control.
Table 2 Study identification and sample characterization
shows the assessment of dynamic postural control (eg, assessment of postural control while accomplishing any limb or trunk movement) in COPD patients and controls. In all seven studies, the COPD patients showed loss of dynamic postural control when compared with healthy age-matched subjects. For postural control assessment, two studies used the BBS, two used the Activities-specific Balance Confidence test, two used the Timed Up and Go (TUG) test, and one used the BESTest with Clinical Instrument Assess and the Tinetti scale. The main conclusions of the authors were that COPD patients present neurofunctional alteration, motor incoordination, and loss of postural control when performing daily tasks. Further, these patients also have an increased risk of falls, a lower level of physical activity, muscle weakness, loss of proprioceptive control, and higher body oscillation frequency.
Table 3 Outcomes reported by the included studies
Discussion
The main findings of this systematic review are as follows. First, impairment of postural control is more frequent in COPD patients than in healthy age-matched subjects. Second, impairment of postural control is associated with loss of muscle strength. Third, impairment of postural control is associated with a lower functional capacity and independence and a lack of physical activity.
Impairment of postural control in the elderly is well established.Citation8,Citation19,Citation23–Citation25 However, postural control has only been studied in COPD patients in the past few years and its assessment has not been standardized in this population, which has led to inconsistent results in the studies.
Hamilton et alCitation24 showed that the latency time for the Achilles and patellar tendon reflex is longer in COPD patients than in control subjects. The authors believe that this nerve conduction delay is secondary to peripheral muscle impairment in COPD patients, and this delay could affect the reaction time for correction of postural control.
Butcher et alCitation12 assessed postural control in two groups of COPD patients, ie, with and without use of continuous oxygen therapy, and compared the results for both groups with those in healthy controls. They found that COPD patients had deficits in functional balance, coordination, and mobility tasks that were associated with disease severity or with differences in activity levels. The activities tested were the TUG test, the fast gait speed test, posturography, and the finger-to-nose and toe-tapping coordination tests. Patients who required supplemental oxygen showed worse coordination and a longer delay to complete the finger-to-nose test when compared with the healthy control group. The COPD oxygen group also had a greater sway index and peak sway index with eyes open while standing in the platform test than the healthy control group. In addition, the COPD oxygen group performed worse on the TUG test and on the fast gait speed test than the COPD group that did not require oxygen.
The most significant deficits in balance, coordination, and mobility were found in the oxygen-dependent group, but these findings should be interpreted cautiously because this group had more severe disease.
Smith et alCitation20 found that COPD patients had increased displacement of mediolateral center of pressure and increased angular motion of the hip in the standing position when compared with healthy controls. Mediolateral center of pressure displacement was further increased in these patients during upper limb exercise, but was unchanged in controls. However, anteroposterior center of pressure displacement did not differ between the groups. The authors concluded that COPD patients have increased mediolateral center of pressure displacement at rest and during upper limb exercise, possibly as a result of increased respiratory demand given by the trunk muscles contraction.
It is also possible to consider the hypothesis that this mediolateral body oscillation in COPD patients may be due to thoracoabdominal asynchrony with an inadequate contribution of the thorax compartment to tidal volume that eases postural sway.Citation7
Beauchamp et alCitation16 showed that impaired postural control, evaluated by the BBS and TUG test, is frequently seen in COPD patients with a previous history of falls, a deficit in functional mobility, or a need for supplementary oxygen. They also found a small improvement in postural control (ie, improvement of BBS and TUG scores) after a 6-week multidisciplinary pulmonary rehabilitation program consisting of exercise training, breathing exercises, education, and psychological support. Accordingly, they recommend that a balance assessment should be part of routine examination in COPD patients given their high prevalence of falls. Further, the authors state that, despite this initiative having yet to be fully explored, incorporation of specific balance training and fall prevention strategies may contribute to the comprehensive treatment of COPD patients.
Two years later, Beauchamp et alCitation17 reported several other factors related to impaired postural control, ie, a decrease in muscle strength, advancing age, and decreased self-reported physical activity levels. The authors found that COPD patients had reduced balance scores on each component of the BESTest, with marked deficits (a 30% reduction) in biomechanics, transitions, and gait. Lower BBS scores, balance confidence scores, and physical activity levels were also evident in patients with COPD when compared with control subjects. Normalized peak torque for the knee extensors and flexors, ankle plantar flexors, and dorsiflexors were reduced in patients with COPD when compared with controls.
The same studyCitation17 also found that muscle strength and self-reported physical activity explained 35% of the variance in postural control in COPD patients. Although not part of the regression model, a slower reaction time to recover postural control in response to any instability was also associated with impairment of postural control.
Janssens et alCitation22 assessed postural control in COPD patients when standing on a foamy surface, and also assessed their postural control strategy according to the patient’s inspira-tory muscle strength. During an upright stance on an unstable support surface, patients with COPD showed increased body sway in the anterior-posterior direction when compared with controls. The authors showed that ankle-steered postural control was the main strategy adopted by COPD patients while standing on an unstable surface. In addition, the authors divided their sample according to inspiratory muscle strength, and found that the subgroup of patients with weaker inspiratory muscles showed greater body sway and a more ankle-steered strategy during postural control.
Although these authors did not measure respiratory muscle fiber strength, they considered that this association occurred due to the fact that decreased inspiratory muscle strength would impair proprioceptive muscle function and therefore realignment of the patient’s body.
This systematic review allows us to conclude that COPD patients have impairment of postural control when compared with healthy age-matched controls. In addition, many of the associated factors that contribute to impaired postural control, like muscle weakness, physical inactivity, and limited mobility are amenable to change with appropriate education. Although the study sample sizes were sufficient to detect differences between COPD patients and healthy age-matched controls for most of the outcomes, larger studies are required to confirm these findings.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors have no conflicts of interest to declare in relation to this work. They have no financial and personal relationships with other people or organizations that could inappropriately influence their work such as employment, consultancies, stock ownership, honoraria, paid expert testimony, speakers bureaus, retainers, patent applications/registrations, travel grants, or other funding. No tobacco company and/or pharmaceutical/other company funded any part of this manuscript. This study has not had any sponsorship and no medical writing/editorial assistance was given.
References
- RabeKFHurdSAnzuetoAGlobal Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease: GOLD executive summaryAm J Respir Crit Care Med200717653255517507545
- RoigMEngJJRoadJDReidWDFalls in patients with chronic obstructive pulmonary disease: a call for further researchRespir Med20091031257126919419852
- MenezesAMPerez-PadillaRJardimJRChronic obstructive pulmonary disease in five Latin American cities (the PLATINO study): a prevalence studyLancet20053661875188116310554
- GanançaFFGazzolaJMGanançaCFCaovillaHHGanançaMMCruzOLElderly falls associated with benign paroxysmal positional vertigoBraz J Otorhinolaryngol20107611312020339699
- TinettiMESpeechleyMGinterSFRisk factors for falls among elderly persons living in the communityN Engl J Med1988319170117073205267
- BernardSLeBlancPWhittomFPeripheral muscle weakness in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med19981586296349700144
- GaiJGomesLNobrega OdeTFactors related to falls of elderly women residents in a communityRev Assoc Med Bras20105632733220676542
- CastroAAKumpelCRangueriRCDaily activities are sufficient to induce dynamic pulmonary hyperinflation and dyspnea in chronic obstructive pulmonary disease patientsClinics (Sao Paulo)20126731932522522756
- BeauchampMKHillKGoldsteinRSGoldsteinRSJanaudis-FerreiraTBrooksDImpairments in balance discriminate fallers from non-fallers in COPDRespir Med20091031885189119592229
- MorelloRTBarkerALHainesTIn-hospital falls and fall-related injuries: a protocol for a cost of fall studyInj Prev20131936323302144
- MaherCGSherringtonCHerbertRDMoseleyAMElkinsMReliability of the PEDro scale for rating quality of randomized controlled trialsPhys Ther20038371372112882612
- ButcherSJMeshkeJMSheppardMSReductions in functional balance, coordination, and mobility measures among patients with stable chronic obstructive pulmonary diseaseJ Cardiopulm Rehabil20042427428015286536
- RoccoCCSampaioLMStirbulovRCorrêaJCNeurophysiological aspects and their relationship to clinical and functional impairment in patients with chronic obstructive pulmonary diseaseClinics (São Paulo)20116612512921437448
- AnnegarnJMeijerKPassosVLProblematic activities of daily life are weakly associated with clinical characteristics in COPDJ Am Med Dir Assoc20111328429021450242
- BeauchampMKBrooksDGoldsteinRSDeficits in postural control in individuals with COPD – emerging evidence for an important secondary impairmentMultidiscip Respir Med2010541742122958342
- BeauchampMKO’HoskiSGoldsteinRSBrooksDEffect of pulmonary rehabilitation on balance in persons with chronic obstructive pulmonary diseaseArch Phys Med Rehabil2010911460146520801268
- BeauchampMKSibleyKMLakhaniBImpairments in systems underlying control of balance in COPDChest20121411496150322116798
- GazzolaJMPerraciniMRGanançaMMFunctional balance associated factors in the elderly with chronic vestibular disorderBraz J Otorhinolaryngol20067268369017221062
- KayacanOBederSDedaGKarnakDNeurophysiological changes in COPD patients with chronic respiratory insufficiencyActa Neurol Belg200110116016511817264
- SmithMDChangATSealeHEWalshJRHodgesPWBalance is impaired in people with chronic obstructive pulmonary diseaseGait Posture20103145646020206529
- JanssensLPijnenburgMClaeysKMcConnellAKTroostersTBrumagneSPostural strategy and back muscle oxygenation during inspiratory muscle loadingMed Sci Sports Exerc2013451355136223470314
- JanssensLBrumagneSMcConnellAKProprioceptive changes impair balance control in individuals with chronic obstructive pulmonary diseasePLoS One20138e5794923469255
- Bogle ThorbahnLDNewtonRAUse of the Berg Balance Test to predict falls in elderly personsPhys Ther1996765765838650273
- HamiltonALKillianKJSummersEJonesNLMuscle strength, symptom intensity, and exercise capacity in patients with cardiorespiratory disordersAm J Respir Crit Care Med1995152202120318520771
- De TroyerALeeperJBMcKenzieDKGandeviaSCNeural drive to the diaphragm in patients with severe COPDAm J Respir Crit Care Med1997155133511349105076